www.jped.com.br
ORIGINAL
ARTICLE
Maternal
depression
and
anxiety
and
fetal-neonatal
growth
夽
Tiago
Miguel
Pinto
a,∗,
Filipa
Caldas
b,
Cristina
Nogueira-Silva
c,d,e,
Bárbara
Figueiredo
aaUniversidadedoMinho,EscoladePsicologia,Braga,Portugal
bUniversidadedoMinho,EscoladeCiênciasdaSaúde,Braga,Portugal
cUniversidadedoMinho,EscoladeCiênciasdaSaúde,InstitutodePesquisaemCiênciasdeVidaeSaúde(ICVS),Braga,Portugal
dICVS/3B’s---PTGovernmentAssociateLaboratory,Braga/Guimarães,Portugal eHospitaldeBraga,DepartamentodeObstetríciaeGinecologia,Braga,Portugal
Received21August2016;accepted10November2016 Availableonline20February2017
KEYWORDS Maternaldepression; Maternalanxiety; Fetal-neonatal growthoutcomes; Fetal-neonatal growthtrajectories
Abstract
Objective: Maternaldepressionandanxietyhave beenfound tonegativelyaffect fetaland
neonatalgrowth. However, the independent effectsofmaternal depression andanxietyon fetal-neonatalgrowthoutcomesandtrajectoriesremainunclear.Thisstudyaimedtoanalyze simultaneouslytheeffectsofmaternalprenataldepressionandanxietyon(1)neonatalgrowth outcomes,and(2),onfetal-neonatalgrowthtrajectories,fromthe2ndtrimesterofpregnancy tochildbirth.
Methods: A sample of172 women was recruited andcompleted self-reportedmeasures of
depressionandanxietyduringthe2ndand3rdtrimestersofpregnancy,andatchildbirth.Fetal andneonatalbiometrical datawere collectedfromclinicalreports atthesameassessment moments.
Results: Neonates of prenatally anxious mothers showed lower weight (p=0.006), length
(p=0.025),andponderal index(p=0.049)atbirth thanneonates ofprenatallynon-anxious mothers.Moreover,fetuses-neonatesofhigh-anxietymothersshowedalowerincreaseofweight fromthe2ndtrimesterofpregnancytochildbirththanfetuses-neonatesoflow-anxiety moth-ers(p<0.001).Consideringmaternaldepressionandanxietysimultaneously,onlytheeffectof maternalanxietywasfoundonthesemarkersoffetal-neonatalgrowthoutcomesand trajecto-ries.
夽
Pleasecitethisarticleas:PintoTM,CaldasF,Nogueira-SilvaC,FigueiredoB.Maternaldepressionandanxietyandfetal-neonatalgrowth. JPediatr(RioJ).2017;93:452---9.
∗Correspondingauthor.
E-mail:tmpinto@psi.uminho.pt(T.M.Pinto). http://dx.doi.org/10.1016/j.jped.2016.11.005
Conclusion: Thisstudydemonstratestheindependentlongitudinaleffectofmaternalanxietyon majormarkersoffetal-neonatalgrowthoutcomesandtrajectories,simultaneouslyconsidering theeffectofmaternaldepressionandanxiety.
©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 4.0/).
PALAVRAS-CHAVE Depressãomaternal; Ansiedadematernal; Resultadosde crescimentofetale neonatal;
Trajetóriasde crescimentofetale neonatal
Depressãoeansiedadematernalecrescimentofetal-neonatal
Resumo
Objetivo: Foiconstatadoqueadepressãoeansiedadematernaafetamnegativamenteo
cresci-mento fetaleneonatal.Contudo,oefeitoindependentedadepressãoeansiedadematerna sobreosresultadoseastrajetóriasdecrescimentofetaleneonatalcontinuaincerto.Esteestudo visouanalisarsimultaneamenteoefeitodadepressãoeansiedadematernapré-natal(1)sobre osresultadosdecrescimentoneonatale(2)sobreastrajetóriasdocrescimentofetal-neonatal apartirdo2◦trimestredegravidezatéoparto.
Métodos: Uma amostra de 172 mulheres foi recrutada e as mesmas relataram graus de
depressãoeansiedadeno2◦e3◦trimestredegravidezeparto.Osdadosbiométricosfetaise
neonataisforamcoletadosdosprontuáriosclínicosnasmesmasondasdeavaliac¸ão.
Resultados: Os neonatos de mães ansiosas no período pré-natal mostraram menor peso
(p=0.006),comprimento(p=0.025)eíndiceponderal(p=0.049)nonascimentoqueosneonatos demãesnãoansiosasnoperíodopré-natal.Alémdisso,osneonatosdemãesmuitoansiosas mostraramummenoraumentodepesodo2◦ trimestredegravidezatéopartoqueos
fetos-neonatosdemãespoucoansiosas(p<0.001).Considerandosimultaneamenteadepressãoea ansiedadematernal,apenasoefeitodaansiedadematernafoiconstatadonessesmarcadores deresultadosetrajetóriasdecrescimentofetal-neonatal.
Conclusão: Esteestudodemonstraoefeitolongitudinalindependentedaansiedadematerna
sobreosprincipaismarcadoresderesultadosetrajetóriasdecrescimentofetal-neonatal, con-siderandosimultaneamenteoefeitodadepressãoeansiedadematerna.
©2017SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4. 0/).
Introduction
The short-term consequences of prenatal depression and anxietyonpregnantwomen’sphysicalhealthinclude obstet-ric complications and physical symptoms, which areboth associatedwithlowerfetalandneonatalgrowthandlower autonomicnervoussystem (ANS)maturation.1,2 Depression
and anxiety share a common genetic pathway, and often
appear simultaneously, making it difficult to assess their
independenteffects. Thus, when analyzing the effectsof
maternal depression and anxiety, it may be important to
consider both simultaneously, in order to control their
mutualeffectsandtobetteridentifytheindependenteffect
ofeachone.3
Various studies have found similar effects of maternal
prenataldepressionandanxietyonfetalgrowth,behavior,
and ANS maturation. Bothfetuses of depressed and
anx-iousmotherswerefoundtopresentlowerestimatedweight
andhighertotalfetalactivity.4---6 Inaddition,studieshave
found that both fetuses of depressed or anxious mothers
showhigherheartratereactivitycomparedwithfetusesof
non-depressedornon-anxiousmothers.2,7---10
Moreover, studies also have found similar effects of
maternal prenatal depression and anxiety on
neona-tal growth, behavioral, and maturation outcomes. Both
neonatesof prenatally depressedor anxious mothers
pre-sented higher risk of premature birth and low weight,
both major problems of infant health.11---13 Neonates of
depressedor anxious mothers were found topresent
dis-organizedsleeppatternsand frequent changes of mood.2
Lowermaturationwasalsofoundinneonatesofprenatally
depressedor anxious mothers, includingless vagal tonus,
and lower neurobehavioral maturity.2,11,13,14 Furthermore,
both neonates of prenatally depressed or anxious
moth-erswerefoundtoshowhigherlevelsofcortisolandlower
levelsofdopamineandserotoninwhencomparedwith
hor-monal levels of neonates of prenatally non-depressed or
non-anxious mothers.15 Other studies also reported that
both infants of prenatally depressed or anxious mothers
presentincreasedadmissionratestotheneonatalcareunit
andgrowthretardationduringthefirstyearoflife.16,17
Few studies have simultaneously considered
mater-nal depression and anxiety when analyzing the effect
on fetal/neonatal growth and behavior. When
simul-taneously considering maternal depression and anxiety,
studies only found an independent effect of maternal
anxiety on fetal/neonatal growth and behavior.18---20 One
cross-sectional study only found an effect of maternal
anxiety on fetal growth and behavior (fetuses of
activity at mid-pregnancy).18 Additionally, two
longitudi-nal studies only found an effect of maternal anxiety on
fetal-neonatal growth trajectories (higher maternal
anxi-ety during pregnancy was associated with lower increase
offetal-neonatalweight).19,20 However,thesestudiesonly
included one assessment of maternal prenatal depression
andanxiety(duringpregnancy)whenanalyzingtheireffect
onfetal/neonatal growth,not addressing the longitudinal
effectofbothmaternaldepressionandanxiety.
Both maternal depression and anxiety were found to
negativelyaffectfetalandneonatalgrowth.Despitethese
effectshaving been widely documented in literature,the
independent effects of maternal depression and anxiety
onfetal-neonatalgrowthoutcomesandtrajectoriesremain
unclear.Moreover,thereisalackofstudiesthathave
simul-taneouslyaddressedtheindependentlongitudinaleffectof
maternaldepression andanxietyonfetal-neonatalgrowth
trajectories.Thisstudyaimedtosimultaneouslyanalyzethe
effectofmaternal prenataldepression andanxietyon(1)
neonataloutcomes,and(2),onfetal-neonatalgrowth
tra-jectories,fromthe2ndtrimesterofpregnancytochildbirth.
Method
Participants
The sample wascomprised of 172 mothers recruitedat a public health service in Northern Portugal during the 1st trimesterofpregnancy(8---14gestationalweeks).Inclusion criteriawere:abletoreadandwriteinPortuguese;resident inPortugalforatleastoneyear;atmost14weekspregnant; and,singletongestationswithoutmedicaland/orobstetric complications. Fromthe 172 mothers whocompleted the 1stmomentofassessment,88.4%(n=152)completedallthe threemomentsofassessment.
Procedures
Thisstudywasconductedinaccordancewiththe Declara-tionofHelsinkiandwaspreviouslyapprovedbytheethics committeesof all institutions involved. Women willing to participate provided written informed consent, after an explanationof the study aimsandprocedures. This study hadalongitudinaldesignwiththreeassessmentmoments: 2nd trimester of pregnancy (20---24 gestational weeks), 3rd trimester of pregnancy (30---34 gestational weeks), and childbirth (1---3 postnatal days). Mothers repeatedly completed a measure of depression and anxiety. Obstet-ricrecords and fetaland neonatalbiometrical datawere collected from clinical reports during the 2nd and 3rd trimesterof pregnancy,andat childbirth. Toavoid poten-tialerrors associatedwithestimated age, gestationalage wasestimatedbasedonmothers’lastmenstrualperiodand confirmedusingultrasoundmeasurements.
Measures
Socio-demographicandobstetricinformationwasobtained usingasocio-demographicquestionnaire. Toassess mater-nal depression, the Portuguese version of the Edinburgh
PostnatalDepressionScale(EPDS)21,22wasused.TheEPDSis
aself-reportedscalecomposedoftenitemsonafour-point
Likert scale.A cutoffpoint of10wassuggested toscreen
fordepressioninPortuguesewomen.22Severalstudieshave
usedthisscaleinwomenduringpregnancyandthe
postna-talperiod.18---20 ThePortugueseversionoftheEPDSshowed
goodinternal consistency inwomenduring pregnancyand
the postnatal period (˛=0.85).18,22 In the present study,
Cronbach’salphacoefficientsrangedfrom0.84to0.85.
To assess maternal anxiety, the Portuguese version of
the State-TraitAnxiety Inventory(STAI)23,24 wasused.The
STAIiscomposedoftwosubscales:onetoassessanxietyas
anemotional state(STAI-S)andanothertoassessthetrait
of anxiety (STAI-T), each containing20 items scored ona
four-pointLikertscale.Acutoffpointof45wassuggested
toscreenfor highanxietyinPortuguese women.24 Several
studieshaveusedthismeasureinwomenduringpregnancy
andthepostnatalperiod.18,19ThePortugueseversionofthe
STAI-S showed goodinternal consistency in women during
pregnancyandthepostnatalperiod(˛rangedfrom0.87to
0.93).24Inthepresentsample,Cronbach’salphacoefficients
ofSTAI-Srangedfrom0.89to0.93.
Toassessfetalgrowth,estimatedfetalweight(measured
ingrams)wasobtainedfromtheobstetricultrasoundsatthe
2ndand3rdtrimestersofpregnancy.Thesemeasureswere
obtainedfollowingastandardclinicalmeasurement
proto-colby an obstetrician fromtheresearchteam. Estimated
fetalweightwascalculatedusingtheHadlockformula.25
To assess neonatalgrowth outcomes, neonatalweight,
length (measured in centimeters), ponderal index
(100× [weight/length3]), and gestational age at birth
(measuredinweeks)werecollectedfrommedicalreports.
These measures were suggested by previous research as
majormarkersoffetal-neonatalgrowthandoutcomes.18---20
Dataanalysisstrategy
To simultaneouslyanalyzetheeffectofmaternal prenatal depression and anxiety onneonataloutcomes, a two-way multivariate analysis of covariance (MANCOVA) was per-formed. In the model, maternal prenatal depression and anxiety (meanof thescores at the 2ndand3rd trimester of pregnancy; coded as0=EPDS<10 and 1=EPDS≥10 for
depression; 0=STAI-S<45 and 1=STAI-S≥45 for anxiety)
wereincludedasindependentvariablesandneonatalgrowth outcomes(weight,length,ponderalindex,andgestational ageatbirth)asdependentvariables.Themother’sweight before pregnancy and tobacco and coffee consumption during pregnancy were included as covariates. The two-way MANCOVAwas performed using SPSS (IBM Corp; SPSS StatisticsforWindows,version23.0.USA).Theeffectsize, measured aspartial eta squared (p2),waspresented for
thetwo-wayMANCOVAresults.
anxiety symptoms (STAI-S scores) wereexamined at each assessmentmoment.Fixedeffectsformaternaldepressive and anxiety symptoms (time-varying effects centered on their grand means) were included in the model. Two dif-ferent models were performed (the unconditional model andthemodelwithpredictors).Themother’sweightbefore pregnancyandtobaccoandcoffeeconsumptionduring preg-nancywereincluded ascovariates.Significant interactions wereinterpretedandgraphedusingonestandarddeviation above and below the grand mean of the predictor varia-blesashighandlowvalues.Adeviancedifferencetestwas performedbetweentheunconditionalmodelandthemodel withpredictors toexaminemodelfitimprovements.GCMs wereperformed in apairwise person-perioddatasetusing SPSSversion23.0(SPSSInc.,UnitedStates).The resulting data consisted of 516 potential observations(172 partici-pantsbythreetimepoints).Theeffectsizerwasestimated forallsignificanteffects.
Results
Nearly all the mothers were Portuguese (92.1%), white (94.8%), married or cohabiting (86.8%), and living with a partner (86.2%). More than half were aged between 18 and 29 years old (M=27.69, SD=5.82), were of medium-low or low socio-economic level (62.0%), were employed (67.1%),and hadbetweennine and12yearsof education (54.5%).Additionally,morethanahalfofthemotherswere primiparous (52.1%) and had an eutocic delivery (with or withoutepidural;56.3%).Themajorityreportednotobacco consumption during pregnancy (83.8%), more than a half reportednocoffee consumption (70.7%),and allreported noalcoholanddrugconsumptionduringpregnancy.
Morethanahalfoftheneonatesweremales(56.3%)and bornwithalength≥50cm(63.5%).Themajoritywerenot
reanimated at birth (94.0%),born witha weightbetween 2500and4199g(91.0%),aponderalindex≥2.50(81.2%),a
gestationalage atbirthof≥37weeks(95.8%),andhadan
Apgar scorebetween 7 and10 at the1st (92.6%)and 5th minute(98.8%),respectively(Table1).
Noassociationsanddifferenceswerefoundbetweenthe
mothers that completed and did not complete the three
assessment moments, regarding mothers’ and neonates’
variables.
Additionally,noassociationsanddifferenceswerefound
betweenthemothersthatcompletedanddidnotcomplete
thethreeassessmentmomentsinallthestudyvariablesat
eachmomentofassessment.
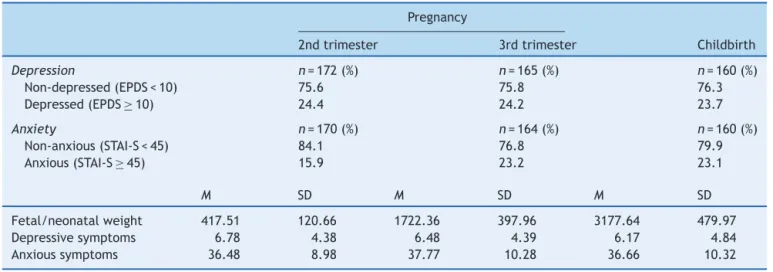
Descriptive statistics for all study variables at each
assessment were performed (Table2). Significant
associa-tionswerefoundamongthestudyvariablesatthebaseline
(r ranging from−0.289, p<0.05, to 0.652, p<0.001). No
association wasfoundbetween fetalweightandmaternal
depressivesymptomsatthebaseline.
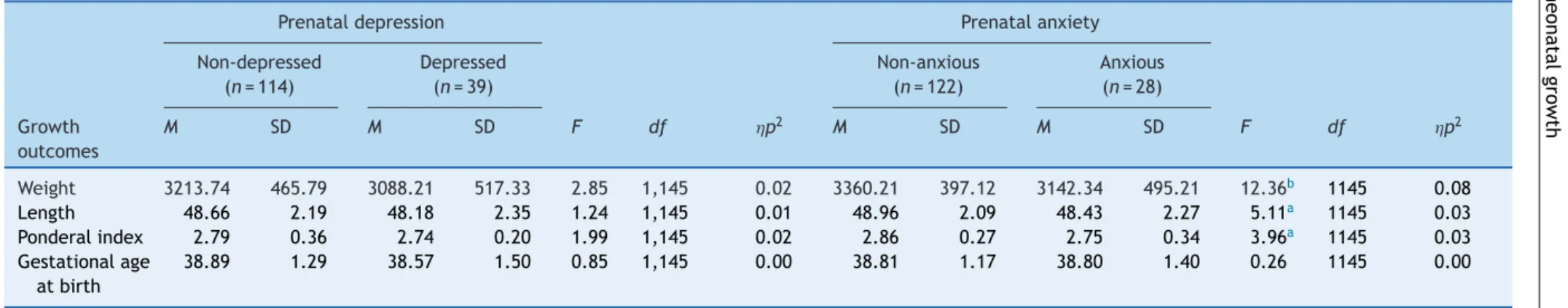
Theeffectsofmaternalprenataldepressionand
anxietyonneonatalgrowthoutcomes
The two-way MANCOVA revealed significant multivariate effects of maternal prenatal anxiety on neonatal growth outcomes,Wilk’s Lambda=0.91, F(4,142)=3.29, p=0.013,
Table1 Mothers’obstetricandsocio-demographic charac-teristicsandneonates’biometricdata.
Mothers
n=172(%)
Age(years) 15---17 4.8 18---29 51.5 30---41 43.7 Socio-economic
level
High 15.7
Medium-high 4.7 Medium 17.6 Medium-low 22.2
Low 39.8
Professional status
Employed 67.1 Unemployed 25.7 Household/student 7.2 Education(in
years)
<9 27.5 9---12 54.5 >12 18.0 Parity Primiparous 52.1 Multiparous 47.9 Deliverytype Eutocic 56.3 Dystocic 43.7 Tobacco
consumption
Yes 16.2
No 83.8
Coffee consumption
Yes 29.3
No 70.7
Neonates
n=168(%)
Sex Male 56.3
Female 43.7 Reanimation Yes 6.0
No 94.0
Weight(g) <2500 6.6 2500---4199 91.0
≥4200 2.4
Length(cm) <50 63.5
≥50 36.5
PonderalIndex <2.50 18.8
≥2.50 81.2
Gestationalage atbirth (weeks)
<37 4.2
≥37 95.8
p2=0.09. Results revealed significant univariate effects
Table2 Descriptivestatisticsofstudyvariablesacrosstime.
Pregnancy
2ndtrimester 3rdtrimester Childbirth
Depression n=172(%) n=165(%) n=160(%)
Non-depressed(EPDS<10) 75.6 75.8 76.3 Depressed(EPDS≥10) 24.4 24.2 23.7
Anxiety n=170(%) n=164(%) n=160(%)
Non-anxious(STAI-S<45) 84.1 76.8 79.9 Anxious(STAI-S≥45) 15.9 23.2 23.1
M SD M SD M SD
Fetal/neonatalweight 417.51 120.66 1722.36 397.96 3177.64 479.97 Depressivesymptoms 6.78 4.38 6.48 4.39 6.17 4.84 Anxioussymptoms 36.48 8.98 37.77 10.28 36.66 10.32
M,mean;SD,standarddeviation;EPDS,EdinburghPostnatalDepressionScale;STAI-S,stateanxietyinventory.
Nosignificantmultivariateeffectsofprenatalmaternal depressionwerefoundonneonatalgrowthoutcomes,Wilk’s Lambda=0.95,F(4,142)=1.92,p=0.110,p2=0.05.
Theeffectsofmaternaldepressionandanxietyon
fetal-neonatalgrowthtrajectories,fromthe2nd
trimesterofpregnancytochildbirth
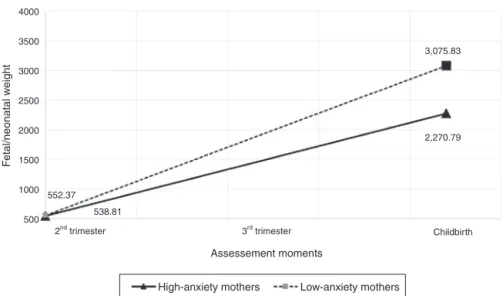
The main effects over timewere found onfetal-neonatal weight, b=96.71, SE=1.71, 95% CI=[93.33, 100.08],
p<0.001, effect size r=0.95. From the 2nd trimester of pregnancytochildbirth,fetal-neonatalweightincreased,on average,97gperweek.Additionally,interactioneffectsof anxietysymptomsandtimewerefound,b=2.65,SE=0.10, 95%CI=[2.45,2.86],p<0.001,effectsizer=0.86. Fetuses-neonatesofhigh-anxietymothersshowedalowerincrease ofweightfromthe2ndtrimesterofpregnancytochildbirth thanfetuses-neonatesoflow-anxiety mothers(Fig.1).No
maineffectsofmaternalanxietysymptomswerefoundon
fetalweight.
No main effects of maternal depressive symptoms
were found on fetal weight. Likewise, no effects of
the interaction between maternal depressive symptoms
and time, and no effects of the interaction between
maternal depressive symptoms, maternal anxiety
symp-toms,andtimewerefound. Interceptandrandomeffects
(intercept+time; residuals) were statistically significant
(all values of p<0.001). The deviance difference test
showedthat themodel withpredictors (maternal
depres-siveandanxietysymptoms)providedagoodfittothedata,
2(5)=138.87,p<0.001.
Discussion
Simultaneously considering the effect of maternal prena-taldepressionandanxiety,asignificantindependenteffect ofprenatalmaternal anxietywasfoundonmajormarkers ofneonatalgrowthoutcomes.Neonatesofprenatally anx-ious mothers showed lower weight, length, and ponderal
indexatbirththanneonatesofprenatallynon-anxious moth-ers. These results are consistent withprior research that found that neonates of anxious mothers were born with lowerweight,length,andponderalindex.2Moreover,
simul-taneously considering maternal depression and anxiety, a
significantinteractioneffectofmaternalanxietysymptoms
and time wasfound on a major markerof fetal-neonatal
growth.Thisresultsuggestedaneffectofmaternalanxiety
symptoms onfetal-neonatalweighttrajectories, fromthe
2ndtrimesterofpregnancytochildbirth.Fetuses-neonates
ofanxiousmothersshowedalowerincreaseofweight,from
the2ndtrimesterofpregnancytochildbirth,than
fetuses-neonates of non-anxious mothers. These findings suggest
thatmaternal anxietynegatively affectthismajormarker
of normativefetal-neonatal growthtrajectories, fromthe
prenatal period to childbirth, even when simultaneously
considering the effectof maternal depression.This result
is consistent with previous research that found a lower
increaseof weightin fetuses-neonatesof anxiousmothers
thaninfetuses-neonatesofnon-anxiousmothersfrom
preg-nancytochildbirth.18,19
Severalunderlyingmechanismshavebeen suggestedto
explain the effect of maternal anxiety on fetal-neonatal
growth. Epigenetic mechanisms have been proposed as
possiblemediatorsoftheprenatalanxietyeffecton
fetal-neonatal growth. Studies have suggested that prenatal
anxiety can permanently alter fetal physiology, namely
hyperactivationofthefetalhypothalamicpituitaryadrenal
(HPA)axis.26,27 Literaturehasalso suggestedthe mother’s
HPAhyperactivationasamediatorofthematernalprenatal
anxiety effect on fetal-neonatal growth.28 Prenatal
anxi-ety could be a stressor for pregnant women, stimulating
the HPA-axis to produce higher levels of glucocorticoids.
Maternal glucocorticoids can be transduced to the fetus
by transplacental transport andby stress-induced release
of placental hormones into fetal circulation. Increased
fetal cortisol contributes to the maturation of organ
systemsrequiredforextra-uterinesurvival.However,
exces-sive levels of feto-placental glucocorticoid may result in
intrauterinegrowthrestriction.28 Further,maternal
depression
and
anxiety
,
fetal-neonatal
growth
457
Table3 Theeffectofmaternalprenataldepressionandanxietyonneonatalgrowthoutcomes.
Prenataldepression Prenatalanxiety Non-depressed Depressed Non-anxious Anxious
(n=114) (n=39) (n=122) (n=28) Growth
outcomes
M SD M SD F df p2 M SD M SD F df p2
Weight 3213.74 465.79 3088.21 517.33 2.85 1,145 0.02 3360.21 397.12 3142.34 495.21 12.36b 1145 0.08
Length 48.66 2.19 48.18 2.35 1.24 1,145 0.01 48.96 2.09 48.43 2.27 5.11a 1145 0.03
Ponderalindex 2.79 0.36 2.74 0.20 1.99 1,145 0.02 2.86 0.27 2.75 0.34 3.96a 1145 0.03
Gestationalage atbirth
38.89 1.29 38.57 1.50 0.85 1,145 0.00 38.81 1.17 38.80 1.40 0.26 1145 0.00
M,mean;SD,standarddeviation.
Note:Mother’sweightbeforepregnancyandtobaccoandcoffeeconsumptionduringpregnancywereincludedascovariates. a p<0.05.
4000
3500
3000
2500
2000
1500
1000
500
2nd trimester 3rd trimester
Assessement moments
F
etal/neonatal w
eight
Childbirth
High-anxiety mothers Low-anxiety mothers
552.37 538.81
3,075.83
2,270.79
Figure1 Estimatedweighttrajectoriesforfetuses-neonatesofhigh-anxietyandlow-anxietymothers.
intakeandlowintakeofessentialvitaminsandfattyacids (e.g.,folicacid,vitaminB12).29
Majorconcernsaboutlowbirthweight,length,and
pon-deralindexemergedduetotheirnegativeeffectoninfant
health,associatedwithhigherperinatalmortality:
mechan-ical ventilation, supplemental oxygen support, later oral
feeding, retinopathy, bronchopulmonary dysplasia,
pneu-mothorax,intraventricularhemorrhage,andotherpediatric
complications.30 Moreover, more developmental problems
wereidentifiedinlowbirthweightneonates,including
prob-lemsofattention, cognition,andneuromotorfunctioning,
andincreasingtheriskofearlychildhoodmorbidity.30
Some limitations shouldbe pointed out.The voluntary
natureofthe participationinthe studymay havelead to
a selection bias. Mothers who agreed to participate and
completed all moments of assessment may be those who
feelmoresatisfiedandinvolvedwiththepregnancy
expe-rience.However, nodifferences were found between the
participantswho completedand did notcomplete allthe
momentsofassessment.Ahighersamplesizemightincrease
thestatisticalpoweroftheanalysis.Astandardizedclinical
interviewtoassess depression and anxiety couldincrease
thevalidityoftheresults.However,bothmeasuresshowed
goodinternalconsistency.Unmeasuredconfoundingfactors
mayhaveinfluencedtheeffectsdescribed.However,some
ofthesefactors(mother’sweightbeforepregnancy,tobacco
andcoffeeconsumptionduringpregnancy)werecontrolled
intheanalysis.
This study demonstrates the independent longitudinal
effect of maternal anxiety on major markers of
fetal-neonatalgrowthoutcomesandtrajectories,simultaneously
considering the effect of maternal depression and
anxi-ety. This highlights an increased necessity of systematic
screeningforanxietyduringpregnancy.Thesefindingsalso
suggested that fetuses of anxious mothers are those who
might benefit from individualized care in neonatal care
units.
Suggestionstofutureresearchcanbeindicated.Future
studies could simultaneously explore the independent
effects of both maternal depression and anxiety on
other markers of fetal-neonatal growth, behavior, and
maturation. Futureresearchcouldalso explorethe
medi-atorroleofepigeneticandendophenotypicmechanismson
the effectof maternal prenatalanxiety on fetal-neonatal
growthoutcomesandtrajectories.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgments
ThisstudywasconductedatthePsychologyResearchCenter (UID/PSI/01662/2013),University ofMinho,andsupported by the Portuguese Foundation for Science and Technol-ogyand thePortuguese Ministryof Education andScience throughnational funds andco-financed by FEDERthrough COMPETE2020 under the PT2020 Partnership Agreement (POCI-01-0145-FEDER-007653). This study was also sup-portedby FEDERFundsthroughthe ProgramaOperacional Factores deCompetitividade --- COMPETE and by National FundsthroughFCT---Fundac¸ãoparaaCiênciaeaTecnologia undertheprojectPTDC/SAU/SAP/116738/2010.
References
1.AnderssonL,Sundström-PoromaaI,WulffM,AströmM,BixoM. Implicationsofantenataldepressionandanxietyforobstetric outcome.ObstetGynecol.2004;104:467---76.
2.Field T, Diego M, Hernandez-Reif M, Schanberg S, Kuhn C, YandoR, et al. Pregnancy anxiety and comorbid depression andanger:effectsonthefetusandneonate.DepressAnxiety. 2003;17:140---51.
3.BeukeCJ,FischerR,McDowallJ.Anxietyanddepression:why andhowtomeasuretheirseparate effects.ClinPsycholRev. 2003;23:831---48.
5.Diego MA, Field T, Hernandez-Reif M, Schanberg S, Kuhn C,Gonzalez-Quintero VH. Prenataldepression restricts fetal growth.EarlyHumDev.2009;85:65---70.
6.DieterJN,FieldT,Hernandez-ReifM,JonesNA,LecanuetJP, SalmanFA,etal.Maternaldepressionandincreasedfetal activ-ity.JObstetGynaecol.2001;21:468---73.
7.AllisterL, Lester BM,CarrS, LiuJ. Theeffects ofmaternal depressiononfetalheartrateresponsetovibroacoustic stimu-lation.DevNeuropsychol.2001;20:639---51.
8.FuJ,YangR,MaX,XiaH.Associationbetweenmaternal psy-chological status and fetal hemodynamic circulation in late pregnancy.ChinMedJ(Engl).2014;127:2475---8.
9.MonkC,Myers MM,SloanRP,EllmanLM,Fifer WP.Effectsof women’sstress-elicitedphysiologicalactivityandchronic anxi-etyonfetalheartrate.JDevBehavPediatr.2003;24:32---8. 10.DiPietroJA, Costigan KA, Gurewitsch ED. Fetal response to
inducedmaternalstress.EarlyHumDev.2003;74:125---38. 11.FieldT,DiegoM,DieterJ,Hernandez-ReifM,SchanbergS,Kuhn
C,etal.Prenataldepressioneffectsonthefetusandthe new-born.InfBehavDev.2004;27:216---29.
12.HoffmanMC,MazzoniSE,WagnerBD,LaudenslagerML,RossRG. Measuresofmaternalstressandmoodinrelationtopreterm birth.ObstetGynecol.2016;127:545---52.
13.MartiniJ,KnappeS,Beesdo-BaumK,LiebR,WittchenHU. Anx-ietydisordersbefore birthandself-perceived distress during pregnancy:associationswithmaternaldepressionand obstet-ric,neonatal and earlychildhood outcomes.EarlyHum Dev. 2010;86:305---10.
14.FieldT,DiegoM,DieterJ,Hernandez-ReifM,SchanbergS,Kuhn C,etal.Depressedwithdrawnandintrusivemothers’effectson theirfetusesandneonates.InfantBehavDev.2001;24:27---39. 15.AshmanSB,DawsonG,PanagiotidesH,YamadaE,WilkinsonCW.
Stresshormonelevelsofchildrenofdepressedmothers.Dev Psychopathol.2002;14:333---49.
16.CarterJD,MulderRT,BartramAF,DarlowBA.Infantsina neona-talintensivecareunit:parentalresponse.ArchDisChildFetal NeonatalEd.2005;90:F109---13.
17.Davis EP, Sandman CA. The timing of prenatal exposure to maternal cortisol and psychosocial stress is associ-ated with human infant cognitive development. Child Dev. 2010;81:131---48.
18.CondeA,FigueiredoB,TendaisI,TeixeiraC,CostaR,PachecoA, etal.Mother’sanxietyanddepressionandassociatedrisk fac-torsduringearlypregnancy:effectsonfetalgrowthandactivity at20---22 weeksofgestation. JPsychosom ObstetGynaecol. 2010;31:70---82.
19.Henrichs J, Schenk JJ, Roza SJ, van den Berg MP, Schmidt HG, Steegers EA, et al. Maternal psychological distress and
fetalgrowthtrajectories:theGenerationRStudy.PsycholMed. 2010;40:633---43.
20.HompesT, VriezeE,FieuwsS,SimonsA, JaspersL, Van Bus-selJ,etal.Theinfluenceofmaternalcortisolandemotional state duringpregnancyon fetal intrauterine growth.Pediatr Res.2012;72:305---15.
21.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Developmentofthe10-item Edinburgh Postnatal DepressionScale.BrJPsychiatry.1987;150:782---6.
22.AreiasME,KumarR,BarrosH,FigueiredoE.Comparative inci-dence of depression in women and men, during pregnancy and after childbirth. Validation of the Edinburgh Postna-talDepression Scalein Portuguesemothers. Br JPsychiatry. 1996;169:30---5.
23.BiaggioAM,NatalicioL,SpielbergerCD.Thedevelopmentand validation ofanexperimental Portugueseform ofthe State-TraitAnxiety Inventory. In: SpielbergerCD, Dias-Guerrero R, editors.Cross-culturalresearchonanxiety.Washington,D.C.: Hemisphere/Wiley;1976.p.29---40.
24.SpielbergerCD,GorsuchRL,LusheneR, VaggPR,JacobsGA. Manualforthestate-traitanxietyinventory.PaloAlto: Consul-tingPsychologistsPressInc.;1983.
25.HadlockFP,HarristRB,CarpenterRJ,DeterRL,ParkSK. Sono-graphicestimationoffetalweight.Thevalueoffemurlength in addition to head and abdomen measurements. Radiology. 1984;150:535---40.
26.Palma-Gudiel H, Córdova-Palomera A, Eixarch E, Deuschle M,Fa˜nanás L. Maternalpsychosocialstress duringpregnancy alterstheepigeneticsignatureoftheglucocorticoidreceptor genepromoterintheiroffspring:ameta-analysis.Epigenetics. 2015;10:893---902.
27.HompesT,IzziB,GellensE,MorreelsM,FieuwsS,PexstersA, etal.Investigatingtheinfluenceofmaternalcortisoland emo-tionalstateduringpregnancyontheDNAmethylationstatusof theglucocorticoidreceptorgene(NR3C1)promoterregionin cordblood.JPsychiatrRes.2013;47:880---91.
28.Wadhwa PD, Garite TJ, Porto M, Glynn L, Chicz-DeMet A, Dunkel-SchetterC,etal.Placentalcorticotropin-releasing hor-mone (CRH), spontaneous preterm birth, and fetal growth restriction:aprospectiveinvestigation.AmJObstetGynecol. 2004;191:1063---9.
29.EmmettPM,JonesLR, GoldingJ. Pregnancydietand associ-atedoutcomesintheAvonLongitudinalStudyofParentsand Children.NutrRev.2015;73:154---74.