w w w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
Brazilian
multicenter
study
of
71
patients
with
juvenile-onset
Takayasu’s
arteritis:
clinical
and
angiographic
features
夽
Gleice
Clemente
a,
Maria
Odete
Hilário
a,
Claudio
Len
a,
Clovis
A.
Silva
b,
Adriana
M.
Sallum
b,
Lúcia
M.
Campos
b,
Silvana
Sacchetti
c,
Maria
Carolina
dos
Santos
c,
Andressa
Guariento
Alves
c,
Virgínia
P.
Ferriani
d,
Flávio
Sztajnbok
e,
Rozana
Gasparello
e,
Sheila
Knupp
Oliveira
f,
Marise
Lessa
f,
Blanca
Bica
g,
André
Cavalcanti
h,
Teresa
Robazzi
i,
Marcia
Bandeira
j,
Maria
Teresa
Terreri
a,∗aSectorofPediatricRheumatology,DepartmentofPediatrics,UniversidadeFederaldeSãoPaulo,SãoPaulo,SP,Brazil
bPediatricRheumatologySector,InstitutodaCrianc¸a,UniversidadedeSãoPaulo,SãoPaulo,SP,Brazil
cSantaCasadeMisericórdiadoSãoPaulo,SãoPaulo,SP,Brazil
dMedicineSchool,UniversidadedeSãoPaulo,RibeirãoPreto,SP,Brazil
eUniversidadedoEstadodoRiodeJaneiro,RiodeJaneiro,RJ,Brazil
fInstitutodePediatriaMartagãoGesteira,UniversidadeFederaldoRiodeJaneiro,RiodeJaneiro,RJ,Brazil
gRheumatologyUnit,UniversidadeFederaldoRiodeJaneiro,RiodeJaneiro,RJ,Brazil
hRheumatologyUnit,UniversidadeFederaldePernambuco,Recife,PE,Brazil
iUniversidadeFederaldaBahia,Salvador,BA,Brazil
jHospitalPequenoPríncipe,Curitiba,PR,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received5December2014 Accepted5September2015 Availableonline18February2016
Keywords:
Takayasu’sarteritis Child
Teenager Image
a
b
s
t
r
a
c
t
Objective:TodescribetheclinicalandangiographiccharacteristicsofTakayasu’sarteritisin Brazilianchildrenandadolescents.
Methods:A retrospectivedata collectionwasperformedin 71 childrenandadolescents followedin10BrazilianreferencecentersinPediatricRheumatology.Theevaluationwas carriedoutinthreedifferenttimepoints:fromonsetofsymptomstodiagnosis,fromthe 6thto12thmonthofdiagnosis,andinthelastvisit.
Results:Of71selectedpatients,51(71.8%)weregirls.Themeanageofonsetofsymptoms andoftimetodiagnosiswas9.2(±4.2)yearsand1.2(±1.4)years,respectively.Attheendof thestudy,20patientswereinastateofdiseaseactivity,39inremissionand5hadevolvedto death.Themostcommonsymptomsinbaselineassessment,secondevaluation,andfinal evaluationwere,respectively:constitutional,musculoskeletal,andneurologicalsymptoms.
夽
StudylinkedtotheSectorofPediatricRheumatology,DepartmentofPediatrics,UniversidadeFederaldeSãoPaulo(UNIFESP),São Paulo,SP,Brazil.
∗ Correspondingauthor.
E-mail:teterreri@terra.com.br(M.T.Terreri).
http://dx.doi.org/10.1016/j.rbre.2016.01.004
Adecreaseinperipheralpulseswasthemostfrequentcardiovascularsignal,andanincrease inerythrocytesedimentationratewasthemostfrequentlaboratoryfindinginallthree evaluationperiods.Thetuberculintestwaspositivein41%ofthosetested.Stenosiswas themostfrequentangiographiclesion,abdominalarterywasthemostaffectedsegment, andangiographic typeIVthemostfrequent.Most(90%)participantsweretreatedwith glucocorticoids,85.9%requiredanotherimmunosuppressivedrug,and29.6%underwent angioplasty.
Conclusion:Thisisthelargeststudyonjuvenile-onsetTakayasuarteritis,andahighnumber ofpatientsundertheageof10years,withpredominanceofconstitutionalsymptomsearly inthedisease,wasobserved.
©2016ElsevierEditoraLtda.Allrightsreserved.
Estudo
multicêntrico
brasileiro
de
71
pacientes
com
arterite
de
Takayasu
juvenil:
características
clínicas
e
angiográficas
Palavras-chave: ArteritedeTakayasu Crianc¸a
Adolescente Imagem
r
e
s
u
m
o
Objetivo: DescreverascaracterísticasclínicaseangiográficasdaarteritedeTakayasuem crianc¸aseadolescentesbrasileiros.
Métodos: Foirealizadacoletaretrospectivadedadosde71crianc¸aseadolescentes acom-panhadosem10centrosbrasileirosdereferênciaemreumatologiapediátrica.Aavaliac¸ão foifeitaem3temposdiferentes:iníciodossintomasatéodiagnóstico,do6◦ao12◦mêsde diagnósticoeúltimaconsulta.
Resultados: Dos71pacientesselecionados,51(71,8%)erammeninas.Asmédiasdeidade deiníciodossintomasedetempoatédiagnósticoforam9,2anos(±4,2)e1,2anos(±1,4), respectivamente.Nofinaldoestudo,20pacientesestavamematividadededoenc¸a,39em remissãoe5haviamevoluídoaoóbito.Ossintomasmaisfrequentesnasavaliac¸ãoinicial, segundaavaliac¸ãoeavaliac¸ãofinalforam,respectivamente:osconstitucionais,os muscu-loesqueléticoseosneurológicos.Areduc¸ãodepulsosperiféricosfoiosinalcardiovascular maisfrequenteeaelevac¸ãodavelocidadedehemossedimentac¸ãofoioachadolaboratorial maisfrequentenostrêsperíodosdeavaliac¸ão.Otestetuberculínicofoireagenteem41% daquelesqueorealizaram.Aestenosefoialesãoangiográficamaisencontrada,aartéria abdominalfoiosegmentomaisafetadoetipoangiográficoIVomaisfrequente.Amaioria (90%)fezterapiacomglicocorticoides,85,9%necessitoudeoutroimunossupressore29,6% foisubmetidoàangioplastia.
Conclusão: EsteéomaiorestudodearteritedeTakayasujuvenilenóspudemosobservar elevadonúmerodepacientescomidadeinferiora10anoseapredominânciadesintomas constitucionaisnoiníciodadoenc¸a.
©2016ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Takayasu’s arteritis (TA) is achronic vasculitis that affects
large-and medium-caliber arteriesand is accompaniedby
highmorbidity,duetoanimpairedbloodsupplytoorgansand limbs.Thediseaseisrareandaffectspredominantlyyoung femaleadults,beingmostprevalentinEastAsiancountries. ThismakesTAapoorlycharacterizeddiseaseinthepediatric population, particularlyin Westerncountries. The descrip-tions of the disease in the pediatric population, including infants,hasincreasedinrecentdecades,oftenreaching32% ofpatientsagedunder20years.1–5
Clinical signs and symptoms found in patients with
juvenile-onset TAare similarto those found inadults, for
instance, the presence of constitutional, neurological and musculoskeletalsymptoms,highbloodpressure,adecreaseof peripheralpulsesandpresenceofvascularmurmur.However, theinitialclinicalmanifestationsseemtobemoreinsidious and nonspecificinchildren.4,6–9 Thismaycontributetothe greaterdelayofdiagnosisinthepediatricagegroup,whichis uptofourtimeshigherthanthatforadults.2
Theworldliteratureonjuvenile-onsetATarescarce,being
derived from specific populations with small numbers of
Patients
and
methods
ThisisaBrazilianmulticenterstudyonclinical,angiographic andtherapeuticcharacteristicsofpatientsagedunder19years withadiagnosisofTA.Datacollectionwascarriedoutbetween the2010and2011throughasearchofmedicalrecords.
Centersinvolved
FifteenBraziliantertiarymedicalcentersofreferencein Pedi-atricRheumatologywereinvitedtoparticipateinthisstudy. Centerswithatleastthreepatientswithjuvenile-onset TA whofulfilledtheclassificationcriteriaofthedisease10were included.Thestudyincluded10Braziliancentersofthree dif-ferentgeographicregions,includingthecoordinatingcenter.
Participatingpatients
Patients with incomplete relevant data were excluded (2
patients).Thestudyincluded 71patientsfollowed between
1988 and 2011 with a diagnosis of juvenile-onset TA. The
diagnosiswasestablishedbasedonclinicalfindingsand angi-ographicimagescompatiblewiththedisease,withexclusion ofotherpossiblecauses;andallpatientsmettheclassification criteriaforpediatricTakayasu’sarteritis.10
Questionnaire
A detailed questionnaire containing demographic, clinical, laboratory, angiographic and therapeuticdata wasapplied. Thesedatawerecollectedatthreedifferenttimepoints, in ordertoallowalongitudinalfollow-up ofpatients, making easierthedatacollectionbytheheadofeachparticipating center.Thequestionnairewascomposedof4Excel® spread-sheetsdividedasfollows:baselineassessment(referringto
data from the onset of symptoms to diagnosis
establish-ment);a secondevaluation(for datacollected betweenthe 6thand12thmonthofdiagnosis);finalassessment(referring to data of the last visit and last examination); and treat-ment(referringtotherapyperformedduringfollow-up).This
questionnaire, along with a Word® document with
expla-nations of how to properly fill out the information and
standardize the responses, was emailed by the
coordinat-ingcenter tothedoctorsresponsible foreach participating center.
Patientswereclassifiedaccordingtodiseaseactivityinthe lastsixmonthsofthefinalevaluation:diseaseinactivity,in remission,ordeath.Astherearenovalidatedcriteriafor defin-ingdiseaseactivityforpediatricpatientstodate,wedefined “disease activity” as the presence ofcharacteristic clinical
symptoms/signs of the disease and/or laboratory changes
(increases in erythrocyte sedimentation rate [VHS] and C-reactiveprotein[CRP],withexclusionofotherpossiblecauses forincreasesininflammatorytests)inthelastsixmonths;and “remission”astheabsenceofclinicalsigns/symptomsandof laboratorychanges inthelast 6monthsoffollow-up, with orwithoutpharmacologicalcare.Theangiographic examina-tionswerenotconsideredfortheevaluationofdiseaseactivity, duetothelargenumberofparticipatingcenterswithdifferent
imagingmodalities(conventionalangiography,CTAandMRA) andalsoduetothelargenumberofradiologistsinterpreting theimages.
AngiographictypesweredefinedaccordingtoHata’s angi-ographic classification, developed at the International TA ConferenceinTokyoin1994,asshowninFig.1.11
ThestudywasapprovedbytheEthicsCommitteeofthe
coordinatinginstitutionandbytheotherCommitteesofthe participatingcenters.
Results
Ofthe71patientsselectedforthestudy,51(71.8%)weregirls. Attheonsetofthedisease,36patients(50.7%)werechildren –youngerthan10years;and35(49.3%)wereteenagers–aged 10–19years,accordingtothedefinitionoftheWorldHealth
Organization. Themean ageatonsetofsymptomswas9.2
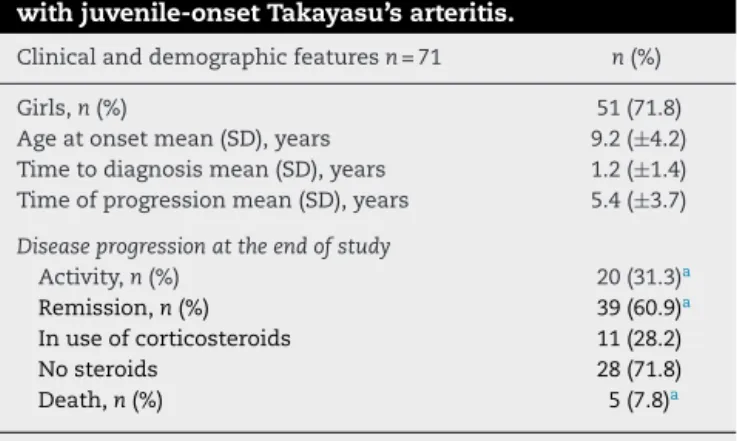
years(±4.2).Themeansfortimetodiagnosisandprogression timeofthediseasewere1.2(±1.4)yearsand5.4(±3.7)years, respectively.Attheendofthestudy,20patientswerewith theirdiseaseinactivity,39inremission(ofthese,11wereusing corticosteroids),and5died(Table1).Timetilldeathsincethe onsetoffollow-upwasone,two,sixand44months, respec-tively(thisinformationwasnotavailableforonepatient).The causesofdeathwereheartfailure,kidneyfailureandsurgical complications,andwecouldnotidentifythecausamortisof twopatients.
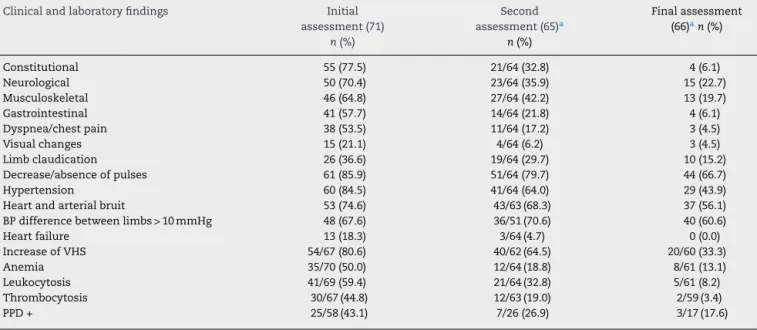
Clinicalfindings
Constitutionalsymptoms–fever,astheniaandweightloss– occurredin77.5%ofpatientsandwerethepredominant symp-toms atthe baseline assessment, followed byneurological –headache,stroke,andsyncope (70.4%)and musculoskele-tal – arthritis,arthralgia, and limbpain(64.8%) symptoms; inthesecondevaluation,themostfrequentsymptomswere musculoskeletal(42.2%),followedbyneurological(35.9%)and constitutional(32.8%)symptoms;andinthefinalevaluation,a
predominanceofneurologicalsymptoms(22.7%)wasfound,
Table1–Clinicalanddemographicfeaturesofpatients withjuvenile-onsetTakayasu’sarteritis.
Clinicalanddemographicfeaturesn=71 n(%)
Girls,n(%) 51(71.8)
Ageatonsetmean(SD),years 9.2(±4.2) Timetodiagnosismean(SD),years 1.2(±1.4) Timeofprogressionmean(SD),years 5.4(±3.7)
Diseaseprogressionattheendofstudy
Activity,n(%) 20(31.3)a
Remission,n(%) 39(60.9)a
Inuseofcorticosteroids 11(28.2)
Nosteroids 28(71.8)
Death,n(%) 5(7.8)a
n,numberofpatients.
a Valuesfor64patients,becauseinsevenwewerenotableto
Type
I
IIa
IIb
III
IV
V
Fig.1–Hata’sangiographicclassification.11
followedbymusculoskeletal–arthritis,arthralgia,andlimb pain (19.7%)and constitutional/gastrointestinal (6.1% each) symptoms(Table2).
Themostfrequentcardiovascularsignalwasadecrease/ absenceofperipheralpulsesinthethreeevaluationperiods, followedbyhighbloodpressureinthefirstevaluationandbya bloodpressuredifferenceinthesecondandthirdevaluations (Table2).
Laboratoryfindings
Regarding laboratorytests,ESRelevationwasthemost fre-quentfindinginallthreeevaluations,beingpresentinover 80%ofpatientsatbaselineassessment,withnormalizationof itsvalueinthemajorityofpatientsduringfollow-up. Tuber-culinskintestwasperformedin58patients,and25(43.1%)of themtestedpositive(Table2).
Table2–Clinicalandlaboratorydataofpatientswithjuvenile-onsetTakayasu’sarteritisatthethreeassessmenttime points.
Clinicalandlaboratoryfindings Initial assessment(71)
n(%)
Second assessment(65)a
n(%)
Finalassessment (66)an(%)
Constitutional 55(77.5) 21/64(32.8) 4(6.1)
Neurological 50(70.4) 23/64(35.9) 15(22.7)
Musculoskeletal 46(64.8) 27/64(42.2) 13(19.7)
Gastrointestinal 41(57.7) 14/64(21.8) 4(6.1)
Dyspnea/chestpain 38(53.5) 11/64(17.2) 3(4.5)
Visualchanges 15(21.1) 4/64(6.2) 3(4.5)
Limbclaudication 26(36.6) 19/64(29.7) 10(15.2)
Decrease/absenceofpulses 61(85.9) 51/64(79.7) 44(66.7)
Hypertension 60(84.5) 41/64(64.0) 29(43.9)
Heartandarterialbruit 53(74.6) 43/63(68.3) 37(56.1)
BPdifferencebetweenlimbs>10mmHg 48(67.6) 36/51(70.6) 40(60.6)
Heartfailure 13(18.3) 3/64(4.7) 0(0.0)
IncreaseofVHS 54/67(80.6) 40/62(64.5) 20/60(33.3)
Anemia 35/70(50.0) 12/64(18.8) 8/61(13.1)
Leukocytosis 41/69(59.4) 21/64(32.8) 5/61(8.2)
Thrombocytosis 30/67(44.8) 12/63(19.0) 2/59(3.4)
PPD+ 25/58(43.1) 7/26(26.9) 3/17(17.6)
ESR,erythrocytesedimentationrate;PPD,purifiedproteinderivative.
Constitutionalsymptoms:fever,astheniaandweightloss;neurologicalsymptoms:headache,stroke,syncope;musculoskeletalsymptoms: arthritis,arthralgia,limbpain;gastrointestinalsymptoms:abdominalpain,diarrhea,vomiting;visualchange:conjunctivalhyperemia,visual blurring,blindness,decreasedvisualacuity,uveitis.
a 6patientswerelosttofollow-upafterthediagnosisandoneofthemreturnedafter5years.
Table3–Angiographicclassificationofpatientswith juvenile-onsetTakayasu’sarteritis,accordingtoHata’s classification.11
Angiographicclassification n(%)
TypeI 8(11.9)
TypeIIa 4(6.0)
TypeIIb 1(1.5)
TypeIII 9(13.4)
TypeIV 27(40.3)
TypeV 18(26.9)
Thefrequencyofangiographictypesdescribedwasrelatedto67 patients,consideringthatfourpatientslackedfullinitial angiogra-phicdata.
During the baselineassessment, 47 patients underwent conventionalangiography,34MRAand16TCA.Imagingtests werenotperformedonaconsiderablenumberofpatientsin thesecond and thirdevaluations;inview ofthat, onlythe firststudieswereevaluated.Accordingtothestudyofimages takenatbaseline,achangeinabdominalaortawasthemost frequentfinding,and waspresentin67.2%ofpatients, fol-lowedbyrenalarteries(55.2%)andbysubclavianarteriesand descendingthoracicaorta (26.9%each);The mostfrequent typeofarterialinjurywasstenosis(89.6%)followedby obstruc-tion(28.4%),swelling(17.9%)andaneurysm(14.9%);andthe mostfrequentangiographictypewastypeIV,followedbytype V(Table3).Therewasnosignificantdifferencewithrespect toangiographictypesamongchildrenandadolescentswhen typesI, IIaand IIbwere gathered inagroup,and typesIII andIVinanothergroup,beingsubsequentlycomparedamong themselvesandagainstVgroup(p=0.624).
Astodrugtherapyperformedbypatientsduring follow-up,themajority(90.0%)madeuseoforalglucocorticoids,or intheformofpulsetherapy.Sixty-one(85.9%)patientsused
other immunosuppressive drugs (methotrexate,
cyclophos-phamide, azathioprine and mycophenolate) and only four
have used biological therapy (infliximab). Thirty patients
(42.3%) used methotrexateand 18 (25.4%) used
cyclophos-phamide as initial immunosuppressive medication.Of the
25 patients with apositive tuberculin skintest, 10 (40.0%) requiredthe introduction oftriple therapy dueto astrong suspicionoftuberculosis(clinicalfindings,chestradiography, bacilloscopy,orbiopsyorsputumculture),nine(36.0%)used isoniazidfortreatmentoflatenttuberculosis,andtwo(8.0%) hadbeentreatedforlatenttuberculosisinfection,andwere treatedwithtripletherapyatdifferentfollow-uptimes.Four (16.0%)patients, who were weakreactors,did notundergo treatmentwithtripletherapynorforlatentTB.Twopatients withanegativeresultfortuberculintestunderwenttreatment fortuberculosis(1)andforlatenttuberculosis(2),intheface oftheirpositiveepidemiology.Twenty-sevenpatients(38.0%) underwentsomekindofinterventionaltherapy,and angio-plastywasthe mostperformed procedure, in21 (77.8%)of thesepatients.Attheendofthisstudy,thediseaseevolution inthegroupofpatientswhounderwentsurgicalprocedures wasasfollows:7(25.9%)wereinastateofdiseaseactivity,16 (59.3%)wereinremission,and2(7.4%)hadevolvedtodeath. Two(7.4%)ofthesepatientshadnodataavailable(Table4).
Table4–Pharmacologicalandinterventionisttherapy carriedoutduringfollow-upofpatientswith
juvenile-onsetTakayasu’sarteritis.
Treatment Total,n(%)
Corticosteroids 64/71(90.1)b
Methotrexate 52/71(73.2)
Cyclophosphamide 36/68(52.9)b
Azathioprine 7/63(11.1)b
Mycophenolate 3/66(4.5)b
Infliximab 4/64(6.3)b
Antiplatelet 36/68(52.9)b
Anticoagulant 7/65(10.8)b
Antihypertensive 58/70(82.9)b
LatentTBtreatmenta 13/67(19.4)b
TBtreatmenta 13/52(25.0)b
Angioplastywithorwithoutstent 21/71(29.6)
Bypass 10/71(14.1)
Nephrectomy 5/71(7.0)
a Onepatientwas treatedforlatent tuberculosis(TB)andfor
tuberculosisindifferenttimesduringthemonitoring. b Mostpercentageswerecalculatedwithdifferentdenominators,
accordingtothequestionnairedataofeachpatient.
Discussion
Thisstudywasconductedinamixed-racecountry,withlarge geographicdimensionsandwithalargenumberofpatients withjuvenile-onsetTA.Thisallowedusabetterknowledge ofthedisease inthisagegroup.Weobservedahigh num-berofpatientsunder10inourseriesandahighfrequencyof constitutionalsymptomsatpresentationofthedisease.
Thepredominanceoffemalesinourstudyisconsistent with studiesindifferent populations, bothinthe pediatric population,wherethisfrequencyvariesbetween58and83%, asintheadultpopulation,thatshowsanevenhigher propor-tionofwomen.4,5,12–16Thehighnumberofchildrenunder10 years inthisstudy,whichincluded patientsupto18 years of age atdiagnosis, draws attention and differs from Park et al. series, where 108 children and adults with TAwere evaluated.14Inthisstudy,childrenupto10yearsat diagno-sisaccountedfor6.5%ofallpatients,andadolescentsaged between10and20yearsaccountedfor19%.Themeanageat diseaseonsetwasalsolowerthanthatfoundinsomestudies, wherethismeanreachedupto14years,buthigherthanthe meanfoundbyHahnetal.in31childrenofSouthAfrica(8.4 years).5,12,13Wecouldnotjustifythevariationinageamong thedifferentpopulations;thus,wehypothesizedthatgenetic andenvironmentalfactorsmayinfluencetheearlieronsetof thediseaseinsomeregions.Themortalityrateof8%found inourcohortwassimilartothatinotherstudiesonpediatric populations(range:7–22%).6,12,13Ourpatientsdiedinashort time,whichreflectstheseverityofthisvasculitis.
Constitutionalsymptomswere presentinalmost80%of
lowerdegreeofinflammationofthediseaseafterits
treat-ment.Otherstudiesalsoshowedthesesymptomsinpeople
withjuvenile-onsetTA,buttheirassessmentwascarriedout separately:fever was present in 4–26%of patients; loss of
weight in 4–47.5%; and fatigue (which was evaluated in a
recentUSstudy),occurredin38%ofpatientsatthe presenta-tionofthedisease.4,5,12,13Thehighfrequencyofconstitutional
symptoms inthe presentation ofTA isa well-known fact,
particularlyinpediatricpopulations;andbecauseoftheir non-specificcharacter,thiscausesadelayindiagnosis,whichin somepatientsmeanta4-yearsetback.
Neurological symptomswere alsovery prevalent in our
series,withimprovementduringfollow-up,similarlyto car-diovascularsigns(lowerperipheralpulsesandbloodpressure), findingsconsistentwiththeliterature.4,6,12,13,17Thedecreases inperipheralpulsesandblood pressure,especiallythefirst ofthesesigns,didnotshowsignificantimprovementduring follow-up,asthesearesecondarymanifestationsofstructural arterialchanges,athinghardlymodifiablewiththerapy.
VHSelevationwasthemostfrequentlaboratoryfindingin allthreeevaluations,reaching80%ofpatientsatthe presen-tationofthedisease,whichisconsistentwiththehighrate ofincreaseininflammatorymarkersfoundinotherstudies inpediatricpatients.5,12,17Anotherfrequentlaboratory find-inginourpatientswasatuberculinskintestpositivity,which wasalsofoundinotherpopulationswithTAwhere tubercu-losis(TB)isendemic,suchasMexicoandSouthAfrica.12,18
ThehighfrequencyofTBfoundinourchildrenwasmuch
higherthanthatreportedinhealthyBrazilianchildrenbythe BrazilianInstitute of Geographyand Statistics, thus show-ing an association between Mycobacterium tuberculosis and TA.19ItisstilluncleartherelationshipbetweenTBandTA, but oneexplanation isthat the heatshock protein65-kDa foundinmycobacteriacross-reactwiththehomologous pro-teinpresent inthe vascular wallofthe host,triggering an
immuneresponse.
Regarding angiographic changes,stenosis was the most
prevalenttypeofinjury,being foundinmostpatients;this finding is consistent with studies on adults and children, where this is the predominant type of injury.4,15 The fre-quencyofaneurysmsfoundinourpatientswashigherthan the related instudies based on adultpopulations, ranging between5and12%.14,15,20,21 Theabdominalaortaandrenal arteries were the most affected arterial segments, a find-inginlinewithotherstudiesconductedinchildren.4,13,17,22 Therecent studybySzugieet al.foundahigherfrequency ofinvolvementoftheabdominalaortaanddescending tho-racicaorta;but therenalarterieswereanalyzedseparately, andpossiblytheirfrequencywouldchangeiftheyhadbeen analyzedtogether.5 With respectto angiographic type,the mostcommonwastypeIV,followedbytypeV,afindinga lit-tledifferentfromthatinIndianchildren,wheretherewasa higherprevalenceoftypeV,followedbytypeIV.Ontheother hand,ourfindingsaresimilartothoseinchildreninSouth Africa,whereinfradiafragmaticcommitment(corresponding totypeIV)was themostpredominantfinding,followed by diffuseinvolvement(correspondingtotypeV).12,13 Angiogra-phictypespresentedbyadolescentswereevaluatedseparately fromthetypespresentedbychildren;thus,weintendedtosee iftherewasmorelikenesswiththedistributioninadults,in
whom typesIandVaccountforvirtuallyall cases.16 How-ever, the difference between our adolescents versus adults remained.
Thevastmajorityofpatientsneededglucocorticoidsand
immunosuppressive drugs during follow-up, as shown in
other studies,and asignificant portionunderwent surgery, highlightingthechronicandrelapsingnatureofthedisease.23 Withthistreatment,morethan60%ofpatientswerein remis-sionattheendofthestudy;andthisnumbercouldpossibly bemoreencouragingwithashortertimetodiagnosis.
Thisstudyenabledustoanalyzeasignificantnumberof patientswithjuvenile-onsetTA,makingthisthelargeststudy in this agegroup so far.Because ofthe detailed question-naire which produced datafrom three differentevaluation periods, we could describe clinical and laboratory charac-teristics regardingpresentationand evolution ofTA inour population.
Themajorlimitationofthisstudystemmedfromits retro-spectivenatureandfromthelargenumberofevaluatorsfor datacollection,aswellastheuseofdifferentradiologistsfor interpretationoftheangiographicimagestaken.Tominimize possiblediscrepanciesinassessmentsfromthevarious cen-tersinvolved,aWord®documentwithexplanationsofhowto properlyfilloutthedataandstandardizetheresponseswas senttothedoctorsresponsibleforeachcenter.
In our series, that included patients up to 18 years of age,weobservedahighnumberofpatientsunder10years
and high frequencyofconstitutional symptoms atTA
pre-sentation. These findings confirm the importance of the
clinical suspicionwithrespecttothisvasculitis inchildren andadolescents,whenthesepopulationspresentlong-term
constitutional symptomsofunknown cause,aswell asthe
importanceofcheckingbloodpressureandperipheralpulses inourroutinephysicalexaminations.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.ClementeG,HilarioMO,LedermanH,SilvaCA,SallumAM, CamposLM,etal.TakayasuarteritisinaBrazilianmulticenter study:childrenwithalongerdiagnosisdelaythan
adolescents.ClinExpRheumatol.2014;32Suppl82:S128–33.
2.KerrGS,HallahanCW,GiordanoJ,LeavittRY,FauciAS,Rottem M,etal.Takayasuarteritis.AnnInternMed.1994;120:919–29.
3.StanleyP,RoebuckD,BarbozaA.Takayasu’sarteritisin children.TechVascIntervRadiol.2003;6:158–68.
4.CakarN,YalcinkayaF,DuzovaA,CaliskanS,SirinA,OnerA, etal.Takayasuarteritisinchildren.JRheumatol.2008;35: 913–9.
5.SzugyeHS,ZeftAS,SpaldingSJ.Takayasuarteritisinthe pediatricpopulation:acontemporaryUnitedStates-based singlecentercohort.PediatrRheumatolOnlineJ.2014;12:21.
6.OzenS,BakkalogluA,DusunselR,SoylemezogluO,OzaltinF, PoyrazogluH,etal.ChildhoodvasculitidesinTurkey.A nationwidesurvey.ClinRheumatol.2007;26:196–200.
revisãodeliteraturaapropósitode6casos.JBrasNefrol. 1998;20:263–75.
8. UltachalkF,TerreriMT,LenCA,HattaFS,LedermanH,Hilário MO.Takayasu’sarteritisinchildhood:clinicaland
angiographicstudyoffivecases.RevBrasReumatol. 2000;40:189–95.
9. CastellanosAZ,CamposLA,LiphausBL,MarinoJC,KissMHB, SilvaCA.ArteritedeTakayasu.AnPediatr.2003;58:211–6.
10.OzenS,PistorioA,IusanSM,BakkalogluA,HerlinT,BrikR, etal.EULAR/PRINTO/PREScriteriaforHenoch-Schoenlein purpura,childhoodpolyarteritisnodosa,childhoodWegener granulomatosisandchildhoodTakayasu’sarteritis:Ankara 2008.PartII:Finalclassificationcriteria.AnnRheumDis. 2010;69:798–806.
11.HataA,NodaM,MoriwakiR,NumanoF.Angiographic findingsofTakayasuarteritis:newclassification.IntJCardiol. 1996;54suppl:S155–63.
12.HahnD,ThomsonPD,KalaU,BealePG,LevinSE.Areviewof TakayasuarteritisinchildreninGauteng,SouthAfrica. PediatrNephrol.1998;12:668–75.
13.JainS,SharmaN,SinghS,BaliHK,KumarL,SharmaBK. TakayasuarteritisinchildrenandyoungIndians.IntJCardiol. 2000;75:53–7.
14.ParkMC,LeeSW,ParkYB,ChungNS,LeeSK.Clinical characteristicsandoutcomesofTakayasu’sarteritis:analysis of108patientsusingstandardizedcriteriafordiagnosis, activityassessmentandangiographicclassification. ScandJRheumatol.2005;34:284–92.
15.Maksimowicz-McKinnonK,ClarkTM,HoffmanGS. Limitationsoftherapyandaguardedprognosisinan
AmericancohortofTakayasuarteritispatients.Arthritis Rheum.2007;56:1000–9.
16.FreitasDS,CamargoCZ,MarizHA,ArraesAED,SouzaAWS. Takayasuarteritis:assessmentofresponsetomedical therapybasedonclinicalactivitycriteriaandimaging techniques.RheumatolInt.2012;32:703–9.
17.HongCY,YongYS,ChoiJY,SulJH,LeeKS,ChaSH,etal. TakayasuarteritisinKoreanchildren:clinicalreportof seventycases.HeartVessels.1992;7:91–6.
18.Lupi-HerreraE,Sanchez-TorresG,MarcushamerJ,MispiretaJ, HorwitzS,VelaJE.Takayasu’sarteritis:clinicalstudyof107 cases.AmHeartJ.1977;93:94–103.
19.InstitutoBrasileirodeGeografiaeEstatística–2010. 20.VanoliM,DaianaE,SalvaraniC,SabbadiniMG,RossiC,
BacchianiG,etal.Takayasu’sarteritis:astudyof104Italian patients.ArthritisRheum.2005;53:100–7.
21.ArnaudL,HarocheJ,LimalN,ToledanoD,GambottiL, CostedoatChalumeau,etal.TakayasuarteritisinFrance:a single-centerretrospectivestudyof82casescomparing White,NorthAfricanandBlackpatients.Medicine (Baltimore).2010;89:1–17.
22.D’SouzaSJ,TsaiWS,SilverMM,ChaitP,BensonLN,Silverman E,etal.Diagnosisandmanagementofstenotic
aorto-arteriopathyinchildhood.JPediatr.1998;132: 1016–22.