SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
article
Acute
distal
biceps
ruptures:
single
incision
repair
by
use
of
suture
anchors
夽
Rafael
Almeida
Maciel
∗,
Priscilla
Silva
Costa,
Eduardo
Antônio
Figueiredo,
Paulo
Santoro
Belangero,
Alberto
de
Castro
Pochini,
Benno
Ejnisman
UniversidadeFederaldeSãoPaulo,DepartamentodeOrtopediaeTraumatologia,CentrodeTraumatologiadoEsporte,SãoPaulo,SP, Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received27January2016 Accepted31May2016 Availableonline9March2017
Keywords: Elbow/surgery Elbow/injuries Treatmentoutcome
a
b
s
t
r
a
c
t
Objective:Clinicalandfunctionalassessmentofthesurgicaltreatmentforacuteinjuryof thedistalinsertionofthebicepsbrachialperformedwithasurgicaltechniqueusingasingle incisioninproximalforearmandfixationwithsutureanchorsintheradialtuberosity. Methods:This study reviewed the medical recordsofpatients who underwent surgical treatmentofdistalbicepsinjuryduringtheperiodbetweenJanuary2008andJuly2014. Ina mean follow-up of12 months,22 patients with completeand acute injury, diag-nosedthroughphysicalexaminationandimagingstudies,werefunctionallyassessedin thepostoperativeperiodregardingtherangeofmotion(degreesofflexion-extensionand pronation–supination),thepresenceofpain(VAS),theAndrewsCarson-score,andtheMayo ElbowPerformanceScore(MEPS).
Results:Duringthepostoperativefollow-upassessment,nopatientreportedpainbyVAS scale;allweresatisfiedwiththeestheticappearanceofthesurgery.Therangeofarticular movementremainedunchangedat95.4%ofpatients,withthelossof8◦ofsupinationin onepatient.Nochangesinmusclestrengthwereobserved.Theresultsofthe Andrews-Carsonscoreweregoodin4.6%andexcellentin95.4%ofcases;theMEPSpresented100% ofexcellentresults.Therateofcomplicationswas27.2%,similartotheliterature. Conclusion:Surgicalrepairofacuteinjuryofthedistalbicepstroughasingleincisioninthe proximalforearmandfixationwithtwosutureanchorsintheradialtuberosityisaneffective andsafetherapeuticoption,allowingearlymotionandgoodfunctionalresults.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedattheUniversidadeFederaldeSãoPaulo,DepartamentodeOrtopediaeTraumatologia,CentrodeTraumatologiado Esporte,GrupodeOmbroeCotovelo,SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mail:rafaelalmeidamaciel@gmail.com(R.A.Maciel). http://dx.doi.org/10.1016/j.rboe.2017.03.004
Lesão
do
bíceps
distal
aguda:
reparo
por
via
única
e
fixac¸ão
por
âncora
de
sutura
Palavras-chave: Cotovelo/cirurgia Cotovelo/lesões Resultadodetratamento
r
e
s
u
m
o
Objetivo: Avaliac¸ãoclínicaefuncionaldotratamentocirúrgicodalesãoagudadainserc¸ão distaldobícepsbraquialpelatécnicacirúrgicaporviadeacessoúnicanoantebrac¸oproximal efixac¸ãocomâncorasdesuturanatuberosidaderadial.
Método: Estudofeitopormeiodarevisãodosprontuáriosdepacientessubmetidosa trata-mentocirúrgicodelesãodainserc¸ãodistaldobícepsbraquialentrejaneirode2008ejulho de2014.Emumseguimentomédiode12meses,22pacientescomlesãocompletaeaguda, diagnosticadosporexamefísicoeexamesdeimagem,foramavaliadosfuncionalmenteno pós-operatóriopormeiodamensurac¸ãodaamplitudedemovimentos(grausde flexoex-tensãoepronossupinac¸ão),pelapresenc¸adedor(EVA)epelasescoresdeAndrews-Carson eMayoElbowPerformanceScore(MEPS).
Resultados: Durantea avaliac¸ão dos pacientesnoseguimento pós-operatório,nenhum pacientereferiadorpelaescalaEVAetodosestavamsatisfeitoscomaaparênciaestética dacirurgia.Aamplitudedemovimentoarticularencontrava-seinalteradaem95,4%dos pacientes,coma perda de 8◦ de supinac¸ãoem um paciente.Os resultados segundoo escoredeAndrews-Carsonforambonsem4,6%eexcelentesem95,4%doscasos;noMEPS, observaram-se100%deresultadosexcelentes.Ataxadecomplicac¸õesfoide27,2%,valor semelhanteaosdadosdaliteratura.
Conclusão: Otratamentocirúrgicodaslesõesagudasdobícepsdistalporviaúnicacom fixac¸ãocomousodeduasâncorasdesuturamostrou-seumaopc¸ãoterapêuticasegurae eficaz,permitiumovimentac¸ãoprecoceebonsresultadosclínicosefuncionais.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Injuriesofthedistalinsertionofthebicepsbrachiiare uncom-mon,withanincidenceof1.2per100,000patientsperyear.1
Themostcommonmechanismofinjuryischaracterizedby aneccentricmusclecontraction,withtheelbowflexedat90◦ andtheforearminsupination,occurringpredominantlyinthe dominantupperlimbofmalesaround40–50years.2
Surgical treatmentis superior toconservative approach regardingclinicalandfunctionalresults.Conservative treat-mentsusuallyleadtomuscleweakness,mobilitydisorders, andestheticdeformities.3,4
Numeroussurgicaltechniquesarereportedforthe reinser-tionofdistalbiceps, throughdoubleor singleaccessroute, withdifferentfixationmethods,amongwhichthemost com-monlyusedarebonetunnel,interferencescrew,endobutton, andsutureanchor.5Clinicalstudieshavedemonstratedthe
advantagesofsingleaccess route,withexcellent resultsin repairsusingsutureanchors.6,7
Thisstudyaimedtodescribeaminimallyinvasivesurgical techniqueforrepairofthedistalbicepstendonthroughtwo double-loadedsutureanchors,aswellastodescribeitsclinical andfunctionalresults.
Material
and
methods
This study reviewed the medical records of patients who underwent surgical treatment ofdistal biceps brachii
insertioninjuryduringtheperiodbetweenJanuary2008and July2014.
Atfirst,39casesofdistalbicepsinjurywereretrieved. Inclu-sioncriteriaweredistal,isolatedandclosedbicepslesion;less than sixweeksbetweeninjuryand surgicaltreatment; use ofthesamesurgicaltechnique;andaminimum postopera-tivefollow-upofsixmonths.Exclusioncriteriawerepartial andchronicinjuriesofthedistalbicepstendon;surgical tech-niquewithdoubleaccessroute;fixationmaterialotherthan sutureanchors;useofgraftfortendonfixation;and postoper-ativefollow-upoflessthansixmonths.Thus,afterreviewing charts,22patientswereincludedinthepresentstudy(Table1). Lesions were diagnosed by physical examination (hook test)andimaging(magneticresonanceimaging[MRI]or ultra-sound)confirmingacompleteruptureofthedistalinsertion ofthebiceps.
Patientswereassessedregardingrangeofmotionwitha goniometer,whichmeasuredthedegreesofflexion-extension andpronosupination,andpresenceofpain,assessedbythe visualanalogscale(VAS);theAndrews-Carson8andtheMayo
ElbowPerformanceScore(MEPS)scoreswereapplied.9
Allpatientssignedaninformedconsentformpriortotheir participationinthisstudy,whichwassubmittedtothe eval-uationandapprovaloftheEthicsCommitteeforResearchin HumanBeings.
Surgicaltechnique
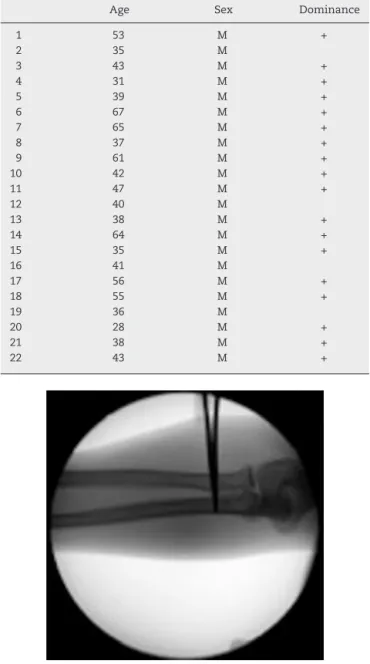
Table1–Epidemiologicaldataofpatientswithacute injuryofthedistalbicepsbrachiiinsertion.
Age Sex Dominance
1 53 M +
2 35 M
3 43 M +
4 31 M +
5 39 M +
6 67 M +
7 65 M +
8 37 M +
9 61 M +
10 42 M +
11 47 M +
12 40 M
13 38 M +
14 64 M +
15 35 M +
16 41 M
17 56 M +
18 55 M +
19 36 M
20 28 M +
21 38 M +
22 43 M +
Fig.1–Intraoperativelocationoftheradialtuberosity, usingradioscopy.
tourniquet,astheauthors believethattheuse ofa tourni-quetincreasesthedifficultyoftheprocedurebylimitingthe mobilizationofthedistalbicepstendon.
Asingle accessroute was created approximately 2.5cm fromthecubitalflexioncrease,guidedbyfluoroscopyfor ini-tiallocationoftheradialtuberosityonitsulnaredge(Fig.1).A 5-cmsurgicalincisionintheanteriorregionoftheproximal
thirdofthe forearm, atthe radial tuberosity,inthe trans-verseplane,withcarefuldissectionofsoft tissues,allowed thesearchinthesuperficialplaneforthedistalbiceps ten-donstump,proximallyretracted(Fig.2).Tractionsutureswere passedthroughthebicepstendoninitstendinousportionto enableitsmobilizationandre-approximationatits anatomi-calinsertion,attheulnaredgeoftheradius,withtheforearm incompletesupinationandat10◦ofelbowflexion(Fig.3).The
Fig.2–Singleaccessroute.
Fig.3–Tractionsutureintheruptureddistalbicepstendon.
soft tissueand thelacertusfibrosus werereleased toallow increasedmobilitywhennecessary.Theradialtuberositywas exposed bydelicatelydisplacingsoft tissues,thus avoiding neurologicalandvascularinjury.Then,theradialtuberosity wasdebridedforremovalofresidualtendontissueand scar-ring,inordertoallowbleeding,aimingtopotentiateadhesion ofthereinsertion.
Two3-mmsutureanchors,loadedwithhigh-resistance fil-aments,werepositionedintheradialtuberosity,aligned(one proximalandonedistal),withapproximately1cmdistance betweenthem.Twoindependentsutureswerepassedthrough the regularized distal stump, with self-locking stitches, to allowthetendontobere-attachedtothebone(Fig.4).The distalanchorrepairwasfixatedfirsttoestablishthelength of the tendon;then, proximalanchor repairswere fixated, whichallowedthetendonfootprinttoberecreated maximiz-ingtendon-bonecontactarea.
Stabilityoftherepairwasconfirmedunderdirect visual-ization,withevaluationofthebicepsbrachiitendontension. Woundwasthenstitched,withapproximationofthe subcu-taneoustissueandsteriledressing.
Results
Fig.4–Self-lockingstitchtoallowthetendontobe re-approximatedtothebone.
All patients presented elbow flexion against resistance withtheforearminsupinationasthemechanismoftrauma; onlytwooccurredduringsportstraining.Allpatients under-wentphysicalexaminationwithhooktest,whichwasfound tobepositivein19patients(86.3%).Thefollowing comple-mentaryexamswererequested:elbowradiographs(frontand profile)inallcases;14 elbowMRIs(63.6%);and eight ultra-sounds(36.3%)forconfirmationandassessmentoftheelbow lesion.
Mean time between injury and surgery was eightdays (1–35).
Meanfollow-upwas12months(6–18).During postopera-tivefollow-upassessment,nopatientreportedpainbyVAS scale;allwere satisfiedwiththeestheticappearanceofthe surgery.Range ofmotionremained unchanged at95.4% of patients,withlossof8◦ofsupinationinonepatient.Results oftheAndrews-Carsonscoreweregoodin4.6%andexcellent in95.4%ofcases;MEPSpresentedexcellentresultsin100%.
Inthepresentsample,acomplicationrateof27.2%was observed. Sixcases were reported: four patients presented neuropraxia ofthelateral cutaneous nerveofthe forearm; one, radialneuropraxia; and one, partialloss of ROM, but withoutclinicalrepercussionsduringdailyactivitiesandwith improvementinclinicalfollow-up.
Returntoactivityand thepracticeofsportsoccurred in threemonths,atthesamelevelasbeforeinjury.
Discussion
Distal biceps tendon ruptures represent 3% of biceps ruptures.10 However,arecentstudybySafranandGraham1
showedanapproximateincidenceof10%.Itoccurs preferen-tiallyinmalesinthefifthandsixth decadesoflife,mostly inthedominantlimb,andtraumamechanismismainlyan eccentricbicepscontractiononaflexedelbow.Inthepresent study,onlymalepatientswereincluded,withameanageof45 years,involvementofthedominantsidein86%ofthelesions, analogoustotheliteraturedata.3
Diagnosticevaluationofacutedistalbicepsinjuryis ini-tiated by medical history and physical examination, with
specifictestssuchasthehooktest.Basedonclinicalhistory, withreportsofthemaintraumamechanismbyeccentric con-traction,followedbyclinicaldevelopmentofpain,edema,and ecchymosesinthecubital fossa,aswell asapositivehook test,wecanestablishdistalbicepsinjuryasthemain diag-nostichypothesis.Intheliterature,thehooktestpresentsa sensitivityandspecificity of100%.11 Nonetheless,complete
rupture,degreeofretractionofthetendonstump,and pres-enceofassociatedlesionswereconfirmedthroughadditional tests.Ultrasonographyallowsidentificationoflesionas par-tialorcomplete,withstudiesshowing95%sensitivityand71% specificity.Itisalsopossibletodeterminedegreeofretraction ofthetendonstump.12Thisexamisinexpensiveandeasyto
performinBrazil;therefore,itwasusedin40%ofthe sam-ple.MRIisconsideredthegoldstandardexamfordefinitive diagnosis;italsoaidssurgicalplanninganddiscards associ-atedlesions.13Thus,thismethodwaspreferredandapplied
in60%ofthepresentcases(Fig.5).
The best treatment for distal biceps injuries, whether conservative or surgical, is no longer questioned in the literature.14Conservativetreatmentresultsinmuscle
weak-ness,withlossofsupinationforceofapproximately40%and flexionforceofapproximately30%,aswellasrestrictionsin activities ofdailyliving.4 Thus,the authorsagreewith the
literature,reservingconservativemodality forpatientswho cannotbesubmittedtosurgeryandelderlypatientswithlow functionaldemands.4,14
Surgicaltreatmentisthechosenapproachandshouldbe performedasearlyaspossible;aperiodofuptosixweeks hasbeenestablished,asitallowsrecoveryandmobilizationof theretracteddistalbicepstendonand,thus,allows anatom-icalfixationofthetendonintheradialtuberosity.Another importantfactoristoavoidclosureofthespacepreviously occupiedbythetendontotheplaceofitsinsertion,byfibrous tissueand/orpseudotendon.Thisclosureleadstochangesin localanatomy, causedbyadhesionsandlocalfibrosis, hin-dering safeexposure and the identification and protection ofnoblestructures,especiallythelateralcutaneousnerveof theforearm.Thelateralcutaneousnerveislocatedlaterally tothedistalbicepstendon,closetotheradialtuberosity;it maybeaffectedinbothruptureandsurgicalreinsertion,being responsibleforthemostfrequentcomplicationinthistypeof procedure.3,15,16Therefore,thepresentapproachallowsfora
safedissectionofsofttissues;thetunnelofthedistalbiceps tendoncanbevisualized,withtendonexcursiontoits reinser-tionpoint.Thisreducestheriskofneurologicalinjuries,which reducestheratesofcomplicationsrelatedtothetimeperiod betweeninjuryandsurgicalrepair.Thisapproachalsoallows restorationofforearmsupinationforceandelbowflexionto nearpre-injurylevel.6
There is no consensus in the literature regarding best approachandbestmethodoffixationfordistalbiceps rup-tures,andtherearemanypossibilities.Grewaletal.,17intheir
randomized clinical trial, observedno difference inresults whencomparingsingleanddoubleaccessroutes.In2014,a systematicreviewbyWatsonetal.18foundsmalldifferences,
Fig.5–T2-weightedmagneticresonanceimagingoftheforearmafterinjury,withfatsuppression,showingcomplete ruptureofthedistalbiceps(arrows).A,coronalcut;B,axialcut;C,sagittalcut.
withtransverseorientation,asthisapproachprovides excel-lentvisualizationoftheradialtuberosity,allowsresectionof thestumpofthedistally-retractedrupturedtendonand lim-iteddissectionofsoftparts,reducestherisksofcomplications, andhasabetterestheticresult(Fig.6).Thechoiceofasingle accessrouteontheradialtuberosity,inwhichthecorrect fore-armpositioningformaximumsupinationandsemi-flexionfor thereinsertionofthedistaltendonofthebicepsare impor-tant, is based on the anatomical knowledge described by Mazzoccaetal.,19supplementedbyotheranatomicalstudies
thatdescribethefootprintofthedistalbicepstendonregion locatedinpostero-ulnarradialtuberosity,measuring21mm inlengthand7mminwidth.20,21
Duetotheavailabilityofdifferentfixationmethodsforthe reinsertionofthedistalbiceps,eachwithitsown character-istics,advantages,anddisadvantages,severalbiomechanical studies comparing these methods have been conducted, showing divergent results, powering the doubt of which methodispreferential.Mazzocaetal.5assessedthefourmost
common methods of treatment (bonetunnel, endobutton, interferencescrew,andsutureanchors)incadavericelbows subjectedtocyclicloadsof50Nforcefrom0◦to90◦flexionand concludedthat the endobutton technique presents greater resistancetofailure.However,mostclinicalstudiesusesuture anchorsasamethodofcomparisonbetweentheavailable fix-ation techniques,observing optimalclinicaland functional
Fig.6–Clinicalevaluationatfourweekspostoperative, withevaluationofsurgicalscarintheproximalforearm (arrow).
results.3,22Fewclinicalstudieswiththeuseofendobuttonare
available;therefore,newstudiesare neededtoallowa bet-tercomparisonofthelattertwotechniques.23Inthepresent
study,reinsertionwasmadewithtwosutureanchors,which reestablishedlengthandrecreatedthefootprintofthetendon. Inthepresentpractice,thismaterialisavailable,andgood sur-gicalresultsinshort-andlong-termfollow-upwereachieved withthistechnique,withoutlossoffixation.
Inthepresentsample,complicationratewas27.2%,similar tothat reportedinthe literature,which is26.4%.18
Associ-atedwiththisfactor,duringfollow-up4.6%goodand95.4% excellentresultswereobservedintheAndrews-Carsonscore, as well as100%excellent resultsin theMEPS scale.These findingsconfirmthesatisfactoryresultsofthissurgical tech-nique. Mostcommon complicationwas neuropraxia ofthe lateral cutaneousnerveoftheforearm;this wasalso men-tionedinmoststudiesasthemaincomplication.18Recovery
fromneurologicalsymptomsoccurredinthefirstmonthsof postoperativefollow-up.Neuropraxiaoftheradialnervewas observedinthepatientwiththelongesttimeperiodbetween injuryandsurgicalprocedure(35days).
Allpatientsfollowedthespecificrehabilitationprotocolset forth bythisgroup.Therepairallowedearlypassive move-mentwithinoneweekpostoperatively;aslingwasusedfor two weeks, and active movements were initiated at four weeks,whichevidencedtheeffectivenessofthismethodof fixation.Meantimetoreturntoactivitieswithalevel simi-lartothatpresentedbeforeinjurywasthreemonths,withno complaintsandwithahighsatisfactionindex.
Conclusion
Earlysurgicalrepairofacuteinjuryofthedistalbicepsthrough asingleincisionattheproximalforearmandfixationwithtwo sutureanchorsintheradialtuberosityisaneffectiveandsafe therapeuticoption,allowingearlymotionandgoodfunctional results.
Conflicts
of
interest
r
e
f
e
r
e
n
c
e
s
1. SafranMR,GrahamSM.Distalbicepstendonruptures: incidence,demographics,andtheeffectofsmoking.Clin OrthopRelatRes.2002;(404):275–83.
2. MorreyBF.Bicepstendoninjury.AAOSInstrCourseLect. 1999;48:405–10.
3. SuttonKM,DoddsSD,AhmadCS,SethiPM.Surgical treatmentofdistalbicepsrupture.JAmAcadOrthopSurg. 2010;18(3):139–48.
4. BakerBE,BierwagenD.Ruptureofthedistaltendonofthe bicepsbrachii.Operativeversusnon-operativetreatment.J BoneJointSurgAm.1985;67(3):414–7.
5. MazzoccaAD,BurtonKJ,RomeoAA,SantangeloS,AdamsDA, ArcieroRA.Biomechanicalevaluationof4techniquesof distalbicepsbrachiitendonrepair.AmJSportsMed. 2007;35(2):252–8.
6. LemosSE,EbramzedehE,KvitneRS.Anewtechnique:invitro sutureanchorfixationhassuperioryieldstrengthtobone tunnelfixationfordistalbicepstendonrepair.AmJSports Med.2004;32(2):406–10.
7. JohnCK,FieldLD,WeissKS,SavoieFH3rd.Single-incision repairofacutedistalbicepsrupturesbyuseofsuture anchors.JShoulderElbowSurg.2007;16(1):78–83. 8. AndrewsJR,CarsonWG.Arthroscopyoftheelbow.
Arthroscopy.1985;1(2):97–107.
9. BrigatoRM,MourariaGG,KikutaFK,CoelhoSP,CruzMA, ZoppiFilhoA.Functionalevaluationofpatientswith surgicallytreatedterribletriadoftheelbow.ActaOrtopBras. 2015;23(3):138–41.
10.MorreyBF,AskewLJ,AnKN,DobynsJH.Ruptureofthedistal tendonofthebicepsbrachii:abiomechanicalstudy.JBone JointSurgAm.1985;67(3):418–21.
11.O’DriscollSW,GoncalvesLB,DietzP.Thehooktestfordistal bicepstendonavulsion.AmJSportsMed.2007;35(11):1865–9. 12.LoboLG,FessellDP,MillerBS,KellyA,LeeJY,BrandonC,etal.
Theroleofsonographyindifferentiatingfullversuspartial distalbicepstendontears:correlationwithsurgicalfindings. AmJRoentgenol.2013;200(1):158–62.
13.FitzgeraldSW,CurryDR,EricksonSJ,QuinnSF,FriedmanHF. Distalbicepstendoninjury:MRimagingdiagnosis.Radiology. 1994;191(1):203–6.
14.ChillemiC,MarinelliM,DeCupisV.Ruptureofthedistal bicepsbrachiitendon:conservativetreatmentversus anatomicreinsertion–clinicalandradiologicalevaluation after2years.ArchOrthopTraumaSurg.2007;127(8):705–8. 15.ChiavarasMM,JacobsonJA,BilloneL,LawtonJM,LawtonJ.
Sonographyofthelateralantebrachialcutaneousnervewith magneticresonanceimagingandanatomiccorrelation.J UltrasoundMed.2014;33(8):1475–83.
16.KellyEW,MorreyBF,O’DriscollSW.Complicationsofrepairof thedistalbicepstendonwiththemodifiedtwo-incision technique.JBoneJointSurgAm.2000;82(11):1575–81. 17.GrewalR,AthwalGS,MacDermidJC,FaberKJ,Drosdowech
DS,El-HawaryR,etal.Singleversusdouble-incision techniquefortherepairofacutedistalbicepstendon ruptures.Arandomizedclinicaltrial.JBoneJointSurgAm. 2012;94(13):1166–74.
18.WatsonJN,MorettiVM,SchwindelL,HutchinsonMR.Repair techniquesforacutedistalbicepstendonruptures:a systematicreview.JBoneJointSurgAm.2014;96(24):2086–90. 19.MazzoccaAD,CohenM,BerksonE,NicholsonG,CarofinoBC,
ArcieroR,etal.Theanatomyofthebicipitaltuberosityand distalbicepstendon.JShoulderElbowSurg.2007;16(1):122–7. 20.AthwalGS,SteinmannSP,RispoliDM.Thedistalbiceps
tendon:footprintandrelevantclinicalanatomy.JHandSurg Am.2007;32(8):1225–9.
21.HutchinsonHL,GloysteinD,GillespieM.Distalbicepstendon insertion:ananatomicstudy.JShoulderElbowSurg. 2008;17(2):342–6.
22.SardaP,QaddoriA,NauschutzF,BoultonL,NandaR,Bayliss N.Distalbicepstendonrupture:currentconcepts.Injury. 2013;44(4):417–20.