r e v b r a s r e u m a t o l . 2016;56(2):181–184
w w w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Case
report
Acute
acalculous
cholecystitis
in
systemic
lupus
erythematosus:
a
rare
initial
manifestation
夽
Valdano
Manuel
a,∗,
Gertrudes
Maria
Pedro
b,
Lemuel
Bornelli
Cordeiro
a,
Sandra
Maria
da
Rocha
Neto
de
Miranda
aaEducationOffice,Post-GraduationandResearch,ClínicaGirassol,Luanda,Angola
bDepartmentofInternalMedicine,ClínicaGirassol,Luanda,Angola
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received20December2013 Accepted26March2014 Availableonline25October2014
Keywords:
Systemiclupuserythematosus Acuteacalculouscholecystitis Abdominalcomputedtomography Initialmanifestation
a
b
s
t
r
a
c
t
Acuteacalculouscholecystitisisaveryraregastrointestinalmanifestationinsystemiclupus erythematosusandbecomesrarerasaninitialmanifestation.Thereareonlytwocases reported.Theauthorsreporta20-year-oldblackwomanthatpresentedacuteacalculous cholecystitisrevealedbyabdominalcomputedtomography.Duringhospitalization,shewas diagnosedsystemiclupuserythematosus.Conservativetreatmentwithantibioticswas per-formedwithcompleteremissionofthesymptoms.Corticosteroidwasstartedinambulatory. Cholecystectomyhasbeenthetreatmentofchoiceinacuteacalculouscholecystitisasa complicationofsystemiclupuserythematosus.Thepatientrespondedwelltoconservative treatment,andsurgerywasnotrequired.Thiscaseisuniqueinthewaythatcorticosteroid wasstartedinambulatorycare.Weshouldnotforgetthattheacuteacalculouscholecystitis canbetheinitialpresentationofsystemiclupuserythematosusalthoughitsoccurrenceis veryrare.Conservativetreatmentshouldbeconsidered.Abdominalcomputedtomography wasadeterminantexamforbetterassessmentofacuteacalculouscholecystitis.
©2013ElsevierEditoraLtda.Allrightsreserved.
Colecistite
aguda
acalculosa
no
lúpus
eritematoso
sistêmico:
uma
manifestac¸ão
inicial
rara
Palavras-chave:
Lúpuseritematososistêmico Colecistiteagudaacalculosa Tomografiacomputadorizadado abdome
Manifestac¸ãoinicial
r
e
s
u
m
o
Acolecistiteagudaacalculosaéumamanifestac¸ãogastrointestinalraranolúpus eritem-atoso sistêmicoe ainda mais rara como manifestac¸ão inicial. Foramdescritos apenas doiscasosatéomomento.Osautoresrelatamocasodeumamulhernegrade20anos, com quadrode colecistiteaguda acalculosa reveladapelatomografiacomputadorizada do abdome. Durantea hospitalizac¸ão, a paciente foi diagnosticada com lúpus eritem-atososistêmico.Houveremissãocompletadossintomasapóstratamentoconservadorcom
夽
ThestudywasoriginatedatClínicaGirassol,Luanda,Angola.
∗ Correspondingauthor.
E-mail:valdanympub@gmail.com(V.Manuel).
http://dx.doi.org/10.1016/j.rbre.2014.03.027
182
rev bras reumatol.2016;56(2):181–184antibióticos.Iniciou-setratamentocomcorticosteroidesnoambulatório.Emboraa cole-cistectomiasejaotratamentodeescolhaemcasosdecolecistiteagudaacalculosacomo complicac¸ãodolúpuseritematososistêmico,apacienterespondeubemaotratamento con-servador;logo,acirurgianãofoinecessária.Estecasoéúnicoemrazãodomodocomo ocorticosteroidefoiiniciadonoatendimentoambulatorial.Éimportantelembrarquea colecistiteagudaacalculosapodeseramanifestac¸ãoinicialdolúpuseritematososistêmico, emborasuaocorrênciasejarara.Deve-seconsiderararealizac¸ãodetratamento conser-vador.Atomografiacomputadorizadadoabdomefoideterminante paraquefossefeita umamelhoravaliac¸ãodacolecistiteagudaacalculosa.
©2013ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Systemiclupuserythematosus(SLE)isanautoimmune dis-ease found predominantly in female gender1–3 in which
almostallorgans canbeinvolvedwithwide rangeof clini-calmanifestations.Gastrointestinalmanifestationisusually mild, but gallbladder involvementis an uncommon event. Acuteacalculouscholecystitis(AAC)isveryrareasa compli-cationofSLEandbecomesrarerasaninitialpresentation.1–9
SeveralcasesofAACasacomplicationofSLEwerereported; nevertheless only two cases have been reported as initial manifestation.5,9
Case
report
A 20-year-old black woman with history ofmigratory pol-yarthralgia was admitted with fever, nausea and vomit, acute abdominal pain in the right upper quadrant and referred loss of appetite. Physical examination evidenced febrile (38.6◦C), tachycardia (102 beats per minute),
dehy-dratedandsubictericmucousmembranes.Abdominalpain intherightupperquadrantwithhepatomegalyof8cmbelow thecostalmarginwasfound.Cardiacauscultation,revealed agrade-II/VIprotosystolicmurmurinall cardiacfocus. Ini-tiallaboratorydatashowedhemoglobin7.6g/dL,leucocytes 3300/L, albumin 2.2g/dL, alanine aminotransferase 86U/L, aspartateaminotransferase127U/L,totalbilirubin1.8mg/dL; lactatedehydrogenase1719U/Landtestforplasmodium neg-ative. Abdominal ultrasound confirmed hepatomegaly and revealedsplenomegaly,gallbladderslightlydistendedwithout wallthickening.During hospitalization,the patientevolved withretrosternalpain,orthopnea,surfeitsensation,increased pain in the right upper quadrant, nausea, vomiting, diar-rheaand fever. Pulmonary auscultation revealed abolished in both bases. Cardiac auscultation was the same. The abdomenwas distended withhepatomegaly of8cm below the right costal margin; liquid wave signal and murphy
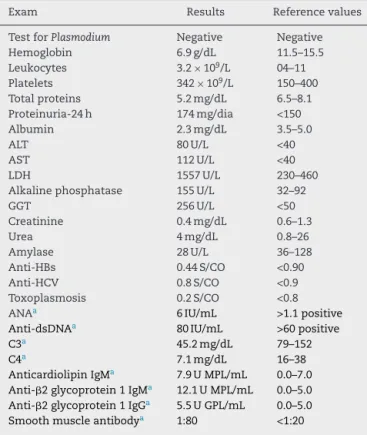
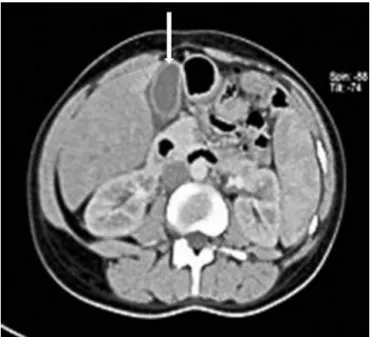
werepresent.Lowerlimbspresentedmalleolaredema.The main laboratory findings are shown (Table 1). Teleradiog-raphy of chest showed bilateral pleural effusion of small volume. Echocardiography revealed pericardial effusion of 1.5cm.Abdominalcomputedtomographyrevealedincreased wall thickness without any evidence of stone and edema aroundthegallbladder(Fig.1),andconfirmedsplenomegaly,
hepatomegaly andascites. Basedonthephysical examina-tion,laboratoryandimagefindings,adiagnosisofinaugural systemiclupuserythematosustriggeredbyacuteacalculous cholecystitis was established. The patient initiated treat-ment with ceftriaxone and metronidazole, furosemide and albumin. Within10 days, therewas complete remissionof symptoms. The corticosteroid was initiated in ambulatory of rheumatology.Surgical interventionwas not performed. Accordingtotherheumatologists’feedback,shelookedwell and did not have any symptoms until four months after discharge.
Table1–Laboratoryfindingsduringadmissioncourse.
Exam Results Referencevalues
TestforPlasmodium Negative Negative Hemoglobin 6.9g/dL 11.5–15.5 Leukocytes 3.2×109/L 04–11 Platelets 342×109/L 150–400 Totalproteins 5.2mg/dL 6.5–8.1 Proteinuria-24h 174mg/dia <150 Albumin 2.3mg/dL 3.5–5.0
ALT 80U/L <40
AST 112U/L <40
LDH 1557U/L 230–460
Alkalinephosphatase 155U/L 32–92
GGT 256U/L <50
Creatinine 0.4mg/dL 0.6–1.3
Urea 4mg/dL 0.8–26
Amylase 28U/L 36–128
Anti-HBs 0.44S/CO <0.90 Anti-HCV 0.8S/CO <0.9 Toxoplasmosis 0.2S/CO <0.8
ANAa 6IU/mL >1.1positive
Anti-dsDNAa 80IU/mL >60positive
C3a 45.2mg/dL 79–152
C4a 7.1mg/dL 16–38
AnticardiolipinIgMa 7.9UMPL/mL 0.0–7.0
Anti-2glycoprotein1IgMa 12.1UMPL/mL 0.0–5.0
Anti-2glycoprotein1IgGa 5.5UGPL/mL 0.0–5.0
Smoothmuscleantibodya 1:80 <1:20
ALT,alanineaminotransferase;AST,aspartateaminotransferase; LDH, lactatedehydrogenase;GGT, gamma-glutamyltransferase; ANA,antinuclearantibody.
rev bras reumatol.2016;56(2):181–184
183
Fig.1–AbdominalCTshowgallbladderwallthickness withoutstonewithedemaaround(arrow).
Discussion
Abdominal pain is always a challenge for diagnosis and treatment in patients with SLE; it may be caused by the disease itself, other comorbidities or drug effects.1–3 The
involvement of gastrointestinal and hepatobiliary systems sparinggallbladderhavebeenreported.1–9Thedepositionof
immunecomplexesinbloodvesselwallsresultsinacute vas-culitis; these events result in ischemia and fibrosis in the targetorgan.4–9Thromboemboliceventsaremostfrequently
observedin patients withSLE; this risk isincreasedwhen anticardiolipinantibodyispositive,10asinthecaseof
anticar-diolipinIgM,anti-2glycoprotein1positive,althoughitwas alowtiter.Thepatientdoesnothavecriteriafordiagnosis ofantiphospholipidsyndrome.10Histologically,
antiphospho-lipidsyndrome ischaracterizedbymultiplethrombi inthe vesselsofthegallbladderwithoutevidenceofvasculite.5The
gallbladder is rarely involved in patients with SLE.1–9
Sev-eral casesofAAC as a complicationof SLEwere reported, butonlytwocasesofAACasaninitialmanifestationofSLE were described,onein apediatric patientand other in an adult.5,9Themostwidelyusedclassificationcriteriafor
diag-nosis of SLE are those proposed by the American College ofRheumatologyand SystemicLupusInternational Collab-oratingClinicsthatrequirefour ormoreitemstodiagnose SLE(cutaneous manifestation,joints, serositis, renal disor-der,hematologicdisorder,immunologicabnormality).11,12In
thiscase,thepatientpresentedwithpainintheperipheral joints,pleuralandpericardialeffusion,proteinuria,hemolytic anemia,leukopenia,positiveANA,positiveanti-dsDNA, posi-tiveanti-2glycoprotein1,positiveSmandlowcomplement. Whenthereisasuspicionofinvolvementofthegallbladder asthe cause ofabdominal paininthese patients, abdomi-nalultrasoundandcomputedtomography(CT)areindicated forbetterassessmentofAAC.13Inthiscase,theabdominal
ultrasound performed at admission was inconclusive. The abdominalCTperformedwasessentialforrevealingthe gall-bladder wall thickness withedema aroundthe gallbladder without the presenceofstones,important findingsfor the diagnosisofAACcasesthathavenotbeendisclosedbythe ultrasoundmadeintheadmission.Nootherriskfactorsfor cholecystitiswerefound.Inthiscase,AACmaybedueto mul-tiple thrombi in thegallbladder vessels.8 Thetreatmentof
AAChasbeencontroversial.Therearefourcasesreportedof patientswithAACinSLE,whichdidnothavecholecystectomy, and responded well to medicaltreatment with high doses of corticosteroid.4,5,7,9 In this case, due to major
improve-ment ofthe symptoms withantibiotics, corticosteroidwas started inoutpatientfollow-up.Surgerywasnotperformed whichjustifynohistologicaldescription.Highdosesof cor-ticosteroids are usuallysuggestedas first-line treatment if patientshaveagoodgeneralconditionwithoutother chole-cystitisriskfactors,noserioushealthcomplicationsandno infections.7
Conclusions
Despitetherarity,weshouldnotforgetthatacuteacalculous cholecystitis,besidesbeingacomplication,canbetheinitial manifestationofSLE.Conservativetreatmentshouldbe con-sidered.Inthiscase,corticosteroidwasstartedafterpatient discharge;itmadethiscaseunique.Computedtomographyis agoodexamforbetterassessmentofAAC.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgments
WewouldliketoacknowledgeDr.HumbertoMoraisandDra BrunaDavidforsuggestions.
r
e
f
e
r
e
n
c
e
s
1.TuY-T,YehK-W,ChenL-C,YaoT-C,OuL-S,LeeW-I,etal. Differencesindiseasefeaturesbetweenchildhood–onsetand adult–onsetinsystemiclupuserythematosuspatients presentingwithAcuteAbdominalPain.SeminArthritis Rheum.2011;40:447–54.
2.RicherO,UlinskiT,LemelleI,RanchinB,LoiratC,PietteJC, etal.Abdominalmanifestationsinchildhood–onsetsystemic lupuserythematosus.AnnRheumDis.2007;66:
174–8.
3.EbertEC,HagspielKD.Gastrointestinalandhepatic manifestationsofsystemiclupuserythematosus.JClin Gastroenterol.2011;45:436–41.
4.KamimmuraT,MimoriA,TakedaA,MasuyamaJ,YoshioT, OkazakiH,etal.Acuteacalculuoscholecystitisinsystemic lupuserythematosus.Lupus.1998;7:361–3.
5.Mendonc¸aJA,Marques-NetoJ,PrandoP,AppenzellerS.Acute acalculuoscholecystitisinjuvenilsystemiclupus
184
rev bras reumatol.2016;56(2):181–1846. BasiratniaM,VaseiM,BahadorA,EbrahimE,DarakhshanA. Acuteacalculouscholecystitisinachildwithsystemiclupus erythematosus.PediatrNephrol.2006;21:873–6.
7. ShinSJ,NaKS,JungSS,BaeSC,YooDH,KimSY,etal.Acute acalculouscholecystitisassociatedwithsystemiclupus erythematosuswithSjogren’ssyndrome.KoreanJIntern Med.2002;17:61–4.
8. SwanepoelCR,FloydA,AllisonH,LearmonthGM,CassidyMJ, PascoeMD.Acuteacalculouscholecystitiscomplicating systemiclupuserythematosus:casereportandreview.Br MedJClinResEd.1983;286:251–2.
9. GhorbelIB,SouabniL,LamloumM,KhanfirM,BrahamA, MiledM,etal.Unecholécystiteaiguëalithiasiquerévélantun lupusérythémateuxsystémique.GastroenterolClinBiol. 2009;33:1175–8.
10.WilsonAW,GharaviAE,KoikeT,LockshinMD,BranchDW, PietteJC,etal.Internationalconsensusstatementon
preliminaryclassificationcriteriafordefinite
antiphospholipidsyndrome.Reportonaninternational workshop.ArthritisRheum.1999;42:
1309–11.
11.HochbergMC.UpdatingtheAmericanCollegeof Rheumatologyrevisedcriteriafortheclassificationof systemicLupuserythematosus.ArthritisRheum. 1997;40:1725.
12.PetriM,OrbaiAM,AlarconGS,GordonC,MerrillJT,FortinPR, etal.Derivationandvalidationofthesystemiclupus internationalcollaboratingclinicsclassificationcriteriafor systemiclupuserythematosus.ArthritisRheum.
2012;64:2677e86.