PROGRESSIVE SUPRANUCLEAR PALSY IN A
SAM PLE OF BRAZILIAN POPULATION
Clinical feat ures of 16 pat ient s
Paulo Eduardo Mest rinelli Carrilho
1, Egbert o Reis Barbosa
2ABSTRACT - Progressive supranuclear palsy (PSP) is an uncommon disorder charact erized by marked post ural inst abilit y, vert ical gaze abnormalit ies and axial rigidit y. The purpose of t his st udy is t o report t he clinical feat ures of 16 consecut ive subject s seen over a 10-year period at a M ovement Disorders Clinic. These subject s fulfilled crit eria for probable PSP namely t hose of t he Nat ional Inst it ut e of Neurologic Disorders and St roke (NINDS) and t he Societ y for PSP (SPSP). This pat ient -group represent ed 2.1% of all degenerat ive parkinsonians observed and t he mean age of onset of t he disease w as 64.7 years (sd = ± 7.2). Post ural inst abilit y w it h falls w as t he most frequent init ial feat ure present ed in PSP pat ient s (62.5%). The hallmark of t he disease, t he supranuclear vert ical gaze palsy, appeared af t er 2.3 years of disease onset , and only 12.5% had such manifest at ion at t he first evaluat ion. Transient t remor w as observed w it h a relat ively high frequency in t his group (44%), but only 19% had rest t remor. Chronic dacryocyst it is, probably relat ed t o a paucit y of blinking, w as observed in t w o pat ient s as an inaugural manifest at ion. In t he first evaluat ion, only 19% of t he 16 pat ient s w ere diagnosed as probable PSP. The mean int erval prior t o t he final diagnosis w as 2.4 years.
KEY WORDS: progressive supranuclear palsy, parkinsonism, movement disorders, chronic dacryocyst it is.
Paralisia supranuclear progressiva em uma amostra da população brasileira: aspectos clínicos de 16 pacientes
RESUM O - A paralisia supranuclear progressiva (PSP) é entidade incomum, caracterizada por severa instabilidade post ural, anormalidades do olhar conjugado vert ical e rigidez axial. O propósit o desse est udo é apresent ar os aspect os clínicos de 16 pacient es consecut ivament e at endidos em período de 10 anos em uma unidade especializada no atendimento de movimentos anormais. Tais pacientes preencheram os critérios para diagnóstico de PSP provável, de acordo com aqueles recomendados pelo NINDS (EUA) e pela SPSP. O grupo represent ou 2,1% de t odos os casos de parkinsonismo degenerat ivo at endidos naquele período. O início das primeiras manifest ações se deu, em média, aos 64,7 anos (± 7,2). Inst abilidade post ural inaugurou o quadro na maioria dos casos (62,5%) e a manifest ação mais caract eríst ica da doença, a paralisia supranuclear vert ical do olhar conjugado, est eve present e inicialment e em apenas 12,5%. Ela só foi observada após 2,3 anos, em media, de evolução da moléstia. Tremor transitório foi observado com frequencia relativamente alta (44%), porém apenas 19% apresent avam t remor de repouso. Sint omas iniciais sugest ivos de dacriocist it e crônica, provavelment e relacionada à pobreza de piscament o, foram observados em 2 casos. Na primeira avaliação, soment e 19% dos pacientes foram diagnosticados como PSP provável e o intervalo médio para esse diagnóstico final foi 2,4 anos.
PALAVRAS-CHAVES: paralisia supranuclear progressiva, parkinsonismo, desordens do movimento, dacriocistite crônica.
1Disciplina de Neurologia – Curso de M edicina da Universidade Est adual do Oest e do Paraná (UNIOESTE), Cascavel PR, Brasil; 2Grupo de Est udos de M oviment os Anormais (GEM A) da Divião de Neurologia do Hospit al das Clínicas da Faculdade de M edicina da Universidade de São Paulo (USP), São Paulo SP, Brasil. Est udo realizado com bolsa de mest rado fornecida pela Fundação de Amparo à Pesquisa do Est ado de São Paulo (FAPESP).
Received 4 M arch 2002, received in final form 29 M ay 2002. Accept ed 11 June 2002.
Dr. Paulo Carrilho - Rua Sant a Cat arina 925 – 85506-040 Cascavel PR – Brasil. E-mail: carrilho@cert t o.com.br
Thirt yeight years ago, John St eele, Jerzy Olszew -ski and J. Clifford Richardson described nine pat i-ent s1,2 w it h a different form of clinical parkinsonism.
The brains of four of t hese pat ient s w ere submit t ed t o a post-mortem st udy t hat show ed a pat t ern of
pat hological abnorm alit ies, com plet ely dif f erent from t hat of classical Parkinson’s disease. The clinical
hallmarks of progressive supranuclear palsy (PSP) are: axial rigidity w ith postural instability frequently asso-ciated w ith falls and supranuclear vertical gaze palsy 1-12. Despit e t he disease being seem ingly easy t o
diagnose, this can sometimes prove difficult. Litvan et al.9 found an unexpect edly high false posit ive PSP
presented blindly to six neurologists, whereas Rajput et al.13 had no misdiagnosis of PSP in their prospective study.
Wit h t he aim of increasing t he sensit ivit y and spe-cificit y of PSP clinical diagnosis, w it h no biological m arker having been est ablished, an int ernat ional w orkshop w as jointly sponsored by the National Insti-tute of Neurologic Disorders and Stroke of the United St at es (NINDS) and t he Societ y for PSP (SPSP). Aft er t his meet ing, t he result ing clinical consensual cri-t eria w ere draw n up and divided incri-t o cri-t hree groups: mandatory inclusion criteria, mandatory exclusion cri-teria and auxiliary cricri-teria14, w ich are listed in Table 1.
According t o Lit van15, t he clinical crit eria for
pro-bable PSP have a high predict ive value, high speci-ficit y but low er sensit ivit y. They are ideal for use in
scient ific st udies, mainly in genet ics, drug t rials, and epidemiological analyt ical st udies on PSP. The pos-sible PSP crit eria have a low er specificit y but maint ain high sensit ivit y, making early diagnosis easier. They are more useful for current clinical pract ice and des-cript ive epidemiological st udies.
In Brazil, t here had never been a st udy of a large number of PSP pat ient s. Therefore, a survey based on probable PSP crit eria w as performed at t he M o-vement Disorder Unit of t he Depart ment of Neuro-logy of São Paulo Universit y M edical School from 1987 t o 1997. The object ive of t his st udy is t o des-cribe t he main clinical manifest at ions, at ypical fea-t ures and possible differenfea-t pafea-t fea-t erns of PSP in fea-t his group of Brazilian pat ient s.
Table 1. Ninds/Spsp crit eria. Mandat ory inclusion crit eria
Possible PSP
1. Gradually progressive disease onset w it h init ial manifest at ion aft er t he age of fort y.
2. Supranuclear vert ical gaze abnormalit ies w it h pursuit movement s dow nw ards or upw ards w it h a rest rict ion of less t han 50% compared t o normal, or t he t w o follow ing crit eria: slow ed vert ical saccades and post ural inst abilit y w it h falls in t he first year of t he disease.
3. There are no ot her ent it ies t hat can explain t he clinical manifest at ions as indicat ed by t he exclusion clinical crit eria. Probable PSP
4. Obligat ory presence of supranuclear vert ical gaze palsy (upw ards or dow nw ards) and post ural inst abilit y w it h falls in t he first year of t he disease.
Definit e PSP
5. Possible or probable PSP w it h pat hologic confirmat ion.
Auxiliary crit eria
6. Symmet rical akinesia or rigidit y, more proximal t han dist al 7. Abnormal neck post ures, especially ret rocollus
8. Poor L-dopa response 9. Early dysart hria and dysphagia
10. Early cognit ive deficit s, including at least t w o of t he follow ing: apat hy, deficit of abst ract ion, poor verbal fluency, imit at ion behavior, front al release signs.
Mandat ory exclusion crit eria
• Presence of recent encephalit is,
• Presence of alien hand syndrome, sensorial cort ical deficit s, front al or t emporo-pariet al focal at rophy, • Presence of hallucinat ions or delusions unrelat ed t o L-dopa,
• Presence of Alzheimer’s cort ical dement ia t ype,
• Presence of unexplained early and prominent cerebellar signs or dysaut onomia, • Presence of severe asymmet ric parkinsonian signs,
M ETHOD
Sixteen patients w ho fulfilled the NINDS -SPSP criteria for probable PSP w ere studied. The follow ing data w as ana-lyzed: sex, race, age at first evaluation, age at disease onset, first clinical manifestation, time-interval before detection of vertical gaze palsy, presence of tremors, presence of axial rig id it y, p seu d o b u lb ar m an if est at io n s, st arin g f acial expression, first diagnosis given, and time-interval before diagnosis of PSP. The assessment of this information w as carried out retrospectively in seven cases and prospectively in t he rem aining nine. The presence of dem ent ia w as diagnosed according to DSM -IV criteria. Statistical analysis of relevant data w as performed by the M INITAB softw are program and Anderson-Darling normality test.
The analysis of L-dopa response w as performed in an open and uncont rolled st udy. The init ial drug dosage regimen w as 125 mg of L-dopa t hree t imes a day, being increased t o t he maximum level t olerat ed by t he pat ient . The analysis of t he L-d op a b enef it w as ob t ained b y object ive exam inat ion perf orm ed by a f ully qualif ied movement disorder neurologist and, subject ively, by t he pat ient ’s ow n impression. The drug’s effect iveness w as classified according t o t hree different t ypes of response: a) absence of response - no object ive or subject ive benefit ; b) modest response - object ive benefit w it hout subject ive benefit or vice versa; c) good response - object ive and subject ive benefit s.
Cr an i al co m p u t er i zed t o m o g r ap h y o r m ag n et i c resonance imaging w as performed in all cases t o exclude f ront al or t em poro-pariet al f ocal at rophy, one of t he NINDS-SPSP mandat ory exclusion crit eria.
RESULTS
In t his M ovement Disorder Unit , PSP represent ed only 2.1 % of all cases of degenerat ive parkinsonism seen t hroughout t he t en-year survey.
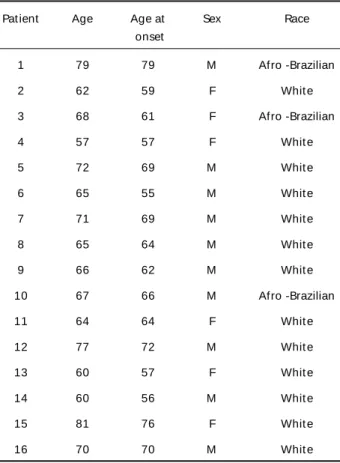
Table 2 depicts the follow ing data: sex, age, race, age at first evaluation and age at onset. According to the analysis of there data, a slight predominance of male (1.6/1) and w hite (81%) individuals w ere obser-ved in this group. The mean age at onset of this group w as 64.75 years (sd= ± 7.28). The age w as 66.28 years for men (sd= ± 7.30) and 62.33 years for w omen (sd= ± 7.20). Concerning race, the mean age of the Afro-Brazilian patients in this group w as 68.67 years (sd = ± 9.29) w h ile f o r w h it es w as 63.85 years (sd= ± 6.87). The mean period of t ime before t he detection or appearance of vertical gaze palsy (up-w ards and do(up-w n(up-w ards) (up-w as 2.34 years (min:0/max:5) as depicted in Figure 1. We did not subject Case 3 to statistical analysis, because the patient had only sought neurological assistance after 7 years of the disease and so precise information pertaining to the manifestation of vertical gaze palsy could not be obtained.
The most common first clinical manifest at ion w as post ural inst abilit y w it h falls (n= 10;62.5%). Inau-gural supranuclear vert ical gaze palsy occurred in only t w o pat ient s (12.5%). Curiously, t w o pat ient s (12.5%) had ocular complaint s, as probable inau-gural manifest at ions, resembling chronic dacryocys-t idacryocys-t is. These padacryocys-t iendacryocys-t s w ere firsdacryocys-t seen by ophdacryocys-t halmolo-gist s but dacryocyst ography did not conf irm t he diagnosis of chronic dacryocyst it is.
Table 2. Dat a on pat ient s w it h PSP.
Pat ient Age Age at Sex Race
onset
1 79 79 M Afro -Brazilian
2 62 59 F Whit e
3 68 61 F Afro -Brazilian
4 57 57 F Whit e
5 72 69 M Whit e
6 65 55 M Whit e
7 71 69 M Whit e
8 65 64 M Whit e
9 66 62 M Whit e
10 67 66 M Afro -Brazilian
11 64 64 F Whit e
12 77 72 M Whit e
13 60 57 F Whit e
14 60 56 M Whit e
15 81 76 F Whit e
16 70 70 M Whit e
F, female; M , male.
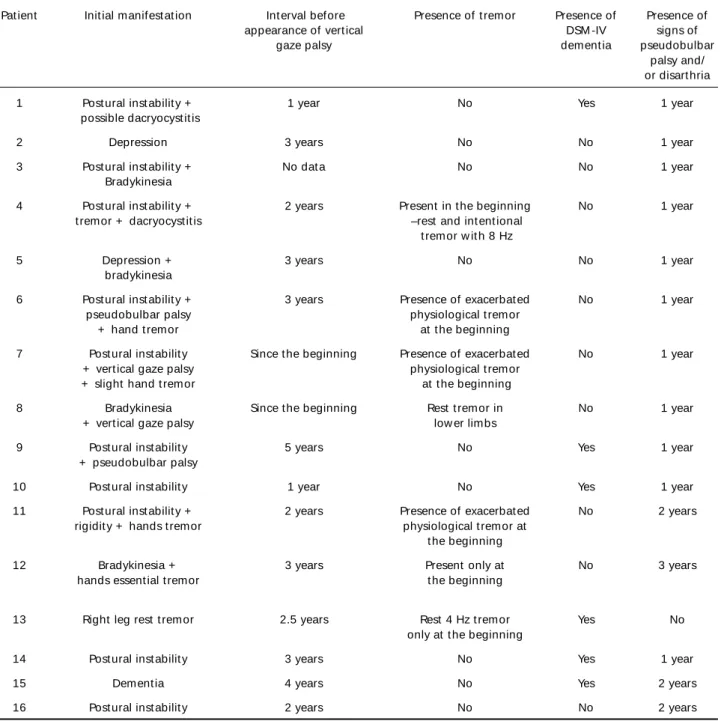
Tremor w as observed transiently in 44% (n= 7) of the cases, w hereas the typical rest tremor of Parkin-son’s disease w as observed in only 19% (n= 3). Axial rigidit y w as present in all pat ient s, albeit not obser-ved or report ed as t he first manifest at ion and pro-gressive pseudobulbar palsy w as observed in 94% of t he pat ient s being one of t he init ial manifest at ions in five (31%) cases. Only 37.5 % (n= 6) of patients had dementia according to DSM -IV criteria, although only 33% (n= 2) of this subgroup performed badly in recent memory t asks of t he M ini-M ent al St at e Examina-t ion16. The main clinical dat a are list ed in Table 3.
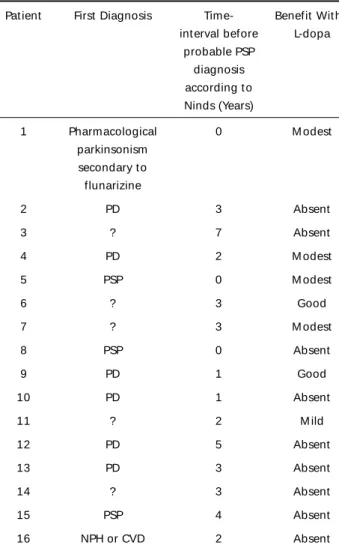
Parkinson’s disease w as the most commonly given
first diagnosis (n= 6;31%) w here PSP w as considered as t he first diagnosis in only 19% (n= 3) of t he cases. Excluding Case 3, t he mean period of t ime before a suspect ed PSP diagnosis in t his group w as 2.13 years (sd= ± 1.50).
All patients received L-dopa according to the me-thod described above. No L-dopa related dyskinesia w as observed and possibly only 13% of the patients experienced any t emporary benefit w it h t his drug. Thirty-one percent of the cases had a modest benefit w hilst the majority (56%) had no benefit. Table 4 show s the data of first diagnosis, the time–interval before the diagnosis of PSP and the benefit w ith L-dopa.
Table 3. Main clinical manifest at ions.
Pat ient Init ial manifest at ion Int erval before Presence of t remor Presence of Presence of
appearance of vert ical DSM -IV signs of
gaze palsy dement ia pseudobulbar
palsy and/ or disart hria
1 Post ural inst abilit y + 1 year No Yes 1 year
possible dacryocyst it is
2 Depression 3 years No No 1 year
3 Post ural inst abilit y + No dat a No No 1 year
Bradykinesia
4 Post ural inst abilit y + 2 years Present in t he beginning No 1 year t remor + dacryocyst it is –rest and int ent ional
t remor w it h 8 Hz
5 Depression + 3 years No No 1 year
bradykinesia
6 Post ural inst abilit y + 3 years Presence of exacerbat ed No 1 year
pseudobulbar palsy physiological t remor
+ hand t remor at t he beginning
7 Post ural inst abilit y Since t he beginning Presence of exacerbat ed No 1 year + vert ical gaze palsy physiological t remor
+ slight hand t remor at t he beginning
8 Bradykinesia Since t he beginning Rest t remor in No 1 year
+ vert ical gaze palsy low er limbs
9 Post ural inst abilit y 5 years No Yes 1 year
+ pseudobulbar palsy
10 Post ural inst abilit y 1 year No Yes 1 year
11 Post ural inst abilit y + 2 years Presence of exacerbat ed No 2 years rigidit y + hands t remor physiological t remor at
t he beginning
12 Bradykinesia + 3 years Present only at No 3 years
hands essent ial t remor t he beginning
13 Right leg rest t remor 2.5 years Rest 4 Hz t remor Yes No
only at t he beginning
14 Post ural inst abilit y 3 years No Yes 1 year
15 Dement ia 4 years No Yes 2 years
DISCUSSION
The correct diagnosis of PSP is not a difficult task w hen the clinical profile of the disease is completely developed. How ever, at the early stage of the disease, it can be quite difficult to make a precise diagnosis. In this group, only 19% of the patients received the right diagnosis. In 54% of our patients, diagnoses other than PSP w ere given, and 85% of such cases w ere misdi-agnosed as Parkinson’s disease. These difficulties in diagnosis had already been reported by Litvan et al.9.
Though it seems easy t o ident ify PSP, t he mean period of t ime before correct diagnosis w as 2.4 years in t he present st udy. Krist ensen7 report ed t hat t his
period w as 3.9 years in his series and Lit van et al.8
found t hat t he mean lat ency for diagnosis w as 3.5 years. They est im at ed t hat only 50% of pat ient s receive t he correct PSP diagnosis at first evaluat ion.
The presence of a 4 Hz rest t remor is a t ypical sign, generally associat ed w it h Parkinson’s disease,
and some researchers considered t hat t he presence of such t remors almost excludes t he diagnosis of PSP6. How ever, t he NINDS-SPSP crit eria brought new
concept s t o diagnosis. The presence of rest t remor w as not includ ed as a m ajor exclusion crit eria. Despit e such manifest at ions in PSP being quit e rare, t heir very presence does not exclude t he diagnosis of probable PSP. In our st udy, 3 pat ient s (19%) had rest t remors, w hich w ere subsequent ly classified as t ypical parkinsonian t remors. This finding is similar t o t hat of ot her series3,4,8,11,17, except low er w hen
compared w it h t he Fénelon et al. st udy5. The
pre-sence of t remor might have significant impact on t he difficult y in making t he correct diagnosis. We observed t hat 50% of t he cases init ially diagnosed as Parkinson’s disease, had t remors (Cases 4, 12 and 13). M oreover, 5 pat ient s had t remors as one of t he inaugural manifest at ions.
Good response t o L-dopa is commonly relat ed as an auxiliary crit erion for t he diagnosis of Parkinson’s disease, but ot her diseases may also respond t o t his drug. Only 13% of our pat ient s had a t emporary good response t o L-dopa, w hich w as sim ilar t o anot her st udies st udy18.
Recent ly, Lit van et al.10 observed a slight
predo-minance of males in a group of patients w ith autopsy confirmat ion. This fact w as also not ed in t his st udy, alt hough for st at ist ical confirmat ion, it w ould be ne-cessary to compare that data w ith the sex distribution of t he pat ient s seen in our M ovement Disorders Unit . The same problem occurred concerning race dat a: apparent ly, t here is a predominance of w hit e pa-t ienpa-t s, bupa-t pa-t his has yepa-t pa-t o be confirmed by spa-t apa-t ispa-t ical analysis. The mean age at onset of t he disease is similar t o t hat found in ot her st udies, suggest ing t hat PSP in Brazil follow s t he same pat t ern described w orldw ide. The same conclusion can be draw n con-cerning t he most common first clinical manifest at ion w here post ural inst abilit y w as also t he m ain ina-ugural finding described in our survey.
In t he present st udy, it is import ant t o point out an uncommon finding: t w o of our pat ient s looked f irst f or opt halm ological care w it h ocular clinical complaint s resembling chronic dacryocyst it is, even t h o u g h t h i s d i ag n o si s w as n o t co n f i r m ed b y dacryocyst ography. We speculat e t hat such compla-int s w ere probably relat ed t o t he paucit y of blinking commonly observed in PSP pat ient s.
The classic study of Albert et al.19, PSP w as
con-sidered a paradigm of “ subcortical dementia” since the lesions w ere concentrated at basal ganglia. Recent
Table 4. First Diagnosis And Time-interval Before Diagnosis of PSP.
Pat ient First Diagnosis Time- Benefit Wit h int erval before L-dopa
probable PSP diagnosis according t o Ninds (Years)
1 Pharmacological 0 M odest
parkinsonism secondary t o flunarizine
2 PD 3 Absent
3 ? 7 Absent
4 PD 2 M odest
5 PSP 0 M odest
6 ? 3 Good
7 ? 3 M odest
8 PSP 0 Absent
9 PD 1 Good
10 PD 1 Absent
11 ? 2 M ild
12 PD 5 Absent
13 PD 3 Absent
14 ? 3 Absent
15 PSP 4 Absent
16 NPH or CVD 2 Absent
PD, Parkinson’s disease; PSP, progressive supranuclear palsy; NPH, normal
evidence of damage at slices 2 and 3 of frontal lobe associat ion cort ex, along w it h presence of neuro-fibrillary PSP tangles (NFT) and deposits of tau protein in pat ient s w it h clinical PSP20-22 has show n t hat a
“ cortical” lesion is also present in many cases of PSP. DeBruin and Lees reported in a meta-analysis5 that
almost 40% of post-mortem confirmed cases of PSP
had NFT in the cortex, but they did not find a clear link bet w een t he presence of cort ical NFT and poor cognit ive performance. In cont rast , Forst er et al.23
found a correlation betw een the severity of dementia and cortical damage w ith cortical neuronal loss and gliosis, in PSP patients. In the present study, w e also observed that dementia w as not a prominent finding in PSP patients, w hereas others5 had observed 71%
dementia, in their series of PSP patients. So that, w e considered the term “ subcortical dementia” inappro-priate in many PSP patients w ith cognitive dysfunction.
REFERENCES
1. Richardson JC, Steele J, Olszewski J. Supranuclear ophthalmoplegia, pseudobulbar palsy, nuchal dystonia and dementia. A clinical report on eight cases of heterogeneous system degeneration. Trans Am Neurol Ass 1963;88:25-29.
2. Steele JC, Richardson JC, Olszewski J. Progressive supranuclear palsy: a heterogeneous degeneration involving the brain stem, basal ganglia and cerebellum w ith vertical gaze and pseudobulbar palsy, nuchal dystonia and dementia. Arch Neurol 1964;10:333-358.
3. Colosimo C, Albanese A, Hughes AJ, De Bruin VM, Lees AJ. Some sp ecific clinical features d ifferentiate multip le system atro p hy (striato nig ral v ariety ) fro m Parkinso n’ s d isease. A rch N euro l 1995;52:294-298.
4. De Bruin VM, Lees A J. Subco rtical neuro fibrillary d egeneratio n presenting as SRO and o ther related syndro mes: a review o f 90 pathologically verified cases. Mov Disord 1994;9:381-389.
5. Fénelon G, Guillard A , Romatet S, Feve A , Mahieux F. Les signes parkinsoniens du syndrome de Steele-Richardson-Olszew ski. Rev Neurol (Paris) 1993;149:30-36.
6. Golbe LI, Davis PH. Progressive supranuclear palsy. In Jankovic J, To lo sa E (Ed s.). Parkinso n’ s d isease and mo v ement d iso rd ers. Baltimore, Williams & Wilkins, 1993:145-161.
7. Kristensen MO. Progressive supranuclear palsy: 20 years later. Acta Neurol Scand 1985;71:177.
8. Litvan I. The clinical and patho lo gical hallmarks o f pro gressive supranuclear palsy. Cur Opin Neurol 1997;10:346-350.
9. Litvan I, Mangone CA, Mckee A, et al. Natural history of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome) and clinical prediction of survival: a clinicopathological study. J Neurol Neurosurg Psychiatry 1996;60:615-620.
10. Litvan I, Agid Y, Calne D, et al. Clinical research criteria for the diagnosis o f pro gressive supranuclear palsy (Steele-Richard so n-Olszew ski synd ro me): repo rt o f the NINDS-SPSP internatio nal w o rksho p. Neurology 1996;47:1-9.
11. Maher ER, Lees AJ. The clinical features and natural hystory of Steele-Richardson-Olszew ski syndrome (progressive supranuclear palsy). Neurology 1986;36:1005-1008.
12. Steele JC. Progressive supranuclear palsy. Brain 1972; 95:693-704. 13. Rajput AH, Rozdilsky B, Rajput A. Accuracy of clinical diagnosis in
parkinsonism: a prospective study. Can J Neurol Sci 1991;18:275-278. 14. Litvan I, Agid Y, Jankovic J, et al. Accuracy of clinical criteria for the diagno sis o f pro gressive supranuclear palsy (Steele-Richardso n-Olszewski syndrome). Neurology 1996;46:922-930.
15. Litvan I. Progressive supranuclear palsy: staring into the past, moving into the future. Neurologist 1998;4:13-20.
16. Folstein MF, Folstein SE, Mchugh PR. “ Mini – mental state” : a clinical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189-198.
17. Co llins SJ, A hlsko g JE, Parisi JE, Marangano re DM. Pro gressive supranuclear palsy: neuropathologically based diagnostic criteria. J Neurol Neurosurg Psychiatry 1995;58:167-173.
18. Jackson JA, Jankovic J, Ford J. Progressive supranuclear palsy: clinical features and resp o nse to tratment in 16 p atients. A nn N euro l 1983;13:273-278.
19. Albert Ml, Feldman RG, Willis AL. The “subcortical dementia” of progressive supranuclear palsy. J Neurol Neurosurg Psychiatry 1974;17:121-130. 20. Daniel SE, De Bruin VM, Lees AJ. The clinical and pathological spectrum of
Steele-Richardson-Olszew ski syndrome (PSP): a reappraisal. Brain 1995;118:759-770.
21. Vermesch P, Ro bitaille Y, Bernier L. Bio chemical map p ing o f neurofibrillary degeneration in a case of psp: evidence for general cortical involvement. Acta Neuropathol (Berlin) 1994;87:572-577. 22. Verny M, Duyckaert S, Agid Y, Hauw JJ. The significance of cortical
pathology in progressive supranuclear palsy: clinico-pathological data in 10 cases. Brain 1996;119:1123-1136.