Revista
Brasileira
de
Hematologia
e
Hemoterapia
Brazilian
Journal
of
Hematology
and
Hemotherapy
w w w . r b h h . o r g
Original
article
Results
of
high-risk
neutropenia
therapy
of
hematology–oncology
patients
in
a
university
hospital
in
Uruguay
Matilde
Boada
Burutaran
∗,1,
Regina
Guadagna
1,
Sofia
Grille
1,
Mariana
Stevenazzi,
Cecilia
Guillermo,
Lilian
Diaz
UniversidaddelaRepública,Montevideo,Uruguay
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received5May2014
Accepted9July2014
Availableonline21November2014
Keywords: Neutropenia Clinicalprotocols
Hematologicdiseases
Gram-negativebacterialinfections
Drugresistance,bacterial
a
b
s
t
r
a
c
t
Background:Febrile neutropenia is an important cause of mortality and morbidity in
hematology–oncologypatientsundergoingchemotherapy.Themanagementoffebrile
neu-tropeniaistypicallyalgorithm-driven.Theaimofthisstudywastoassesstheresultsofa standardizedprotocolforthetreatmentoffebrileneutropenia.
Methods:Aretrospectivecohortstudy(2011–2012)wasconductedofpatientswithhigh-risk
neutropeniainahematology–oncologyservice.
Results:Forty-fourepisodesof17patientswithamedianageof48years(range:18–78years) wereincluded.Theincidenceoffebrileneutropeniawas61.4%.Thepresenceoffebrile neu-tropeniawasassociatedwithboththedurationandseverityofneutropenia.Microbiological
agentswereisolatedfromdifferentsourcesin59.3%oftheepisodeswithbacteremia
iso-latedfrombloodbeingthemostprevalent(81.3%).Multipledrug-resistantgram-negative
bacilliwereisolatedin62.5%ofallmicrobiologicallydocumentedinfections.Treatmentof 63%oftheepisodesinwhichtheinitialtreatmentwaspiperacillin/tazobactamneededtobe
escalatedtomeropenem.Themortalityrateduetofebrileneutropeniaepisodeswas18.5%.
Conclusion:Thehighrateofgram-negativebacilliresistanttopiperacillin/tazobactam
(front-lineantibioticsinourprotocol)andtheearlyneedtoescalatetocarbapenemsraisesthe
questionastowhetheritisnecessarytochangethecurrentprotocol.
©2014Associac¸ãoBrasileiradeHematologia,HemoterapiaeTerapiaCelular.Published
byElsevierEditoraLtda.Allrightsreserved.
Introduction
Febrile neutropenia (FN) is among the leading causes of
mortality and morbidity in hematology-oncologic patients
∗ Correspondingauthorat:HospitaldeClínicas,FacultaddeMedicina,UniversidaddelaRepública,Av.Italias.n.,CP11600Montevideo,
Uruguay.
E-mailaddress:matildeboada@hotmail.com(M.BoadaBurutaran).
1 Theseauthorscontributedequallytothiswork.
undergoing intensive cytotoxic chemotherapy. It implies a
largeeconomicandsocialburdenonthehealthsystem1,2asit
representsthemostfrequentcomplicationinthesepatients.3
Infectious complications are the main cause of death not
relatedtocancerprogression.
http://dx.doi.org/10.1016/j.bjhh.2014.11.012
1516-8484/©2014Associac¸ãoBrasileiradeHematologia,HemoterapiaeTerapiaCelular.PublishedbyElsevierEditoraLtda.Allrights
Theincidence ofFN was reported inaround 10–50% of
patients with solid tumors and up to 80% of those with
hematologicmalignancies.4Inthepre-empiricantibioticsera,
mortalityduetoinfectiouscomplicationsinpatients
receiv-ingintensivechemotherapywasashighas70%.5Nowadays,
thisfigurehasdroppedtobetween1%and18%,4,6,7butstill
representsaseriousproblemthatmustbeaddressedactively
usingamultidisciplinaryapproach.
FNisapotentiallylife-threateningsituationthatrequires
promptmedicalintervention.Asneutropenicpatients have
an impaired inflammatory response, infection can occur
with minimal signs and symptoms and progress rapidly,
evolving withhypotension, renal failure, acidosis, or other
life-threateningcomplicationsthatleadtosepsiswith
mul-tiorganfailure.2Asfevermayconstitutetheisolatedsignin
thesepatients,itshouldbeconsideredarealemergency.Early
recognitionofFNiscriticaltoinitiatebroad-spectrum,empiric
systemicantibacterialtherapypromptlyinordertoavoid
pro-gressiontosepsisandpossibledeath.8
The prophylactic use of granulocyte colony-stimulating
factor (G-CSF)to reducethe incidenceofFN, aswell as to
enhanceantibiotictherapy, hasbeen widelystudiedinthe
lastfewyears withconflictingresults.9 In2004aCochrane
collaborationreviewconcludedthattheuseofgrowthfactors
combinedwithantibiotic therapyinestablishedFNcaused
bychemotherapyreducedthehospitalstayandtheduration
ofneutropenia,buttheoverallmortalitywasnotinfluenced
significantly.9Furthermore,ameta-analysisin2011concluded
that the use ofG-CSF asprimary prophylaxis reduced the
incidenceofFNinpatientsreceivingchemotherapyforsolid
tumorsandlymphoma.10
ThemanagementofFNistypicallyalgorithm-driven.The
effectivenessoftheantibacterialprotocolproposedby
inter-nationalguidelinestoreduceFN-relatedmortalityhasalready
beenreported.4,7 Thus,theaimofthis studywastoassess
the impact of the implementation of international
recom-mendationsasthestandardizedprotocoloflocalguidelines
in2011.11Oneofthespecificobjectivesofthisstudywasto
assesswhether theprotocolwas correctlyfollowedineach
case.
Methods
Thisisananalyticobservational,retrospective,cohortstudy
conductedfromJuly2011toAugust2012.Thedatawere
col-lectedfromthemedicalchartspreservingtheconfidentiality
ofeachpatient.
Patients
Theinclusioncriteriawerepatientsolderthan18years,
under-goingintensive chemotherapyinthe Hematology–oncology
DepartmentoftheHospitaldeclínicas Dr.ManuelQuintela
inMontevideo,Uruguay,forwhomhigh-riskneutropeniawas
expected.Patientstreatedinthisservicethat,becauseoftheir
personal risk factors and comorbidities, suffered high-risk
neutropeniabutdidnotreceiveintensivechemotherapywere
excluded.
Definitions
Intensivechemotherapywasdefinedaschemotherapy
regi-mensthat causehigh-risk neutropeniasuchasthose used
totreatacutemyeloid leukemia,acute lymphoidleukemia,
Burkittlymphoma,andsecondlinesforHodgkin’sand
Non-Hodgkin’slymphoma.High-risk neutropeniawasdefinedas
onethatisexpectedtolastmorethansevendays.
Neutropenia was defined as a neutrophil count under
0.5×109/Lorunder1.0×109/Lwhenitwasexpectedtoreach
under0.5×109/Lwithinthefollowing48h.Severeneutropenia
wasdefinedasaneutrophilcountunder0.1×109/L.Patients
diagnosedwithacuteleukemiawereconsideredtohave
func-tionalneutropeniaeventhoughtheyhadneutrophilcounts
above1.0×109/L. Feverwasdefinedasanoraltemperature
above38◦Corapersistenttemperatureabove37.8◦C.
Alarmsignsweredefinedintheprotocolasthepresence
ofatleastoneofthefollowing:heartrateabove100beatsper
minute,respiratoryfrequencyabove20breathsperminute,
lowcarbondioxideunder35mmHg,oxygenunder100mmHg
oroxygensaturationunder93%whilereceiving
supplemen-taryoxygen,capillaryrefilllongerthaneightseconds,lowpH,
baseexcessunder5meq/L,serumlactateabove2mmol/L,
sys-tolicbloodpressureunder90mmHg,confusion,oroliguria.
Clinicalandlaboratorystudies
When a febrile episodewas diagnosed, adetailed physical
examinationwasmadeandrepeateddaily.Additionally,
sam-plesofblood,andurineand samplesfrom othersuspected
infection sites were taken before the initiation of
empiri-calantibiotictreatment.Ifthepatienthadacentralvenous
catheter, at least oneblood culture was preparedforeach
lumenofthecatheterandoneofaperipheralvein.Achest
radiographwasobtainedandurinalysisperformedwithinthe
first 24h. Computed tomographies (CT) ofthe lung, head,
sinuses, abdomen, and pelvis were performed asclinically
indicated.Routinehematologicalinvestigationsand
biochem-icalanalysiswerecarriedoutbeforetreatmentwasstartedand
everythreedaysthereafterduringthecourseofthetherapy.
Additionally, C-reactive protein and procalcitonin levels
weredetermined.AsinusandlungCTandserial
galactoman-nan antigen testwere performed priorto the initiation of
antifungal therapy when afungal infection was suspected
in patients who remained febrile after 6–7 days of
broad-spectrumantibiotictreatment.
Antibiotictreatmentprotocol
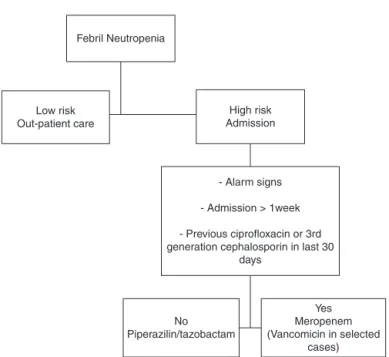
Theprotocolconsistedintheuseofabroad-spectrum
antimi-crobial (Figure 1).11 Piperacillin–tazobactam therapy (4.5g
every6h)wasstartedinpatientswithoutoneofthefollowing:
alarmsigns,morethanoneweekofhospitalstay,orhaving
received ciprofloxacin or third-generationcephalosporin as
prophylaxiswithintheprevious30days.Theotherpatients
receivedmeropenem(1gevery8h).Prophylacticantiviral
(acy-clovir)andantifungal(fluconazole)medicationsweregivenin
allcases.
The initialempiricaltreatment was modifiedby
Febril Neutropenia
Low risk Out-patient care
High risk Admission
- Alarm signs
- Admission > 1week
- Previous ciprofloxacin or 3rd generation cephalosporin in last 30
days
No Piperazilin/tazobactam
Yes Meropenem (Vancomicin in selected
cases)
Figure1–Protocol-basedalgorithminthemanagementof febrileneutropenia.
deterioration in the clinical state after 24h, (b) alarm
signs, hemodynamic instability or other organ
dysfunc-tion, (c)fever persistence afterfour days oftreatment, (d)
culture with antibiotic-resistant organism (particularly
methicillin-resistant Staphylococcus aureus [MRSA] or
extended-spectrum b-lactamase [ESBL]-producing
gram-negativebacteria).Inpatientswithhemodynamicinstability,
skinorsofttissueinfection,suspectedcatheter-related
infec-tion or MRSA culturepositive, vancomycin was added (1g
every12h).Vancomycinwasstoppedaftertwodaysifthere
was no evidence of gram-positive infection. Documented
clinical and/ormicrobiological infectionswere treatedwith
antibiotics appropriate for the site and susceptibility of
each isolated organism. Empirical antifungal coverage was
consideredinpatientswhohadpersistentfeverafter6–7days
ofantibiotictreatmentwithoutidentifiedfeversource.
Statisticalanalysis
Statistical analysis was made using the Statistics Program
forSocialSciences software. TheChi-squaretest wasused
tocomparecategoricalvariablesandtheMann–Whitneytest
for continuousvariables. TheOdds ratiowas calculated.A
p-value<0.05wasconsideredstatisticallysignificant.
Results
Forty-fourepisodesofhigh-riskneutropenia(17patients)with
amedianageof48years(range:18–78years)wereincluded
inthisstudy (Table1).There wasaslightpredominanceof
females(female:maleratio1.1:1).Thedistributionofcancer
Table1–Patients’characteristic.
Febrileepisodes Non-febrileepisodes Total p-Value
Episodes–n(%) 27(61.4) 17(38.6) 44–100 0.49
Age–median(range)years 43 40.1 48(18–78) 0.06
Gender–female:male 1.0:1.0 0.7:1.0 1.1:1 0.49
Febriledays–median±SD 4.5±4.4 4.5±4.4
Neutropenia–median±SD(days) 16.1±8 9±3.8 13.1±7.8 0.001
Severeneutropenia–median±SD(days) 7.8±5.3 3.5±3.0 6.2±5.0 0.005
Hematology–oncologydiagnosis n (%) n (%) n (%)
AML/myelodysplasticsyndromes 18 66.6 7 41.2 25 56.8
Acutelymphoidleukemia 2 7.5 1 5.9 3 6.8
Non-Hodgkin’slymphoma 7 25.9 7 41.2 14 31.9
Hodgkin’slymphoma 0 0 2 11.7 2 4.5
Chemotherapyregimen n (%) n (%) n (%)
High-dosecytarabine(HIDAC) 6 24.0 7 41.2 13 29.5
Cytarabine–Daunorubicin(7+3) 8 32.0 0 0 8 18.2
CODOX-M 4 16.0 3 17.6 7 15.9
IVAC 1 4.0 2 11.8 3 6.8
FLAG 2 8.0 0 0 2 4.5
ESHAP 0 0.0 2 11.8 2 4.5
MINIBEAM 0 0.0 2 11.8 2 4.5
Berlin–Frankfurt–Munich(BFM)2008protocol 1 4.0 1 5.8 2 4.5
Hyper-CVAD 1 4.0 0 0 1 2.3
IVE 1 4.0 0 0 1 2.3
HIDAC+Daunorubicin 1 4.0 0 0 1 2.3
20
18
16
14
12
10
8
6
4
2
0
P-value=0.001
P-value=0.005 Febrile episodes Non-febrile episodes
Days of neutropenia Days of severe neutropenia
Figure2–Daysoffebrileneutropenia.
typesandchemotherapytreatment regimensare shown in
Table1.Acutemyeloidleukemia(AML)anditstreatmentwere
themostcommontypeofcancerandchemotherapyregimen.
Non-Hodgkin’slymphomascomprisingBurkitt’slymphomas
(nineepisodesregisteredintwopatients),lymphoblastic
lym-phoma(oneepisode),entheropathy-associatedTLymphoma
(oneepisode),andrefractoryorrelapseddiffuselargecell
lym-phomaorTlymphomas(threeepisodesintwopatients)were
observed.
Ofthe 44 episodes ofhigh-risk neutropenia, 27 (61.4%)
experiencedfeverduringneutropenia.Everypatientincluded
inthisstudyexperiencedFNinatleastoneoftheepisodes.
Accordingtothe results,FNwassignificantlyassociated
withboththedurationofneutropenia(p-value=0.001)witha
medianofninedaysforafebrilevs.16daysforfebrileepisodes,
andthedurationofsevereneutropenia(p-value=0.005)with
amedianof3.5daysforafebrilecomparedwith7.8daysfor
febrileepisodes(Figure2).Theprophylacticuseoffilgrastim
was notstandardizedin our serviceand dependedon the
choiceofeachphysician.Theuseoffilgrastimwasassociated
withneitherthedurationnortheincidenceofFN.In62%of
theepisodes,thesiteofinfectionwasidentified,either
clini-cally,byimagingtechniques,orbymicrobiologicalcultures.As
Table2–Clinicalsiteofinfection.
Clinicalsiteofinfection n(%)
Notidentified 23(52.3%)
Lungs 8(18.2%)
Skin 3(6.8%)
Urinarytract 2(4.5%)
Abdominal 1(2.3%)
Ear,nose,orthroat 1(2.3%)
Others 1(2.3%)
Table3–Microbiologicalisolation.
Microbiologicalagent Relativefrequency(%)
Multi-resistantKlebsiella 37.5 Multi-resistantE.coli 25.0
SensitiveE.coli 12.5
Methicillin-resistantStaphylococcusaureus 6.3 CoagulasenegativeStaphylococcus 6.3
Chriseobacteriumindologens 6.3
Mycobacteriumtuberculosis 6.3
showninTable2,therespiratorytractwasthemostcommon
siteofinfection(41%),followedbytheskinandothers.
Microbiologicalcultureswereachievedin59.3%(n=16)of
the febrile episodes (Table 2).A totalof75% ofall isolates
weregram-negativebacilli(GNB).Ofthe
multiple-antibiotic-resistant (MR)GNB(62.5%),definedasresistancetoatleast
threedifferentantibioticgroups,sixisolateswereMRKlebsiella pneumoniae(specificallyESBLK.pneumonia)andfourisolates wereMREscherichiacoli(ESBL).Regardingthesourceofthe iso-late(Table3),13werefrombloodcultures,representing48%of
bacteremiainallFNepisodesand81.3%ofallmicrobiological
documentedinfections.AlloftheMR-GNBweresusceptible
toimipenem,meropenemandamikacinandresistanttoall
other antibioticclasses, includingpiperacillin and
tazobac-tam.
WhenconsideringonlythefirstFNepisodeofeachpatient,
microbiological isolates were identified in 53% of episodes
with77.7%ofthesebeingMR-GNB.For14(63%)oftheepisodes
inwhich theinitialtreatment waspiperacillin/tazobactam,
therapy needed to be escalated to meropenem in amean
timeof4.5±2.5daysoftreatment.Themortalityrateofthese
episodeswas28%;47%hadaMR-GNBand35%hadnegative
cultures.Onepatientwasdiagnosedwithpulmonary
tubercu-losis.
Theoverallmortalityrateinallneutropenicepisodeswas
13.6% (n=6) and the mortality rate in febrile neutropenic
episodesalonewas18.5%.Threeofthesepatientsdieddueto
sepsis(11.1%ofmortalityduetosepsisinFNepisodes)andthe
othersduetodiseaseprogression.Everydeath-related
infec-tionwasreportedinthefirstFNepisode.Deathoccurredin
35%oftheepisodesinwhichthemicrobiologicalagentwas
isolatedandtherewerenodeathsinepisodeswithnegative
cultures(p-value=0.027).
Nine(33%)oftheFNepisodespresentedatleastoneofthe
alarmsignsdefinedintheprotocolofthisstudy.The
mortal-ityrateofthesewas44%vs.6%inepisodeswithoutalarm
signs(p-value=0.018).ThisdeterminesanORof13.0forthe
presenceofalarmsigns.
There were 15 (34.1%) episodes that were treated with
piperacillin–tazobactam as front-line therapy even though
thesepatientshadreceivedprophylaxiswithciprofloxacin.
Discussion
Infectious diseases are an important complication in
hematology-oncologic patients resulting in longer hospital
stays,andincreasedmorbidityandmortality.Neutropeniahas
developmentofinfectionsinhematology-oncologicpatients
undergoingchemotherapy.12
Here,wepresentthefirst-yearresultsandfeaturesof
infec-tiousdiseases sincethe implementation ofanewprotocol
inthemanagementofFNinhigh-riskhematology-oncologic
patientsataUniversityHospitalinUruguay.Beforethe
imple-mentationofthis protocolthe managementofFNwas not
standardizedinthisserviceandphysiciansdecidedbasedon
theavailableevidence,theinternationalguidelines,andtheir
ownpersonalexperience.
Themainfindingsofthisworkwerethehighrateof
micro-biologicalagents isolated inFN episodes, and theelevated
prevalenceofMR-GNB.
Microbiological documentedinfections were statistically
associated with higher mortality. This finding can be
explainedbythefactthatbacteremiawasthemostfrequent
documentedinfection(81.3%).Teixeiraetal.recentlyreported
that in hematopoietic stem cell transplantation patients,
microbiologicallydocumentedinfectionsrepresentedadeath
riskfactorandthatbacteremiawasthemostcommonly
doc-umentedinfection(46.3%).13Furthermore,itisknownthatin
otherinfectiousdiseases,suchascommunity-acquired
pneu-mococcalpneumonia,bacteremiaisassociatedwithincreased
severityandmortality.14
TheetiologyofinfectionsinFNhasvariedinthelastfifty
years.Inthe1970sandearly1980stherewasapredominance
ofgram-negativemicroorganismsbut inthe late1980sand
inthe1990stherewasadramaticincreaseingram-positive
bacteria, withthese becoming themost commoninfecting
organisms.15,16 Thisledtochangesinantibiotictreatments,
focusing on resistant gram-positive strains.17 However, in
the last few years, an increase in GNB has been reported
worldwide.16Thisworkidentifiedanimportantpredominance
ofGNBconcordantwithotherrecentregionalreports.14,15
However,thereweremoreresistantGNB,particularlyESBL,
thanreportedinmostseries.13,15,16
Therewasanearlyneedtoescalatetomeropenemina
highnumberofepisodes,andinmanyofthemMR-GNBwere
isolated.
Themortalityrateobservedduetosepsiswas23.5%and
thiswasstatisticallyassociatedwiththeisolationof
microbi-ologicalagentsandthepresenceofatleastonealarmsign.
Theincidence of FN in our service was similar to
oth-ersreportedintheliterature.4,6,7However,themortalityrates
wereslightlyhigherthanreportedbyreferralservicesbut
sim-ilartothosereportedinotherLatinAmericancountries.18,19
Thepresenceoffeverwasassociatedwithdurationand
severityofneutropenia.Historical studiesshowthatasthe
neutrophil countdrops below0.5×109/L, the susceptibility
toinfectionincreases.20 Moreover,ithasbeenreportedthat
thefrequencyandseverityofinfectionareinversely
propor-tionaltothe neutrophil count.Theriskofsevere infection
andbacteremiaare highwhentheneutrophil countisless
than1.0×109/L.Therateofdeclineoftheneutrophilcount
andthe durationofneutropeniaare alsoimportantfactors
to consider.21–23 Additionally, it has been reported that an
increaseintheneutrophilcountduringtreatmentimproves
outcomes.Bodeyetal.informedthatthemortalityratewas
higher(80%)amongpatientswhoinitiallystartedwith
neu-trophil counts below 1.0×109/L that did not rise during
the first weekofinfection comparedtothe mortalityrates
(27%)seen inpatientswhose neutrophilcountsroseabove
10.0×109/L.21
Hematopoietic growth-stimulating factors are a classof
cytokinesthatregulateproliferation,differentiation,and
func-tions of hematopoietic cells. G-CSF regulates neutrophil
production.24TheadministrationofG-CSFtohumansresults
in a dose-dependent increase in circulating neutrophils.24
Inthis study,asignificantreductionintheincidenceofFN
usingfilgrastimwasnotfound,contrarytowhatwasexpected
accordingtotheliterature.9,10 Thisresultmaybeduetothe
small samplesize.Mostofthe episodes(77%)weretreated
usingfilgrastim.Thisresultshouldbere-analyzedwithmore
episodes.
Theprotocolwasnotadequatelyfollowedineverycase.
Althoughthismayrepresentalimitationwheninterpreting
thefindingsofthisstudy,detectingthesekindsoffailuresis
importantinorderforthemtobecorrected.
This study emphasizes the high isolation rates of
microbiological agents, especially GNB resistant to
piperacillin/tazobactam, which constitute the front-line
antibiotics inourprotocol. Theearlyneed ofescalationto
carbapenemsraisesthequestionastowhethertheseshould
bethefront-linetreatmentforhigh-riskneutropeniapatients
inourservice.Moreover,thisisabigstepascarbapenemsare
atthetopoftheantibioticoptionlistandwhenusedas
first-linetreatment,manyproblemswithresistantstrainswould
probablyarise.Asalternativestocarbapenem,acombination
ofpiperacillin–tazobactamandamikacinmaybeaneffective
empirical therapeuticoption forpatients with neutropenic
fever who are at high risk of developing bacteremia with
ESBL-producingpathogens.
Webelievethatalargerstudyshouldbeconductedbefore
makingafinaldecisionbecause,althoughthepresentwork
representsoneyear’sexperienceoftheevolutionofhigh-risk
neutropeniaatauniversityhospital,thenumberofthe
ana-lyzed episodes istoo smallto conclude thatour front-line
antibioticoptionisnotsuitable.
Conclusions
Inthis workweobservedahigh isolationrateof
microbio-logicalagentsinFNepisodes;thiswasstatisticallyassociated
with higher mortality. Bacteremia was the most common
microbiological isolate identified with a predominance of
GNB,particularlyMR.RiskfactorsforFNweredurationand
severity ofneutropeniaand the isolationofa
microbiolog-icalagent,and thepresenceofalarmsignswasassociated
with poor outcomes. The high rate of GNB resistant to
piperacillin/tazobactam,thefront-lineantibioticsinour
pro-tocol,andtheearlyneedtoescalatetocarbapenemsraises
the question as to whether it is necessary to change our
antibiotictreatmentprotocolforhigh-riskneutropenia.
Fur-therprospectivestudieswithalargernumberofpatientsand
episodesofFNshouldbeconductedtoconfirmtheseresults.
Conflicts
of
interest
Acknowledgments
Theauthors thankallthose whoparticipatedinthe
devel-opment and implementation of the febrile neutropenia
therapeuticprotocol: Infectious Diseases Department,
Bac-teriology (Clinical Laboratory Department), Pharmacology
DepartmentandIntensiveCareMedicineDepartment.
r
e
f
e
r
e
n
c
e
s
1. DulisseB,LiX,GayleJA,BarronRL,ErnstFR,RothmanKJ, etal.Aretrospectivestudyoftheclinicalandeconomic burdenduringhospitalizationsamongcancerpatientswith febrileneutropenia.JMedEcon.2013;16(6):720–35.
2. CrawfordJ,DaleDC,LymanGH.Chemotherapy-induced neutropenia:risks,consequences,andnewdirectionsforits management.Cancer.2004;100(2):228–37.
3. VandykAD,HarrisonMB,MacartneyG,Ross-WhiteA,Stacey D.Emergencydepartmentvisitsforsymptomsexperienced byoncologypatients:asystematicreview.SupportCare Cancer.2012;20(8):1589–99.
4. KlasterskyJ.Managementoffeverinneutropenicpatients withdifferentrisksofcomplications.ClinInfectDis.2004;39 Suppl.1:S32–7.
5. HershEM,BodeyGP,NiesBA,FreireichEJ.Causesofdeathin acuteleukemia:aten-yearstudyof414patientsfrom 1954–1963.JAMA.1965;193:105–9.
6. FreifeldAG,BowEJ,SepkowitzKA,BoeckhMJ,ItoJI,Mullen CA,etal.Clinicalpracticeguidelinefortheuseof
antimicrobialagentsinneutropenicpatientswithcancer: 2010updatebytheinfectiousdiseasessocietyofAmerica. ClinInfectDis.2011;52(4):e56–93.
7. WeyckerD,BarronR,KartashovA,LeggJ,LymanGH. Incidence,treatment,andconsequencesof
chemotherapy-inducedfebrileneutropeniaintheinpatient andoutpatientsettings.JOncolPharmPract.2014;20(3): 190–8.
8. LynnJ-J,ChenK-F,WengY-M,ChiuT-F.Riskfactorsassociated withcomplicationsinpatientswithchemotherapy-induced febrileneutropeniainemergencydepartment.Hematol Oncol.2013;31(4):189–96.
9. ClarkOA,LymanGH,CastroAA,ClarkLG,DjulbegovicB. Colony-stimulatingfactorsforchemotherapy-inducedfebrile neutropenia:ameta-analysisofrandomizedcontrolledtrials. JClinOncol.2005;23(18):4198–214.
10.CooperKL,MadanJ,WhyteS,StevensonMD,AkehurstRL. Granulocytecolony-stimulatingfactorsforfebrile
neutropeniaprophylaxisfollowingchemotherapy:systematic reviewandmeta-analysis.BMCCancer.2011;11:404.
11.ManejodelPacienteneutropénico.CátedradeHematología. OficinaDelLibroFEFMUR;2011.
12.KudererNM,DaleDC,CrawfordJ,CoslerLE,LymanGH. Mortality,morbidity,andcostassociatedwithfebrile neutropeniainadultcancerpatients.Cancer. 2006;106(10):2258–66.
13.MendesET,DulleyF,BassoM,BatistaMV,CoracinF, GuimarãesT,etal.Healthcare-associatedinfectionin hematopoieticstemcelltransplantationpatients:riskfactors andimpactonoutcome.IntJInfectDisIJIDOffPublIntSoc InfectDis.2012;16:e424–8.
14.KangC-I,SongJ-H,KimSH,ChungDR,PeckKR,Thamlikitkul V,etal.Riskfactorsandpathogenicsignificanceofbacteremic pneumoniainadultpatientswithcommunity-acquired pneumococcalpneumonia.JInfect.2013;66(1):34–40.
15.MarchettiO,CalandraT.Infectionsinneutropeniccancer patients.Lancet.2002;359(9308):723–5.
16.ViscoliC,VarnierO,MachettiM.Infectionsinpatientswith febrileneutropenia:epidemiology,microbiology,andrisk stratification.ClinInfectDis.2005;40Suppl.4:S240–5.
17.JarqueI,SanzMA.Applicationoftheconceptsof
evidence-basedmedicinetotheevidenceonthetreatmentof febrileneutropenia.EnfermInfeccMicrobiolClin.1999;17 Suppl.2:95–102.
18.MadridC,DíazL,CombarizaJ,GálvezK,OlayaV,RamírezI, etal.Epidemiologíadelaneutropeniafebrilenpacientes adultosconneoplasiahematológica,enunperíodode26 mesesenelHospitalPabloTobónUribe,Colombia.Rev ChilenaInfectol.2013;30(2):195–201.
19.LimaSS,Franc¸aMS,GodoiCC,MartinhoGH,deJesusLA, RomanelliRM,etal.Neutropenicpatientsandtheirinfectious complicationsataUniversityHospital.RevBrasHematol Hemoter.2013;35(1):18–22.
20.BodeyGP.Antibioticsinpatientswithneutropenia.Arch InternMed.1984;144(9):1845–51.
21.BodeyGP,BuckleyM,SatheYS,FreireichEJ.Quantitative relationshipsbetweencirculatingleukocytesandinfectionin patientswithacuteleukemia.AnnInternMed.
1966;64(2):328–40.
22.LymanGH,KudererNM.Epidemiologyoffebrileneutropenia. SupportCancerTher.2003;1(1):23–35.
23.EltingLS,RubensteinEB,RolstonKV,BodeyGP.Outcomesof bacteremiainpatientswithcancerandneutropenia: observationsfromtwodecadesofepidemiologicaland clinicaltrials.ClinInfectDis.1997;25(2):247–59.