w w w . r b o . o r g . b r
Original
article
Treatment
of
two-part
fractures
of
the
surgical
neck
of
the
humerus
using
a
locked
metaphyseal
intramedullary
nail
proximally
with
angular
stability
夽
Leandro
Viecili
∗,
Donato
Lo
Turco,
João
Henrique
Arruda
Ramalho,
Carlos
Augusto
Finelli,
Alexandre
Penna
Torini
CarminoCaricchioMunicipalHospital,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received30November2013 Accepted13February2014 Availableonline23January2015
Keywords:
Humeralfracture
Intramedullaryfracturefixation Surgicalprocedures
a
b
s
t
r
a
c
t
Objectives:Toevaluatethe functionalresultsfrompatientswithsurgical neckfractures treatedwithalockedmetaphysealintramedullarynailandangularstability.
Methods:Twenty-twopatientsbetweentheagesof21and69yearswereevaluated prospec-tivelybetweenJanuary2010andJanuary2011.Theirtimetakenforconsolidation,age,sex, complicationsandfunctionalresultswerecorrelatedusingthemodifiedprotocolofthe UniversityofCaliforniaatLosAngeles(UCLA).
Results:Themeantimetakenforconsolidationwas9.26weeks±confidenceinterval(CI)of 0.40weeks.Onecase(4.5%)didnotbecomeconsolidated.Therewerenocasesofinfection. Therewasonecase(4.5%)ofadhesivecapsulitiswithgoodevolutionthroughclinical treat-ment.Fivepatients(22.7%)presentedoccasionalmildpainandonecase(4.5%)reported medium-intensitypainassociatedwiththesubacromialimpactoftheimplant.Themean scoreonthemodifiedUCLAscalewas30.4±CI1.6points,obtainedattheendof12weeks ofevaluation:18cases(81.8%)with“excellent”and“good”scores,threecases(13.6%)with “fair”scoresandonecase(4.5%)witha“poor”score.
Conclusion:Inthegroupofpatientsevaluated,treatmentoftwo-partsurgicalneckfractures bymeansofalockedmetaphysealintramedullarynailandangularstabilitydemonstrated satisfactoryfunctionalresultsandalowcomplicationrate,similartowhatisseeninthe literature.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
夽
WorkdevelopedintheInstituteofOrthopedicsandTraumatology,CarminoCaricchioMunicipalHospital,SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mails:leandro.viecili@hotmail.com,leandro.viecili@me.com(L.Viecili).
http://dx.doi.org/10.1016/j.rboe.2015.01.001
Tratamento
das
fraturas
em
duas
partes
do
colo
cirúrgico
do
úmero
com
o
uso
de
haste
intramedular
metafisária
bloqueada
proximalmente
com
estabilidade
angular
Palavras-chave:
Fraturadoúmero
Fixac¸ãointramedulardefraturas Procedimentoscirúrgicos
r
e
s
u
m
o
Objetivos: Avaliaros resultados funcionaisdepacientescomfraturas docolocirúrgico tratadoscomhasteintramedularmetafisáriabloqueada(HIMB)eestabilidadeangular.
Métodos: Foramanalisados22pacientesprospectivosentre21e69anos,avaliadosentre janeirode2010ejaneirode2011,ecorrelacionadostempodeconsolidac¸ão,idade,sexo, complicac¸ões e resultadofuncional comoprotocoloda Universityof CaliforniaatLos Angeles(UCLA)modificado.
Resultados: Otempodeconsolidac¸ãomédiofoide9,26±intervalodeconfianc¸a(IC)de0,40 semana.Umcaso(4,5%)nãoseconsolidou.Nãohouveinfecc¸ão.Houveumcaso(4,5%)de capsuliteadesivacomboaevoluc¸ãoaotratamentoclínico.Cincopacientes(22,7%) apre-sentaramlevedoreventualeumcaso(4,5%)referiudordemédiaintensidadeassociadaa impactosubacromialdoimplante.OescoremédioUCLAmodificadofoi30,4±IC1,6ponto obtidosnofimde12mesesdeavaliac¸ão,18casos(81,8%)comescore«excelente»e«bom»,
trêscasos(13,6%)comescore«razoável»eumcaso(4,5%)comescore«ruim».
Conclusão: Nogrupodepacientesavaliados,otratamentodasfraturas emduaspartes docolocirúrgicocomHIMBeaestabilidadeangulardemonstraramresultadosfuncionais satisfatóriosebaixoíndicedecomplicac¸ões,semelhantesaosencontradosnaliteratura.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Fractures of the proximal humerus represent 5% of all fractures. They are more prevalent in the elderly pop-ulation and among females.1 Surgical indications are
based on the displacement presented by the fragments, according to the criteria described by Neer,2 and on the
variations in expectations from the final result, which depend on the patient’s age and activity levels before the injury.3–5
Mostfracturesdonotpresentdisplacement.6Among
ado-lescentsandyoungadults,high-energymechanismsaremore common.Amongelderlypeople,low-energymechanismsare morecommon,suchas fallingtothe ground withindirect injurytooneoftheupperlimbs.7Useofdrugs,alcoholand
tobacco,alongwithanyclinicalconditionthatleadsto osteo-porosis,increasestheriskoffracturesinyoungpatients.8–10
Fracturesofthe surgicalneckofthehumerus represent 25%ofthefracturesoftheproximalregion.Providedthatthe softtissuesand bloodsupplyare notgreatlycompromised, thereisalowriskofosteonecrosis.Neerdescribedthreetypes offractureofthesurgicalneck:angled,translated/separated andcomminuted.2Thediaphysistendstobepulled
antero-mediallythroughtheactionofthepectoralismajormuscle. Thedisplacementexpectedfromtheproximalregionthrough theactionoftherotator cuffisforaneutralpositiontobe adopted,oronethatisprogressivelytowardvarus.2
Thereare severaloptionsforsurgicaltreatment.11 Open
reduction and fixation using a fixed-angle plate is an optionthathasbeenwidelydisseminatedintheliterature.12
However, indirect reduction and fixation using a locked
metaphyseal intramedullarynail(LMIN)hasbeengradually gainingspaceinthetherapeuticarsenal.13
Materials
and
methods
Twenty-twopatients(ninefemalesand13males)aged21–69 years, with mean age 41.4±confidence interval (CI) of6.2 years, were evaluated prospectively between January 2010 and January2011.Allofthempresentedtwo-partfractures of the surgical neck of the humerus that were classi-fied as Neer type II.2 They underwent closed reduction
and internalfixation using LMIN and angularstabilization
(Figs.1and2).
Thepatientsunderwentregionalblockanesthesia,which complemented generalanesthesia,and were placedin the deckchairposition.Askinincisionofapproximatelength2cm wasmadeintheanterolateralregionoftheshoulder,atthe projectionofthegreatertubercle.Boththedeltoidmuscleand therotator cuffwere pushedbacklongitudinally.Theentry pointforthenailwasbetween8and9mmmediallytothe bone-cartilagetransition(centralizedonthehumeralheadin frontalandlateralviews)andtheinitialdrillingdiameterwas 9mm(Fig.3).
Tofacilitatelocalizationoftheentrypointandintroduction oftheguidewire,weoftenusedaKirschnerwireof2.5mmin diameter,placedeccentrically,which enabledinternal rota-tionandadductionoftheproximalfragmentandgenerated truefrontalandlateralfluoroscopyimages(Fig.4).
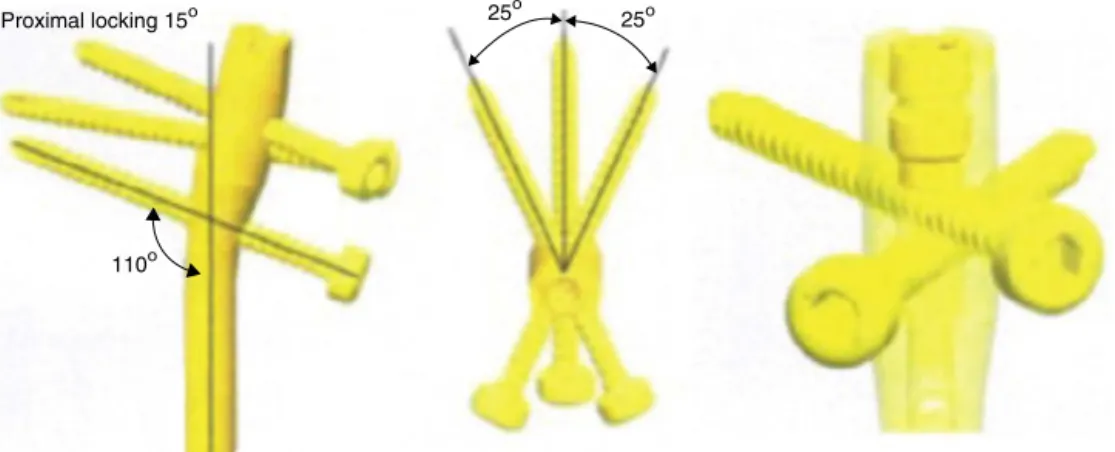
Proximal locking 15ο 25 ο
25ο
110ο
Fig.1–Schematicdrawingoftheintramedullarymetaphysealnailwithproximallockingandangularstabilization.
Thenailneededtobeintroducedsuchthatits proximal extremitywouldbeapproximately4mminsidethecortical bone.Wedirectedtheguideatapproximately20–30◦ inthe
anteroposteriordirection(wefollowedtheretroversionofthe humeralhead), so that the proximallocking (inserted per-cutaneously)wouldremainatthecenterofthehead.Using fluoroscopy,wecheckedthatthecannulawasincontactwith thelateralcortexofthehumerus,sincethemeasurementof theproximalscrew(diameter4mm)wasdonebymeansof thedrillbit(diameter3.2mm),inmillimeters.
The fracture was reduced under fluoroscopic control (Fig.5).Acannulawastheninsertedtoperformdistallocking, bymeansoftheexternalguide.Thesizeofthedistalscrew (diameter 4mm) was alsomeasured by means ofmarking usingthedrillbit(diameter3.2mm),inmillimeters.
Finally,ascrewwasplacedtocloseoffthenailfromabove (plug),which lockedthetwomoreproximalscrewsagainst
Fig.2–Intramedullarymetaphysealnailwithproximal lockingandangularstabilization.
eachother.Inthismanner,angularstabilitywasachieved.The incisioninthecuffwassuturedusingabsorbablethread.
The skin was sutured and a dressing was applied. The patient was instructed to use a Velpeau sling for
Fig.3–Pointofentryofthenail.
Fig.5–Anteroposteriorandlateral-viewfluoroscopic imagesshowingreductionofthefracture,theimplantand theproximallocking.
approximatelyfourweeks.Onthefirstdayafterthe opera-tion,guidance wasgiven regardingactiveexercisesforthe elbow, wrist and hand, swinging exercises for the shoul-derandisometricexercisesfortheupperarm.Thestitches wereremoved10–14dayslater,accordingtowhenthe con-ditionsobservedthroughclinicalexaminationweredeemed appropriate. Radiographs for checking on the reduction were requested every week until consolidation had been achieved.
Fourweeksaftertheoperation,thepatientwasreferredfor physiotherapy,inordertoincreasetherangeofmotionand strengthenthemusclesofthelimbinvolved.
Allthepatientswerefollowedupaftertheoperationfor atleast12months(Fig.6),withradiographiccontrols(Fig.7), andtheywereevaluatedattheendofthisperiodusingthe modifiedUCLAscore14(Table1).
Nonparametric tests, tests on the equality of two pro-portions,correlation tests,Spearman’scorrelations andthe Mann–Whitney test were used, with complete descriptive
Fig.6–Imagedemonstratingevaluationontheleft shoulder12monthsafterthetreatment.
Table1–UCLAscoringsystem.Scaletranslatedand adaptedtothePortugueselanguage.14
I–Pain
1)Presentallthetimeandintolerable; medicationusedregularly
1
2)Presentallthetimebuttolerable; medicationusedfromtimetotime
2
3)Nopainorlittlepainwhenthearmis notmoving,butoccursduringlightwork; medicationusedregularly
4
4)Occursonlyduringheavyworkor specificwork;medicationusedfromtime totime
6
5)Mildpainoccurringfromtimetotime 8
6)Nopain 10
II–Function
1)Incapableofusingthearm 1
2)Onlycapableofperforminglight activities
2
3)Capableofperforminglightdomestic workorthemajorityofday-to-daywork
4
4)Capableofperformingmostdomestic work,includingshopping,driving, combinghair,gettingdressed,getting undressedandclosingabra
6
5)Littledifficultypresented;capableof makingmovementsaboveshoulderlevel
8
6)Normalactivities 10
Instructionsforgoniometry Thepatientshouldbeinaseated positionwiththelimbatthesideofthe body,intheneutralposition.The examinershouldinstructthepatientto raisehisarmasfaraspossiblewithout makingcompensations.
Thegoniometerwillbepositionedwith theproximalarmonthemidaxillaryline ofthethoraxandthedistalarmonthe lateralmidlineofthehumerus,andthe axiswasplacedclosetotheacromion.
III–Activeanteriorflexion
1)150◦ormore 5
2)120–150◦ 4
3)90–120◦ 3
4)45–90◦ 2
5)30–45◦ 1
6)Lessthan30◦ 0
Instructionsforthemanualstrengthtest Thepatientshouldbeinaseated positionwiththelimbbesidethebody andtheforearmpronated.Thepatient shouldthenraisethisarmto90◦.The examinershouldinstructhimtomaintain thispositionagainsttheresistancethat willbeappliedtothedistalportionofthe humerus(abovetheelbow).
IV–Activeanteriorflexionstrength(manualstrengthtest)
1)Grade5(normal) 5
2)Grade4(good) 4
3)Grade3(fair) 3
4)Grade2(weak) 2
5)Grade1(musclecontraction) 1
Table1–(Continued)
V–Patient’ssatisfaction
1)Satisfiedandbetter 5
2)Dissatisfiedandworse 0
UCLAclassification Scoring
Excellent 34–35
Good 28–33
Reasonable 21–27
Poor 0–20
analysisonthevariables.Correlationsbetweenthetimetaken toconsolidate,age,sexandfunctionalresultwereevaluated usingthemodifiedUCLAprotocol.14Short-termcomplications
andthosethatappearedupto12monthsafterthetreatment werealsoevaluated.
Fig.7–Anteroposteriorandlateral-viewradiographs showingconsolidationofthefracture.
Table3–Completedescriptionforage,UCLAandTC.
Description Age UCLA TC
Mean 41.4 30.4 9.26
Median 40.5 31.0 9.0
Standarddeviation 14.9 3.9 0.94
CV 36% 13% 10%
Q1 28.3 29.0 9.0
Q3 48.8 33.0 10.0
Min 21 19 7.5
Max 69 35 11
N 22 22 21
CI 6.2 1.6 0.40
TC,timetakentoconsolidateinweeks;CV,coefficientofvariation; Q1,firstquartile(distributionupto25%ofthesample);Q3,third quartile(distributionupto75%ofthesample;N,quantityincluded; CI,confidenceinterval.
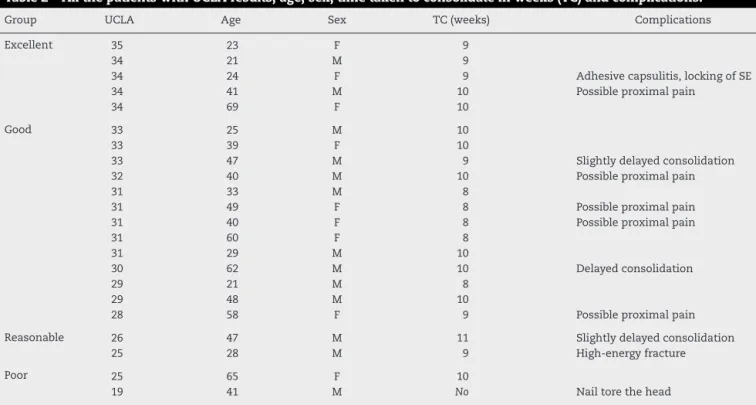
Results
Themeantimetakentoconsolidate(TC)was9.26±CI0.94 weeks.Onecase(4.5%)didnotconsolidateandevolvedwith loss of reduction. Subsequently, this case was reoperated using alocked plate.There wasno infection.Five patients (22.7%)presentedoccasionalmildpainandone(4.5%)reported medium-intensitypainthatwasassociatedwithsubacromial impactoftheimplant.Therewasonecase(4.5%)ofadhesive capsulitis,whichevolvedwellthroughclinicaltreatment.The meanmodifiedUCLAscore14was30.4±CI3.9pointsafter12
months:fivecases(22.7%)with“excellent”scores;13(59.1%) with“good”;three(13.6%)with“reasonable”;andone(4.5%) with“poor”(Tables2–4).
Table2–AllthepatientswithUCLAresults,age,sex,timetakentoconsolidateinweeks(TC)andcomplications.
Group UCLA Age Sex TC(weeks) Complications
Excellent 35 23 F 9
34 21 M 9
34 24 F 9 Adhesivecapsulitis,lockingofSE
34 41 M 10 Possibleproximalpain
34 69 F 10
Good 33 25 M 10
33 39 F 10
33 47 M 9 Slightlydelayedconsolidation
32 40 M 10 Possibleproximalpain
31 33 M 8
31 49 F 8 Possibleproximalpain
31 40 F 8 Possibleproximalpain
31 60 F 8
31 29 M 10
30 62 M 10 Delayedconsolidation
29 21 M 8
29 48 M 10
28 58 F 9 Possibleproximalpain
Reasonable 26 47 M 11 Slightlydelayedconsolidation
25 28 M 9 High-energyfracture
Poor 25 65 F 10
Confidence interval for the mean 95% CI for the mean
32
31
30
29 48
45
42
39
36
9.6
9.4
9.2
9.0
8.8
TC
UCLA Age
Fig.8–Confidenceintervalforthemeanage,UCLAscoreandtimetakentoconsolidate(TC).
Table4–DistributionintoUCLAbands.
UCLAband n % p-value
Poor 1 4.5% <0.001
Reasonable 3 13.6% 0.002
Good 13 59.1% Ref.
Excellent 5 22.7% 0.014
n,numberinthesample;%,percentageofthegroup;p-value,value ofp.
Itwasobservedthattherewasnostatisticallysignificant difference between the sexes, in relation to age, modified UCLAscore14orTC(Table5,Figs.8and9).
Discussion
There is a great diversity of methods and techniques for osteosynthesis of fractures of the surgical neck of the humerus. Fixation using LMIN and angular stabilization,
Age
UCLA
TC
36 28
20 60
40 20
7 9 11 20 28 36
Fig.9–Correlationbetweenage,UCLAscoreandtime takentoconsolidate(TC).
whichhastheaimoffacilitatingtheoperation,canbe high-lightedamongthesetechniques.
Anenormousvarietyofstudiescitingtheadvantagesand disadvantagesofthedifferentmethodsandimplantscanbe
Table5–Comparisonofsex,age,UCLA14andTC.
Sex Age UCLA TC
Female Male Female Male Female Male
Mean 47.4 37.2 31.3 29.7 8.9 9.5
Median 49.0 40.0 31.0 31.0 9.0 10.0
Standarddeviation 17.0 12.3 3.2 4.3 1.0 0.9
Q1 39.0 28.0 31.0 29.0 8.0 9.0
Q3 60.0 47.0 34.0 33.0 10.0 10.0
N 9 13 9 13 9 12
CI 11.1 6.7 2.1 2.3 0.6 0.5
p-value 0.181 0.345 0.188
found.However,fewauthorshavedealtwiththeadvantages ofosteosynthesisusingLMINandangularstabilization.13,15,16
Mostauthorsagreethatnon-operativetreatmentshouldbe usedforfracturesoftheproximalextremityofthehumerus thatdonotpresentdisplacementorarestablewithminimal displacement.Othershavealreadydescribedthenatural his-toryoffractures ofthe proximalhumerus.17 Non-operative
treatmentdoesnotallowearlymobilization.
Surgical management becomesmore difficultwhen the fracturesoccur inelderlypatientswithosteoporoticbones, poorbonestockorahighdegreeofcomminutionand displace-ment.Injurytothebloodsupplymayresultinosteonecrosis. Proximitytotheshoulderjointandinjuryoftherotatorcuff may lead tosevere stiffnessand necessitatea program of intensive rehabilitation in order to improve the return of functions.18
There isinsufficient evidence todetermine what isthe besttreatmentforfracturesoftheproximalhumerus.Tension bandsrequireextensiveexposureinordertoachieve reduc-tionand fixationandmay giverisetoaposteromedialgap andcut-out.16Fixationbymeansoftransosseoussuturingalso
necessitatesmajorexposureandmaynotprovidesufficient stability.Transcutaneous pinningmaycause skinirritation, infectionofthepathwayandlossofreduction,andrequires goodsurgicalskills.19Fixationwithlockedplatesandscrewsis
agoodoptionwhentheboneisosteoporotic.20However,this
requiresextensivedissectionofsofttissuesandincreasesthe riskofavascularnecrosisandsubacromialimpact.21
In a biomechanical study conducted on cadavers, intramedullary fixation with proximal angular stabiliza-tion was shown to be less rotationally stable than use of fixed-angleplates.However,therewassufficientstabilityto allowclinical use,especiallywithregard tofractures ofthe surgicalneck.15,21–23
Sinceiatrogenicinjuryseemstobeimportantwithregard tothepathogenesisofavascularnecrosisofthehumeralhead and the fracture pattern, closed reduction and associated intramedullaryfixationcanbejustified.24Ageisanimportant
prognosticfactorinrelationtononunionandtheseverityof thefracture.25
Another problem is the development of osteoporosis, which has a large impact on the proximal third of the humerus,giventhatthebonemineraldensityofthehumeral headrepresentsonly65%ofthedensity ofthe baseofthe femoralhead.26 Moreover,thehumerusfunctionsfreefrom
theactionofloads,whichmayworsenthedemineralization. The possible complications from surgery include: sub-acromialimpactofthenail,rotatorcuffinjury,nerveinjury (axillary nerve), pseudarthrosis, skewed consolidation and superficialanddeepinfection.24,26–28
Recently withthe aimofadding aresource fortreating fracturesoftheproximalhumerus,severalnailswith multi-plelockingscrewshavebeendesigned,andtherehavebeen refinementstothetechniquesinvolved.Intwo-partfractures, satisfactory resultscan be obtainedusing locked plates or intramedullarynails.29
This reduction and fixation method has the following advantages:itenablesearlymobility;doesnotopenthefocus ofthefracture;isnotaggressivetowardtheperiosteumand soft tissues; provides good stability; and causes very little
bleeding. Thedisadvantagesare itshighcostand theneed tousefluoroscopy(irradiation).15
Conclusion
Inthegroupofpatientsevaluated,treatmentoftwo-part frac-turesofthesurgicalneckusingLMINandangularstabilization showedsatisfactoryfunctionalresultsandalowcomplication rate,similartowhathasbeenshownintheliterature.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.Court-BrownCM,GargA,McQueenMM.Theepidemiologyof
proximalhumeralfractures.ActaOrthopScand.
2001;72(4):365–71.
2.NeerCS2nd.Displacedproximalhumeralfractures.I.
Classificationandevaluation.JBoneJointSurgAm.
1970;52(6):1077–89.
3.Court-BrownCM,CattermoleH,McQueenMM.Impacted
valgusfractures(B1.1)oftheproximalhumerus.Theresults
ofnon-operativetreatment.JBoneJointSurgBr.
2002;84(4):504–8.
4.Court-BrownCM,GargA,McQueenMM.Thetranslated
two-partfractureoftheproximalhumerus.Epidemiologyand
outcomeintheolderpatient.JBoneJointSurgBr.
2001;83(6):799–804.
5.Court-BrownCM,McQueenMM.Theimpactedvarus(A2.2)
proximalhumeralfracture:predictionofoutcomeandresults
ofnonoperativetreatmentin99patients.ActaOrthopScand.
2004;75(6):736–40.
6.BaronJA,BarrettJA,KaragasMR.Theepidemiologyof
peripheralfractures.Bone.1996;183Suppl.:209S–13S.
7.BartlettCS3rd,HausmanMR,WitschiTH.Gunshotwounds
totheshoulder.OrthopClinNorthAm.1995;26(1):37–53.
8.LeeSH,Dargent-MolinaP,BréartG.Epidemiologiede
l’Osteoporosestudyriskfactorsforfracturesoftheproximal
humerus:resultsfromtheEpidosprospectivestudy.JBone
MinerRes.2002;17(5):817–25.
9.NguyenTV,CenterJR,SambrookPN,EismanJA.Riskfactors
forproximalhumerus,forearm,andwristfracturesinelderly
menandwomen:theDubboOsteoporosisEpidemiology
Study.AmJEpidemiol.2001;153(6):587–95.
10.NordqvistA,PeterssonCJ.Shoulderinjuriescommonin
alcoholics.Ananalysisof413injuries.ActaOrthopScand.
1996;67(4):364–6.
11.TepassA,BlumenstockG,WeiseK,RolauffsB,BahrsC.
Currentstrategiesforthetreatmentofproximalhumeral
fractures:ananalysisofasurveycarriedoutat348hospitals
inGermanyAustria,andSwitzerland.JShoulderElbowSurg.
2013;22(1):e8–14.
12.CohenM,AmaralMV,MonteiroM,BrandãoBL,MottaFilho
GR.Osteossíntesedasfraturasdaextremidadeproximaldo
úmerocomsistemadeplacadeângulofixocomparafusos
bloqueados:técnicaeresultados.RevBrasOrtop.
2009;4(2):106–11.
13.AgelJ,JonesCB,SanzoneAG,CamusoM,HenleyMB.
TreatmentofproximalhumeralfractureswithPolarusnail
fixation.JShoulderElbowSurg.2004;13(2):191–5.
14.OkuEC,AndradeAP,StadinikySP,CarreraEF,TelliniGG.
CaliforniaatLosAngelesShoulderRatingScaleparaalíngua
portuguesa.RevBrasReumatol.2006;46(4):246–52.
15.HessmannMH,HansenWS,KrummenauerF,PolTF,
RommensP.Lockedplatefixationandintramedullarynailing
forproximalhumerusfractures:abiomechanicalevaluation.
JTrauma.2005;58(6):1194–201.
16.LinJ,HouSM,HangYS.Lockednailingfordisplacedsurgical
neckfracturesofthehumerus.JTrauma.1998;45(6):1051–7.
17.RasmussenS,HvassI,DalsgaardJ,ChristensenBS,HolstadE.
Displacedproximalhumeralfractures:resultsofconservative
treatment.Injury.1992;23(1):41–3.
18.KumarV,DatirS,VenkateswaranB.Intramedullarynailingfor
displacedproximalhumeralfractures.JOrthopSurg(Hong
Kong).2010;18(3):324–7.
19.KovalKJ,BlairB,TakeiR,KummerFJ,ZuckermanJD.Surgical
neckfracturesoftheproximalhumerus:alaboratory
evaluationoftenfixationtechniques.JTrauma.
1996;40(5):778–83.
20.HawkinsRJ,KieferGN.Internalfixationtechniquesfor
proximalhumeralfractures.ClinOrthopRelatRes.
1987;(223):77–85.
21.SturzeneggerM,FornaroE,JakobRP.Resultsofsurgical
treatmentofmultifragmentedfracturesofthehumeralhead.
ArchOrthopTraumaSurg.1982;100(4):249–59.
22.FüchtmeierB,MayR,FierlbeckJ,HammerJ,NerlichM.A
comparativebiomechanicalanalysisofimplantsforthe
stabilizationofproximalhumerusfractures.TechnolHealth
Care.2006;14(4–5):261–70.
23.FüchtmeierB,MayR,HenteR,MaghsudiM,VölkM,Hammer
J,etal.Proximalhumerusfractures:acomparative
biomechanicalanalysisofintraandextramedullaryimplants.
ArchOrthopTraumaSurg.2007;127(6):441–7.
24.RiemerBL,D’AmbrosiaR.Theriskofinjurytotheaxillary
nerve,artery,andveinfromproximallockingscrewsof
humeralintramedullarynails.Orthopedics.1992;15(6):
697–9.
25.GradlG,DietzeA,ArndtD,BeckM,GiererP,BörschT,etal.
Angularandslidingstableantegradenailing(TargonPH)for
thetreatmentofproximalhumeralfractures.ArchOrthop
TraumaSurg.2007;127(10):937–44.
26.SaitohS,NakatsuchiY.Osteoporosisoftheproximal
humerus:comparisonofbone-mineraldensityand
mechanicalstrengthwiththeproximalfemur.JShoulder
ElbowSurg.1993;2(2):78–84.
27.BernardJ,CharalambidesC,AderintoJ,MokD.Earlyfailureof
intramedullarynailingforproximalhumeralfractures.Injury.
2000;31(10):789–92.
28.BlumJ,RommensPM.Proximalinterlockingofhumeral
intramedullarynailsandriskofaxillarynerveinjury.
Unfallchirurg.2002;105(1):9–13.
29.CalvoE,deMiguelI,delaCruzJJ,López-MartínN.
Percutaneousfixationofdisplacedproximalhumeral
fractures:indicationsbasedonthecorrelationbetween
clinicalandradiographicresults.JShoulderElbowSurg.