SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
Article
Evaluation
of
the
effectiveness
of
platelet-rich
plasma
in
the
bone
consolidation
of
patients
submitted
to
lumbar
arthrodesis
夽
Caroline
Ferraz
Rezende
a,
Danielly
de
Paula
Azevedo
a,
Rafael
Burgomeister
Lourenc¸o
b,
José
Fernando
Duarte
c,
Igor
Machado
Cardoso
d,
Charbel
Jacob
Júnior
d,∗aEscolaSuperiordeCiênciasdaSantaCasadeMisericórdia(Emescam),Vitória,ES,Brazil
bCentrodeDiagnósticoporImagem(CDI)doEspíritoSanto,Vitória,ES,Brazil
cUniversidadeFederaldoEspíritoSanto(UFES),DepartamentodeOrtopediaeTraumatologia,Vitória,ES,Brazil
dHospitalSantaCasadeMisericórdiadeVitória,GrupodeColunaVertebral,Vitória,ES,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received14June2016 Accepted3October2016 Availableonline19October2017
Keywords: Lowbackpain Arthrodesis Plasma
a
b
s
t
r
a
c
t
Objective:Todeterminewhethertheuseofautograftassociatedwithplatelet-richplasma (PRP)increasesbonehealinginpatientsundergoinglumbarfusion.
Method:Thiswasa prospective, descriptive, andcomparative study,whichincluded40 patientsundergoinglumbarfusion,whoweredividedintotwogroups:groupI,autograft
only,andgroupII,autograftassociatedwithPRP.Aftersurgery,patientswerefollowed-up
onthefirst,third,andsixthmonth.TheMolinariradiographicclassificationandGlassman tomographicclassificationwereusedascriteriatoanalyzetheboneconsolidation. Result:ComparingthegroupIwithgroupII,accordingtothecriteriaofMolinari,bilateral
fusionwasobservedin27.5%ofthepatientsingroupIinthefirstmonthaftersurgery.
IngroupII,therateofbilateralfusionwas25.0%and20%inthethirdandsixthmonths,
respectively.Theresultsofcomputedtomographyscansperformedatsixmonthsafter surgeryindicated,accordingtothecriteriaofGlassman,arateofbilateralsolidfusionof 15.0%and10.0%ingroupsIandII,respectively.
Conclusion: TheuseofPRP showednosignificantdifferenceinbonehealingincasesof lumbararthrodesis.
©2017PublishedbyElsevierEditoraLtda.onbehalfofSociedadeBrasileiradeOrtopedia eTraumatologia.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedattheHospitalSantaCasadeMisericórdiadeVitória,GrupodeColunaVertebral,Vitória,ES,Brazil.
∗ Correspondingauthor.
E-mail:jcharbel@gmail.com(C.JacobJúnior).
http://dx.doi.org/10.1016/j.rboe.2017.10.006
Avaliac¸ão
da
eficácia
do
plasma
rico
em
plaquetas
na
consolidac¸ão
óssea
de
pacientes
submetidos
a
artrodese
lombar
Palavras-chave: Dorlombar Artrodese Plasma
r
e
s
u
m
o
Objetivo: Analisarseousodeenxertoautólogoassociadoaplasmaricoemplaqueta(PRP) aumentaaconsolidac¸ãoósseaempacientessubmetidosàartrodeselombar.
Método: Estudo prospectivo,decaráterdescritivoecomparativo,com40 pacientes sub-metidosàartrodeselombar,queforamdivididosemdoisgrupos:grupoI,somenteenxerto
autólogo,egrupoII,enxertoautólogoassociadoaPRP.Apósoprocedimentocirúrgico,o
acompanhamentofoifeitonoprimeiro,terceiroesextomês.Oscritériosdeclassificac¸ão radiográficadeMolinarietomográficadeGlassmanforamusadoscomopadrãoparaanalisar aconsolidac¸ão.
Resultado: Nacomparac¸ãodogrupoIcomogrupoIInoprimeiromêsdepós-operatório,de
acordocomoscritériosdeMolinari,27,5%dospacientesapresentaramfusãobilateralno grupoI.Noterceiroesextomês,observou-seumataxadefusãobilateralde25%e20%para
ogrupoII.Oresultadodastomografiasfeitasnosextomêsdepós-operatórioindicou,de
acordocomoscritériosdeGlassman,umataxadefusãosólidabilateralde15%e10%nos gruposIeII,respectivamente.
Conclusão: Observou-se que o uso do PRP não apresentou diferenc¸a significativa na consolidac¸ãoósseanasartrodeseslombares.
©2017PublicadoporElsevierEditoraLtda.emnomedeSociedadeBrasileirade OrtopediaeTraumatologia.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Low back pain has been considered a frequent cause of morbidityand disabilityinthegeneralpopulation, present-ing a higher prevalence among females and those aged 40–80 years.1 Vertebral instability, whether or not
associ-atedwithdisk disease,isanimportantetiologicalfactor in thispathology.Incasesrefractorytoconservativetreatment, and aftercarefuland accurate diagnosis ofinstability, sta-bilizationof theaffected segment (vertebral arthrodesis) is indicated.
Whenvertebralarthrodesisisperformed,itisnecessaryto usesometypeofgraftand/orbonesubstituteattheosteotomy siteinordertoacceleratetheprocessofboneconsolidation. Themostcommonlyusedoneforthispurposeisthe autolo-gousgraft.2
Theuseoftheautologousgraft isthegoldstandard for arthrodesis,duetoitsosteogenic(osteoblasticcells derived fromthemedullaandpre-osteoblasts),osteoconductive (col-lagen and mineral matrix), and osteoinductive properties (growthfactors),inadditiontothefactthatitdoesnottrigger immuneresponseandinfectiousdiseases.Inturn,itpresents severallimitations,suchas:exhaustiblesources,whichlimits itsuse inchildrenandinsurgicalrevisions; frequent pres-ence ofmorbidity atthe donor site; and the fact that its quality depends on the age and general condition of the individual.3
The first lumbar arthrodesis was described in 1911 by Russel Hibbs and Fred Albee; the procedure, which was done in situ with autologous graft, was indicated for the preventionofprogressivespinaldeformity.4–6 In the 1970s,
Roy-Camillepopularizedtheuseofpediclescrewsinvertebral arthrodeses,7,8whichgreatlycontributedtothereductionof
thenonunionrate,acomplicationstillverymuchfearedby spinesurgeons.9
Consideringtheimportanceofadequatebonehealingfor the success of vertebral arthrodesis surgery and the vari-ousexistinglimitationsfortheuseofautologousgrafts,an increase in the number of studies with the use of bone substitutesassociatedwithhydroxyapatite(HA),bone mor-phogeneticproteins(BMP),andplatelet-richplasma(PRP)has been observed. Amongthe aforementioned materialswith osteoinductiveproperties,theliteraturedescribesPRPasone ofthemostusedandresearched.2
PRPisobtainedfromautologousbloodcentrifugation;its application at the surgical site releases several naturally occurring growth factors, such as platelet-derived growth factor (PDGF),transforminggrowth factorbeta(TGF-),and vascular endothelial growth factor (VEGF). It is comprised of these growth factors and clot-forming cells. These, in turn,serveasthecarrierofsaidgrowth factors.This prop-ertydifferentiatesitfromrecombinantgrowthfactors,such as BMPs and HA, allowing it to promote and stimulate the differentiation of stem cells from the mesenchymal system into osteoblasts and accelerate the bone healing process.2
Materials
and
methods
Thisis a retrospective, descriptive, and comparative study with 40 randomized patients. Sample size was calculated basedonbibliographicreviews,forconvenience,inpatients who were attended to at the Department ofDegenerative PathologiesoftheSpineGroupoftheHospitalSantaCasade MisericórdiadeVitória,fromAugustof2013toAugustof2015. Thestudy wasapprovedbytheResearchEthics Committee underno.009632/2013andCAAE12039813.3.0000.5065.
Througha carefulselection,the samplecomprisedonly of patients with degenerative pathologies who underwent arthrodesisofuptotwolumbarlevels (comprisingthe lev-els between L3-L4, L4-L5, and L5-S1), older than 18 years, who were attended to at the Department ofDegenerative Pathologiesof the SpineGroup ofthe HospitalSanta Casa de Misericórdia de Vitória, in the aforementioned period, andwhosignedtheinformed consent.Patientswithtumor pathologiesandinfections,surgicalrevisions,traumas,and thoseunder18yearsofagewereexcluded.
Asheetwithpatientdataincludedvariablessuchasage, gender, diagnosis, participant group, level of surgery, and follow-upduration.Thegroupsweredividedinthe preoper-ativeperiodbyamemberoftheorthopedicgroupwhowas notamongtheauthorsofthestudy,throughasimplepaper drawinwhich40 cardswereplacedinabox,20 labeledas groupIand20asgroupIl.IngroupI,patientsreceivedonly
autologousgraft;ingroupII,theyreceivedautologousgraft
associatedwithPRP.Aftereachdraw,thecardremovedfrom theurnwasdiscarded.
Duringsurgery,theautologousgraftwasremovedfromthe spinalprocess,laminae,andarticularfacetsduring decom-pression of the vertebral canal at the level in question. Subsequently,thisgraftwaspreparedinthinsections,leaving only cancellous bone. The graft was placed in the inter-transversespacetofinishthelumbararthrodesisonlywith autologousgraft.
For lumbararthrodesiswithautologousgraft associated withPRP,infirstplaceit wasnecessarytopreparethePRP: thepatient’sownbloodwascollected,followedby centrifu-gationandseparationoftheplasma.Thepatient’sbloodwas placedin3.6mLvacuumtubeswithACD(citricacid,sodium citrate,anddextrose)anticoagulant.Thematerialcollectedin theACDtubeswascentrifugedforplateletconcentration,ata speedof1800rpm,foreightminutes.Aftercentrifugation,the upperportion,about80%plasma,wasremovedfromtheACD tubes.Thisportioncorrespondstotheplatelet-poorplasma (PPP).Theremaining20%correspondedtoPRP;0.5–1mLofthis PRPwerecollectedabovethebuffycoat.ForPRP activation, 10%calciumchloridewasaddedattherateof0.1mLforeach 1mLPRPtobeused;thepreparationwasplacedinawarm waterbathfor15min.11Thisconcentratewasthenaddedto
theinitialautologousgraftandappliedtotheintertransverse spaceofthelumbarspine.
Thepostoperativeevaluationoftheconsolidationwas per-formedat threemoments (one, three, and six months) by master surgeonsand byradiologists specialized in muscu-loskeletalimagingwhowerenotawareofthegrouptowhich thepatientinquestionbelonged.Duringtheanalysisofbone
Table1–Molinariradiographicclassification.
Grade Description
I Bilateralfusionwithpresenceofthetrabeculaeinthe
transverseprocess
II Unilateralfusion,withdifficultytovisualizetheother
side
III Suspectedradiolucencyordefectinthefusionarea
IV Reabsorptionofthegraftwithinstrumentationfatigue
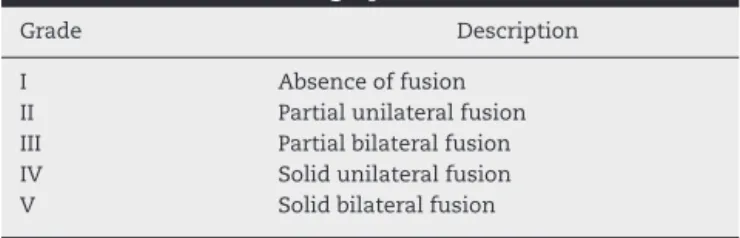
Table2–Glassmantomographicclassification.
Grade Description
I Absenceoffusion
II Partialunilateralfusion
III Partialbilateralfusion
IV Solidunilateralfusion
V Solidbilateralfusion
fusioninthelumbarspine,thesideswerenotevaluated sep-arately, as there is no currently validated classification to compare them.In viewofthis,the criteria ofthe Molinari radiographicclassification(Table1)wereusedasstandard.12
Asinglepostoperativetomographicevaluationwasperformed atsixmonths,followingtheGlassmanclassificationcriteria (Table2).12
A descriptive statistical analysis was performed, using meanandstandarddeviationsforthevariableofage.The chi-squaredtestwasusedtoverifytheassociationbetweenthe qualitativevariablesandtheassociationofsignificanceinthe twogroups.Thelevelofsignificancewassetatp<0.05.Excel 2010andSSPSv.23wereusedfordataanalysis.
Results
Thestudy assessed40patientsfromAugust2013toAugust 2015. The mean age of the study population was 49.18 years±10.02 (SD), with a predominance of females (65%). Theinclusion diagnosis were hernia withinstability(n=5), spondylolisthesis(n=12),andherniawithstenosis(n=23).
Radiologicalfindings
Basedontheradiographsobtainedinthefirstpostoperative month,accordingtotheMolinaricriteria,ingroupsIandII
therateofbilateralfusionwas27.5%and22.5%;ofunilateral fusion,12.5%and10%;andofdefectsinthefusionarea,5% and12.5%,respectively.Therateofgraftresorptionwas5%for bothgroups(p=0.660;Table3).
IngroupsIandII,inthethirdpostoperativemonth,the rateofbilateral fusionwas20%and 25%;unilateralfusion, 17.5% and 7.5%;defects in the fusion area, 7.5%and 10%; and graft resorption, 5% and 7.5%, respectively (p=0.539;
Table4).
Table3–Classificationofthelumbosacralradiographon thefirstpostoperativemonth.
GroupI GroupII Total
Molinari–firstmonth
Bilateralfusion
Number 11 9 20
%ofthetotal 27.5% 22.5% 50.0%
Unilateralfusion
Number 5 4 9
%ofthetotal 12.5% 10.0% 22.5%
Defectinthefusionarea
Number 2 5 7
%ofthetotal 5.0% 12.5% 17.5%
Graftresorption
Number 2 2 4
%ofthetotal 5.0% 5.0% 10.0%
Total
Number 20 20 40
%ofthetotal 50.0% 50.0% 100.0%
Source:Theauthors.
Table4–Classificationofthelumbosacralradiographon thethirdpostoperativemonth.
GroupI GroupII Total
Molinari–thirdmonth
Bilateralfusion
Number 8 10 18
%ofthetotal 20.0% 25.0% 45.0%
Unilateralfusion
Number 7 3 10
%ofthetotal 17.5% 7.5% 25.0%
Defectinthefusionarea
Number 3 4 7
%ofthetotal 7.5% 10.0% 17.5%
Graftresorption
Number 2 3 5
%ofthetotal 5.0% 7.5% 12.5%
Total
Number 20 20 40
%ofthetotal 50.0% 50.0% 100.0%
Source:Theauthors.
Table5–Classificationofthelumbosacralradiographon thesixthpostoperativemonth.
GroupI GroupII Total
Molinari–sixthmonth
Bilateralfusion
Number 6 8 14
%ofthetotal 15.0% 20.0% 35.0%
Unilateralfusion
Number 7 2 9
%ofthetotal 17.5% 5.0% 22.5%
Defectinthefusionarea
Number 5 7 12
%ofthetotal 12.5% 17.5% 30.0%
Graftresorption
Number 2 3 5
%ofthetotal 5.0% 7.5% 12.5%
Total
Number 20 20 40
%ofthetotal 50.0% 50.0% 100.0%
Source:Theauthors.
Table6–Classificationofthelumbosacralcomputed tomographyonthesixthpostoperativemonth.
GroupI GroupII Total
Glassman
Absenceoffusion
Number 0 2 2
%ofthetotal 0.0% 5.0% 5.0%
Partialunilateralfusion
Number 3 2 5
%ofthetotal 7.5% 5.0% 12.5%
Partialbilateralfusion
Number 6 4 10
%ofthetotal 15.0% 10.0% 25.0%
Solidunilateralfusion
Number 5 8 13
%ofthetotal 12.5% 20.0% 32.5%
Solidbilateralfusion
Number 6 4 10
%ofthetotal 15.0% 10.0% 25.0%
Total
Number 20 20 40
%ofthetotal 50.0% 50.0% 100.0%
Source:Theauthors.
Tomographicresults
Basedontheresultsofthecomputedtomographyscans per-formedinthesixthpostoperativemonthingroupsIandII, accordingtoGlassmancriteria,therateofabsenceoffusion was0%and5%;unilateralpartialfusion,7.5%and5%; bilat-eralsolidfusion,15%and10%;solidunilateralfusion,12.5% and20%;andsolidbilateralfusion,15%and10%,respectively (p=0.499;Table6).
Discussion
Thesearch forthedevelopmentoftechniques and materi-alsthatallowbonereplacementisanecessityfororthopedic surgery. Bone fusion is of fundamental importance in the postoperativestabilization ofspinalarthrodeses.Therefore, it is essential to use graft materials that favor bone neo-formationthatsufferedvertebralsegmentosteotomyduring surgery.2
Autologous bone isan idealgraft materialdue tothree mainproperties:thepresenceofosteogeniccells,its osteocon-ductivestructure,anditsosteoinductivematrix.Autologous graft implies greateroperativemorbidityinorder toobtain asmall amountofgraft.Hencetheneedtosearchfor bio-material options that favor bone fusion in arthrodeses.13
One option is HA, a porous synthetic bone that is used as a non immunogenic complementary graft of unlimited quantity; however, it only has osteoconductive properties. Toovercomethislimitation,acombinationwithan osteoin-ductive material,suchasBMP, isrecommended.14 Another
and fibroblasts, fibroblasticproliferation, angiogenesis,and fibroblast and osteoblast mitosis. The latter has a mito-genic actionon fibroblasts, chondroblasts,and osteoblasts; it also has chemotaxis, collagen synthesis, and osteoblas-tic functions, and acts in the synthesis of other factors andinthedifferentiationofundifferentiatedmesenchymal cells.15
Somestudieshavedemonstrated theuse ofPRPforthe treatmentofothermusculoskeletaldiseases,describingthe results in cartilage, bone, muscle, tendon, and ligament, althoughthisaspecthasnotbeenwidelydocumentedinthe literature.16
Lenzaetal.,17inareviewstudy,demonstratedthat
autol-ogousbonegraftscombinedwithPRPshowedpositiveresults inacceleratingbonehealinginanimalmodels.
Marxet al.18 observedpromisingresultsregarding bone
formationinthetreatmentofmandibulardefects.WhenPRP wasused,radiographicbonematurationwas1.62–2.16times faster.In thepresent study,nosignificant differenceswere observedinbonehealingbetweenthetwogroupsinthefirst, third,andsixth postoperativemonths.Itwasobservedthat theuseofPRPinlumbararthrodesesdidnotpresenta sig-nificantdifferenceinthetomographicevaluationinthesixth postoperativemonth.Thesixmonthpostoperativefollow-up didnotharmthepatients.
Agreatdifficultyinevaluatingtheeffectivenessofabone substituteinpromotingconsolidationisthelargenumberof variablespresentintheprocedures inwhichthesubstitute wasapplied.Thereissomeevidencethatthemoreadvanced the ageof the patient, the moreineffectivethe consolida-tion process.8 However,in the present study,inwhich the
meanageofgroupIwas48.7yearsandofgroupIIwas49.6
years,nosignificantdifferenceswereobservedintheresults of bone maturation. Osteoporosis is an important pathol-ogy that negatively influences this process; it is assessed throughbonemineraldensityinwomenagedover65years and menover 70 years.19 As the mean age ofthe present
study population was 49.18 years, this pathology was not investigated.
Inlightoftheaforementionedresults,itisnotedthatthe true potentialofthis blood derivativestill requires further studiesandsubstantialtrialspriortoanindiscriminate appli-cationofPRPinlumbararthrodesis.20
Conclusion
Basedonthe present results,it was observedthatthe use ofPRP didnotpresent a significant differencein the bone consolidationprocess oflumbararthrodeses.However,due tothetruepotentialofthisbloodderivative,furtherstudies areneededinordertodrawbetterconclusionsregardingits efficacy.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.HoyD,BainC,WilliamsG,MarchL,BrooksP,BlythF, etal.Asystematicreviewoftheglobalprevalenceof lowbackpain.ArthritisRheum.2012;64(6):2028–37.
2.D’EliaC[Dissertac¸ãodemestrado]Comparac¸ãoentreo
usodoplasmaricoemplaquetasassociadocom
aspiradodemedularósseaaoenxertoautólogode
ilíaconaconsolidac¸ãodasosteotomiasdatíbia
proximal:estudoprospectivorandomizado.SãoPaulo:
FaculdadedeMedicinadeUniversidadedeSãoPaulo,
DepartamentodeOrtopediaeTraumatologia;2009.
3.AhlmannE,PatzakisM,RoidisN,ShepherdL,HoltomP.
Comparisonofanteriorandposterioriliaccrestbone graftsintermsofharvest-sitemorbidityandfunctional outcomes.JBoneJointSurgAm.2002;84(5):716–20.
4.MoonMS.Developmentinthemanagementof
tuberculosisofthespine.CurrOrthop.2006;20: 132–40.
5.HearyRF,MadhavanK.Thehistoryofspinaldeformity. Neurosurgery.2008;633Suppl.:5–15.
6.YoungPM,BerquistTH,BancroftLW,PetersonJJ.
Complicationsofspinalinstrumentation.
Radiographics.2007;27(3):775–89.
7.HuSS,PashmanRS.Spinalinstrumentation.Evolution
andstateoftheart.InvestRadiol.1992;27(8):632–47.
8.KabinsMB,WeinsteinJN.Thehistoryofvertebralscrew andpediclescrewfixation.IowaOrthopJ.
1991;11:127–36.
9.EtminanM,GirardiFP,KhanSN,CammisaFPJr.
Revisionstrategiesforlumbarpseudarthrosis.Orthop ClinNorthAm.2002;33(2):381–92.
10.ParkJJ,HershmanSH,KimYH.Updatesintheuseof
bonegraftsinthelumbarspine.BullHospJtDis. 2013;71(1):39–48.
11.VendraminFS,FrancoD,NogueiraCM,PereiraMS,
FrancoTR.Plasmaricoemplaquetasefatoresde
crescimento:técnicadepreparoeutilizac¸ãoemcirurgia plástica.RevColBrasCir.2006;33(1):24–8.
12.RodriguesDG,CoelhoJA,OliveiraCEA,SontoroAG,
TrindadeRMC,PereiraSAC.Análiseda
reprodutibilidadeintraeinter-observadoresdas classificac¸õesradiográficasparaavaliac¸ãodaartrodese
dacolunalombar.Coluna/Columna.2008;7(3):257–61.
13.DelgadoR,BonatelliAPF,AlvesMTS.Studyaboutfusion usingceramicwithplatelet-richplasmainthespineof rats.ActaOrtopBras.2009;17(5):282–5.
14.KimH,LeeCK,YeomJS,LeeJH,LeeKH,ChangBS.The
efficacyofporoushydroxyapatitebonechipasan extenderoflocalbonegraftinposteriorlumbar interbodyfusion.EurSpineJ.2012;21(7):1324–30.
15.PagliosaGM,AlvesGES.Considerac¸õessobrea
obtenc¸ãoeousodoplasmaricoemplaquetasedas
célulasmesenquimaisindiferenciadasemenxertos
ósseos.CiêncRural.2007;37(4):1202–5.
16.KonE,FilardoG,DiMartinoA,MarcacciM.Platelet-rich plasma(PRP)totreatsportsinjuries:evidenceto supportitsuse.KneeSurgSportsTraumatolArthrosc. 2011;19(4):516–27.
17.LenzaM,FerrazSB,ViolaDC,SantosOF,Cendoroglo NetoM,FerrettiM.Platelet-richplasmaforlongbone healing.Einstein(SaoPaulo).2013;11(1):122–7.
18.MarxRE,CarlsonER,EichstaedtRM,SchimmeleSR,
factorenhancementforbonegrafts.OralSurgOralMed OralPatholOralRadiolEndod.1998;85(6):638–46.
19. BrandãoCMA,CamargosBM,ZerbiniCA,PlaplerPG,
Mendonc¸aLMC,AlbergariaBH,etal.Posic¸õesoficiais 2008daSociedadeBrasileiradeDensitometriaClínica. ArqBrasEndocrinolMetab.2009;53(1):107–12.
20.RoffiA,FilardoG,KonE,MarcacciM.DoesPRPenhance boneintegrationwithgrafts,graftsubstitutes,or
implants?Asystematicreview.BMCMusculoskelet