www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
REVIEW
ARTICLE
Relation
between
chronic
rhinosinusitis
and
gastroesophageal
reflux
in
adults:
systematic
review
夽
Guilherme
Constante
Preis
Sella,
Edwin
Tamashiro,
Wilma
Terezinha
Anselmo-Lima,
Fabiana
Cardoso
Pereira
Valera
∗UniversidadedeSãoPaulo,FaculdadedeMedicinadeRibeirãoPreto,DepartamentodeOftalmologia,Otorrinolaringologiae CirurgiadeCabec¸aePescoc¸o,RibeirãoPreto,SP,Brazil
Received11May2016;accepted30May2016
Availableonline14July2016
KEYWORDS Rhinosinusitis; Laryngopharyngeal reflux;
Gastroesophageal refluxdisease; pH-metry;
Protonpumpinhibitor
Abstract
Introduction:The relationship betweengastroesophageal reflux disease (GERD)andchronic rhinosinusitis(CRS)isstillacontroversialissueinliterature.
Objective:Asystematicreviewoftheassociationbetweenthesetwodiseasesinadultpatients.
Methods:SystematicreviewinPubMedandCochraneDatabasewitharticlespublishedbetween 1951and2015.WeincludedallarticlesthatspecificallystudiedtherelationshipbetweenCRS andGERD.
Results:Of the436 articles found, only12 met theinclusion criteria.Eight cross-sectional articlessuggestarelationbetweenCRSandGERD,especiallyonCRSthatisrefractorytoclinical orsurgicaltreatment.However, thegroups aresmallandmethodologiesaredifferent.Four otherlongitudinalstudieshaveassessedtheeffectoftreatmentwithprotonpumpinhibitors (PPIs)ontheimprovementofsymptomsofCRS,buttheresultswereconflicting.
Conclusions:ThereseemstoberelativeprevalenceofrefluxwithintractableCRS.Thereisstill alackofcontrolledstudieswithasignificantnumberofpatients toconfirmthishypothesis. Fewstudiesspecificallyassesstheimpactoftreatmentofrefluxonsymptomimprovementin patientswithCRS.
© 2016 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Published by Elsevier Editora Ltda. This is an open access article under the CC BY license (http:// creativecommons.org/licenses/by/4.0/).
夽 Pleasecitethisarticleas:SellaGC,TamashiroE,Anselmo-LimaWT,ValeraFC.Relationbetweenchronicrhinosinusitisand gastroesoph-agealrefluxinadults:systematicreview.BrazJOtorhinolaryngol.2017;83:356---63.
∗Correspondingauthor.
E-mail:facpvalera@uol.com.br(F.C.Valera).
PeerReviewundertheresponsibilityofAssociac¸ãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial.
http://dx.doi.org/10.1016/j.bjorl.2016.05.012
Systematicreview:chronicrhinosinusitisandreflux 357
PALAVRAS-CHAVE Rinossinusite; Refluxo
laringofaríngeo; Doenc¸adorefluxo gastroesofágico; pHmetria;
Inibidordebombade prótons
Relac¸ãoentrerinossinusitecrônicaerefluxogastroesofágicoemadultos:revisão sistemática
Resumo
Introduc¸ão: A relac¸ão entre a Doenc¸a do RefluxoGastroesofágico (DRGE) ea Rinossinusite Crônica(RSC)aindaétemadecontrovérsiaemliteratura.
Objetivo: Revisãosistemáticasobreaassociac¸ãoentreessasduasdoenc¸asempacientes adul-tos.
Método: RevisãosistemáticanoPubmedeCochraneDatabasecomosartigospublicadosentre 1951e2015.Foramincluídostodososartigosqueestudassemespecificamentearelac¸ãoentre RSCeDRGE.
Resultados: Dos436artigosencontrados,apenas12satisfaziamoscritériosdeinclusão.Oito artigostransversaissugeremrelac¸ãodaRSCcomaDRGE,especialmentesobreaRSCrefratária atratamentoclínicooucirúrgicoprévio.Noentanto,osgrupossãopequenoseasmetodologias sãomuitodiferentes.Outrosquatroestudoslongitudinaisavaliaramoefeitodotratamentocom InibidoresdeBombadePrótons(IBP)sobreamelhoradossintomasdeRSC,porémosresultados foramdiscordantes.
Conclusões: Parecehaverrelac¸ãodeprevalênciaderefluxoeRSCdedifícilcontrole. Ainda faltamestudoscontroladoscomumnúmeroexpressivodepacientesparaqueseconfirmeessa hipótese.Sãoescassososestudosqueavaliem especificamenteoimpactodotratamentode refluxonamelhoradossintomasempacientescomRSC.
© 2016 Associac¸˜ao Brasileira de Otorrinolaringologia e Cirurgia C´ervico-Facial. Publicado por Elsevier Editora Ltda. Este ´e um artigo Open Access sob uma licenc¸a CC BY (http:// creativecommons.org/licenses/by/4.0/).
Introduction
Chronic rhinosinusitis (CRS) remains a major problem of public health worldwide.1 The broad consensus for
rec-ommended treatment is based on an optimal medical treatmentemphasizingtheuseofcorticosteroids.2,3
Endo-scopic nasal surgery (ENS) is indicated for cases that fail maximum medical treatment. However, multiple factors havebeenimplicatedasreasonsthatcasesofCRSbecome refractoryafteroptimizedtreatmentincludinggenotypicor phenotypicalterationofthemucosa,scarsandsynechiae, allergies,smokingandgastroesophagealacidreflux.4,5
Especially in children many studies have postulated a relationshipbetweenCRSandacidreflux,both gastroesoph-ageal reflux disease (GERD) and laryngopharyngeal reflux (LPR).6---8 However,itis difficulttoestablish adirect
rela-tionship between CRS and GERD, since both entities are highlyprevalent,whichmakesiteasierforthemtocoexist independently.9Inaddition,todatethereisnodocumented
evidenceofthispossiblerelationshipinadults.
SometheoriesofarelationbetweenacidrefluxandCRS were raised. The first is the direct exposure of the nasal andnasopharyngealmucosatogastricacid,causing inflam-mationofthemucosaandimpairedmucociliaryclearance, whichcouldcauseobstruction ofsinusostiaandrecurrent infections.10,11 Itis knownthat pHvariationsaffectciliary
motilityandmorphologyintherespiratorymucosa.12
The second hypothesis is a relationship mediated by the vagus nerve, a mechanism already proven in the lowerairway13,14andin thenasalmucosaofpatientswith
rhinitis,10 butnotinpatientswithCRS.Dysfunctionof the
autonomicnervoussystemcanleadtoreflexsinonasal
swell-ingandinflammation,andconsequentblockageoftheostia. Wong et al.15 demonstrated that by infusing saline with
hydrochloric acid in the lower esophagus of healthy vol-unteers, there was increased production of nasal mucus, increasedscoreofnasalsymptoms,andreducedpeaknasal inspiratoryflow,whichwouldsupportthistheory.
Afinalmechanismwouldbethedirectroleof Helicobac-terpylori(H.pylori).Kocetal.16observedH.pyloripresent
innasalpolyps,butnotincontroltissues,whereasMorinaka et al.17 found H. pylori through polymerase chain
reac-tion(PCR) in the nasal mucosaof patients who have CRS andgastroesophagealrefluxcomplaints.Howeverthereare conflicting findings in the literature as to whether there isagreater frequencyof H.pyloriin thenasalmucosaof patientswithCRS.18
More importantly, previous review studies failed to showaclearevidence-basedrelationshipbetweenCRSand
GERD19,20 inadults.Sincethesereviewswerepublishedat
leastfour yearsago, our objectivewas anew systematic review on the topic, to gather all the current evidence published around this issue, and to evaluate the quality andrelevanceoftheinteractionbetweenGERDandCRSin adults.
Methods
For the implementation of this systematic review, we selected all the items present in the PubMed library, developedbytheNational CenterforBiotechnology Infor-mation(NCBI)oftheUSNationalLibraryofMedicine(NLM)
Table 1 Definition of chronic rhinosinusitis in adults, accordingtoEPOS2012.2
Symptoms Nasalblockage/obstruction
Nasalcongestionorrhinorrhea
(anterior/posteriornasaldrip):
-±facialpain/pressure
-±Smellreductionorloss
Endoscopicsigns Nasalpolyps,and/or
Mucopurulentdischarge,mainly
frommiddlemeatus,and/or
Mucosaobstruction/edemamainly
onmiddlemeatus
and/orCTchanges Changesonthemucosawithin
ostiomeatalcomplex,and/or
paranasalsinuses
Cochrane Database(http://www.cochrane.org). The word searchstrategieswere:Gastroesophagealreflux;ORGERD; ORGORD;ORlaryngopharyngealreflux;ORnasopharyngeal reflux;ORpH-metry.Associatedwith:sinusitis;ORchronic rhinosinusitis;ORchronic sinusitis;OR CRS; ORpost-nasal drip.Theminimumrequirementsfortheselectionwere arti-clesin English,whichhadanabstract,publishedbetween January1,1950andDecember31,2015.
The finalsearch resulted in436 articles.Ofthese,415 had abstracts in their respective databases,and 38 were excludedbecausetheywerenotinEnglish.
The abstracts of the selected articles were carefully readbytwoauthors.Afterreading,onlythosearticlesthat specificallyevaluatedtherelationshipbetweenchronic rhi-nosinusitisandacidrefluxinadultswereincluded,resulting in12articles.
Forthisstudy,CRS criteriawereused,accordingtothe latestversionofEPOS2012,2beingdefinedasinflammation
ofthenoseandparanasalsinuses,characterizedbytwoor moresymptomsassociatedwithendoscopicortomographic signsexistingmorethan12weeks(Table1).Thearticles con-sideredwerethoseaboutbothformsofCRS,withorwithout nasalpolyposis(NSP)fortheresearchinquestion.
To include the diagnosis of GERD, the articles consid-eredwerethosewhosepatientshadtypicalsymptomssuch as: heartburn and regurgitation, especially at night, the presenceoflesionsinesophagusmucosaatendoscopy,and
Table3 Endolaryngealreflux findings score (RFS).24,25 A
RFS>11intheappropriateclinicalsituationisstrongly
sug-gestiveoflaryngopharyngealreflux.
Endolaryngealrefluxfindingsscore
Infraglotticedema 0absent
2present
Ventricularobliteration 2partial
4complete
Erythema/hyperemia 2onlyofarytenoids
4diffuse
Vocalfoldedema 1mild
2moderate
3severe
4polypoid
Diffuselaryngealedema 1mild
2moderate
3severe
4obstructive
Posteriorcommissurehypertrophy 1mild
2moderate
3severe
4obstructive
Granuloma/granulationtissue 0absent
2present
Thickendolaryngealmucus 0absent
2present
changesin 24-h ambulatory pH-metry.21 This latter test is
consideredthegoldstandardfordiagnosisofGERDbythese researchers.
Patientswere consideredashavingLPR iftheyshowed extraesophageal symptoms such asmucus, dysphonia and cough, preferablyatdaytime, andother subjective symp-toms such as globus sensation, excessive mucus and postnasaldrip,22aswellaspositivityinatleastoneofthese
scores: Reflux Symptom Index(RSI) (Table 2),23 or Reflux
FindingScore(RFS),24 translatedintoPortugueseasEscala deAchadosEndolaríngeosdeRefluxo(Table3).25
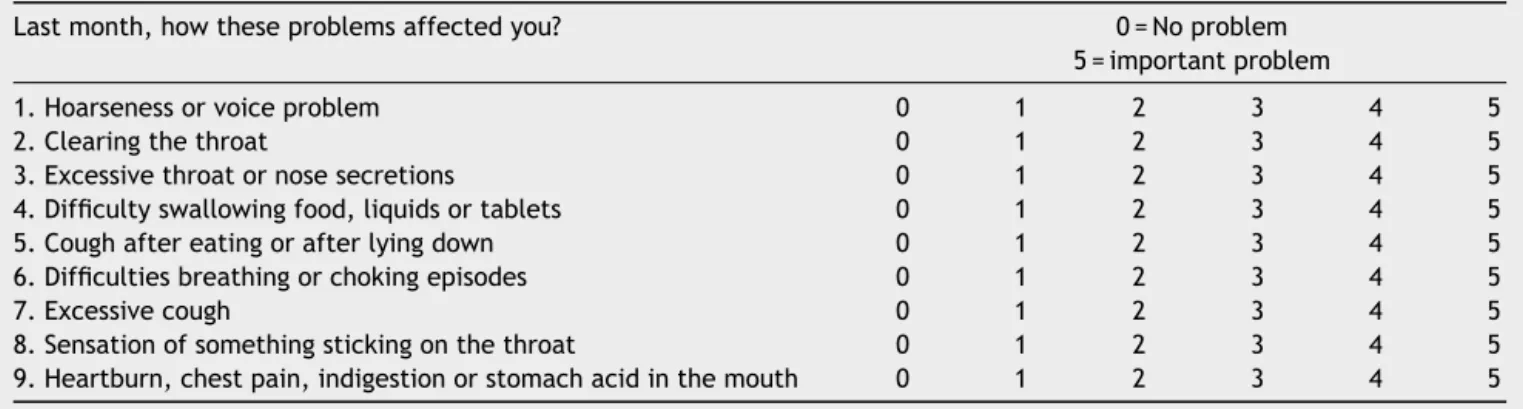
Table2 LaryngopharyngealRefluxSymptomIndex(RSI).23ARSI>13canbeindicativeoflaryngopharyngealreflux.
Lastmonth,howtheseproblemsaffectedyou? 0=Noproblem
5=importantproblem
1.Hoarsenessorvoiceproblem 0 1 2 3 4 5
2.Clearingthethroat 0 1 2 3 4 5
3.Excessivethroatornosesecretions 0 1 2 3 4 5
4.Difficultyswallowingfood,liquidsortablets 0 1 2 3 4 5
5.Coughaftereatingorafterlyingdown 0 1 2 3 4 5
6.Difficultiesbreathingorchokingepisodes 0 1 2 3 4 5
7.Excessivecough 0 1 2 3 4 5
8.Sensationofsomethingstickingonthethroat 0 1 2 3 4 5
Systematicreview:chronicrhinosinusitisandreflux 359
Thearticleswererankedaccordingtotheevidencelevel EBMaccordingtothefollowing:
1a.Systematicreviewarticlesofcontrolledand random-izedclinicaltrials
1b.Controlledandrandomizedclinicaltrials 2a.Systematicreviewofcohortstudies 2b.Cohortstudies
3a.Systematicreviewofcase---controls 3b.Case---controlstudies
4.Casereports 5.Specialistopinion
Results
We found 12 articles that specifically evaluatedthe rela-tionship between CRS and acid reflux in adults,with one of these being a randomizedcontrolled trial, eight being case---controlstudies andthreecohorts. Of thesearticles, eight specifically evaluated the relationship of CRS with reflux,andfourarticlesstudiedtheeffectoftreatmentwith PPIs(protonpumpinhibitor)onthesinonasalsymptomsand signsinpatientswithCRSandGERD.
StudiesevaluatingtherelationofCRSandreflux
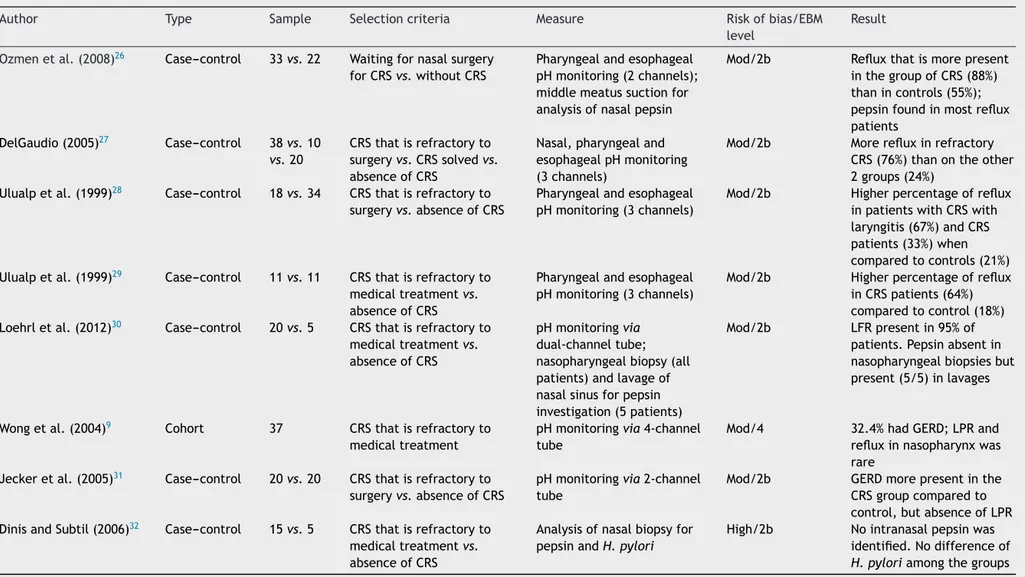
Eight articles were found comparing pHmetry monitoring valuesinpatientswithorwithoutCRS(Table4).
Ozmenetal.26 compared33patientswithCRS(whohad
receivedan indicationof ENS duetoimprovement failure after clinical treatment) to 20 patients, who would also undergo ENS for endonasal anatomical variations such as septaldeformityorconcha bullosa,but withoutCRS (con-firmedbyCT).pHmetrywithdual-channeltube(pharynxand esophagus) wasabnormalin 88%of patientswithCRS and 55%ofcontrols,beingstatisticallysignificant(p=0.01).This studyalsocollectedpepsininnasalsecretionduringENS;the specificactivityofpepsinwasdetectedin82%ofpatientsin thestudygroupandin50%ofthecontrolgroup(p=0.014). In allpatients withCRS, in which pepsinwas detectedin the nasal sample, LPR was documented by pHmetry, and onlythreepatients withLPRat pHmetryshowednegative pepsininvestigation.Theauthorssuggestedthatrefractory CRSmaybeassociatedwithLPRandthatpepsinwouldbea goodindicatorforthediagnosisofLPR.
DelGaudio27analyzed38patientswithsymptomaticCRS
andendoscopicsignsof nasalinflammationaftertheyhad been submitted to ENS, andcompared them to a control group (10 patients who underwent ENS due to CRS, who remainedasymptomatic aftersurgery,and20 withno his-tory of CRS or prior ENS). pHmetry was performed with three-channeltubeandtheauthornotedthattheLPRwas significantly more often present in the group with persis-tentCRSthaninthecontrolgroup,bothwhenthecriterion wasapH below4(39%vs. 7%)andapH below5(76% vs.
24%)(respectively,p=0.004andp=0.002).Thepresenceof refluxinthepersistentCRSgrouppatientswassignificantly highercomparedtothecontrolgroup,bothabovetheupper esophagealsphincterandinthedistalesophagus.
Ulualpetal.28evaluatedseveralgroupsofpatientswith
sinonasalcomplaintsthroughwithathree-channelpHmetry.
Theauthorsfoundahigherprevalenceofacidrefluxinthe hypopharynxandsignsof posteriorlaryngitisatendoscopy inpatientswithCRSandpersistentcomplaintsafterENS(4 of6patients,or67%)whencomparedtohealthycontrols(7 of34,or 21%) orCRS patientswithout posterior laryngitis (4of12or33%).Therewasnodifferenceintheparameters ofintensityofdistalorproximalesophagealrefluxbetween groups.He concludedthatthe LPRcan playan important roleinasubgroupofpatientswithCRS,andposterior laryn-gitismaybeacommonfinding.
Ulualpetal.29alsoobservedahigherprevalenceofLPR
inagroupof11patientswithCRS,whohadnotresponded toconventional treatment (7 of 11, or 64%) compared to 11healthycontrols(2of11,or18%),inastudyemploying pHmetrywiththree-channeltube.
Loehrlet al.30 evaluated20patients withCRS with no
improvementaftermedicalandsurgicaltreatmentthrough pHmetry with two tubes (in the esophagus and nasopha-rynx),comparedtopepsininnasalsecretions.Theauthors reported that 95% (19/20) of the patients had abnormal pHmetryin nasopharynx, and the DeMeester scorevalues fromthe esophagus were changed (<14.72) in 47% (9/19) ofpatients. Biopsy of the nasopharynx for pepsin investi-gationwasnegativein allpatients. In contrast,in fiveof thosepatients,pepsinwasassessedbytestingnasallavage samples,andwaspositiveinallcases.Infiveotherhealthy patients (with no history of paranasal sinuses diseases or GERDandnegativenasalendoscopy),pepsinwasnot iden-tifiedinnasallavage.
Wongetal.9 studied37patientswithCRSrefractoryto
clinicaltreatmentthroughpHmetrywithfour-channeltube thatincludedoneinthenasopharynx.Theauthorsobserved GERD in 32.4% of patients. Of the 809 episodes of reflux thatweredetected,usingasan acidcriterionapHbelow 4, only 2 (0.2%) reached the nasopharynx (in two differ-entpatients). The authors concludedthat reflux intothe nasopharynxisa rareeventandthattheremust beother differentmechanismsofdirectcontactoftheacidwiththe sinonasalmucosa for the persistenceof the inflammatory processinthesepatients.
Jeckeretal.31comparedagroupof20patientswith
per-sistentCRS even afterENS to 20 healthycontrol patients (medical students withno history of CRS, GERD or smok-ing)throughdual-channelpHmetry.Patientswithrefractory CRShadsignificantly morerefluxevents inthe distal sen-sor(DeMeesterindexinpatients of32.9±8.7 vs.controls of6.6±1.3)and thefractionwithapH below4 wasfour timesmorefrequentinpatientsthanincontrols.However, thisstatisticaldifferencebetweenthetwogroupswasnot evident withthe same parametersin the hypopharyngeal sensor,whichledtheauthorstoconcludethereisan asso-ciationbetweenCRSandGERD,butnotwiththeLPR.This wouldsupportavagalresponseasthemostlikelymechanism forthisinter-relationbetweenthetwodiseases.
DinisandSubtil32 analyzed15patientswithCRS
Sella
GC
et
al.
Table4 StudiesevaluatingCRS/refluxrelationship.
Author Type Sample Selectioncriteria Measure Riskofbias/EBM level
Result
Ozmenetal.(2008)26 Case---control 33vs.22 Waitingfornasalsurgery
forCRSvs.withoutCRS
Pharyngealandesophageal
pHmonitoring(2channels);
middlemeatussuctionfor
analysisofnasalpepsin
Mod/2b Refluxthatismorepresent
inthegroupofCRS(88%)
thanincontrols(55%);
pepsinfoundinmostreflux
patients
DelGaudio(2005)27 Case---control 38vs.10
vs.20
CRSthatisrefractoryto
surgeryvs.CRSsolvedvs.
absenceofCRS
Nasal,pharyngealand
esophagealpHmonitoring
(3channels)
Mod/2b Morerefluxinrefractory
CRS(76%)thanontheother
2groups(24%)
Ulualpetal.(1999)28 Case---control 18vs.34 CRSthatisrefractoryto
surgeryvs.absenceofCRS
Pharyngealandesophageal
pHmonitoring(3channels)
Mod/2b Higherpercentageofreflux
inpatientswithCRSwith
laryngitis(67%)andCRS
patients(33%)when
comparedtocontrols(21%)
Ulualpetal.(1999)29 Case---control 11vs.11 CRSthatisrefractoryto
medicaltreatmentvs.
absenceofCRS
Pharyngealandesophageal
pHmonitoring(3channels)
Mod/2b Higherpercentageofreflux
inCRSpatients(64%)
comparedtocontrol(18%)
Loehrletal.(2012)30 Case---control 20vs.5 CRSthatisrefractoryto
medicaltreatmentvs.
absenceofCRS
pHmonitoringvia
dual-channeltube;
nasopharyngealbiopsy(all
patients)andlavageof
nasalsinusforpepsin
investigation(5patients)
Mod/2b LFRpresentin95%of
patients.Pepsinabsentin
nasopharyngealbiopsiesbut
present(5/5)inlavages
Wongetal.(2004)9 Cohort 37 CRSthatisrefractoryto
medicaltreatment
pHmonitoringvia4-channel
tube
Mod/4 32.4%hadGERD;LPRand
refluxinnasopharynxwas
rare
Jeckeretal.(2005)31 Case---control 20vs.20 CRSthatisrefractoryto
surgeryvs.absenceofCRS
pHmonitoringvia2-channel
tube
Mod/2b GERDmorepresentinthe
CRSgroupcomparedto
control,butabsenceofLPR
DinisandSubtil(2006)32 Case---control 15vs.5 CRSthatisrefractoryto
medicaltreatmentvs.
absenceofCRS
Analysisofnasalbiopsyfor
pepsinandH.pylori
High/2b Nointranasalpepsinwas
identified.Nodifferenceof
H.pyloriamongthegroups
Systematicreview:chronicrhinosinusitisandreflux 361
which was similar to blood levels in all patients of both groups.
Thus, most controlled studies suggest that there is a higherprevalence of refluxina specificgroup ofpatients withrefractoryCRS.Alimitingfactorforthefinalconclusion isthatthestudieshavearelativelysmallnumberof partic-ipantsandare veryheterogeneousin methodology,which hindersthemeta-analysis.
Longitudinalstudiesaimedateffectoftreatment
withPPIs
Fourstudieswerefoundthatevaluatedtheeffectof treat-ment with PPIon the improvement of nasal symptomsin patientswithCRS(Table5).
Vaezi et al.33 conducted a controlled, randomized,
double-blind study toevaluate the effect of lansoprazole 30mg twice daily in 75 patients with chronic rhinitis, a complaint of postnasal drip, no CT abnormalities in the sinuses andanegativeRAST. Patientsunderwent pHmetry withatube intotheesophagus andimpedancemonitoring beforetreatment,andwerefollowedbyvalidated question-naires(SNOT-20,RSOM-31andQOLRAD)8and16weeksafter initiationoftreatment.Patientsreceivingtherapywith lan-soprazolewere3.12times(at8weeksoftreatment)and3.5 times(after16 weeksoftreatment) morelikelytonotice improvementoftheirpostnasaldripcomparedtocontrols. After16weeks,theaverageimprovementinthetreatment armwas50%comparedto5%intheplacebo group.There wasalsoasignificantimprovementintheSNOT-20and QOL-RADscoresinthetreatmentarm.Thepresenceofrefluxin pHmetrybeforetreatmentwasnotdecisivefortheanswer. In a prospective study, DiBaise et al.,34 compared 11
patients whohad failedclinical andsurgical treatmentof CRSto19patientswithGERDwhohadnoCRS(nonasal symp-toms and negativenasal endoscopy),evaluating sinonasal symptoms and reflux with a non-validated questionnaire (thatassessed14symptomsofGERDandrhinosinusitis,the frequencyofthesesymptoms,improvementwithtreatment, and overall satisfaction) and with dual-channel pHmetry. A similar percentage of abnormal pHmetry wasobserved betweenthetwogroups(82%intheCRSgroupand79%in theGERDgroup)atbaseline.Treatmentwith20mg omepra-zole twice daily for 12 weeks was instituted only in the CRSgroup,andthiswasreassessedonamonthlybasis.The authorsnotedmodestimprovementinsymptomsandoverall satisfactionwiththetreatmentamongthesepatients.
Pincusetal.35performedpHmetryin30patientswithCRS
withnoimprovementwithclinicalandsurgicaltreatment. Ofthese,25hadanassociateddiagnosisofGERD.Forthese patients,atreatmentwithPPIswasstarted,withan inter-viewbeingperformedbytelephoneonemonthlater.Ofthe 15 patientswhowere re-evaluated,14 reported improve-ment of nasal symptoms, and seven fully improved their complaints.
Durmusetal.36 studied50patientswithGERDandLPR,
basedonclinicalandendoscopicdiagnosis, andcompared themto30healthypatients.Pretreatmenttestsofsucrose weresimilarbetweenthetwogroups,whiletheRSIandRFS questionnairesweresignificantlyworseinthegroupofLPR.
Allpatientsthenunderwentatreatmentwithlansoprazole T
30mgtwicedailyfor12weeks.Therewasnostatistical dif-ferencebetweentheresultsofsaccharintestinthecontrol andstudy groups before treatment. After treatment, the differencesbetweenRSI andRFSremained similarto pre-treatment levels,asdid the saccharintest results. These authorsconcludedthatbothGERDandtheLPRdonotseem toaffectthenasalmucociliarytransport.
Thus, current studies available in the literature are conflicting as to the effect of PPI therapy in symptom improvementinpatientswithCRS.Inaddition,CRSorreflux diagnoses were not confirmed by complementary tests, whichmakestherealinterpretationoftheresultsdifficult.
Discussion
LPR was present with significantly greater difference in patientswithCRScomparedtogroupsof patientswithout CRSin4studies.26---29Althoughtheywerecontrolledstudies,
none of the groups were matched for age, weight, ana-tomicalabnormalitiespredisposingtoreflux(suchashiatal hernia),previous treatment of GERD,or findings ofupper digestiveendoscopy.Inaddition,thereisgreatvariabilityin theuseofpHmetryfordiagnosticconfirmation,withrespect tothenumberoftubes,theirpositioning,andcriteriaused fordiagnosisconfirmation.Thishugevariabilitymakes defin-itiveconclusiononthesubjectevenmoredifficult.
Twostudiesdidnotshowarelationshipbetweenhighacid reflux(LPRor nasopharynx)andCRS.9,31 Inonesuchstudy
(Jeckeretal.),31 despitesimilarLPRfindingsbetweenthe
controlgroupandstudygroup,thegroupwithpersistentCRS afterENShadahigherprevalenceofGERDthanthecontrol group.Theseauthorsevensuggestedthatthereshouldbe anassociationbetweenthetwodiseases,probablymediated byvagalreflex.
Somestudiesusedananalysisofpepsininthenasal cav-ityfor diagnosis of reflux.While Loehrl etal.30 and Dinis
and Subtil32 analyzed a nasal tissue biopsy and did not
observethepresenceofpepsinintheirresults,thepepsin in nasal lavage was present in large amounts in patients withCRS in two studies.26,30 The comparisonof pepsin in
lavagewiththecontrolgroup,however,wasnotconsistent: whileLoehrletal.30observedanamountthatissignificantly
greaterintheCSR groupcomparedtothecontrol,Ozmen etal.26 reportedthat the controlgroup alsoshowed high
amountofpepsin,andthattherewasnosignificant differ-encebetweenthegroupsanalyzed.Apparentlytheresultof thistestdependsgreatlyonthecollectiontechnique,with sensitivity being higherwhen pepsin is collected in nasal lavagethan when it is evaluatedin a nasal biopsy. More-over, thesmallnumber ofsubjects in each ofthe studies makesthefinalanalysisonthetopicimpossible.Finally,we found nodata in the literature tovalidate the collection ofpepsininthenasalcavityasatesttobeusedforreflux investigation.
In general,thestudies currently availablesuggest that thereisarelationshipbetweenrefluxandaspecificsubtype ofCRS,refractorytoclinicalandsurgicaltreatment. How-ever,studiesarefew,andthesmallnumberofpatientsand thedifferentmethodologies,employedmakeitdifficultto conductameta-analysis.Allthesehinderthemostreliable interpretation of the data. Thus,more controlled studies
withlargernumbers of patientsand probablymulticenter participationwillbeneededtoconfirmthishypothesis.
When randomized controlled trials were conducted to assesstheimprovementofsymptomsofCRSaftertreatment ofreflux,Vaezietal.33observedimprovementofpostnasal
dripintheevaluatedpatients,withnoCRSorallergies. Pin-cusetal.35reportedasignificantimprovementofsymptoms
ofCRSaftertreatment,whileDiBaiseetal.34reportedthat
treatmentwithPPIsshowedaslightimpactonthe improve-mentofsymptoms.Durmusetal.36reportedthattherewas
no difference in pre- and post-treatment saccharine test withPPIsforthreeweeks,althoughtheynotedimprovement inrefluxsymptoms.Thus,currentcontrolled,randomized, double-blind studies available in the literature, describe extremelydifferentmethodologies.Evenworse, manyfail toconfirmthediagnosisofCRSorGERD/LPRandarebased only ontheimprovement ofnasalsymptoms.Thus, multi-centerstudies,withamoresignificantnumberofpatients, thathavespecifiedcriteriafordiagnosis,andstandardized methodology, should help considerablyin elucidating this question.
Conclusions
Accordingtothestudiesfoundintheliterature,itwas con-cludedthatthereappearstoberelativeprevalenceofreflux inpatientswithdifficulttocontrolCRS.However,controlled studies with a significant number of patients are lacking toconfirm thishypothesis. Similarly,therearefewstudies thatspecificallyassesstheimpactoftreatmentofrefluxin symptomimprovementinpatientswithCRS.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.BenningerMS,FergusonBJ,HadleyJA,HamilosDL,JacobsM, Kennedy DW, et al. Adultchronic rhinosinusitis: definitions, diagnosis,epidemiology,andpathophysiology.OtolaryngolHead NeckSurg.2003;129:S1---32.
2.FokkensWJ,LundVJ,MullolJ,BachertC,AlobidI,BaroodyF, etal.Europeanpositionpaperonrhinosinusitisandnasalpolyps 2012.RhinolSuppl.2012;23:1---298.
3.OrlandiRR,KingdomTT,HwangPH,SmithTL,AltJA,Baroody FM,etal.Internationalconsensusstatementonallergyand rhi-nology:rhinosinusitis.IntForumAllergyRhinol.2016;6:S22---09. 4.KennedyDW.Prognosticfactors,outcomesandstagingin
eth-moidsinussurgery.Laryngoscope.1992;102:1---18.
5.ChambersDW,DavisWE, CookPR, NishiokaGJ,RudmanDT. Long-term outcome analysis of functional endoscopic sinus surgery: correlation of symptoms with endoscopic examina-tionfindingsandpotentialprognosticvariables.Laryngoscope. 1997;107:504---10.
6.BarberoGJ.Gastroesophagealrefluxandupperairwaydisease. OtolaryngolClinNAm.1996;29:27---38.
Systematicreview:chronicrhinosinusitisandreflux 363
8.ContencinP,NarcyP.NasopharyngealpHmonitoringininfants andchildrenwithchronicrhinopharyngitis.IntJPediatr Otorhi-nolaryngol.1991;22:249---56.
9.Wong IW, Omari TI, Myers JC, Rees G, Nair SB, Jamieson GG, et al. Nasopharyngeal pH monitoring in chronic sinus-itispatientsusinga novelfourchannelprobe.Laryngoscope. 2004;114:1582---5.
10.LoehrlTA, SmithTL, DarlingRJ, TorricoL,PrietoTE,Shaker R, et al. Autonomic dysfunction, vasomotor rhinitis, and extraesophageal manifestations of gastroesophageal reflux. OtolaryngolHeadNeckSurg.2002;126:382---7.
11.DelehayeE,Dore MP, BozzoC,Mameli L, DelitalaG, Meloni F.Correlation betweennasal mucociliaryclearancetimeand gastroesophagealrefluxdisease:ourexperienceon50patients. AurisNasusLarynx.2009;36:157---61.
12.HolmaB,LindegrenM,AndersenJM.pHeffectsonciliomotility andmorphology ofrespiratorymucosa. Arch EnvironHealth. 1977;32:216---26.
13.LodiU,HardingSM,CoghlanHC,GuzzoMR,WalkerLH. Auto-nomicregulationinasthmatics withgastroesophagealreflux. Chest.1997;111:65---70.
14.HardingSM,RichterJE.Theroleofgastroesophagealrefluxin chroniccoughandasthma.Chest.1997;111:1389---402. 15.WongIWY,ReesG,GreiffL,MyersJC,JamiesonGG,Wormald
P-J.Gastroesophagealrefluxdisease andchronic sinusitis:in search of an esophageal-nasal reflex. Am J Rhinol Allergy. 2010;24:255---9.
16.KocC,ArikanOK,AtasoyP,AksoyA.Prevalenceof Helicobac-terpyloriinpatientswithnasalpolyps:apreliminaryreport. Laryngoscope.2004;114:1941---4.
17.MorinakaS,IchimiyaM,NakamuraH.DetectionofHelicobacter pyloriinnasalandmaxillarysinusspecimensfrompatientswith chronicsinusitis.Laryngoscope.2003;113:1557---63.
18.OzdekA, CirakMY, Samim E,Bayiz U,Safak MA,Turet S. A possibleroleofHelicobacterpyloriinchronicrhinosinusitis:a preliminaryreport.Laryngoscope.2003;113:679---82.
19.FlookEP,KumarBN.Isthereevidencetolinkacidrefluxwith chronicsinusitisoranynasalsymptoms?Areviewofthe evi-dence.Rhinology.2011;49:11---6.
20.LupaM,DelGaudio JM.Evidence-based practice. Otolaryngol ClinNAm.2012;45:983---92.
21.RichterJE.Typicalandatypicalpresentationsof gastroesopha-gealrefluxdisease.Theroleofesophagealtestingindiagnosis andmanagement.GastroenterolClinNAm.1996;25:75---102. 22.KoufmanJ.Laryngopharyngealreflux:positionstatementofthe
committeeonspeech,voice,andswallowingdisordersofthe
AmericanAcademyofOtolaryngology-HeadandNeckSurgery. OtolaryngolHeadNeckSurg.2002;127:32---5.
23.BelafskyPC,PostmaGN,KoufmanJA.Validityandreliabilityof therefluxsymptomindex(RSI).JVoice.2002;16:274---7. 24.Belafsky PC, Postma GN, Koufman JA. The validity and
reliability of the reflux finding score (RFS). Laryngoscope. 2001;111:1313---7.
25.AlmeidaAGdoP,SalitureTBS,daSilvaAS,EckleyCA.Translation andculturaladaptationoftheRefluxFindingScoreintoBrazilian Portuguese.BrazJOtorhinolaryngol.2013;79:47---53.
26.OzmenS,YücelOT,SiniciI,OzmenOA,SüslüAE,O˘gretmeno˘glu O,etal.NasalpepsinassayandpHmonitoringinchronic rhi-nosinusitis.Laryngoscope.2008;118:890---4.
27.DelGaudioJM.Directnasopharyngealrefluxofgastricacidisa contributingfactorinrefractorychronicrhinosinusitis. Laryn-goscope.2005;115:946---57.
28.Ulualp SO, Toohill RJ, Shaker R. Pharyngeal acid reflux in patients with single and multiple otolaryngologic disorders. OtolaryngolNeckSurg.1999;121:725---30.
29.UlualpSO,ToohillRJ,HoffmannR,ShakerR.Possible relation-shipofgastroesophagopharyngealacidrefluxwithpathogenesis ofchronicsinusitis.AmJRhinol.1999;13:197---202.
30.Loehrl TA, Samuels TL, Poetker DM, Toohill RJ, Blumin JH, Johnston N. The role of extraesophageal reflux in medi-cally and surgically refractory rhinosinusitis. Laryngoscope. 2012;122:1425---30.
31.Jecker P, Orloff LA, Wohlfeil M, Mann WJ. Gastroesopha-geal refluxdisease(GERD),extraesophagealreflux(EER)and recurrent chronic rhinosinusitis. Eur Arch Otorhinolaryngol. 2006;263:664---7.
32.Dinis P, Subtil J. Helicobacter pylori and laryngopharyngeal reflux inchronic rhinosinusitis. Otolaryngol Head Neck Surg. 2006;134:67---72.
33.Vaezi MF, HagamanDD, Slaughter JC, TannerSB, Duncavage JA,AlloccoCT,etal.Protonpumpinhibitortherapyimproves symptomsinpostnasal drainage.Gastroenterology. 2010;139, 1887---1893.e1.
34.DiBaiseJK,OlusolaBF,HuerterJV,QuigleyEMM.RoleofGERDin chronicresistantsinusitis:aprospective,openlabel,pilottrial. AmJGastroenterol.2002;97:843---50.
35.PincusRL,KimHH,SilversS,GoldS.Astudyofthelinkbetween gastricrefluxandchronicsinusitisinadults.EarNoseThroatJ. 2006;85:174---8.