www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
The
importance
of
retesting
the
hearing
screening
as
an
indicator
of
the
real
early
hearing
disorder
夽
,
夽夽
Daniela
Polo
Camargo
da
Silva
a,b,∗,
Priscila
Suman
Lopez
b,
Georgea
Espíndola
Ribeiro
a,b,
Marcos
Otávio
de
Mesquita
Luna
c,
João
César
Lyra
d,
Jair
Cortez
Montovani
eaSecretariatofHealthoftheStateofSaoPaulo,SãoPaulo,SP,Brazil
bGraduateProgram,GeneralBasicSurgery,BotucatuMedicineSchool,UniversidadeEstadualPaulista(UNESP),Botucatu,
SP,Brazil
cNeonatology,BotucatuMedicineSchool,UniversidadeEstadualPaulista(UNESP),Botucatu,SP,Brazil dBotucatuMedicineSchool,UniversidadeEstadualPaulista(UNESP),Botucatu,SP,Brazil
eDepartmentofOphthalmology,OtorhinolaryngologyandHeadandNeckSurgery,BotucatuMedicineSchool,
UniversidadeEstadualPaulista(UNESP),Botucatu,SP,Brazil
Received15January2014;accepted4July2014 Availableonline9June2015
KEYWORDS
Hearing;
Acousticstimulation; Newborn;
Neonatalscreening
Abstract
Introduction:Early diagnosisofhearinglossminimizesitsimpactonchilddevelopment.We studiedfactorsthatinfluencetheeffectivenessofscreeningprograms.
Objective: Toinvestigatetherelationshipbetweengender,weightatbirth,gestationalage,risk factorsforhearingloss,venuefornewbornhearingscreeningand‘‘pass’’and‘‘fail’’resultsin theretest.
Methods: Prospectivecohortstudywascarriedoutinatertiaryreferralhospital.Thescreening wasperformedin565newbornsthroughtransientevokedotoacousticemissionsinthree admis-sionunitsbeforehospitaldischargeandretestintheoutpatientclinic.Gender,weightatbirth, gestational age,presenceofriskindicators for hearingloss andvenuefor newbornhearing screeningwereconsidered.
Results:Full-terminfantscomprised86%ofthecases,preterm14%,andriskfactorsforhearing losswereidentifiedin11%.Consideringthe165newbornsretested,onlythevenueforscreening, IntermediateCareUnit,wasrelatedto‘‘fail’’resultintheretest.
夽 Pleasecitethisarticleas:daSilvaDPC,LopezPS,RibeiroGE,LunaMOM,LyraJC,MontovaniJC.Theimportanceofretestingthehearing screeningasanindicatoroftherealearlyhearingdisorder.BrazJOtorhinolaryngol.2015;81:363---7.
夽夽Institution:BotucatuMedicineSchool,UniversidadeEstadualPaulista(UNESP),Botucatu,SP,Brazil. ∗Correspondingauthor.
E-mail:daniela-polo@uol.com(D.P.C.daSilva).
http://dx.doi.org/10.1016/j.bjorl.2014.07.019
1808-8694/©2015Associac¸ãoBrasileirade OtorrinolaringologiaeCirurgiaCérvico-Facial.Published byElsevierEditoraLtda.Allrights
Conclusions:Gender,weightatbirth,gestationalageandpresenceofriskfactorsforhearing losswerenotrelatedto‘‘pass’’and/or‘‘fail’’resultsintheretest.Thescreeningperformed inintermediatecare unitsincreasesthechanceofcontinued‘‘fail’’ resultintheTransient OtoacousticEvokedEmissionstest.
© 2015Associac¸ãoBrasileira de Otorrinolaringologiae CirurgiaCérvico-Facial. Publishedby ElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Audic¸ão;
Estimulac¸ãoacústica; Recém-nascido; Triagemneonatal
Aimportânciadoretestedatriagemauditivacomoindicadordarealalterac¸ão auditivaprecoce
Resumo
Introduc¸ão:Odiagnósticoprecocedasurdezminimizaimpactosnodesenvolvimentoinfantil. Fatoresqueinterferemnaefetividadedosprogramasdetriagemsãoestudados.
Objetivo:Verificararelac¸ãoentresexo,pesoaonascimento,idadegestacional,presenc¸ade riscopardeficiênciaauditiva,local derealizac¸ãodatriagem auditivaneonatale resultados ‘‘passa’’e‘‘falha’’noreteste.
Método: Estudodecoorteprospectiva,emhospitaldereferênciaterciário.Atriagemfoi real-izada em 565 neonatos,por meio dasemissões otoacústicas evocadas transientes, em três unidades deinternac¸ãoantesdaaltahospitalareoreteste,noambulatório.Sexo,peso ao nascimento,idadegestacional, presenc¸a deindicadoresderiscopara deficiênciaauditivae localderealizac¸ãodoexameforamconsiderados.
Resultados: Nascerama termo 86%,prematuros14% e riscopara deficiênciaauditiva,11%. Dentreos165neonatosretestados,apenasolocalderealizac¸ãodoexame,UnidadedeCuidados Intermediários,serelacionoucommanutenc¸ãoda‘‘falha’’noreteste.
Conclusões:Sexo,pesoaonascimento,idadegestacionalepresenc¸adeindicadoresderisco para deficiência auditiva não se relacionaram com ‘‘passar’’ e/ou ‘‘falhar’’ no reteste. A realizac¸ãodoexameemunidadesdecuidadosintermediáriosaumentaachancedepermanência de‘‘falha’’noexamedeEmissõesOtoacústicasEvocadasTransientes.
©2015Associac¸ãoBrasileira deOtorrinolaringologiaeCirurgiaCérvico-Facial.Publicadopor ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
With the use of electrophysiological and electroacoustic testsinchildren,theearlydiagnosisforhearinglossbecame apossibilityinthefirstmonthsoflife,throughtheuniversal newbornhearingscreening(UNHS).1InBrazil,UNHSbecame
mandatoryforallnewbornsbyFederalLawNo.12,303. Severalfactorsareimportantfor agoodunderstanding andeffectivenessofUNHStesting;theseincludetestsite, clinicalconditionsofthenewborn,andperformingthetest priortohospitaldischarge. Inaddition,in at least90% of thosewhofailthefirstUNHSexam,aretestshouldbe per-formed, either beforehospital discharge, or by the third monthoflife.2
Inabilitytoachievethisrecommendedstandardcanoccur forreasonsinherenttoneonates,suchasdeath,postnatal illnessandhospitalizationinanotherunit,orbylackof fam-ilycompliance.Thus,thechallengeofreducingthenumber offailuresintheinitialexaminationandalsothechallenge ofavoidingnon-attendanceofthesechildrenforretestare stillgoodreasonsforstudyingthistopic.3---5Theaimofthis
studywastoinvestigatethe relationshipbetween gender, birthweight,gestational age,presence of riskfactors for
hearing loss,site where UNHSis carried out,and ‘‘pass’’ and‘‘fail’’resultsintheretest.
Methods
The study was conducted in a tertiary referral hospital, withlocalEthicsCommitteeapproval(ProcessNo.3395/09), fromSeptember2011toJune2012.TheFreeandInformed ConsentFormwassignedbytheparentorlegalguardianof thenewborn.
Thiswasaprospectivecohortstudy.
Duringthestudyperiod,565neonatesunderwentUNHS inthreedifferentunitsofhospitalization:neonatal rooming-in (NRI), special care unit (ECU) and intermediate care unit (ICU), before hospital discharge. Forbabies withan abnormalinitialexamination,retestingwasperformedinan outpatient speechtherapy clinic after hospital discharge. Hearing screening was performed by means of transient evoked otoacoustic emissions, using portable equipment (OtoRead/Interacoustics), withthe newborn in a state of naturalsleepinitsmother’slap,orinthecradle.
stimuli at an intensity of 83dB SPL; six frequency bands (1500---4000Hz)were evaluated. The valuesconsidered as ‘‘PASS’’wereotoacousticemissionspresentinasignal/noise ratioof6dBinatleastthreeconsecutivefrequencybands, including4000Hz,andamaximum timeof64s toperform thetest.
The variables of gender, birth weight,gestational age, presenceofriskfactorsforhearingloss2andtestsite(NRI,
ECU and ICU) were considered in the statistical analysis ofneonateswith‘‘failure’’ intheirinitialevaluation. Chi-squared andFisher’sexact testswere used.Analyseswere consideredsignificantifp≤0.05.Inthestatisticalanalysis,
SPSSsoftwareversion21.0wasused.
Results
Beforehospitaldischarge,565 neonatesunderwentUNHS; 48%(n=270)werefemaleand52%(n=295)weremale.The averagebirthweightwas3663g(minimumof695gand max-imumof 4700g). Regarding gestationalage, 86% (n=484) werebornatterm,and14%(n=81)werepremature.
Riskfactorsforhearinglosswerepresentin11%(n=65) ofthe neonates.A lowApgar scoreat birth(n=24),birth weight<1500g(n=11),ICU>48h(n=10),mechanical venti-lationinexcessoffivedays(n=6),congenitalsyphilis(n=6), use of ototoxic drugs (n=4), child of drug-user mother (n=3), craniofacial malformation(n=2), congenital toxo-plasmosis(n=1)andfamilyhistoryofhearinglossinchildren (n=1)weretheriskfactors.
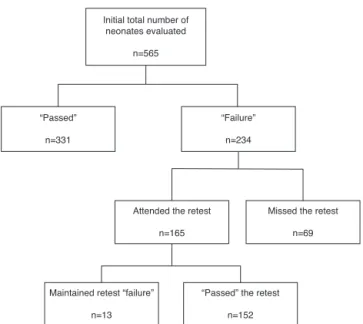
As shown in the flowchart of Fig. 1, 59% of neonates (n=331)‘‘passed’’intheinitialevaluation.Amongthe234 neonates who ‘‘failed’’, 30% (n=69) did not attend the retest,resultinginreassessmentof165 neonates,only8% ofwhom(n=13)confirmedtheinitial‘‘failure’’.
The relationship amongthevariables gender, prematu-rity,presenceofriskfactorsforhearingloss,examsite,and
Initial total number of neonates evaluated
n=565
“Passed”
n=331
Attended the retest
n=165
Maintained retest “failure”
n=13
“Passed” the retest
n=152
Missed the retest
n=69 “Failure”
n=234
Figure1 Flowchartofpatientsseenduringthestudyperiod (n,number).
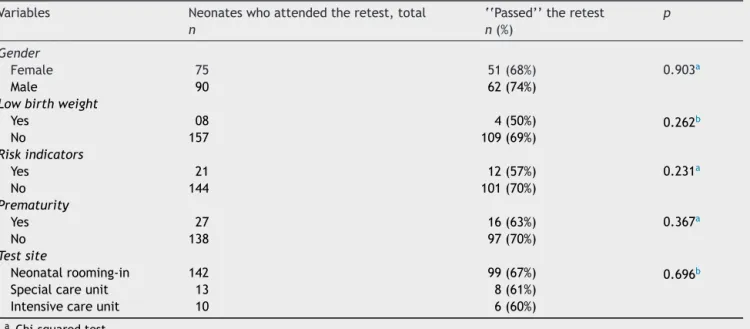
a‘‘pass’’ onthe retest wasnotstatistically significant in bothears(Tables1and2).
Ontheotherhand,theratiobetweenthesesame varia-bles andthe persistence of ‘‘failure’’ onthe retest in at leastoneearwassignificantwhenthefirstexaminationwas carriedoutattheintermediatecareunit(Table3).
Discussion
Hearingassessment in the firstdaysof life thatidentifies hearingloss can result in a betterprognosis for language development; the first months of life are considered a
Table1 Relationshipbetween‘‘topass’’theretestontherightearandthefollowingvariables:gender,lowbirthweight,risk factors,prematurityandtestsite.
Variables Neonateswhoattendedtheretest,total ‘‘Passed’’theretest p
n n(%)
Gender
Female 75 46(61%) 0.071a
Male 90 67(74%)
Lowbirthweight
Yes 08 5(62%) 0.708b
No 157 108(69%)
Riskindicators
Yes 21 13(62%) 0.487a
No 144 100(69%)
Prematurity
Yes 27 20(74%) 0.647b
No 138 93(67%)
Testsite
Neonatalrooming-in 142 95(67%) 0.141b
Specialcareunit 13 12(92%)
Intensivecareunit 10 6(60%)
a Chi-squaredtest.
Table2 Relationshipbetween‘‘topass’’theretestontheleftearandthefollowingvariables:gender,lowbirthweight,risk factors,prematurityandtestsite.
Variables Neonateswhoattendedtheretest,total ‘‘Passed’’theretest p
n n(%)
Gender
Female 75 51(68%) 0.903a
Male 90 62(74%)
Lowbirthweight
Yes 08 4(50%) 0.262b
No 157 109(69%)
Riskindicators
Yes 21 12(57%) 0.231a
No 144 101(70%)
Prematurity
Yes 27 16(63%) 0.367a
No 138 97(70%)
Testsite
Neonatalrooming-in 142 99(67%) 0.696b
Specialcareunit 13 8(61%)
Intensivecareunit 10 6(60%)
aChi-squaredtest.
b Fisher’sexacttest.
criticalperiodof maturation andplasticity of thecentral auditorysystem.6,7
For an early identification of deafness, the use of objectivemeasures such as recording evoked otoacoustic emissionsandbrainstem auditoryevokedpotential(BAEP) isrecommended.2,7 However,onalarge scale,Brazil
util-izesevokedotoacousticemissionsasafirstdiagnosticstep and,afteraconfirmed‘‘failure’’ofthistest,employsBAEP tosubstantiatethediagnosis.1,4
Withconfirmationofdeafness,thesechildrenshouldbe submittedtoearly interventionthroughindividualhearing aidadaptation/cochlearimplant,andspeechtherapy;these
shouldbeimplementedbythesixthmonthoflife.2
There-fore,hearingscreeningisrecommended,preferablybefore hospitaldischarge.8---11
However, in the very first days of life before dis-charge fromthehospital,therearesome factorsthatcan cause a UNHS test ‘‘failure’’ such as an elevated ambi-ent noise level in inpatient units, the clinical conditions of thenewborn,or thepresenceof vernixintheexternal auditory canal.4,12 But in the retest, when test
condi-tionsarebetter,itis possibletoverifythatthe‘‘failure’’ was due to a hearing problem, and not to unrelated factors.
Table3 Relationshipbetweenmaintenanceofretest‘‘failure’’inatleastoneearandthefollowingvariables:gender,low birthweight,riskfactors,prematurityandtestsite.
Variables Neonateswhoattendedtheretest,total ‘‘Passed’’theretest p
n n(%)
Gender
Female 75 9(12%) 0.087
Male 90 4(04%)
Lowbirthweight
Yes 08 4(50%) 0.262
No 157 109(69%)
Riskindicators
Yes 21 4(19%) 0.065
No 144 9(06%)
Prematurity
Yes 27 4(15%) 0.230
No 138 9(06%)
Testsite
Neonatalrooming-in 142 9(06%)a 0.039a
Specialcareunit 13 1(08%)a
Intensivecareunit 10 3(30%)b
Sinceoursisateachinghospitalwithalargenumberof birthspermonth,differentinpatientunitsforthenewborn wereconsidered in this study.Ourhospitalhas four inpa-tient units. NRI comprises healthy neonates, ECU houses neonateswithanyofthefollowingfactors:lowbirthweight (<2000g), gestationalage less than 34 weeks, respiratory distresswithoutimmediateneedforintubationand mechan-icalventilation,orneonates whosemothers areunableto care for their children in the NRI, soon after birth. ICU receives newborns who need monitoring, but who do not requirecare inaneonatalintensivecareunit(ICU),which isresponsibleonlyforseverecases.
This study shows that 92% of newborns ‘‘passed’’ the retest,anindexveryclosetothatrecommendedbyJCIH,2
eventhough itoccurredinahospitalthatserves pregnant womenandinfantsathighriskforhearingloss.
Thelossof30%inthepopulationappropriateforretest canbeexplainedinpartbyanincreaseofneonatalhearing screening programsin the cities of origin, thatgives par-entsanoptionwitheasieraccess.Also,high-riskpregnancies increase the possibility of readmission of these neonates that would preventtheir return. The lack of recognition, orevenofunderstanding,oftheimportanceofthehearing testis commonandmayalsohave animpactontheearly identificationofdeafness.
Although the presence of risk factors for hearing loss and prematurity increases the chances of ‘‘failure’’ on UNHS,13,14 our study found no relationship between these
factorsand thepersistence of‘‘failure’’ onretest, butit didfinda correlationwithexam site,especiallyfor those babieswhounderwent theinitial examination in theICU. This finding may be explained by the fact that neonates that remained in this unit are those presenting major complicationsbefore,duringand/orafterbirth.
This studyaddressedthe importanceofcompleting the retest of otoacoustic emissions, but does not rule out a referraltoBAEP,orevencarryingoutBAEPasafirststep, especiallyinneonatesatriskforhearingloss.However,the practiceofconductingotoacousticemissiontests,mainlyin theretest,reducedthenumberoffalsepositives,especially when the initial assessment wasconducted in in-hospital criticalenvironments.
Thechildrenassessedinthisstudy,afterconfirmationof retest‘‘failure’’, werereferred fordiagnostic evaluation; and,after confirmationof hearing loss,were referredfor medicalandaudiologictreatment.
Even considering that the conditions for carrying out screening procedures before hospital discharge are not ideal, the retest is essential for an early identification ofthe baby’sactual hearingimpairment,emphasizing the importance of investing in factors that contribute to the adherencetoretest,for example,educationofthose pro-fessionalsinvolvedinmaternalandchildhealthandinfamily counseling.
Conclusion
Gender,birthweight,gestationalageandpresenceofrisk factorsforhearinglosswerenotrelatedto‘‘topass’’and/or
‘‘tofail’’theretest.Theexaminationcarriedoutin inter-mediatecare units increases the chances of permanence of‘‘failure’’ in thetransient evokedotoacoustic emission test.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.DuranteAS,CarvalhoRMM,CostaMTZ,CianciarulloMA,Voegels RL, TakahashiGM, et al. A implementac¸ão de programa de triagem auditiva neonatal universal em um hospital univer-sitáriobrasileiro.Pediatria.2004;26:78---84.
2.JointCommitteeonInfantHearing.AmericanAcademyof Pedi-atrics.Year2007positionstatement.Principlesandguidelines for earlyhearingdetection and interventionprograms. Pedi-atrics.2007;120:898---921.
3.Shulman S, Besculides M, Saltzman A, Ireys H, White KR, Forsman I. Evaluation of the universal newborn hearing screening and intervention program. Pediatrics. 2010;126 Suppl.1:S19---27.
4.SimonekMCS,AzevedoMF.Respostasfalso-positivasnatriagem auditiva neonatal universal: possíveis causas. Rev CEFAC. 2011;13:292---8.
5.Alvarenga KF, Gadret JM, Araújo ES, Bevilacqua MC. New-born hearing screening: reasons for the evasion of families in the process ofearly detection. Rev Soc BrasFonoaudiol. 2012;17:241---7.
6.VieiraABC,MacedoLR,Gonc¸alvesDV.Odiagnósticodaperda auditivanainfância.Pediatria.2007;29:43---9.
7.LewisDR, MaroneSAM, MendesBCA, Cruz OLM,Nóbrega M. Comitê multiprofissional em saúde auditiva COMUSA. Braz J Otorhinolaringol.2010;76:121---8.
8.Almenar LatorreA, TapiaTocaMC,FernándezPérezC,Moro SerranoM.Acombinedneonatalhearingscreeningprotocol.An EspPediatr.2002;57:55---9.
9.Böhrer MAS. Triagem auditiva neonatal. Correios da SBP. 2002;8:5---7.
10.Díez-Delgado Rubio J, Espín Gálvez J, Lendinez Molinos F, OrtegaMontesMMA,ArcosMartínezJ,López MunõzJ. Hear-ingscreeningwithevokedotoacousticemissionintheneonatal periodarelogisticallyandeconomicallyfeasible.AnEspPediatr. 2002;57:157---62.
11.Durante AS, Carvalho RMM, Costa MTZ, Cianciarullo MA, VoegelsRL,TakahashiGN,etal.Programadetriagemauditiva neonatal --- modelo de implementac¸ão. Arq Otorrinolaringol. 2004;8:56---63.
12.HilúMRPB,ZeigelboimBS.Oconhecimento,a valorizac¸ãoda triagemauditiva neonataleaintervenc¸ãoprecocedaperda auditiva.RevCEFAC.2007;9:563---70.
13.KorresS,NikolopoulosTP,KomkotouV,BalatsourasD,Kandiloros D,Constantinou D,et al.Newborn hearingscreening: effec-tiveness,importanceof high-riskfactors,and characteristics of infantsinthe neonatalintensive care unit and well-baby nursery.OtolNeurotol.2005;26:1186---90.