r e v b r a s o r t o p . 2016;51(1):109–112
w w w . r b o . o r g . b r
Case
Report
Congenital
dislocation
of
the
patella
–
clinical
case
夽
Pedro
Miguel
Sá
a,∗,
Filipa
Raposo
a,
Manuel
Santos
Carvalho
b,
Nuno
Alegrete
b,
Jorge
Coutinho
b,
Gilberto
Costa
baUnidadeLocaldeSaúdeAltoMinho,VianadoCastelo,Portugal
bCentroHospitalarSãoJoão,Porto,Portugal
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received11February2015 Accepted13February2015 Availableonline30December2015
Keywords:
Patellardislocation/surgery Patellardislocation/congenital Kneejoint/surgery
Rangeofjointmotion
Orthopedicprocedures/methods
a
b
s
t
r
a
c
t
Congenitalpatellardislocationisarareconditioninwhichthepatellaispermanently dislo-catedandcannotbereducedmanually.Thepatelladevelopsnormallyasasesamoidbone ofthefemur.Thiscongenitaldislocationresultsfromfailureoftheinternalrotationofthe myotomethatformsthefemur,quadricepsmuscleandextensorapparatus.Itusually man-ifestsimmediatelyafterbirth,althoughinsomerarecases,thediagnosismaybedelayed untiladolescenceoradulthood.Earlydiagnosisisimportant,therebyallowingsurgical cor-rectionandavoidinglatesequelae,includingearlydegenerativechangesintheknee.Acase ofpermanentdislocationofthepatellaispresentedhere,inafemalechildagedsevenyears. ©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
Luxac¸ão
congênita
da
patela
–
caso
clínico
Palavraschave:
Luxac¸ãopatelar/cirurgia Luxac¸ãopatelar/congênito Articulac¸ãodojoelho/cirurgia Amplitudedemovimentoarticular Procedimentos
ortopédicos/métodos
r
e
s
u
m
o
A luxac¸ãocongênitada patelaéumapatologiarara,em quea patelaseencontra per-manentementeluxadaemanualmenteirredutível.Apateladesenvolve-senormalmente comoumossosesamoidedofêmur.Aluxac¸ãocongênitadapatelaresultadafalênciada rotac¸ãointernadomiótomoqueformaofêmur,músculoquadricípiteeoaparelho exten-sor.Usualmentemanifesta-seimediatamenteapósonascimento,emboraemalgunscasos rarosodiagnósticopossaseradiadoatéaadolescência/idadeadulta.Odiagnósticoprecoceé importante,permiteacorrec¸ãocirúrgica,evitaassequelastardias,notadamentealterac¸ões degenerativasprecocesdojoelho.Éapresentadoumcasodeluxac¸ãopermanentedapatela, numacrianc¸adesexofeminino,comseteanos.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevierEditora Ltda.Todososdireitosreservados.
夽
WorkperformedintheCentroHospitalarSãoJoão,Porto,Portugal. ∗ Correspondingauthor.
E-mail:pmgs4@iol.pt(P.MiguelSá). http://dx.doi.org/10.1016/j.rboe.2015.12.010
110
rev bras ortop.2016;51(1):109–112Introduction
Congenitaldislocationofthepatellacomprisesa pathologi-calconditionofpermanentlateral dislocationofthis bone. It is impossible to reduce it through manual maneuvers. It may arise in isolation, associated with lower-limb mal-formations, or within the context of a polymalformative syndrome.1
Itisgenerally diagnosedatbirth.These infantspresent genuvalgumandcontractureoftheflexedknee,inassociation withexternalrotationofthetibia.Whenthesedeformitiesare notpresent,thispathologicalconditionmaynotbediagnosed untiladulthoodisreached.2
Radiological examinations, especially X-rays (XR), com-putedtomography(CT)andmagneticresonanceimaging(MRI) areessentialforidentifyingandcharacterizinglesions associ-atedwithpermanentpatellardislocation(trochleardysplasia orchondrallesions).However,thediagnosisforthis patholog-icalconditionisessentiallyclinical.3
Thisconditioncanonlybecorrectedthroughasurgical pro-cedure.Severaloptionsexist.Earlycorrectionisimportantfor avoidingsequelae.4
Case
report
Thepatientwasaseven-year-oldwhitegirlwithoutany rele-vantantecedentswhowasexaminedinanexternalpediatric orthopedicsconsultationduetodeformityoftheleft knee. Shedidnothaveanyprevioushistoryoftrauma.Herparents saidthattherehad notbeenany initialepisode ofpatellar dislocation.
Uponobjectiveexamination,shepresentedirreducible lat-eraldislocationoftheleftpatella.Itwasobservedthat,during activeandpassivemovements,herextensionandflexiondid notpresentanyamplitudedeficitsandwerenotpainful.She presentedgradeIVstrengthdeficitduringextensionoftheleft lowerlimb.
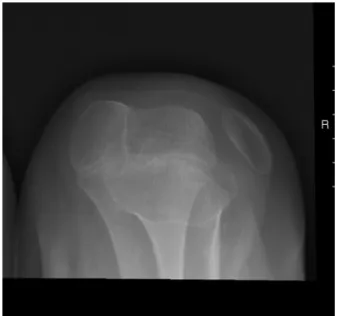
Knee XR was performed under conditions of weight-bearing (Fig. 1) and found lateral patellar dislocation. The lateralXRontheleftkneedidnotshowdislocation(Fig.2). Theaxial XRontheleft patellaagainshowedlateral dislo-cationofthepatella,inassociationwithtrochleardysplasia (Fig. 3). MRI on the left knee (Fig. 4) confirmed that in addition tothe lateral dislocation ofthe left patella, there was dysplasia of the trochlea, but without other asso-ciated lesions. The patient was referred for a pediatric consultation in order to rule out polymalformative syn-drome.
Surgicalcorrectionofthedislocationwasperformed,using thetechniquedescribedbyStanisavljevic,anditfollowedan uneventfulcourse.Plaster-castimmobilizationfromthelower legtothefootwasusedforsixweeks.
Currently,thepatientisbeingfollowedupthrough exter-nal pediatric orthopedic consultations. The patella is now centered, without any episodes of dislocation so far, and thestrength ofthe leftlower limbhasrecovered(grade V). The leg presents flexion of 140◦ and an extension deficit
of5◦.
Fig.1–X-raywithweight-bearingonbothknees.
Discussion
The congenital abnormalities of the patella include its absence,hypoplasiaandpermanentdislocation.
Permanent congenital dislocation isa pathological con-dition in which the patella remains constantly dislocated, evenwhenthe legisextended.Thepatellaremainedfixed onthelateralfaceofthefemoralcondyle.Thedislocationis irreducible, unlesssurgicaltechniquesareused.Itisarare pathologicalconditionofunknownincidence,5whichis
gen-erallydetectedinthefirstdecadeoflife.Itusuallyaffectsboth legsandinmostcasesisassociatedwithpolymalformative
rev bras ortop.2016;51(1):109–112
111
Fig.3–AxialX-rayoftheleftpatella.
syndromes,suchasnail-patellasyndrome,Rubinstein–Taybi syndromeandWilliam–Beurensyndrome.6
Betweentheeighthandtenthweeksofembryo develop-ment,internalrotationofthemyotomeresponsibleforthe formationandorientationoftheextensor apparatusofthe lowerlimbtakesplace.Non-rotationispresumedtobethe causeofcongenitaldislocationofthepatella.7
Thispathologicalentitymaybemanifestedwithavarying spectrumofclinicalpresentations.Whenitisnotdiagnosed atbirth,objectiveexaminationshowsthepresenceof contrac-turewhenthelegisflexed,valgusthatismoreaccentuatedin theaffectedlowerlimbandanassociateddeficitofextension. Itisalsoobservedthattheintercondylarchamferingisempty, withapalpablepatellaonthelateralfaceoftheknee.5
Appar-entgaitimbalancemayalsobeseen,causedbyincompetence oftheextensorapparatus.8
Fig.4–Magneticresonanceimagingoftheleftknee.
Thediagnosis ofcongenital dislocationofthe patellais made through XR,7 if the child ismore than 3–5 years of
age, giventhat ossificationofthe patellastarts atthis age range.9Theanteroposteriorviewoftheknee makesit
pos-sible to view the size and position of the patella, along withotheralterationsassociatedwiththispathological con-dition, such as hypoplasia of the lateral femoral condyle, diminution ofthe jointinterline (latercases) andthe posi-tion of the tibia in relation to the femur. The axial view ofthepatellaalsomakesit possibletoassessthe position, size and shape of the patella, and also the intercondylar groove.7
Echographyisimportant,especiallyforyoungerchildren whosepatellarossificationhasnotyetoccurred.Thismakes itpossibletoviewthecartilaginouspartofthepatella,along withthecartilageofthefemurandtibiaandtheir relation-ships.Italsoenablesviewingofthekneeligamentinsertions andcanbeusedasadynamicexamination,makingit pos-sible todemonstrate theposition ofthepatella inrelation tothefemuratdifferentdegreesofflexion.10–12CTsupplies
detailed informationonthe bonecomponentsoftheknee, butbecauseofitsuseofionizingradiation,itsusefor eval-uatingchildren’sknees isnotrecommended.13MRIhasthe
capacitytoeffectivelydistinguishbetweenthecartilagesof adjacentjointstructures,14whichmakesitessentialfor
pre-operativeassessments.Theappropriatetechniqueincludes producing thin slices in order to avoid a false diagnosis of patellar agenesis and to identify the size and position of the quadriceps muscle and the bone insertions of the quadricepsand patellartendons, therebyaidinginsurgical planning.15
The naturalhistory of undiagnosedand untreated con-genitaldislocationofthepatellafollowsacoursewithmany alterations to the knee, including flattening of the lateral femoralcondyle,withworseningofthevalgusdeformityand externalrotationofthetibia.Thedislocatedpatellaremains hypoplastic and, because ofthe unequal load distribution, anearlydecreaseinthelateraljointinterlineofthekneeis seen,withappearanceofsubchondralcysts.Thus,itis impor-tant torecognize andsurgically treatthis conditionduring childhood.16
Surgicaltreatmentofcongenitaldislocationofthepatella hastheobjectiveofrealigningtheextensorapparatus. Sev-eral surgical procedures exist. Stanisavljevic’s procedure is amongthemostpopularmethodstoday.6Inthisprocedure,
theincisionisstarted5cmbelowthegreatertrochanterand thenextendsdistally,makesacurveatthebaseofthepatella and ends medially below the medial condyle of the tibia. The patella is displacedand aflap from the fascia lata is excisedandconservedinsalinesolution.Thejointcapsule isopenedlaterallyandthequadricepsisreleasedandplaced in its anatomical position. The patellar tendon is divided longitudinallyand itslateral portionissuturedasmedially as possible. The gap in the lateral portion of the thigh is closed using the flap from the fascia that was previously excised.7
112
rev bras ortop.2016;51(1):109–112Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. WalmsleyR.Thedevelopmentofthepatella.JAnat. 1939;74:360–9.
2. JohnsonEWJr,MilicicM.Congenitaldislocationofthe patella.ArchSurg.1972;105(1):110–2.
3. WadaA,FujiiT,TakamuraK,YanagidaH,SurijamornP. Congenitaldislocationofthepatella.JChildOrthop. 2008;2(2):119–23.
4. EilertRE.Congenitaldislocationofthepatella.ClinOrthop RelatRes.2001;(389):22–9.
5. WirthT.Congenitaldislocationofthepatella.Stuttgart: DepartmentofOrthopaedicsOlgahospital;2011.
6. CeynowaM,MazurekT.Congenitalpatelladislocationina childwithRubinstein–Taybisyndrome.JPediatrOrthopB. 2009;18(1):47–50.
7. StanisavljevicS,ZemenickG,MillerD.Congenital,irreducible, permanentlateraldislocationofthepatella.ClinOrthopRelat Res.1976;(116):190–9.
8.GhanemI,WattincourtL,SeringeR.Congenitaldislocationof thepatella.PartII.Orthopaedicmanagement.JPediatr Orthop.2000;20(6):817–22.
9.JonesRD,FisherRL,CurtisBH.Congenitaldislocationofthe patella.ClinOrthopRelatRes.1976;(119):177–83.
10.VaaraP,MarttinenE,PeltonenJ.Ultrasonographyofthe patellofemoraljointindiastrophicdysplasia.JPediatrOrthop. 1997;17(4):512–5.
11.WalkerJ,RangM,DanemanA.Ultrasonographyofthe unossifiedpatellainyoungchildren.JPediatrOrthop. 1991;11(1):100–2.
12.NietosvaaraAY,AaltoKA.Ultrasonographicevaluationof patellartrackinginchildren.ClinOrthopRelatRes. 1993;(297):62–4.
13.MuhleC,BrossmannJ,HellerM.KinematicCTandMR imagingofthepatellofemoraljoint.EurRadiol. 1999;9(3):508–18.
14.RechtM,BobicV,BursteinD,DislerD,GoldG,GrayM,etal. Magneticresonanceimagingofarticularcartilage.Clin OrthopRelatRes.2001;391Suppl.:S379–96.
15.NakanishiK,InoueM,HaradaK,IkezoeJ,MurakamiT, NakamuraH,etal.Subluxationofthepatella:evaluationof patellararticularcartilagewithMRimaging.BrJRadiol. 1992;65(776):662–7.