w w w . j c o l . o r g . b r
Journal
of
Coloproctology
Original
Article
Association
between
vitamin
D
deficiency
and
anemia
in
inflammatory
bowel
disease
patients
with
ileostomy
Andre
Fialho
a,
Andrea
Fialho
a,
Gursimran
Kochhar
b,
Bo
Shen
b,∗ aDepartmentofInternalMedicine,TheClevelandClinicFoundation,Cleveland,UnitedStatesbDepartmentofGastroenterologyandHepatology,TheClevelandClinicFoundation,Cleveland,UnitedStates
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received13May2015
Accepted8June2015
Availableonline2July2015
Keywords:
Anemia Ileostomy
VitaminDdeficiency
a
b
s
t
r
a
c
t
Background:VitaminDdeficiencyiscommonlyseeninpatientswithinflammatorybowel
disease(IBD).VitaminDdeficiencyinIBDpatientswithileostomyhasnotbeensystemically
studied.Theaimofthestudywastoassessthefrequencyandriskfactorsassociatedwith
low25(OH)D3levelsinthosepatients.
Methods:112eligibleIBDpatientswithileostomywerestudied.Demographic,clinical,and
endoscopicvariableswereanalyzed.VitaminDlevelsbeforeandafterileostomywere
com-paredwhenavailable.Levelsofserum25(OH)D3<20ng/mLwereclassedasbeingdeficient.
Results:112 eligible ileostomy patients were included. The mean vitamin D level was
21.47±1.08ng/dl.LowlevelsofvitaminD(<30ng/dl)werepresentin92patients(82%).
Vita-minDdeficiency(<20ng/dL)wasseenin55patients(49%).Therewasnodifferencebetween
patientswithorwithoutvitaminDdeficiencyregardingdemographicvariables,medication
useanddurationofileostomy.Neo-ilealinflammationonendoscopywasnotassociated
withvitaminDdeficiency(p=0.155).Lowerlevelsofphosphorus(p=0.020)orhemoglobin
(p=0.019)andshorterdurationofIBD(p=0.047)werefoundinpatientswithvitaminD
deficiency.Inmultivariateanalysis,lowerlevelsofphosphorus(oddsratio[OR]:1.83,95%
confidenceinterval[CI]:1.16–2.89,p=0.009)andhemoglobin(OR:1.32,95%CI:1.08–1.60,
p=0.006)remainedsignificantlyassociatedwithvitaminDdeficiency.
Conclusion: VitaminDdeficiencyiscommoninIBDpatientswithileostomyandisassociated
withlowhemoglobinlevels.FurtherstudiesareneededtoevaluatevitaminD
supplemen-tationasapossibleadjuvantinthetreatmentofanemiaofchronicdiseaseinIBDpatients.
©2015SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.All
rightsreserved.
∗ Correspondingauthor.
E-mail:shenb@ccf.org(B.Shen).
http://dx.doi.org/10.1016/j.jcol.2015.06.004
Associac¸ão
entre
deficiência
de
vitamina
D
e
anemia
em
pacientes
com
doenc¸a
inflamatória
intestinal
submetidos
a
ileostomia
Palavras-chave:
Anemia Ileostomia
DeficiênciadeVitaminaD
r
e
s
u
m
o
Introduc¸ão: AdeficiênciadevitaminaDempacientescomdoenc¸ainflamatóriaintestinal
submetidosaileostomianãofoiestudadasistematicamente.Oobjetivodesseestudofoi
avaliarafrequênciaeosfatoresderiscoassociadoscomadeficiênciadevitaminaDnesses
pacientes.
Resultados: 112pacienteselegíveisforam incluídos.Amédia dosníveisde vitaminaD
napopulac¸ãoestudadafoide21.47±1.08ng/dl.NíveisdevitaminaDabaixodonormal
(<30ng/dl)edeficiênciadevitaminaD(<20ng/dL)foramencontradosem92pacientes(82%)
eem55pacientes(49%)respectivamente.Encontrou-seumaassociac¸ãoentredeficiência
devitaminaDeníveismaisbaixosdefosforo(p=0.020),hemoglobina(p=0.019)edurac¸ão
dadoenc¸ainflamatóriaintestinal(p=0.047).Naanálisemultivariada,níveismaisbaixosde
fósforo(oddsratio[OR]:1.83,95%confidenceinterval[CI]:1.16–2.89,p=0.009)ehemoglobina
(OR:1.32,95%CI:1.08–1.60,p=0.006)permaneceramassociadoscomdeficiênciadevitamina
D.
Conclusão: AdeficiênciadevitaminaDécomumempacientescomdoenc¸ainflamatória
intestinal submetidosaileostomiae estáassociadacomníveisbaixosdehemoglobina.
Maisestudossãonecessáriosparaavaliarseasuplementac¸ãodevitaminaDpodeserum
adjuvantenotratamentodeanemiadadoenc¸acrônicanessespacientes.
©2015SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda.
Todososdireitosreservados.
Introduction
Vitamin D is a steroid hormone responsible for calcium
hemostasis and metabolism. It also has
immunoregula-tory functions and anti-inflammatory effects.1 The main
source of vitamin D derives from the conversion of
7-dehydrocholesterol in the skin to cholecalciferol (D3) by
sunlight.VitaminDisalsoacquired fromthedietandit is
absorbedintheduodenumandjejunum.Asaliposoluble
vita-min,itdependsonbileacidsforitsabsorption.Thebileacid
poolismaintainedbytheenterohepaticcirculationandrelays
ontheabsorptionofbileacidsintheterminalileum.
VitaminDdeficiencyiscommonworldwide.IntheUnited
States, the reported frequency of vitamin D deficiency is
18–40%inadultfemalesand11–26%inadultmales,with
vari-ationdependingonage,seasonandgeographicallocation.2
Vitamin D deficiency has a significant impact on health,
includinglowbonemineraldensity,increasedriskoffractures
andfalls.3Inaddition,adequatebloodvitaminDlevelsand
intakeofvitaminDmaydecreasetheriskofcancer,4typeI
diabetes,5multiplesclerosis6andrheumatoidarthritis.7
LowvitaminDlevelsarecommoninpatientswith
inflam-matory bowel disease (IBD), occurring in 45–63% of the
patients.8,9 ThemechanismsforvitaminDdeficiencyinIBD
patientsare multifactorial.PatientswithIBDaresubject to
surgery,particularlyilealresectionforCrohn’sdisease,and
maybeatincreasedriskofvitaminDdeficiency.IBDpatients
oftenrequiresurgeryduringthecourseoftheirdisease10and
ileostomyisperformed in asubset ofpatients withCD or
ulcerativecolitis(UC).11
Surgicalproceduressuchasileostomymayposean
addi-tionalriskforvitaminDdeficiencyinIBDpatients.Studies
evaluatingtheratesandassociatedriskfactorsofvitaminD
deficiencyinthispopulationarelacking.Thustheaimsofthis
studyweretoevaluatethefrequencyofvitaminDdeficiency
inIBDpatientswithanileostomyandtoidentifyriskfactors
forvitaminDdeficiencyinthesepatients.
Patients
and
methods
Patients
ThisstudywasapprovedbytheClevelandClinicInstitutional
Review Board (IRB). Three hundred IBD patients with
per-manent ileostomy were retrospectively identified from the
electronicmedicalrecords.Atotalof112patientswithIBD
andatleastoneserum25(OH)D3levelaftertheconstructionof
ileostomywereincludedinthestudy.Inclusioncriteriawere:
(1) diagnosisofIBD;(2)thepresenceofpermanent or
tem-poraryileostomy;and(3)atleastoneserum25(OH)D3 level
measuredaftertheostomy.Exclusioncriteriawereileostomy
forbowelmalignancyorforfamilialadenomatouspolyposis
oretiologiesotherthanIBD.
Variables
Atotalof32demographic,clinicalandendoscopicvariables
were studied.Demographic variables included age, gender,
race,bodymassindex(BMI),smokingstatusandgeographical
location(Northvs.South).TheNorthernlocationwasdefined
aslocationabovethelatitudeof37degreesNorth.The
South-ernlocationwasdefinedasalocationbelowthelatitudeof37
Thefollowingclinicalvariableswereincluded:durationof
disease,duration ofdisease until submission to ileostomy,
duration of ileostomy, season when vitamin D was
mea-suredandclinicalindicationforileostomyandbloodlevels
of25(OH)D3,albumin,hemoglobin(Hb),calcium,parathyroid
hormone (PTH), alkaline phosphatase and C-reactive
pro-tein(CRP).Historyofuse ofcalcium supplements, vitamin
supplements,corticosteroid,immunomodulators,anti-tumor
necrosisfactor (TNF)biologics, antibiotics or non-steroidal
anti-inflammatorydrugs(NSAID)werealsoevaluated.
Endo-scopic variables included the presence or absence of any
mucosalinflammationonileoscopy.
Vitamin D status was assessed by measuringthe most
recent25(OH)D3level.VitaminDlevels≥30ng/mLwere
con-sidered normal. Alow vitamin D was definedas the level
below30ng/mL.LowvitaminDlevelswerefurthercategorized
intovitaminDinsufficiencywhenlevelswerebetween20and
29ng/dlandvitaminDdeficiencywhenlevelswerelessthan
20ng/dl.
Toevaluatethepresenceofanemia,themostrecentHb
levelwithin6monthsofvitaminDlevelmeasurementwas
takenintoaccount.AnemiawasdefinedasHb<12.0g/dLin
femalesandHb<13g/dLinmales.Thepresenceofiron
defi-ciencyanemia(IDA)andanemiaofchronicdisease(ACD)was
definedbased onserum ironlevels, transferrin,transferrin
saturationand ferritin.ThedefinitionofACDand IDAwas
asfollowsaccordingtoWeissandGoodough12:(1)transferrin
saturation<16%withnormalorelevatedserumferritin
lev-els(>100ng/mL)characterizedasACD;(2)lowlevelsofboth
transferrinsaturation(<16%)andserumferritin(<30ng/mL)
characterizedas IDA.Transferrinsaturation <16%,reduced
transferrinconcentration,andserum ferritin>30ng/mLbut
<100ng/mLcharacterizedamixedpatternofIDAandACD.
Outcomemeasurements
Theprimaryoutcomeswerethefrequencyandriskfactorsof
vitaminDdeficiencyinIBDpatientswithileostomy.
Statisticalanalysis
AllstatisticalanalyseswereperformedusingSPSSsoftware
version22(IBMCorp.,Armonk,NY).Mean±SDorn%wasused
topresentcontinuousvariables.Toidentifypotentialrisk
fac-torsforvitaminDdeficiency,univariableanalysiswasused.
Student’sttest(orWilcoxonranksumtestwhen
appropri-ate)wasusedforcontinuousvariables,whileChi-squaretest
(orFishersexact test, whenappropriate) wasused for
cat-egoricalvariables.Variablesthatwere significantly(p<0.05)
associatedwithvitaminDdeficiencyonunivariateanalysis
wereincluded inthemultivariateanalysis alongwith
vari-ablespreviouslyshownintheliteraturetoaffectvitaminD
levels.
Results
Atotalof112eligiblepatientswithIBDandileostomywere
includedinthisstudy,ofwhich107hadCD and5had UC.
Themeanageofthecohortstudiedwas53.4±1.3years(range
24–91years)and70(62.5%)patientswerefemales.Themean
duration of IBD diagnosis was 24.6±1.2 years (range 2–60
years) and the mean duration of ileostomy was 12.7±0.9
years(range2–45years).Themainindicationsforileostomy
inthecohortwerefailureofmedicaltherapyin90patients
(80.4%)andbowelobstructionin22(19.6%).Inthesubgroup
ofpatientswithUC,themainindicationforendileostomy
wascomplicationsoftheilealpouch(3/5).Fivepatientshad
temporaryileostomyand107hadpermanentileostomy.
FrequencyofvitaminDdeficiency
The mean vitamin D level of the whole cohort was
21.47±1.08ng/dl. Low vitamin D (<30ng/dl) levels were
presentin92(82.1%)patients.Thirty-sevenpatients(33.0%)
were classified as having vitamin D insufficiency (level
between20and29ng/dl)and55(49.1%)asvitaminDdeficiency
(<20ng/dl).
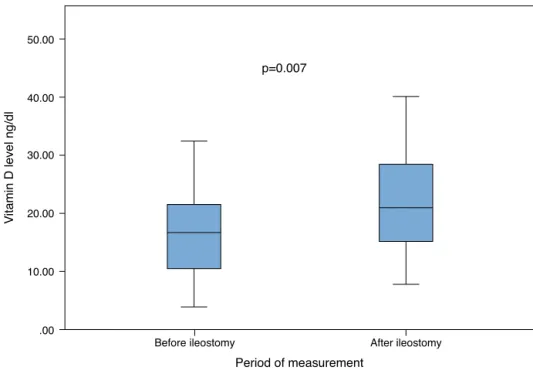
We performed a subanalysis of the trend of vitamin D
status before and after ileostomy, based on available data
in 26 (23.2%) of the 112 patients. The mean level of
vita-minDwassignificantlyhigherafterileostomycomparedto
beforeileostomy(22.4±1.8ng/dL,vs.17.5±1.8ng/dL,p=0.007)
asshowninFig.1.
UnivariateassessmentofriskfactorsforvitaminD deficiency
The112patientsweredividedintothosewithvitaminD
defi-ciency (<20ng/mL) and those without vitaminD deficiency
(>20ng/mL)toanalyzetheriskfactorsassociatedwithvitamin
Ddeficiency.
Intheunivariateanalysis,levelsofphosphoruswere
sig-nificantlylowerinthevitaminDdeficiencygroup(p<0.020).
NumericallylowerlevelsofcalciumandhigherlevelsofPTH
werealsofoundinthesepatientsalthoughthisdidnotreach
statisticalsignificance(Table1).
Inaddition,Hblevelsweresignificantlylowerinthe
vita-minDdeficiencygroup(p=0.019)(Table1).Atotalof47(42.0%)
ofthe112werefoundtohaveanemia,definedasHb<12ng/dL
infemalesandHb<13ng/dLinmales.Amongthe47patients
withdiagnosisofanemia,37hadironstudiesincludingiron
levels,transferrin,transferrinsaturationandferritin.ACDwas
detectedin21(63.6%)patients,IDAwasdetectedin6(18.2%)
patients andmixed patternanemia wasalsodetectedin6
(18.2%)patients.Nostatisticaldifferencewasfoundbetween
patientswithandwithoutvitaminDdeficiencyregardingthe
prevalenceofthedifferenttypesofanemia(ACDvs.IDAvs.
mixedpatternanemia)(p=0.204,Table1).
PatientswithvitaminDdeficiencyhadIBDdiagnosisfora
shorterperiodoftime(p=0.047),butnosignificantdifferences
werefoundneitherinthedurationofileostomy(p=0.080),the
intervalbetweenIBDdiagnosis(p=0.819)andileostomynor
thepresenceofinflammationonileoscopy(p=0.155)asshown
inTable1.
Therewasnodifferenceinage,gender,race,BMI,
smok-ing status, geographical location, season when vitamin D
was measured, albumin, alkaline phosphatase, CRP, the
use ofcalciumsupplements,vitaminsupplements,steroid,
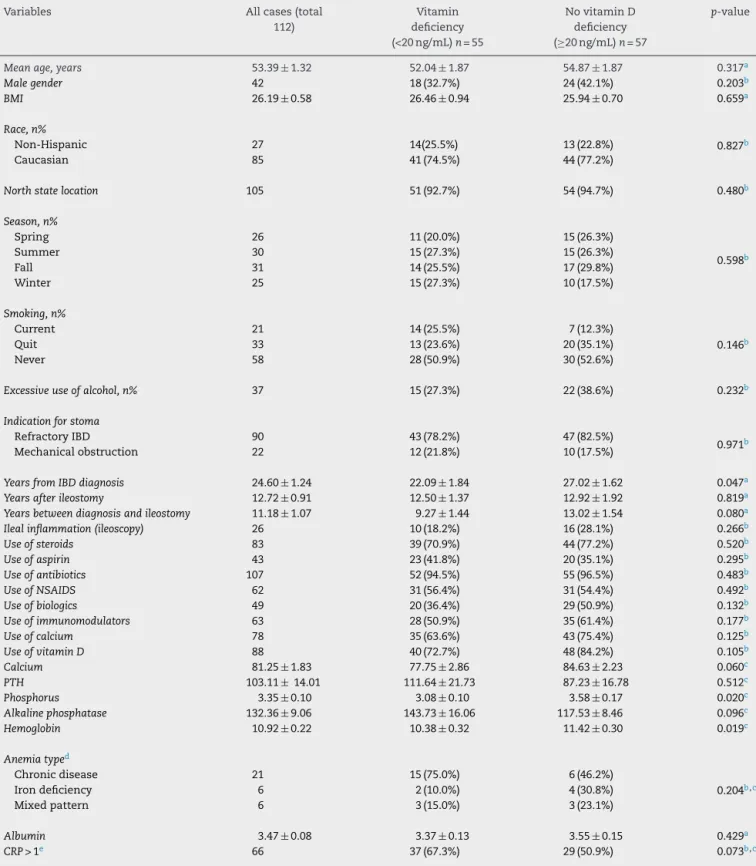
Table1–Demographic,clinical,endoscopicandhistologiccharacteristicsofileostomypatientswithandwithoutvitamin Ddeficiency.
Variables Allcases(total
112)
Vitamin deficiency (<20ng/mL)n=55
NovitaminD deficiency (≥20ng/mL)n=57
p-value
Meanage,years 53.39±1.32 52.04±1.87 54.87±1.87 0.317a
Malegender 42 18(32.7%) 24(42.1%) 0.203b
BMI 26.19±0.58 26.46±0.94 25.94±0.70 0.659a
Race,n%
Non-Hispanic 27 14(25.5%) 13(22.8%) 0.827b
Caucasian 85 41(74.5%) 44(77.2%)
Northstatelocation 105 51(92.7%) 54(94.7%) 0.480b
Season,n%
Spring 26 11(20.0%) 15(26.3%)
0.598b
Summer 30 15(27.3%) 15(26.3%)
Fall 31 14(25.5%) 17(29.8%)
Winter 25 15(27.3%) 10(17.5%)
Smoking,n%
Current 21 14(25.5%) 7(12.3%)
0.146b
Quit 33 13(23.6%) 20(35.1%)
Never 58 28(50.9%) 30(52.6%)
Excessiveuseofalcohol,n% 37 15(27.3%) 22(38.6%) 0.232b
Indicationforstoma
RefractoryIBD 90 43(78.2%) 47(82.5%)
0.971b
Mechanicalobstruction 22 12(21.8%) 10(17.5%)
YearsfromIBDdiagnosis 24.60±1.24 22.09±1.84 27.02±1.62 0.047a
Yearsafterileostomy 12.72±0.91 12.50±1.37 12.92±1.92 0.819a
Yearsbetweendiagnosisandileostomy 11.18±1.07 9.27±1.44 13.02±1.54 0.080a
Ilealinflammation(ileoscopy) 26 10(18.2%) 16(28.1%) 0.266b
Useofsteroids 83 39(70.9%) 44(77.2%) 0.520b
Useofaspirin 43 23(41.8%) 20(35.1%) 0.295b
Useofantibiotics 107 52(94.5%) 55(96.5%) 0.483b
UseofNSAIDS 62 31(56.4%) 31(54.4%) 0.492b
Useofbiologics 49 20(36.4%) 29(50.9%) 0.132b
Useofimmunomodulators 63 28(50.9%) 35(61.4%) 0.177b
Useofcalcium 78 35(63.6%) 43(75.4%) 0.125b
UseofvitaminD 88 40(72.7%) 48(84.2%) 0.105b
Calcium 81.25±1.83 77.75±2.86 84.63±2.23 0.060c
PTH 103.11±14.01 111.64±21.73 87.23±16.78 0.512c
Phosphorus 3.35±0.10 3.08±0.10 3.58±0.17 0.020c
Alkalinephosphatase 132.36±9.06 143.73±16.06 117.53±8.46 0.096c
Hemoglobin 10.92±0.22 10.38±0.32 11.42±0.30 0.019c
Anemiatyped
Chronicdisease 21 15(75.0%) 6(46.2%)
0.204b,c
Irondeficiency 6 2(10.0%) 4(30.8%)
Mixedpattern 6 3(15.0%) 3(23.1%)
Albumin 3.47±0.08 3.37±0.13 3.55±0.15 0.429a
CRP>1e 66 37(67.3%) 29(50.9%) 0.073b,c
BMI,bodymassindex;5ASA,5-aminosalicylicacid;NSAID,non-steroidalanti-inflammatorydrugs;PTH,parathyroidhormone.
a Thepvaluewascalculatedbyt-test. b Thepvaluewascalculatedbychi-squaretest.
c Somevariablesmayhavelessthan112duetomissingdata.
.00 10.00 20.00 30.00
V
itamin D level ng/dl
40.00 50.00
p=0.007
Period of measurement
After ileostomy Before ileostomy
Fig.1–BoxplotdistributionofvitaminDlevelsbeforeandafterileostomy(N=26).
non-steroidalanti-inflammatorydrugs(NSAID),betweenthe
studyandcontrolgroups(Table1).
MultivariateanalysisofriskfactorsforvitaminD deficiency
LowHb, low phosphoruslevel and shorterduration ofIBD
diagnosisweresignificantlyassociatedwithvitaminD
defi-ciencyintheunivariateanalysisandthuswereincludedinthe
multivariableanalysis.Whentheeffectofthesevariableswas
analyzedtogetherinthelogisticregression,lowHb(oddsratio
[OR]:1.32, 95% confidence interval [CI]: 1.08–1.60, p=0.006)
and low phosphorus (OR: 1.83, 95% CI: 1.16–2.89, p=0.009)
remainedindependentlyassociatedwithvitaminDdeficiency
(Table2).
Discussion
Inthisstudy,wefoundthatthelowvitaminDlevels(vitaminD
deficiencyorinsufficiency)werecommoninIBDpatientswith
ileostomy,with afrequency of82.1% (92/112). Surprisingly,
vitaminDstatusimprovedafterileostomy,whencompared
withpre-ileostomystatus,basedonthedatain26patients
with sequential measurements of serum vitamin D level.
VitaminD deficiencywasfoundtobeassociatedwith
ane-mia(p=0.009),suggestingthattheremaybealinkbetween
vitaminDdeficiencyandanemiainthesepatients.Inthe33
patientswhohadavailabledataforanemiatypeidentification,
ACDwasmoreprevalentinpatientswithvitaminDdeficiency
thancontrols(66.7%vs.33.3%),althoughthisfindingdidnot
reachstatisticalsignificance(p=0.204).Therewasno
associ-ationbetweenvitaminDdeficiencyandileuminflammation
onileoscopy(p=0.155).
LowvitaminDlevelsarecommoninpatientswithIBDin
general.7Upto63%ofpatientswithCDhavevitaminD
defi-ciency [39],whileinpatientswithUC vitaminDdeficiency
hasbeenshowntooccurin45%ofthecases.7InbothCDand
UC,severityofdiseasewasfoundtobeassociatedwith
vita-minDdeficiency.13,14SincevitaminDhasbeenshowntohave
anti-inflammatoryproperties,itslowerlevelmaypredispose
togreaterinflammationanddiseaseactivityinbothCDand
UC,creatingaviciouscircle.15,16 Ourstudyshowedthatthe
creationofanileostomymayhelpboostthelevelofserum
vitaminD,presumablyduetothebypassorresectionofthe
diseasedboweldownstream.
ThecauseofvitaminDdeficiencyinIBDpatientsappears
tobemultifactorial,includingdecreasedsunexposure17and
decreased dietary vitamin D intake due to the disease.18
In patients with CD, additional culprits are vitamin D
Table2–MultivariateanalysisofriskfactorsassociatedwithvitaminDdeficiencyinIBDpatientswithileostomy.
Variables OR CI p-value
Lowphosphorus 1.83 1.16–2.89 0.009
Lowhemoglobin 1.32 1.08–1.60 0.006
YearsfromIBDdiagnosis 1.04 1.00–1.07 0.051
malabsorptionand proteinlosing enteropathy causing loss
ofvitaminDbindingprotein.19Terminalileumresectionin
patientsCDhasalsobeenproposedasacontributorto
vita-minDdeficiencyduetodecreasedenterohepaticcirculation
ofbileacids.20
Surgical approach in patients with IBD such as end
ileostomyimposesadditionalmetabolicconsequencestoan
alreadyburdenedpopulation.InIBDpatientswithileostomy,
our group has previously shown a high prevalence oflow
bonemineraldensity,furthercomplicatedbyincreasedrisk
offractures.21TheremaybeanincreasedriskofvitaminB12
deficiencyinthesepatients,althoughthisseemstobemore
commonwhensignificantamountsofileumareresected.22
Inaddition,thereisanincreasedfecalexcretionof
choles-terolandbileacidsinpatientswithileostomy,whichhasbeen
showntoimprovecholesterolprofileinthesepatients,while
itmayfurtherimpairbileacidenterocirculation.23The
associ-ationbetweenvitaminDdeficiencyandanemia,ontheother
hand,hasnotbeenestablishedinthispopulation.
Toourknowledge,this isthefirst studyevaluating
vita-min D deficiency and its risk factors in IBD patients with
ileostomy.Kennedy et al.24 studiedcalcium metabolism in
49 patients with ileostomyand mentioned that the levels
ofvitaminDinthesepatientsvariedfrom21.4±9.5nmol/L
inthewinterto46.4±19.2nmol/Linthesummer.However,
riskfactorsforvitaminDdeficiencywerenotevaluated.In
thepresentstudy,vitaminDdeficiencywascommoninIBD
patients submitted to ileostomy.The exact
etiopathogene-sisforvitaminDdeficiency inIBDpatients withileostomy
isunknown.Wepostulatethatitmay berelated toaltered
intestinaltransittimeandilealresectioninthispopulation.
SomeIBDpatientswithileostomymayhaveextensive
inflam-mationorstrictures,whichleadstostasisoffecalcontentin
thesmallbowelandbacterialovergrowth.25Inturn,bacterial
overgrowthcausesdeconjugationofbileacidsanddecreases
theabsorptionoffatsolublevitaminssuchasvitaminD.26
IleostomywithilealresectioninCDmayleadtoimpairedbile
acidenterohepaticcirculation.InpatientswithilealCD,lower
vitaminDlevelsseemtobemorecommon.20
Tobetterunderstandtheexactburdenthatileostomyposes
towardvitaminDdeficiency,wecomparedthelevelsof
vita-minDbeforeandafterileostomyin26patientswithavailable
data. Surprisingly,the mean level ofvitaminDwas
signif-icantly lower before ileostomythan afterileostomy. These
findings may be a consequence of better disease control
orlessinflammationleadingtonutritionalimprovementin
IBDpatientsafterileostomy.Inaddition,aftersurgerythese
patientsmayhaveimprovedoralintakeandincreasedquality
oflifewithmoreoutdooractivity.
Interestingly,wefoundasignificantassociationbetween
lowvitaminDandHbinbothunivariableandmultivariate
analyses.Thisfinding,along withthe similaronereported
in patients with ileal pouch-anal anastomosis (IPAA),27
promptedourhypothesisthatthelinkbetweenvitaminD
defi-ciencyandanemiaisnotacoincidence.Thisassociationhas
notyetbeenstudiedinIBDpatientswithoutileostomyorIPAA.
Atotalof37patientshadavailablelaboratorydatatofurther
categorizethesubtypeofanemiaintoACD,IDAormixed
pat-tern.ACDwasthemostcommontypeofanemiainthecohort,
occurringin21patients(66.6%).AlthoughACDoccurredmore
frequentlyinpatientswithvitaminDdeficiency,thisdidnot
reachstatisticalsignificance(75.0%vs.46.2%,p=0.204),
prob-ablyduetothesmallsamplesize.
TheassociationofvitaminDdeficiencywithanemiahas
beendemonstratedinpatientswithandwithoutchronic
kid-neydisease.28,29Intheelderly,vitaminDdeficiencyseemsto
beassociatedwithACD,butnotwithothertypesofanemia,
pointingtowardapossibleroleofvitaminDininflammation
suppression.28VitaminDdeficiencywassignificantly
associ-atedwithahighhepcidinlevel,apro-inflammatorymediator
andaplayerinironmetabolism.Hepcidinmayplayarolein
ACDinCD.30Wethereforeattemptedtoconnectthedots.We
postulatethatvitaminDdeficiencyislinkedtoanemiainIBD
patients,specificallyACD,throughtheinflammation-hepcidin
axis.WhethervitaminDdeficiencycontributestoincreased
inflammation leading to ACD or whether both vitamin D
deficiencyandanemiaareacommonendofachronic
inflam-matorystateisunknown.Prospective,longitudinalstudiesare
neededtofurthersortouttheassociationorcausal
relation-ship.
Althoughthepresenceofinflammationintheileum
diag-nosed byileoscopycould potentially bepredisposedtolow
vitaminDlevelsbyfurtherimpairingabsorptionofbileacids
and vitaminD throughthe inflamed mucosa,this wasnot
confirmedinbyourstudy.Thismayindicatethatthemost
importantfactor forvitaminDdeficiency inthesepatients
isdisruptionoftheanatomy.Similarfindingsoflowvitamin
DlevelsinIBDpatientswithIPAAwithoutcorrelationwith
inflammationonendoscopyorhistologyhavebeendescribed
in the literature.27 Alternatively, this may imply that
con-ditions such as ileostomy and IPAA cause a reset of the
immunostat,interferingwithnutritionandmetabolism.
There areseveral clinicalimplications ofthe findingsin
thisstudy.VitaminDdeficiencyiscommoninpatientswith
ileostomyandvitaminDlevelsshouldberoutinelymeasured
inthesepatients.Inaddition,wesuggestthatHblevelsshould
becheckedwhenvitaminDdeficiencyisencounteredandvice
versa.Inaddition,theremaybearoleforvitaminD
supple-mentationthroughimmunomodulationinthe treatmentof
ACDinthispatientpopulation,warrantingfuturestudiesfor
confirmation.
Thisstudyhaslimitations.First,thesamplesizemaylimit
thepower ofthestudy,particularlythe analysisofanemia.
Second,therateofvitaminDdeficiencymayreflectgreater
diseaseseverityoftheIBDpatientpopulationinourtertiary
centerandmaynotrepresenttheIBDpopulationingeneral,
resultinginreferralbias.Becausethisisaretrospectivestudy,
dataonlevelsofvitaminDandanemiabeforeandafterthe
ileostomywerelackinginsomepatients,ascheckingof
vita-minDbeforeileostomyhasnotbeenapartofroutineclinical
practice.Furtherstudiesconfirmingtheassociationofvitamin
DdeficiencywithanemiasubtypesinIBDpatients
indepen-dentofsurgicalstatusmaybeofinterest.Inaddition,itmay
beinterestingtocomparedifferentdosesofvitaminD
supple-mentationinpatientswithileostomyinthefuturetoestablish
if vitamin D supplementationcan ameliorate notonly the
vitamin Ddeficiency but alsoanemia inIBD patientswith
ileostomy.
In conclusion, vitamin D deficiency is common in IBD
endoscopy or histology and is associated with anemia,
PatientswithIBDand anemiashouldberoutinelyscreened
forvitaminDdeficiencyandviceversa.VitaminDdeficiency
mayplayaroleinACD.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgement
Dr.BoShenissupportedbytheEdandJoeyStoryEndowed
Chair.
r
e
f
e
r
e
n
c
e
s
1. ZhuY,MahonBD,FroicuM,CantornaMT.Calciumand1 alpha,25-dihydroxyvitaminD3targettheTNF-alphapathway
tosuppressexperimentalinflammatoryboweldisease.EurJ Immunol.2005;35:217–24.
2. LookerAC,Dawson-HughesB,CalvoMS,GunterEW,Sahyoun NR.Serum25-hydroxyvitaminDstatusofadolescentsand adultsintwoseasonalsubpopulationsfromNHANESIII. Bone.2002;30:771–7.
3. Bischoff-FerrariHA,DietrichT,OravEJ,HuFB,ZhangY, KarlsonEW,etal.Higher25-hydroxyvitaminD
concentrationsareassociatedwithbetterlower-extremity functioninbothactiveandinactivepersonsaged>or=60y. AmJClinNutr.2004;80:752–8.
4. JanowskyEC,LesterGE,WeinbergCR,MillikanRC, SchildkrautJM,GarrettPA,etal.Associationbetweenlow levelsof1,25-dihydroxyvitaminDandbreastcancerrisk. PublicHealthNutr.1999;2:283–91.
5. HyppönenE,LääräE,ReunanenA,JärvelinMR,VirtanenSM. IntakeofvitaminDandriskoftype1diabetes:abirth-cohort study.Lancet.2001;358:1500–3.
6. MungerKL,LevinLI,HollisBW,HowardNS,AscherioA. Serum25-hydroxyvitaminDlevelsandriskofmultiple sclerosis.JAMA.2006;296:2832–8.
7. MerlinoLA,CurtisJ,MikulsTR,CerhanJR,CriswellLA,Saag KG.VitaminDintakeisinverselyassociatedwithrheumatoid arthritis:resultsfromtheIowaWomen’sHealthStudy. ArthritisRheum.2004;50:72–7.
8. FuYT,ChaturN,Cheong-LeeC,SalhB.HypovitaminosisDin adultswithinflammatoryboweldisease:potentialroleof ethnicity.DigDisSci.2012;57:2144–8.
9. SuibhneTN,CoxG,HealyM,O’MorainC,O’SullivanM. VitaminDdeficiencyinCrohn’sdisease:prevalence,risk factorsandsupplementuseinanoutpatientsetting.JCrohns Colitis.2012;6:182–8.
10.NguyenGC,NugentZ,ShawS,BernsteinCN.Outcomesof patientswithCrohn’sdiseaseimprovedfrom1988to2008 andwereassociatedwithincreasedspecialistcare. Gastroenterology.2011;141:90–7.
11.CosciaM,GentiliniL,LauretiS,GionchettiP,RizzelloF, CampieriM,etal.Riskofpermanentstomainextensive Crohn’scolitis:theimpactofbiologicaldrugs.ColorectalDis. 2013;15:1115–22.
12.WeissG,GoodnoughLT.Anemiaofchronicdisease.NEnglJ Med.2005;352:1011–23.
13.BlanckS,AberraF.VitaminDdeficiencyisassociatedwith ulcerativecolitisdiseaseactivity.DigDisSci.
2013;58:1698–702.
14.HamM,LonghiMS,LahiffC,CheifetzA,RobsonS,MossAC. VitaminDlevelsinadultswithCrohn’sdiseaseare
responsivetodiseaseactivityandtreatment.InflammBowel Dis.2014;20:856–60.
15.AnanthakrishnanAN,CaganA,GainerVS,CaiT,ChengSC, SavovaG,etal.Normalizationofplasma25-hydroxyvitamin DisassociatedwithreducedriskofsurgeryinCrohn’s disease.InflammBowelDis.2013;19:1921–7.
16.JorgensenSP,HvasCL,AgnholtJ,ChristensenLA, HeickendorffL,DahlerupJF.ActiveCrohn’sdiseaseis associatedwithlowvitaminDlevels.JCrohnsColitis. 2013;7:407–13.
17.JantchouP,Clavel-ChapelonF,RacineA,KvaskoffM, CarbonnelF,Boutron-RuaultMC.Highresidentialsun exposureisassociatedwithalowriskofincidentCrohn’s diseaseintheprospectiveE3Ncohort.InflammBowelDis. 2014;20:75–81.
18.VagianosK,BectorS,McConnellJ,BernsteinCN.Nutrition assessmentofpatientswithinflammatoryboweldisease. JPENJParenterEnteralNutr.2007;31:311–9.
19.FarrayeFA,NimitphongH,StucchiA,DendrinosK,Boulanger AB,VijjeswarapuA,etal.UseofanovelvitaminD
bioavailabilitytestdemonstratesthatvitaminDabsorptionis decreasedinpatientswithquiescentCrohn’sdisease. InflammBowelDis.2011;17:2116–21.
20.LeichtmannGA,BengoaJM,BoltMJ,SitrinMD.Intestinal absorptionofcholecalciferoland25-hydroxycholecalciferolin patientswithbothCrohn’sdiseaseandintestinalresection. AmJClinNutr.1991;54:548–52.
21.GuptaS,WuX,MooreT,ShenB.Frequency,riskfactors,and adversesequelaeofbonelossinpatientswithostomyfor inflammatoryboweldiseases.InflammBowelDis. 2014;20:259–64.
22.JayaprakashA,CreedT,StewartL,ColtonB,MountfordR, StandenG,etal.ShouldwemonitorvitaminB12levelsin patientswhohavehadend-ileostomyforinflammatory boweldisease?IntJColorectalDis.2004;19:316–8.
23.NissinenMJ,GyllingH,JärvinenHJ,MiettinenTA.Ileal pouch-analanastomosis,conventionalileostomyand ileorectalanastomosismodifycholesterolmetabolism.Dig DisSci.2004;49:1444–53.
24.KennedyHJ,CompstonJ,HeynenG,KanisJA,MerrettAL, TrueloveSC,etal.Calciummetabolisminsubjectslivingwith apermanentileostomy.Digestion.1983;26:131–6.
25.TomitaR,FujisakiS,TanjohK.Relationshipbetween gastrointestinaltransittimeanddailystoolfrequencyin patientsafterIlealJpouch-analanastomosisforulcerative colitis.AmJSurg.2004;187:76–82.
26.GorbachSL,TabaqchaliS.Bacteria,bile,andthesmallbowel. Gut.1969;10:963–72.
27.KhannaR,WuX,ShenB.LowlevelsofvitaminDarecommon inpatientswithilealpouchesirrespectiveofpouch
inflammation.JCrohnsColitis.2013;7:525–33.
28.PerlsteinTS,PandeR,BerlinerN,VanasseGJ.Prevalenceof 25-hydroxyvitaminDdeficiencyinsubgroupsofelderly personswithanemia:associationwithanemiaof inflammation.Blood.2011;117:2800–6.
29.SimJJ,LacPT,LiuIL,MeguerditchianSO,KumarVA,Kujubu DA,etal.VitaminDdeficiencyandanemia:across-sectional study.AnnHematol.2010;89:447–52.