ww w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
Topographic
MRI
evaluation
of
the
sacroiliac
joints
in
patients
with
axial
spondyloarthritis
夽
Laís
Uyeda
Aivazoglou
a,
Orlando
Rondan
Zotti
b,
Marcelo
de
Medeiros
Pinheiro
c,
Moacir
Ribeiro
de
Castro
Junior
c,
Andrea
Puchnick
a,∗,
Artur
da
Rocha
Corrêa
Fernandes
a,
Eloy
de
Ávila
Fernandes
aaUniversidadeFederaldeSãoPaulo(UNIFESP),EscolaPaulistadeMedicina(EPM),DepartamentodeDiagnósticoporImagem(DDI),São
Paulo,SP,Brazil
bUniversidadeFederaldeSãoPaulo(UNIFESP),EscolaPaulistadeMedicina(EPM),DepartamentodeCirurgia,SãoPaulo,SP,Brazil cUniversidadeFederaldeSãoPaulo(UNIFESP),DepartamentodeMedicina,DisciplinadeReumatologia,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received29September2015
Accepted18May2016
Availableonline2December2016
Keywords:
Magneticresonanceimaging
Sacroiliacjoints Spondyloarthritis Sacroiliitis
Topographicevaluation
a
b
s
t
r
a
c
t
Objective:To evaluate the imaging featuresof spondyloarthritis in magneticresonance imaging(MRI)ofthesacroiliac(SI)jointandtopography(inthirds)andaffectedmargin, consideringthatthisissueisrarelyaddressedintheliterature.
Methods:Across-sectionalstudyevaluatingMRI(1.5T)ofSIin16patientswithaxial spondy-loarthritis,forthepresenceofacute(subchondralboneedema,enthesitis,synovitisand capsulitis)andchronic(erosions,subchondralbonesclerosis,bonybridges,andfatty infil-tration)changes,performedbytwoblindedradiologists.MRIfindingswerecorrelatedwith clinicaldata,includingage,durationofdisease,medications,HLA-B27,BASDAI,ASDAS-ESR
andASDAS-CRP,BASMI,BASFI,andmSASSS.
Results:Bone edema pattern and erosions were predominant in the upper third of SI (p=0.050andp=0.0014,respectively).Therewasacorrelationbetweendiseaseduration andstructuralchangesbyaffectedthird(p=0.028–0.037),aswellasbetweenthepresence ofbonebridgeswithBASMI(p=0.028)andmSASSS(p=0.014).Patientswithosteitisinthe lowerthirdshowedhighervaluesforASDAS(ESR:p=0.011andPCR:p=0.017).
Conclusion:Chronicinflammatorychangesandthepatternofboneedemapredominated intheupperthirdofSI,butasimultaneousinvolvementofmiddleorlowerthirdsofthe jointwasalsonoted.ThelocationofinvolvementintheupperthirdofSIisinsufficientto differentiatebetweendegenerationandinflammation.
©2016ElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedattheUniversidadeFederaldeSãoPaulo(UNIFESP),EscolaPaulistadeMedicina(EPM),DepartamentodeDiagnóstico porImagem(DDI),SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mail:andrea.ddi@epm.br(A.Puchnick). http://dx.doi.org/10.1016/j.rbre.2016.09.002
Avaliac¸ão
topográfica
das
articulac¸ões
sacroilíacas
por
ressonância
magnética
em
pacientes
com
espondiloartrite
axial
Palavras-chave:
Ressonânciamagnética
Articulac¸õessacroilíacas Espondiloartrite Sacroiliíte
Avaliac¸ãotopográfica
r
e
s
u
m
o
Objetivo: Avaliarascaracterísticasdeimagemdasespondiloartritesnaressonância mag-nética(RM)dasarticulac¸õessacroilíacas(SI) quantoàtopografia (emterc¸os)emargem acometida,umavezqueesseaspectoépoucoabordadonaliteratura.
Métodos: Estudotransversalcomavaliac¸ãoporRM(1,5T)dasSIem16pacientescom diag-nósticodeespondiloartrite axialquantoàpresenc¸a dealterac¸õesagudas(edemaósseo subcondral,entesite,sinoviteecapsulite)ecrônicas(erosões,escleroseósseasubcondral, ponteósseaesubstituic¸ãogordurosa),feitapordoisradiologistas,comleituracega.Os acha-dosdaRMforamcorrelacionadoscomdadosclínicos,incluindoidade,tempodedoenc¸a, medicac¸ões,HLA-B27,Basdai,Asdas-VHSeAsdas-PCR,Basmi,BasfiemSASSS.
Resultados: Padrãodeedemaósseoeerosõesapresentarampredomínionoterc¸osuperior dasSI(p=0,050ep=0,0014,respectivamente).Houvecorrelac¸ãoentreotempodedoenc¸ae alterac¸õesestruturaisporterc¸oacometido(p=0,028-0,037),bemcomoapresenc¸adepontes ósseascomoBasmi(p=0,028)eomSASSS(p=0,014).Pacientescomosteítenoterc¸oinferior apresentarammaioresvaloresdeAsdas(VHS:p=0,011ePCR:p=0,017).
Conclusão: Asalterac¸õesinflamatóriascrônicaseopadrãodeedemaósseopredominaram noterc¸osuperiordasSI,mastambémhaviaacometimentoconcomitantedosterc¸osmédio ouinferiordaarticulac¸ão.Alocalizac¸ãodoacometimentonoterc¸osuperiordasSIsemostra insuficienteparaadiferenciac¸ãoentredegenerac¸ãoeinflamac¸ão.
©2016ElsevierEditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCC BY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
The spondyloarthritides (SpA) are a group of disorders
withaprevalencefrom0.5to1.9%,encompassing
ankylos-ing spondylitis,psoriatic arthritis, arthritisassociated with inflammatoryboweldisease,reactivearthritis,and undiffer-entiatedforms.Inaddition,SpAexhibitageneticassociation
withhumanleukocyteantigen(HLA)B27,andanoverlapping
inclinicalformsmayoccurinthesame patient,orin first-degreerelatives.1,2
Theconventionalradiography (Rx) isinadequateforthe
diagnosisofthediseaseatanearlystage,especiallybefore
theonsetofstructuraldamage,sincethismodalitydoesnot
detectacuteinflammatorylesions,resultinginameandelay
of8–11yearsforobtainingadiagnosis.1,3
Duetodiagnosticdifficultiesandalsototheoverlapping ofclinicalcasesofmechanicalandinflammatorysacroiliitis,
atopographicstudy ofSpAbymagneticresonanceimaging
(MRI)canhelptofulfillthisgapintheliterature.
Thisstudywasintendedtodescribethetopographical fea-turesoftheinvolvementofsacroiliac(SI)jointswiththeuseof MRI,inordertoaidinginthedifferentiationbetween mechan-icalversusinflammatoryinvolvement,sincethesesubjectsare infrequentlyaddressedintheliterature.Inaddition,thestudy aimstocorrelateclinicalandlaboratorydatawiththeimaging findings.
Materials
and
methods
This is a cross-sectional observational study involving 16
patientsfromtheSpondyloarthritisOutpatientClinicofthe
Universidade FederaldeSãoPaulo (UNIFESP).Patientswith
axial SpAaccordingtothecriteriaproposed bythe
Assess-ment ofSpondyloarthritis InternationalSociety (ASAS) and
whowerereferredtoperformMRIoftheirSIjoints(24patients)
wereincluded.PatientswhoshowednochangeinMRIofthe
sacroiliacjointsandpatientswithincompletelaboratorydata wereexcluded;thus,16patientsremained.Ofthesepatients,
12 were diagnosed withankylosingspondylitisand 4were
diagnosedwithnon-radiographicaxialspondyloarthritis.The
tests were analyzed separately by two blinded radiologists
fromtheDepartmentofDiagnosticImaging(DDI)ofUNIFESP
withaspecializationinthemusculoskeletalsystemandwith
5and15yearsofexperience(MRCandEAF).Thecasesinwhich
therewasdisagreementwereresolvedbyconsensus.
MRI examinations were performed in DDI-UNIFESP in
Siemens (Siemens Medical Solutions, Erlangen, Germany)
andPhilips(Gyroscan;Philips,Eindhoven,TheNetherlands)
1.5-Tdeviceswithamatrixrangingfrom320×70to320×90.
All acquisitionswere of4-mm thickness.Theevaluationof
imageswasperformedonastandardvideomonitorwitha
32-bit,1024×768pixelsresolution.
The routine protocol used in the sacroiliac region
was: 3-plane finder, Coronal Short-Tau Inversion Recovery
(STIR), coronal fatsaturation T1-weightedMR image, axial
T1-weighted MR image; after an intravenous injection of
paramagnetic contrast, axial and coronal fat saturation
T1-weightedMRIimageswereobtained.
With the use of MRI, acute and chronic inflammatory
changesofSIjointswerestudied;SIjointsweredividedinto
threethirds: anupperthirdabovethefirst sacralforamen,
amiddlethirdbetweenthefirsttwosacralforamens,anda
Withregardtoacutechanges,thepresenceofosteitis,
char-acterizedbysubchondralboneedema(high-signalsequences
sensitivetoliquidandenhancedbycontrastmedium),was
checkedand topographed. Furthermore,signals of
capsuli-tis,enthesitisandsynovitiswerechecked;thesesignals, in
the absence of anassociated osteitis, are not sufficient to
ensureadiagnosisofactivesacroiliitis,asdefinedaccordingto
the resolution of the Outcome Measures inRheumatology
ClinicalTrials(OMERACT)104:
• Capsulitis:highsignalonSTIRand/orT1fat-satafter intra-venous(IV)contrastinanteriororposteriorcapsule,witha potentialformedialand/orlateralextensiontotheadjacent periosteum.
• Enthesitis: high signal on STIR and/or T1 fat-sat after
IV contrast in places where ligaments and tendons
are inserted into bones, including the retroarticular
space (interosseous ligaments). The signal change may
extend to the bone marrow and to adjacent soft
tissues.
• Synovitis:highsignalonT1fat-satafterIVcontrastinthe synovialportionoftheSIjoints(signalintensitysimilarto thatofbloodvessels).
Chronic injuries in the sacroiliac joints were
char-acterized by the presence of erosion, subchondral bone
sclerosis,bonybridgesandfattyinfiltration,asestablishedby ASAS.5
Throughananalysisofthemedicalrecords,thefollowing
clinicaldatawere recorded:age, gender,skincolor,disease
duration,continuoususeofnon-steroidalanti-inflammatory
drugs(NSAIDs) and other disease-modifyingantirheumatic
drugs (DMARDs) such as sulphasalazine and
methotrex-ate, as well as tumornecrosis factor inhibitors (anti-TNF),
HLA-B27survey,andspecifictoolsfortheevaluationof
dis-easeactivity(BASDAI–BathAnkylosingSpondylitisDisease
Activity Index and ASDAS – Ankylosing Spondylitis
Dis-easeActivityScorewithCRP–C-reactiveprotein,and with
ESR – erythrocyte sedimentation rate), mobility (BASMI –
BathAnkylosingSpondylitisMetrologyIndex),and function
(BASFI–BathAnkylosingSpondylitisFunctionalIndex),aswell
asforstructuraldamage(mSASSS–modifiedStoke
Ankylos-ingSpondylitisSpineScore).
MRIfindingswerecomparedwitheachotherandalsowith
theclinicaldataobtainedfrommedicalrecords,anda
corre-lationwasestablishedbetweenthedataondiseaseactivity
(BASDAI,BASFI,ASDAS-ESR,andASDAS-CRP)withacute
find-ingsbyMRIanddiseasedurationandclinicaltestsassociated
withchronicity(BASMIandmSASSS)withchronicfindingsby
MRI.
For categorical variables, chi-squared and Fisher exact
tests were used; for numeric variables, the Student’s
t-test for independent samples was used. In order to
simultaneously evaluate the association between
categor-ical (use of medications and changes observed in SI by
MRI) and numeric (disease duration, BASDAI, ASDAS-CRP,
ASDAS-ESR, BASMI, BASFI, mSASSS) variables, a cluster
analysis was carried out with the application of the
Stu-dent’st-test.Thesignificancelevel(p-value)consideredwas 0.05.
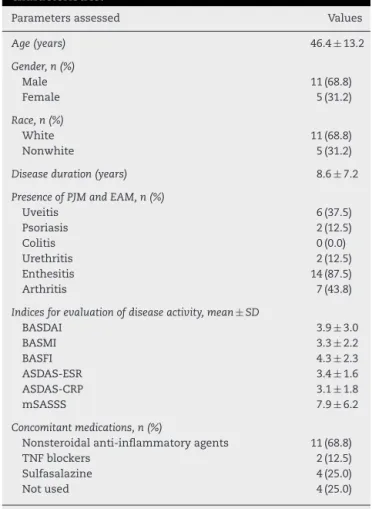
Table1–Demographic,clinicalandlaboratory characteristics.
Parametersassessed Values
Age(years) 46.4±13.2
Gender,n(%)
Male 11(68.8)
Female 5(31.2)
Race,n(%)
White 11(68.8)
Nonwhite 5(31.2)
Diseaseduration(years) 8.6±7.2
PresenceofPJMandEAM,n(%)
Uveitis 6(37.5)
Psoriasis 2(12.5)
Colitis 0(0.0)
Urethritis 2(12.5)
Enthesitis 14(87.5)
Arthritis 7(43.8)
Indicesforevaluationofdiseaseactivity,mean±SD
BASDAI 3.9±3.0
BASMI 3.3±2.2
BASFI 4.3±2.3
ASDAS-ESR 3.4±1.6
ASDAS-CRP 3.1±1.8
mSASSS 7.9±6.2
Concomitantmedications,n(%)
Nonsteroidalanti-inflammatoryagents 11(68.8)
TNFblockers 2(12.5)
Sulfasalazine 4(25.0)
Notused 4(25.0)
PJM, peripheral joint manifestations; EAM, extra-articular manifestations.
Results
Thegroupofpatientsstudiedwascomposedof11maleand
5femalesubjects,withameanageof46.4yearsandamean diseasedurationof8.6years.
TheHLA-B27waspositivein9(56.3%)patients,negative in6(37.5%)andunavailablein1(6.3%)patient.Table1shows demographic,clinicalandlaboratorydata.
InrelationtothetopographyofthefindingsbyMRI,the
upper third was the most affected, both by bone edema
(p=0.049)andbychronicchanges(p=0.0014).Inthecaseof
acutechanges,thesecondmostaffectedthirdwasthelower
third,andinthecaseofchronicchanges,themiddlethird.
Astatisticallysignificant correlationwas notedbetween
changesinupper,middleandlowerthirdscomparedtothe
presenceofedemaintheiliacface(p=0.050),thatis,when thechangewaspresentintheupperthirdoftheiliacborder, itwasalsopresentinthemiddle-orlowerthird.Thisdidnot occurinrelationtothepresenceofedemainthesacralmargin, inwhich2patientsshowedisolatededemaintheupperthird, orwhentheiliacandsacralfaceswereconsideredtogether.
U, upper third; M, middle third; L, lower third. U
M
L
Fig.1–Schematicdrawingofthedivisionintothirds performedtoevaluateimagingfindings.
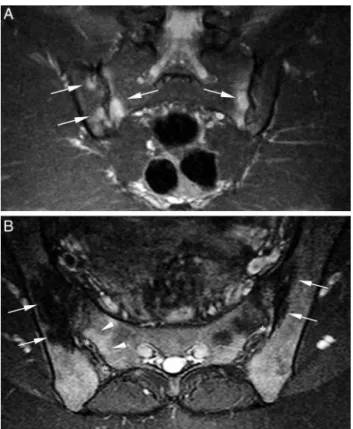
Fig.2–A,T2-weightedcoronalMRIimagewithfatsignal saturation,showingbonemarrowedemaintheupperand middlethirdsofsacroiliacjoints(arrows);B,T2-weighted axialMRIimagewithfatsignalsaturation,showingbone sclerosisintheupperthirdofsacroiliacjoints(arrows). Subchondraledemaintherightsacralaspect(arrowheads) andenthesitisiniliacandsacralaspects(asterisks)are found.
synovitis(n=5,31.2%)andenthesitis(n=4;25%;Fig.2). Cap-sulitiswasnotobserved.
Chronicchangeswereobservedinthemajorityofpatients
(n=14;87.5%).Thefindings(inorderofdecreasingfrequency) were erosions (n=13; 81.2%), subchondral sclerosis (n=6, 37.5%;Fig.2),fattyinfiltration(n=5,31.2%)andbonybridges (n=2;12.5%).
Patients withosteitissignals inthe lower thirdshowed
higher ASDAS-ESR and ASDAS-CRP values (p=0.011
Table2–Correlationofacutechangesandboneedema areasbythirdswithclinicalandlaboratorydatarelated todiseaseactivity.
Acutechanges Clinicallaboratorydata
BASDAI BASFI ASDAS-ESRASDAS-CRP
Boneedema
Presence(n=7) 3.4±3.4 3.5±2.3 3.8±2.0 3.4±2.4 Absence(n=9) 4.3±2.8 5.0±2.2 3.0±1.2 2.9±1.2 t-Test(p) 0.576 0.193 0.299 0.592
Enthesitis
Presence(n=4) 5.4±4.6 3.4±2.4 4.4±2.4 3.8±3.1 Absence(n=12) 3.4±2.3 4.7±2.3 3.0±1.1 2.8±1.2 t-Test(p) 0.256 0.346 0.144 0.357
Synovitis
Presence(n=5) 5.6±4.0 3.1±2.2 4.0±2.2 3.6±2.7 Absence(n=11) 3.1±2.2 4.9±2.3 3.1±1.2 2.9±1.3 t-Test(p) 0.133 0.167 0.261 0.457
Boneedema
Upperthird
Presence(n=6) 4.0±3.3 3.7±2.4 3.6±2.0 3.0±2.4 Absence(n=10) 3.9±3.0 4.7±2.3 3.2±1.3 3.2±1.4 t-Test(p) 0.946 0.416 0.680 0.863
Mediumthird
Presence(n=2) 6.7±4.7 2.8±2.5 5.3±2.7 5.0±3.7 Absence(n=14) 3.5±2.7 4.6±2.3 3.1±1.3 2.8±1.4 t-Test(p) 0.177 0.320 0.060 0.117
Lowerthird
Presence(n=3) 4.4±5.1 2.5±1.8 5.3±1.9 5.2±2.7 Absence(n=13) 3.8±2.6 4.8±2.3 2.9±1.1 2.6±1.2 t-Test(p) 0.752 0.135 0.011 0.017
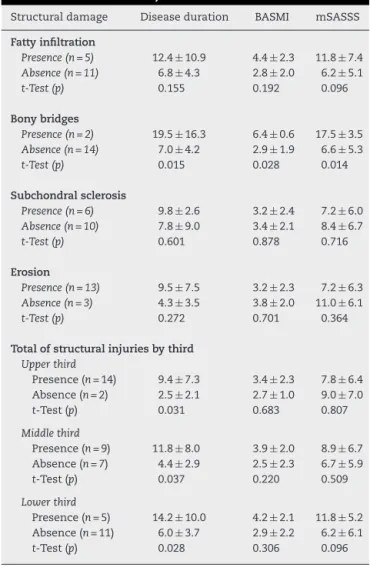
and p=0.017 respectively, Table 2). An association was
observedbetweenlongerdiseasedurationandthepresence
ofchronicchanges,bothgloballyaswellasbyinvolvedthird (upper:p=0.031; middle: p=0.037; lower:p=0.028; Table3).
Furthermore,an associationbetween thepresenceofbony
bridges,independentofthetopography,withlongerdisease
duration(p=0.015)andhighervaluesofBASMI(p=0.028)and mSASSS(p=0.014)wasalsoobserved.
Discussion
Magnetic resonance imagingisa breakthroughtechnology,
not only for diagnosis but possibly in the clinical
man-agement ofspondyloarthritides, including their differential
diagnosis and therapeutic monitoring,6,7 due to its
sensi-tivity and reliability for the evaluation of signs of active
inflammation.8
To the best ofour knowledge,the highestfrequencyof
acuteandchronicfindingsobservedinthisstudyintheupper thirdofsacroiliacjointsisanewfindingintheliterature.The
factthatboneedemaandchronicchangespresentthis
behav-iorsuggeststhatthishasbeenoneoftheactivitysitesofthe
disease,which has raisedquestions about the justification
fromthepointofviewofthejointanatomyandalsoofthe
Table3–Correlationofstructural(chronic)damage
versusdiseaseduration,BASMIandmSASSS.
Structuraldamage Diseaseduration BASMI mSASSS
Fattyinfiltration
Presence(n=5) 12.4±10.9 4.4±2.3 11.8±7.4 Absence(n=11) 6.8±4.3 2.8±2.0 6.2±5.1 t-Test(p) 0.155 0.192 0.096
Bonybridges
Presence(n=2) 19.5±16.3 6.4±0.6 17.5±3.5 Absence(n=14) 7.0±4.2 2.9±1.9 6.6±5.3 t-Test(p) 0.015 0.028 0.014
Subchondralsclerosis
Presence(n=6) 9.8±2.6 3.2±2.4 7.2±6.0 Absence(n=10) 7.8±9.0 3.4±2.1 8.4±6.7 t-Test(p) 0.601 0.878 0.716
Erosion
Presence(n=13) 9.5±7.5 3.2±2.3 7.2±6.3 Absence(n=3) 4.3±3.5 3.8±2.0 11.0±6.1 t-Test(p) 0.272 0.701 0.364
Totalofstructuralinjuriesbythird
Upperthird
Presence(n=14) 9.4±7.3 3.4±2.3 7.8±6.4 Absence(n=2) 2.5±2.1 2.7±1.0 9.0±7.0 t-Test(p) 0.031 0.683 0.807
Middlethird
Presence(n=9) 11.8±8.0 3.9±2.0 8.9±6.7 Absence(n=7) 4.4±2.9 2.5±2.3 6.7±5.9 t-Test(p) 0.037 0.220 0.509
Lowerthird
Presence(n=5) 14.2±10.0 4.2±2.1 11.8±5.2 Absence(n=11) 6.0±3.7 2.9±2.2 6.2±6.1 t-Test(p) 0.028 0.306 0.096
Anatomy
of
the
sacroiliac
joints
Thesacroiliacjointisconsidered a“amphiarthrosis”,9 with
acartilaginousdiarthrodial(synovial) portion(composedof
sacralandiliacauricularfaces),andwithotherfibrousportion (throughinterosseousligaments).Itscartilaginousportion(in theshapeofCwiththeconvexitytowardtheanterioraspect) isconsideredasasynovialjointsince1920,butthisisnota usualsynovialjoint,inviewoftheuniquecharacteristicsof thesacroiliacjoint.First,thearticularsurfacesareprovided, onthesacralside,withathickhyalinecartilage;andinthe iliacface,thejointisfibrocartilaginous.Additionally,thejoint capsuleisfibrousandshowsareasofdiscontinuity.
Intheupperthirdofthesacroiliacjoint,thepresenceof thickbandsoffibroustissuestandsout,withawide transi-tionalareacomposedoffibrocartilage,beginningintheventral sacroiliacligamentwithitsinsertiononthesacralandiliac articularcartilage.Dorsally,intheligamentalportionofthe joint,ligament-resistantfibersinsertbothintheboneandin sacralandiliaccartilages.10
Puhakka et al.,11 when correlating the histology of the
sacroiliacjointwithMRIfindings,showedanabsenceof syn-ovialtissueintheupperthirdofthejointinnormalindividuals
withinthecartilaginousregionandthejointcapsule.Bowen
andCassidy10reportedthatthejointcapsule,fromthethird andfourthdecadesoflife,becomesmorecollagenousandless cellular,whichcouldexplaintheabsenceofsynovialtissuein thepathologystudybyPuhakkaetal.,11inwhichthecadavers
wereagedbetween20and45years.
Pathophysiology
of
spondyloarthritides
In ankylosingspondylitis,thefinding ofanenthesitisisso
striking astobeconsidered theprimary lesionofthis
dis-ease.Inotherspondyloarthritides,BenjaminandMcGonagle12
proposed that the synovitis is secondary to the release of
inflammatory mediatorsfrom the involvementof adjacent
entheses.
Correlatingthesedatatothefactthattheiliacfaceis
cov-ered by fibrocartilage, and sincethe inflammatory activity
usuallyhasitsonsetandpredominatesonthisface,these
lig-amentalandcartilaginousfibrouscomponentsmaybethekey
totheantigentargetinvolved.13,14Theremaybeapossibility thatthefibrouscomponentoffibrocartilageisthepreferred targetofaninflammatoryattack,insteadofthepurelyhyaline cartilagepresentonthesacralsideofthejoint.
There are two typesofentheses12: fibrous and
fibrocar-tilaginous, and the involvement of spondyloarthritides is
generallylocatedintheformertype,sparingthelattertype.
Thefibrocartilaginousenthesesarenotmeretendonor
liga-mentjunctionstothebone,andcanbeconsideredascomplex
organs.Thiscomplexityisnotonlyobservedin“true” enthe-sesbut alsoinattrition siteswithbonesurfacesor fibrous structures,whentheyarethencalledfunctionalentheses.One shouldstillcommentonthesimilarityofthistypeofenthesis withthefibrocartilaginousliningofsomearticularsurfacesin synovialjoints,whosethemoststrikingexampleistheiliac sideofthesacroiliacjoint.
Onlytheconstitutionofenthesesdoesnotdeterminetheir
involvement, and it has been noted that osteitisseems to
followmechanicalstresslines, andalsothatthe functional
enthesesareaffected–althoughthereisnodirectcontactwith
the bonycomponent. Thus, it appears that biomechanical
influencescaninitiateand/orperpetuateboneinflammatory
changes.13
Itislikelythatthepresenceofacuteandchronic
inflam-matory changes prevalent in the upperthirdof thejoints,
foundinthisstudy,relatestotheanatomicaland
pathophys-iologicalcharacteristicscommentedabove,correspondingto
theinflammatoryactivityinentheses,andalsoinvolvingthe upperthirdofthesacroiliacjoints.Boneerosionswerefound predominantlyintheupperthirdsoftheiliacfaces.Assuming thatthoseerosionsarethemostspecificfinding15of spondy-loarthritides,ourfindingssuggestthatinflammatoryactivity hasalsooccurredintheupperthird.However,itisimportant
toemphasizethatinnopatientaninvolvementsolelyonthe
upperthirdoftheSIoccurred.
Thereisnoconsensusintheliteratureregardingthe topo-graphiccriterion ofsclerosisinthe sacroiliacjoints forthe definitionofdegenerativechange.Resnicketal.16evaluated thedegenerativearthropathyofthesacroiliacjointsusing
con-ventional radiography,havingfoundthatthefocal sclerosis
thesacroiliacjointcavity.Shibataetal.17performeda tomo-graphicevaluation;thefindingof(degenerative)sclerosiswas
morecommonintheupperandmiddleportionsofthe
ante-rioriliacjointface.Intheirhistologicalevaluation,Brunner
et al.18 found a higher frequency of degenerative changes
inthemiddlethird.In ourstudy,the greatestfrequencyof
findingsofsclerosisintheupperthirdofthesacroiliacjoint
could raisethe question astoits degenerative origin,
con-sideringthatmorethanhalfofourpatientswereagedover
50yearsand,inaddition,findingsofdegenerativearthropathy aredescribedincreasinglyfromtheageof20.10However,given theconcomitancewithothermorespecificfindingsfor inflam-matoryarthropathy(erosions,fattyinfiltration)intheupper thirdofthesacroiliacjoints,webelievethatsclerosisshould berelatedtochronicstructurallesionsofspondyloarthritis.
In this study, the observation of a higher frequency of
chronicversusacutechangescanbejustifiedbythelongmean
diseasedurationinourpatients, consideredfromdiagnosis
(8.2 years). Consideringthat the diagnosis may have been
delayedprimarilyduetothesoleevaluationbyconventional
radiography,19itcanbeinferredthattheactualdisease dura-tionshouldbeevengreaterthanthatfound.
Thelongdurationofthediseasefavorstheviewpointthat
thechronicchangesshouldchangetheloadaxisofitsaxial
skeleton,bythechangeinsagittalbalanceinthefaceofthe rectificationoflumbarlordosis,andbyvariablechangesof
tho-racickyphosis.KnowingthatthemovementoftheSIjoints
occursbynutationandcounter-nutation,andthatthepivot
ofthejointistheiliactubercleatS2level,posteriorlytothe auricularfaceofthejoint,9,18morestudiesareneededto eval-uatehowthestructuralchangesinfluencethesagittalbalance, andifthisrelatestothetopographyofthelesions.
Correlation
of
MRI
findings
with
clinical
and
laboratory
data
ThehigherASDAS-ESRandASDAS-CRPvaluesinpatientswith
signsofosteitisinthelowerthirdsuggestthattheseareasof
boneedemawererelatedtotheinflammatoryactivity.
Thestatistical correlation between the chronic findings
anddiseasedurationissupportedbythelongmeandisease
duration of the patients, as well as by the possible
diag-nosticdelayinherenttotheconventionalradiologicmethod.
The significant correlation between the presence of bony
bridges,regardlessofthetopography,withBASMIandmSASSS
strengthentherelationshipbetweenthestructuraldamageof
theSIjointswiththejointsofthespineandimpairedmobility.
Thelimitationsofthisstudyincludedthelimitedsample
andthevariabletimeintervalbetweentheonsetofsymptoms, diagnosis,andMRI.
Conclusions
Chronicinflammatorychanges anda patternofbone
mar-rowedemapredominatedintheupperthirdofthesacroiliac
joints,but these findings were also observed in the lower
2/3ofthese joints,suggesting thatthe whole joint can be
affectedbytheinflammatoryprocessofthesynovio-entheseal
complexinpatientswithaxialSpA.Ontheotherhand,only
the location doesnot seemtobe sufficienttodifferentiate
betweeninflammatoryversusdegenerativechanges.
In addition, there was asignificant correlation between
ASDAS-ESRandASDAS-CRPwiththepresenceofosteitisin
thelowerthirdofSIjointsandbetweenthelongdurationof thediseasewiththepresenceofchronicstructuralchanges,as
wellasbetweenclinicalassessmenttoolsBASMIandmSASSS
withthepresenceofbonybridgesinSIjoints.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.MagerAK,AlthoffCE,SieperJ,HammB,HermannKG.Roleof whole-bodymagneticresonanceimagingindiagnosingearly spondyloarthritis.EurJRadiol.2009;71:182–8.
2.RudwaleitM,vanderHeijdeD,KhanMA,BraunJ,SieperJ. Howtodiagnoseaxialspondyloarthritisearly.AnnRheum Dis.2004;63:535–43.
3.WeberU,HodlerJ,KubikRA,RufibachK,LambertRG, KisslingRO,etal.Sensitivityandspecificityofspinal inflammatorylesionsassessedbywhole-bodymagnetic resonanceimaginginpatientswithankylosingspondylitisor recent-onsetinflammatorybackpain.ArthritisRheum. 2009;61:900–8.
4.RudwaleitM,JurikAG,HermannKG,LandeweR,vander HeijdeD,BaraliakosX,etal.Definingactivesacroiliitison magneticresonanceimaging(MRI)forclassificationofaxial spondyloarthritis:aconsensualapproachbythe
ASAS/OMERACTMRIgroup.AnnRheumDis.2009;68:1520–7. 5.SieperJ,RudwaleitM,BaraliakosX,BrandtJ,BraunJ,
Burgos-VargasR,etal.TheAssessmentofSpondyloArthritis internationalSociety(ASAS)handbook:aguidetoassess spondyloarthritis.AnnRheumDis.2009;68Suppl.2:ii1–44. 6.CarmonaR,HarishS,LindaDD,IoannidisG,MatsosM,
KhalidiNA.MRimagingofthespineandsacroiliacjointsfor spondyloarthritis:influenceonclinicaldiagnosticconfidence andpatientmanagement.Radiology.2013;269:208–15. 7.TelesMS,FernandesARC,PinheiroMM,FernandesEA.
Influênciadaressonânciamagnéticadacolunavertebrale dasarticulac¸õessacroilíacasnomanejoclínicodepacientes comespondiliteanquilosante.SãoPaulo:Universidade FederaldeSãoPaulo;2012.
8.RennieWJ,DhillonSS,Conner-SpadyB,MaksymowychWP, LambertRG.Magneticresonanceimagingassessmentof spinalinflammationinankylosingspondylitis:standard clinicalprotocolsmayomitinflammatorylesionsinthoracic vertebrae.ArthritisRheum.2009;61:1187–93.
9.VleemingA,SchuenkeMD,MasiAT,CarreiroJE,DanneelsL, WillardFH.Thesacroiliacjoint:anoverviewofitsanatomy, functionandpotentialclinicalimplications.JAnat. 2012;221:537–67.
10.BowenV,CassidyJD.Macroscopicandmicroscopicanatomy ofthesacroiliacjointfromembryoniclifeuntiltheeighth decade.Spine(PhilaPa1976).1981;6:620–8.
11.PuhakkaKB,MelsenF,JurikAG,BoelLW,VesterbyA,EgundN. MRimagingofthenormalsacroiliacjointwithcorrelationto histology.SkeletalRadiol.2004;33:15–28.
13.BraunJ,SieperJ.Thesacroiliacjointinthe
spondyloarthropathies.CurrOpinRheumatol.1996;8:275–87. 14.McGonagleD,BenjaminM,Marzo-OrtegaH,EmeryP.
Advancesintheunderstandingofenthesealinflammation. CurrRheumatolRep.2002;4:500–6.
15.WickMC,WeissRJ,JaschkeW,KlauserAS.Erosionsarethe mostrelevantmagneticresonanceimagingfeaturesin quantificationofsacroiliacjointsinankylosingspondylitis.J Rheumatol.2010;37:622–7.
16.ResnickD,NiwayamaG,GoergenTG.Comparisonof radiographicabnormalitiesofthesacroiliacjointin
degenerativediseaseandankylosingspondylitis.AmJ Roentgenol.1977;128:189–96.
17.ShibataY,ShiraiY,MiyamotoM.Theagingprocessinthe sacroiliacjoint:helicalcomputedtomographyanalysis.J OrthopSci.2002;7:12–8.
18.BrunnerC,KisslingR,JacobHA.Theeffectsofmorphology andhistopathologicfindingsonthemobilityofthesacroiliac joint.Spine(PhilaPa1976).1991;16:1111–7.