Associations between symptoms and varicose veins and great
saphenous vein reflux seen on Doppler ultrasonography
Associação entre sintomas, veias varicosas e refluxo na veia safena
magna ao eco-Doppler
Amélia Cristina Seidel1
*
, Mariana Baldini Campos1,2, Raquel Baldini Campos1,2, Dérica Sayuri Harada1,3,
Robson Marcelo Rossi4, Pedro Cavalari Junior4, Fausto Miranda Junior5
Abstract
Background: Chronic venous disease demands clinical assessment, quantiication of hemodynamic efects, and deinition of anatomic distribution before diagnostic and treatment decisions can be made. Methods: his is a prospective study conducted in 2015 with a sample of 1,384 patients (2,669 limbs) aged from 17 to 85 years, 1,227 of whom were female. he most common symptoms reported in response to the questionnaire were pain, tiredness, feelings of heaviness, burning, cramps, and tingling. Subsets were formed on the basis of number of limbs distributed by sex, body mass index, and age. After deinition of subsets, Doppler ultrasonography was used to conduct examinations of the great saphenous vein (GSV) and patients were distributed into three clinical groups (I: symptoms present and varicose veins absent, II: symptoms absent and varicose veins present and III: symptoms present and varicose veins present). Statistical analysis employed the chi-square test or Fisher’s exact test to test for homogeneity between groups. When associations signiicant to 5% were detected, odds ratios were calculated. Results: For both sexes, the chance of GSV insuiciency was 11.2 times greater in group III. Among cases with morbid obesity, the chance was 9.1 times greater in the same group. Additionally, patients in this group with ages ranging from 30 to 50 years exhibited a 43.1 times greater chance of GSV insuiciency. Conclusions: Insuiciency of the GSV was signiicantly more frequent in group III, both overall and when considering only cases with morbid obesity, or cases in older age groups.
Keywords: venous relux; saphenous vein; color Doppler ultrasonography; venous insuiciency; lower limbs.
Resumo
Contexto: A doença venosa crônica requer avaliação clínica, quantiicação dos efeitos hemodinâmicos e deinição da distribuição anatômica para decisão diagnóstica e tratamento. Métodos: Estudo prospectivo realizado em 2015 com amostra de 1.384 pacientes (2.669 membros) com idade entre 17 e 85 anos, sendo 1.227 do sexo feminino. Nas respostas do questionário aplicado, os sintomas pesquisados eram dor, cansaço, sensação de peso, queimação, câimbras e formigamento. Para a formação dos grupos, foi considerado o número de membros, distribuídos em relação ao gênero, ao índice de massa corporal e à idade. Após a deinição grupos e a realização do eco-Doppler para estudo da veia safena magna (VSM), os pacientes foram distribuídos em três grupos (I: sintomas presentes e varizes ausentes, II: sintomas ausentes e varizes presentes e III: sintomas presentes e varizes presentes). A análise estatística utilizou o teste qui-quadrado ou exato de Fisher para veriicar a homogeneidade entre os grupos. Em caso de associação com signiicância de 5%, foi calculada a razão de chances. Resultados: Para ambos os gêneros, foi observada chance de insuiciência da VSM 11,2 vezes maior no grupo III. Por sua vez, os casos de obesidade mórbida ocorreram 9,1 vezes mais no mesmo grupo. Além disso, pacientes na faixa etária entre 30 e 50 anos desse grupo apresentaram chance de insuiciência da VSM 43,1 vezes maior. Conclusões: A insuiciência da VSM foi signiicantemente mais frequente no grupo III, tanto globalmente como considerando apenas os casos de obesidade mórbida e a faixa etária mais elevada.
Palavras-chave: reluxo venoso; veia safena; ultrassonograia Doppler em cores; insuiciência venosa; membros inferiores.
1 Universidade Estadual de Maringá – UEM, Departamento de Medicina, Maringá, PR, Brazil. 2 Universidade Estadual de Campinas – UNICAMP, Campinas, SP, Brazil.
3 Universidade de São Paulo – USP, São Paulo, SP, Brazil.
4 Universidade Estadual de Maringá – UEM, Departamento de Cirurgia, Maringá, PR, Brazil.
5 Universidade Federal de São Paulo – UNIFESP, Escola Paulista de Medicina, Departamento de Cirurgia, São Paulo, SP, Brazil. Financial support: None.
Conlicts of interest: No conlicts of interest declared concerning the publication of this article. Submitted: August 31, 2016. Accepted: January 17, 2017.
INTRODUCTION
Chronic venous disease (CVD) is characterized
by valve incompetence in supericial, perforating, or deep veins, obstruction of the deep system, and insuficiency of the calf muscle pump. When present, it is necessary to conduct clinical assessment of severity, quantiication of hemodynamic effects, and arrive at a better deinition of its anatomic distribution.
Detection and quantiication of relux are important steps towards diagnosis and treatment.1 Development of
noninvasive methods such as Doppler ultrasonography has led to increasing rates of identiication of relux in the saphenous veins, very often in patients who are asymptomatic, although less frequently than among patients with venous disease.2
Varicose disease affects 1/3 of the population, impacting on quality of life and increasing healthcare costs. The great saphenous vein (GSV) is involved in the majority of cases. Its manifestations are a consequence of volume overload and hypertension in cutaneous veins caused by distension of the walls, valve incompetence, abnormal blood low, and secondary phenomena such as allergy and inlammation.3 However,
there are no speciic symptoms and other causes or diseases can be confused with venous insuficiency.
In the majority of patients, it is observed that pain is worse after prolonged periods standing up or sitting down. Discomfort and edema of the ankle are less common at the start of the day and cause greater inconvenience at the end of the day.
Doppler ultrasonography is used to detect the presence of functional disease that may be associated with presence of venous dilation, including telangiectasias, varicose veins and skin abnormalities.1
Relux is routinely assessed in the supericial system and perforating veins, which is then followed up with assessment of deep venous relux, which is an indispensable step in completing a diagnosis, particularly in patients who have edema and skin involvement.4,5
Studies that associate venous relux diagnosed with Doppler ultrasonography with presence or absence of symptoms have demonstrated that this method of examination is useful for identifying venous disease while in the initial stages and, therefore, to provide guidance for choosing the most appropriate treatments.
The objective of this study is to test for an association between incidence of GSV relux detected by Doppler ultrasonography examination and presence of varicose veins in the lower limbs of patients with clinical diagnoses of venous insuficiency.
METHOD
This is a cross-sectional, investigative study, conducted by analysis of records for all patients who were seen during a 12-month data-collection period (2015) and volunteered to take part. The protocol for
the study was approved by the UEM’s Permanent
Human Research Commission, under process number 34386814.5.
Patients with a history of deep venous thrombosis, peripheral arterial disease, previous operations on varicose veins, expectant mothers, and patients with vascular malformations were all excluded. Patients were also excluded if they had been diagnosed in
clinical classes C5 or C6, because there were very
few such patients, since the majority had a history of deep thrombosis or venous operations.
The data used for this study is from a sequential sample of 1,384 patients, aged from 17 to 85 years, 1,227 of whom were female and 157 of whom were male, and relates to a total of 2,669 limbs. A calculation conducted to estimate prevalence, considering a population of unknown size, with unknown prevalence, to a signiicance level of 5%, and a maximum error of 3%, indicated that the sample should contain a minimum of 1,067 patients.
Data from patient histories and physical examinations were recorded on a pre-prepared chart. An open questionnaire on the symptoms of CVD was also administered, eliciting spontaneous responses with no multiple choice options. The most frequently reported symptoms were pain, tiredness, feelings of heaviness, burning, cramps, and tingling. From the physical examination indings, weight and height were recorded and used to calculate body mass index (BMI) for all patients. Patients were allocated to clinical groups (I: symptoms present and varicose veins absent, II: symptoms absent and varicose veins present, or III: symptoms present and varicose veins present) taking into consideration varicose veins graded as clinical class C2 or higher.
Doppler ultrasonography was conducted as recommended in the literature, with patients in decubitus dorsal to examine the deep vein system and standing upright for analysis of the supericial system, using 5 to 7 MHz linear transducers or 2 to 3 MHz convex transducers for obese patients. Relux in supericial veins was deined as retrograde low if relux time was greater than 500 ms.
sex, BMI (< 25 and ≥ 25 for women; < 30 and ≥ 30 for men), and age (< 30, 30-50, or > 50 years). Once these subsets had been formed, limbs were allocated to clinical groups for analysis of GSV incompetence according to presence or absence of symptoms of CVD and of varicose veins.
Statistical analysis was conducted using the chi-square test or, depending on the situation, Fisher’s exact test, to test for homogeneity between groups. When associations signiicant to 5% (p < 0.05) were detected, odds ratios (OR) were calculated.6
RESULTS
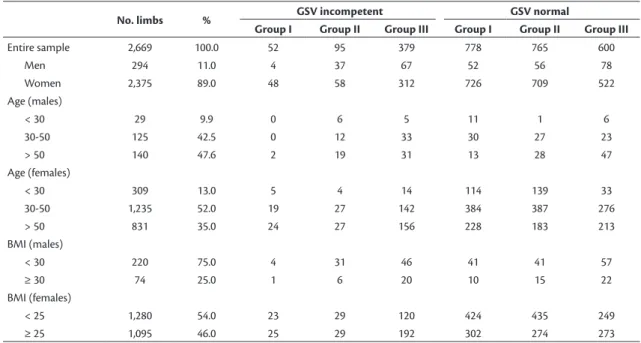
Considering the sample as a whole, Table 1 lists
the clinical groups by presence or absence of GSV incompetence, showing the number of limbs in each.
The statistical analysis for the whole sample reveals a signiicant difference (p < 0.01) between the three groups in terms of GSV incompetence, which was observed in 52 (1.9%) limbs in group I, 95 (3.6%) limbs in group II, and 379 (14.2%) limbs in group III. It was found that the chance of GSV incompetence in group II was approximately twice that of group I (the reference group) and, analogously, 9.5 times greater in group III. On the other hand, comparison of group II with group III indicated that group III had a 5.1 times greater chance of GSV incompetence when compared with group II (the reference group)
(Table 2).
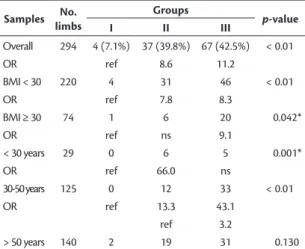
In the male subset of the sample, GSV incompetence was present in 4 (7.1%) limbs in group I, 37 (39.8%) limbs in group II, and 67 (42.5%) limbs in group III. The likelihood of incompetence, taking group I as the reference, was 8.6 times greater in group II and 11.2 times greater in group III. In the subset of males with BMI < 30, the chance of GSV incompetence was 7.8 times greater in group II and 8.3 times greater in group III in comparison to group I (reference group), respectively. In the male subset with BMI ≥ 30, the comparison between groups I and II did not detect statistical signiicance, but there was a 9.1 times greater likelihood in group III when compared with group I (reference group). Still with relation to the values for male patients shown in Table 3, the likelihood of GSV incompetence among patients less than 30 years old was 66 times greater in group II than in group I (reference group), while there was no statistically signiicant difference in the comparison between groups I and III. Among male patients aged 30 to 50, likelihood was 13.3 times greater in group II and 43.1 times greater in group III, in comparison to group I.
Considering the subset of all female limbs, GSV incompetence was present in 48 (6.2%) of the limbs in group I, 58 (7.6%) limbs in group II, and 312 (37.4%) limbs in group III. It can be observed that there were no statistical differences in the comparison between groups I and II in any of their subsets. However,
Table 1. Distribution of limbs in diferent subsets of the sample, with GSV relux and without GSV relux.
No. limbs % GSV incompetent GSV normal
Group I Group II Group III Group I Group II Group III
Entire sample 2,669 100.0 52 95 379 778 765 600
Men 294 11.0 4 37 67 52 56 78
Women 2,375 89.0 48 58 312 726 709 522
Age (males)
< 30 29 9.9 0 6 5 11 1 6
30-50 125 42.5 0 12 33 30 27 23
> 50 140 47.6 2 19 31 13 28 47
Age (females)
< 30 309 13.0 5 4 14 114 139 33
30-50 1,235 52.0 19 27 142 384 387 276
> 50 831 35.0 24 27 156 228 183 213
BMI (males)
< 30 220 75.0 4 31 46 41 41 57
≥ 30 74 25.0 1 6 20 10 15 22
BMI (females)
< 25 1,280 54.0 23 29 120 424 435 249
≥ 25 1,095 46.0 25 29 192 302 274 273
differences were detected between groups I and III and between groups II and III (Table 4).
DISCUSSION
Patients were only recruited from clinical classes
C2 and above, because more than 50% of patients aged
40 or over have telangiectasias and/or thread veins and many of these people do not have symptoms and are not interested in undergoing procedures for esthetic reasons. Symptoms such as heaviness, pain, edema, and itching may be reported, but none of these are speciic to CVD and can be associated with several different etiologies. To conirm that they are related to the presence of varicose veins, it is important to consider the speciic sites of these symptoms, their characteristics and the factors that precipitate them.2
During the anamnesis, although response options were not provided, care was taken to only include symptoms supposedly related to CVD, according to information available in the literature2,7 which
demonstrates the importance of choosing symptoms, particularly in elderly patients, in whom other conditions such as arthritis, neuropathy, claudication, spinal stenosis, congestive heart failure, renal failure, and others, can cause pain and edema in the extremities.
Symptoms of varicose veins in the absence of varicose veins have become one of the most controversial issues in angiology. It has been suggested that the pathophysiology of the presence of symptoms of venous disease in the absence of varicose veins is caused by a reduction in the tone of the vein wall and
the term hypotonic phlebopathy has been proposed
to refer to the condition.8 This may have occurred
in group I, since just 1.9% of the limbs had GSV incompetence.
In 2013, a study was conducted that investigated associations between fears of getting varicose veins and unknown GSV incompetence and prevalence and findings of symptoms of varicose veins in healthy individuals and patients with varicose veins. The authors concluded that healthy people with fears of getting varicose veins exhibit symptoms with the same frequency as people with unknown GSV incompetence and patients with varicose veins.9
Among many other risk factors (obesity,10,11 family
history,9 pregnancy, working standing or sitting for
long periods12), it seems clear that age and female sex
stand out, and have been identiied by the Acireale
project8 and other authors.13,14 However, female sex
has not universally been considered a positive risk factor.2 One of the few studies that has analyzed
the association between varicose veins and CVD in
Table 4. Presence of symptoms and/or varicose veins and their
relationships with GSV incompetence in women.
Samples No. limbs
Groups
p-value
I II III
Overall 2,375 48 (6.2%) 58 (7.6) 312 (37.4%) < 0.01
OR ref ns 9.0
ref 7.3
BMI < 25 1,280 23 29 120 < 0.01
OR ref ns 8.9
ref 7.2
BMI ≥ 25 1,095 25 29 192 < 0.01
OR ref ns 8.5
ref 6.6
< 30 years 309 5 4 14 < 0.01*
OR ref ns 9.7
ref 14.7
30-50 years 1,235 19 27 142 < 0.01
OR ref ns 10.4
ref 7.4
> 50 years 831 24 27 156 < 0.01
OR ref ns 7.0
ref 5.0
*Fisher’s exact test. ref: reference group; ns: not signiicant; GSV: great saphenous vein; OR: odds ratio.
Table 2. Distribution of limbs in diferent subsets of the sample
by presence or absence of symptoms, varicose veins, and GSV incompetence.
Sample No.
limbs
Groups
p-value
I II III
Total 2,669 52 (6.3%) 95 (11.1%) 379 (38.7%) < 0.01*
OR ref 1.9 9.5
ref 5.1
*Fisher’s exact test. ref: reference group; GSV: great saphenous vein; OR: odds ratio.
Table 3. Presence of symptoms and/or varicose veins and their
relationships with GSV incompetence in men.
Samples No. limbs
Groups
p-value
I II III
Overall 294 4 (7.1%) 37 (39.8%) 67 (42.5%) < 0.01
OR ref 8.6 11.2
BMI < 30 220 4 31 46 < 0.01
OR ref 7.8 8.3
BMI ≥ 30 74 1 6 20 0.042*
OR ref ns 9.1
< 30 years 29 0 6 5 0.001*
OR ref 66.0 ns
30-50 years 125 0 12 33 < 0.01
OR ref 13.3 43.1
ref 3.2
> 50 years 140 2 19 31 0.130
the general population, the Edinburgh Vein Study, observed that the incidence of these conditions does not differ signiicantly between the sexes, but stated that incidence of varicose veins does increase with age, family history, and BMI.15
The ideal deinition of obesity is based on body fat. Despite the differences in BMI observed in individuals of different ages and sexes, the World Health Organization still recommends using BMI to determine obesity rates.16,17 There is scientiic evidence
to suggest that different cutoffs should be used to deine excess weight in men and women, because it is normal for women to have more fat than men and for men to have more muscle mass than women and muscle weighs more than fat.18 There are studies that
suggest that different “gaps” in BMI between men and women are appropriate, ranging from 1.4 kg/m2 19
through 2 kg/m2 20 to 5 kg/m2.21 There is no single
correct answer.
In view of the disagreement in the literature with relation to the risk factors for GSV incompetence, the decision was taken to distribute the patients into several subsets. The irst characteristic considered was sex (male or female) and then, within each sex subset, patients were allocated to three further subsets by age (< 30, 30-50, and > 50 years) and two by BMI (with the cutoff for obesity set at 25 for women and 30 for men).22
Doppler ultrasonography was chosen to study the venous system because GSV relux has been identiied in asymptomatic patients,23 and this is considered the
best method for assessment of relux in individual vein segments. Examinations were conducted with the patients standing up and the cutoff for relux in supericial veins was set at > 500 ms.24
One study investigated associations between ultrasonographic findings and Clinical Etiology Anatomy Physiopathology (CEAP) classiication in a group of 1,029 patients and observed that presence of obstruction in the deep vein systems of patients with CVD graded as clinical classes C0-C1 could justify
a recommendation for Doppler ultrasonography in all patients with symptoms of CVD but without clinical signs.25
In the present study, it was observed that GSV incompetence was present in a greater percentage of patients in group III, who had both symptoms and varicose veins, corroborating data from another study1
which evaluated the association between intensity of relux at the saphenofemoral junction (JSF) and changes in the diameter of incompetent GSVs. The authors of that study observed a correlation between diameter,
velocity, and low in the GSV and clinical severity according to the CEAP system.
According to the literature,26 greater relux is
accompanied by more pronounced clinical status. An increase has been observed in the frequency of symptoms and skin problems in the presence of GSV and/or JSF incompetence, particularly when relux extends as far as the malleolus. We have conirmed that observation, showing that patients with symptoms of CVD and varicose veins have a greater incidence of relux. Additionally, in cases of isolated GSV relux, in the absence of signs but with symptoms, as in group I, there is a low percentage of GSV incompetence.
However, contradicting these indings, Chastanet and Pittalugo26 showed that patients with GSV
incompetence but without varicose veins exhibited a high frequency of symptoms and skin abnormalities, which could indicate a speciic form of CVD with early GSV deiciency resulting in increased morbidity. Development of JSF incapacity appears to be a key point, since the rate of trophic lesions increases from 1.7% to 10.6%, depending on JSF function.
Taking the results of three epidemiological studies conducted in the United States together, it was concluded that approximately 15-25% of the population has varicose veins, with greater prevalence among women and the elderly. One of these studies,27
conducted in the San Diego area in 2003, assessed 2,211 participants with Doppler ultrasonography to determine whether they had functional disease and to correlate it with presence of visible venous changes, detecting an incidence of varicose veins equating to 23.3% of the sample. Additionally, the same study also observed that, when assessed with Doppler ultrasonography, 19% of the total sample had supericial functional disease. In the National Venous Screening Program,28 23% of 2,234 people analyzed
had varicose veins. In the Tecumseh Community Health Study,29 25.9% of female participants and
12.9% of males were diagnosed with varicose veins. While this is not an epidemiological study, the results observed were not similar to those of previous studies to the extent that in the groups in which patients had varicose veins (group II - asymptomatic, and group III - symptomatic) the incidence of GSV with relux was 11.1% and 38.7% respectively.
The results of this study are in agreement with
authors26 who have described presence of varicose
veins without GSV relux as being more frequent in younger people and have observed that JSF and GSV
incompetence with symptoms are more common
In agreement with those authors, and on the basis of the indings of this study, we believe that venous insuficiency should be treated early, before symptoms and physiological deterioration occur.
CONCLUSIONS
Among patients who had visible varicose veins in lower limbs and were symptomatic (group III), there was a greater frequency of GSV incompetence (p < 0.01) in all subsets and both sexes. The frequency of GSV incompetence was also higher in patients with BMI ≥ 30 (male) and ≥ 25 (female) and had a signiicantly greater incidence in the age group from 30 to 50 years. In the age group > 50, incidence was only higher among females, whereas among males the difference was not signiicant. However, it should be borne in mind that the number of male patients in this age group was small.
REFERENCES
1. Morbio AP, Sobreira ML, Rollo HA. Correlation between the intensity of venous reflux in the saphenofemoral junction and morphological changes of the great saphenous vein by duplex scanning in patients with primary varicosis. Int Angiol. 2010;29(4):323-30. PMid:20671650.
2. Marston WA. Evaluation of varicose veins: what do the clinical signs and symptoms reveal about the underlying disease and need for intervention? Semin Vasc Surg. 2010;23(2):78-84. PMid:20685561. http://dx.doi.org/10.1053/j.semvascsurg.2010.01.003. 3. Mendoza E, Blättler W, Amsler F. Great saphenous vein diameter
at the saphenofemoral junction and proximal thigh as parameters of venous disease class. Eur J Vasc Endovasc Surg. 2013;45(1):76-83. PMid:23219416. http://dx.doi.org/10.1016/j.ejvs.2012.10.014. 4. Malgor RD, Labropoulos N. Diagnosis and follow-up of varicose
veins with duplex ultrasound: how and why? Phlebology. 2012;27(Suppl):10-5.
5. Malgor RD, Labropoulos N. Diagnosis of venous disease with duplex ultrasound. Phlebology. 2013;28 (Suppl):158-61. 6. Agresti A. An introduction to categorical data analysis. 2th ed.
New York: Wiley; 2007. 372 p.
7. Carpentier PH, Poulain C, Fabry R, Chleir F, Guias B, Bettarel-Binon C. Ascribing leg symptoms to chronic venous disorders: the construction of a diagnostic score. J Vasc Surg. 2007;46(5):991-6. PMid:17980285. http://dx.doi.org/10.1016/j.jvs.2007.06.044. 8. Andreozzi GM, Signorelli S, Di Pino L, et al. Varicose symptoms
without varicoses veins: the hypotonic phlebopathy, epidemiology and pathophysiology: the acireale project. Minerva Cardioangiol. 2000;48(10):277-85. PMid:11195857.
9. Blaettler W, Amsler F, Mendoza E. The relative impact on leg symptoms of fears of getting varicose veins and of great saphenous vein reflux. Phlebology. 2013;28(7):347-52. PMid:22539539. 10. Seidel AC, Belczak CE, Campos MB, Campos RB, Harada DS. The
impact of obesity on venous insufficiency. Phlebology. 2015;30(7):475-80. PMid:25193821. http://dx.doi.org/10.1177/0268355514551087. 11. Seidel AC, Mangolim AS, Rossetti LP, Gomes JR, Miranda F Jr. Prevalência de insuficiência venosa superficial dos membros inferiores
em pacientes obesos e não obesos. J Vasc Bras. 2011;10(2):124-30. http://dx.doi.org/10.1590/S1677-54492011000200006. 12. Belczak CE, Godoy JM, Seidel AC, Ramos RN, Belczak SQ, Caffaro
RA. Influence of prevalent occupational position during working day on occupational lower limb edema. J Vasc Bras. 2015;14(2):153-60. http://dx.doi.org/10.1590/1677-5449.0079.
13. Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. 2005;15(3):175-84. PMid:15723761. http://dx.doi. org/10.1016/j.annepidem.2004.05.015.
14. Evans CJ, Fowkes FG, Ruckley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. J Epidemiol Community Health. 1999;53(3):149-53. PMid:10396491. http:// dx.doi.org/10.1136/jech.53.3.149.
15. Robertson L, Lee AJ, Evans CJ, et al. Incidence of chronic venous disease in the Edinburgh Vein Study. J Vasc Surg. 2013;1(1):59-67. PMid:26993896.
16. Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000;72(3):694-701. PMid:10966886.
17. World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation on obesity. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1-253. PMid:11234459. 18. Halls SB. The BMI gap, the body mass index difference between
men and women [Internet]. 2016 [citado 2016 mar 14]. Disponível em: http://halls.md/bmi-difference-men-women.
19. Jackson AS, Stanforth PR, Gagnon J, et al. The effect of sex, age and race on estimating percentage body fat from body mass index: the heritage family study. Int J Obes Relat Metab Disord. 2002;26(6):789-96. PMid:12037649.
20. Wellens RI, Roche AF, Khamis HJ, Jackson AS, Pollock ML, Siervogel RM. Relationships between the body mass index and body composition. Obes Res. 1996;4(1):35-44. PMid:8787936. http:// dx.doi.org/10.1002/j.1550-8528.1996.tb00510.x.
21. Wang J, Thornton JC, Burastero S, et al. Comparisons for body mass index and body fat percent among Puerto Ricans, blacks, whites and Asians living in New York area. Obes Res. 1996;4(4):377-84. PMid:8822762. http://dx.doi.org/10.1002/j.1550-8528.1996. tb00245.x.
22. National Heart, Lung, and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Bethesda: NHLBI; 1998. Report No.: 98-4083.
23. Engelhorn CA, Engelhorn ALV, Cassou MF, Salles-Cunha S. Patterns of saphenous venous reflux in women presenting with lower extremity telangiectasias. Patterns of Saphenous Venous Reflux in Women Presenting with Lower Extremity Telangiectasias Dermatol Surg. 2007;33(3):282-8. PMid:17338684.
24. Labropoulos N, Tiongson J, Pryor L, et al. Definition of venous reflux in lower-extremityVeins. J Vasc Surg. 2003;38(4):793-8. PMid:14560232. http://dx.doi.org/10.1016/S0741-5214(03)00424-5. 25. Matić PA, Vlajinac HD, Marinković IM, Maksimović MŽ, Radak DI. Chronic venous disease: correlation between ultrasound findings and the clinical, etiologic, anatomic and pathophysiologic classification. Phlebology. 2014;29(8):522-7. PMid:23858025. http:// dx.doi.org/10.1177/0268355513497360.
27. Criqui MH, Jamosmos M, Fronek A, et al. Chronic venous disease in an ethnically diverse population: the San Diego Population Study. Am J Epidemiol. 2003;158(5):448-56. PMid:12936900. http:// dx.doi.org/10.1093/aje/kwg166.
28. McLafferty RB, Passman MA, Caprini JA, et al. Increasing awareness about venous disease: the American Venous Forum expands the National Venous Screening Program. J Vasc Surg. 2008;48(2):394-9. PMid:18572373. http://dx.doi.org/10.1016/j.jvs.2008.03.041. 29. Coon WW, Willis PW 3rd, Keller JB. Thromboembolism and
other venous disease in the Tecumseh health study. Circulation. 1973;48(4):839-46. PMid:4744789. http://dx.doi.org/10.1161/01. CIR.48.4.839.
*
Correspondence Amélia Cristina Seidel Rua Dr. Gerardo Braga, 118 - Jardim Vila Rica CEP 87050-610 - Maringá (PR), Brazil Tel.: +55 (44) 3026-7590 E-mail: amelia_seidel@hotmail.com
Author information ACS - Vascular sonographer from Sociedade Brasileira de Angiologia e Cirurgia Vascular (SBACV) and Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR); Associate Professor, Disciplina de Angiologia e Cirurgia Vascular, Curso de Medicina, Universidade Estadual de Maringá (UEM). MBC and RBC - Resident Physicians (Clinical Medicine), Universidade Estadual de Campinas (UNICAMP). DSH - Resident Physician (Occupational Medicine), Universidade de São Paulo (USP). RMR - Adjunct Professor, Departamento de Estatística, Universidade Estadual de Maringá (UEM). PCJ - Medical student (6th year), Universidade Estadual de Maringá (UEM). FMJ - Vascular sonographer from SBACV and CBR; Full Professor, Disciplina de Cirurgia Vascular, Departamento de Cirurgia, Escola Paulista de Medicina, Universidade Federal de São Paulo (UNIFESP).
Author contributions Conception and design: ACS Analysis and interpretation: RMR, ACS, FMJ, PCJ Data collection: ACS, PCJ Writing the article: ACS, MBC, RBC, DSH, PCJ Critical revision of the article: FMJ, ACS, RMR Final approval of the article*: ACS, FMJ, RMR, PCJ, MBC, RBC, DSH Statistical analysis: RMR Overall responsibility: ACS