www.jped.com.br
REVIEW
ARTICLE
Is
this
child
sick?
Usefulness
of
the
Pediatric
Assessment
Triangle
in
emergency
settings
夽
Ana
Fernandez
∗,
Javier
Benito,
Santiago
Mintegi
HospitalUniversitarioCruces,ServiciodeUrgenciasdePediatría,Barakaldo,Spain
Received25May2017;accepted5July2017 Availableonline25August2017
KEYWORDS
PediatricAssessment Triangle;
Pediatricassessment; Pediatricemergency department
Abstract
Objective: ThePediatricAssessmentTriangleisarapidassessmenttoolthatusesonlyvisual
andauditoryclues,requiresnoequipment,andtakes30---60stoperform.It’sbeingused
inter-nationallyindifferentemergencysettings,butfewstudieshaveassesseditsperformance.The
aimofthisnarrativebiomedicalreviewistosummarizetheliteratureavailableregardingthe
usefulnessofthePediatricAssessmentTriangleinclinicalpractice.
Sources: The authors carried out a non-systematic review inthe PubMed®, MEDLINE®,and
EMBASE® databases,searchingfor articlespublishedbetween1999---2016usingthekeywords
‘‘pediatric assessment triangle,’’ ‘‘pediatric triage,’’ ‘‘pediatric assessment tools,’’ and
‘‘pediatricemergencydepartment.’’
Summaryofthefindings: ThePediatricAssessmentTrianglehasdemonstrateditselftobe
use-fultoassesssickchildrenintheprehospitalsettingandmaketransportdecisions.Ithasbeen
incorporated,asanessentialinstrumentforassessingsickchildren,intodifferentlifesupport
courses,althoughlittlehasbeenwrittenabouttheeffectivenessofteachingit.Littlehasbeen
publishedabouttheperformanceofthistoolintheinitialevaluationintheemergency
depart-ment.Intheemergencydepartment,thePediatricAssessmentTriangleisusefultoidentifythe
childrenattriagewhorequiremoreurgentcare.Recentstudieshaveassessedandprovedits
efficacytoalsoidentifythosepatientshavingmoreserioushealthconditionswhoareeventually
admittedtothehospital.
Conclusions: ThePediatricAssessmentTriangleisquicklyspreadinginternationallyandits
clini-calapplicabilityisverypromising.Nevertheless,itisimperativetopromoteresearchforclinical
validation,especiallyforclinicalusebyemergencypediatriciansandphysicians.
©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen
accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/
4.0/).
夽
Pleasecitethisarticleas:FernandezA,BenitoJ,MintegiS.Isthischildsick?UsefulnessofthePediatricAssessmentTriangleinemergency settings.JPediatr(RioJ).2017;93:60---7.
∗Correspondingauthor.
E-mail:ana.fernandezlandaluce@osakidetza.eus(A.Fernandez).
http://dx.doi.org/10.1016/j.jped.2017.07.002
0021-7557/©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-ND
PALAVRAS-CHAVE
Triângulode
Avaliac¸ãoPediátrica; Avaliac¸ãopediátrica; Departamentode emergência pediátrica
Estacrianc¸aestádoente?UtilidadedoTriângulodeAvaliac¸ãoPediátrica nasconfigurac¸õesdeemergência
Resumo
Objetivo: OTriângulodeAvaliac¸ãoPediátricaéumaferramentadeavaliac¸ãorápidaqueutiliza
apenaspistasvisuaiseauditivas,nãonecessitadeequipamentoselevade30-60segundospara
realizac¸ão.Eletemsidoutilizadointernacionalmenteemdiferentesconfigurac¸õesde
emergên-cia, porém poucos estudos avaliaramseu desempenho. Oobjetivo dessaanálise biomédica
narrativaéresumiraliteraturadisponívelcomrelac¸ãoàutilidadedoTriângulodeAvaliac¸ão
Pediátricanapráticaclínica.
Fontes: RealizamosumaanálisenãosistemáticanasbasesdedadosdoPubMed®,MEDLINE®e
EMBASE®buscandoartigospublicadosentre1999-2016utilizandoaspalavras-chave‘‘triângulo
deavaliac¸ãopediátrica’’,‘‘triângulopediátrico’’, ‘‘ferramentasde avaliac¸ãopediátrica’’e
‘‘departamentodeemergênciapediátrica’’.
Resumodosachados: OTriângulodeAvaliac¸ãoPediátricademonstrouserútilnaavaliac¸ãode
crianc¸asdoentesnaconfigurac¸ãopré-hospitalar enatomadadedecisõesdetransporte.Ele
foiincorporado,como uminstrumentoessencialnaavaliac¸ãodecrianc¸asdoentes,em
difer-entescursosdesuportedevida,apesardepoucotersidoescritosobreaeficáciadeensino
doTriângulodeAvaliac¸ãoPediátrica.PoucofoipublicadosobreodesempenhodoTriângulode
Avaliac¸ãoPediátricanaavaliac¸ãoinicialnodepartamentodeemergência(DE).NoDE,o
Triân-gulodeAvaliac¸ãoPediátricaéútilparaidentificar,natriagem,crianc¸asqueexigemcuidadomais
urgente.EstudosrecentesavaliarameprovaramaeficáciadoTriângulodeAvaliac¸ãoPediátrica
tambémnaidentificac¸ãodospacientescomdoenc¸asdesaúdemaisgravese,eventualmente,
sãointernadosnohospital.
Conclusões: O Triângulo de Avaliac¸ão Pediátrica está se difundindo rapidamente de forma
internacionalesuaaplicabilidadeclínicaémuitopromissora.Contudo,éessencialpromover
pesquisaparavalidac¸ãoclínica,principalmenteparaousoclínicoporpediatrasemédicosde
emergência.
©2017SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo
OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4.
0/).
Introduction
Isthischildsick?ShouldIbeginanyemergencyintervention? Anyprovidershouldbeabletoanswerquicklythese ques-tionswhenevertheprovidercomesinfrontofachildseeking forurgent medicalattention (intheprehospitalsettingor emergencydepartment[ED]).
Everyday,thousandsofchildrenarebroughttodifferent emergencysettingsworldwide.Childrenaccountforabout one-fourthofthevisitstohospitalEDsintheUnitedStates, andaround30millionchildrenareassessedbygeneral prac-titionersorpediatriciansannually.1Infantsyoungerthan12
monthsaretheagegroupwiththehighestpercapitarate ofvisitstotheED(91.3per100infantsin2005).Inthe pre-hospitalsetting,10%to13%ofambulancetransportsarefor children.2InEurope,intheUK,25---30%ofallAccidentand
Emergencyattendancesarechildren.3
Inpediatricemergencymedicine,stabilizingthepatient mustbeperformedbeforeestablishingadiagnosis;a prob-lemsolvingapproachisrequired.Itis,therefore,essential tohaveatoolthatallowsarapidinitialassessmentand iden-tifiestheproblemthatmustbesolved.Unfortunately,initial assessmentofacriticallyillorinjuredchildisoftendifficult, even for the experienced clinician. Physical examination and vital signs assessment, the cornerstone of the adult assessment,maybecompromisedwithahands-on evalua-tion.Initialassessmentofthechildpresentingtoemergency shouldideallybeviaan‘‘acrosstheroom’’assessment.4
The
Pediatric
Assessment
Triangle:
definition
In2000,theAmericanAcademyofPediatrics(AAP)published thefirstnationalpediatriceducationalprogramfor prehos-pitalproviders,which introduced a newrapid assessment tool, called the Pediatric Assessment Triangle (PAT). The PATisnotadiagnostictool,itwasdesignedtoenablethe providertoarticulateformallyageneralimpressionofthe child,establishtheseverityofthepresentationandcategory of pathophysiology, and determine the type and urgency ofintervention.5The PATsomehowsummarizes‘‘gut
feel-ing’’ findings, and promotes consistent communication amongmedicalprofessionalsaboutthechild’sphysiological status.
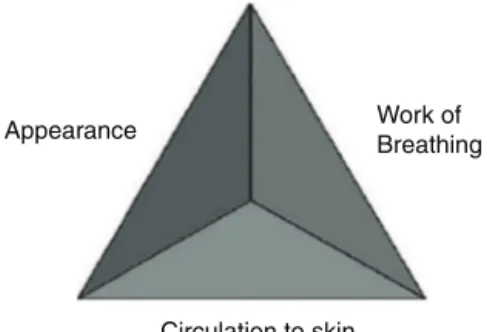
Intended for use in rapid assessment, the PAT uses onlyvisualandauditoryclues,requiresnoequipment,and takes 30---60s to perform. The three components of the PAT are appearance, work of breathing, and circulation tothe skin (Fig.1). Each component of the PAT is evalu-atedseparately, usingspecificpredefinedphysical, visual, or auditory findings. If the clinician detects an abnor-malfinding,thecorrespondingcomponentis,bydefinition, abnormal.Together,thethreecomponentsofthePATreflect the child’s overall physiologic status, or the child’s gen-eralstateofoxygenation,ventilation,perfusion,andbrain function.2
Appearance Work of Breathing
Circulation to skin
Figure1 PediatricAssessmentTriangle.
fortreatment,andtheresponsetotherapy.Itreflectsthe adequacyofventilation,oxygenation,brainperfusion,body homeostasis,andcentralnervoussystemfunction.Thisarm ofthePATis delineatedby the‘‘TICLS’’mnemonic:Tone, Interactiveness,Consolability,LookorGaze,andSpeechor Cry.Importantclues suchastheinfant’s tone, consolabil-ity,interactionwithcaregiversandothers,andstrengthof crycaninformtheproviderofthechild’sappearanceas nor-malorabnormal(forageanddevelopment).Theinteraction withtheenvironmentandexpectednormalbehaviorvaries accordingtotheageof thepatient.Knowledgeofnormal developmentinchildhoodisessentialfortheassessmentof theappearance.
The other elements of the PAT provide more specific informationaboutthetypeofphysiologicderangement.
Workof breathingdescribesthechild’srespiratory sta-tus,especiallythedegreetowhichthechildmustworkin ordertooxygenateandventilate.Assessingworkof breath-ingrequireslisteningcarefullyforaudibleabnormalairway sounds(e.g.,stridor,grunting,andwheezing),andlooking forsignsofincreasedbreathingeffort(abnormal position-ing,retractions,orflaringofthenostrilsoninspiration).The typeofabnormalairwaynoiseprovidesinformationabout the location of the disease, while the number and loca-tionof retractions and the position of the patientreport theintensityofrespiratorywork.
Circulationtotheskin reflectsthegeneralperfusionof blood throughout the body. The provider notes the color andcolor pattern of the skin and mucous membranes. In the context of blood loss/fluid loss or changes in venous tone,compensatorymechanismsshuntbloodtovitalorgans suchasthe heart and brain,and awayfrom theskin and theperipheryofthebody. Bynotingchangesinskin color andskin perfusion (suchas pallor, cyanosis,or mottling), theprovidermayrecognizeearlysignsofshock.
An abnormality noted in any of the arms of the PAT denotesanunstablechild;i.e.,achildwhowillrequiresome immediate clinical intervention. The pattern of affected armswithinthePATfurthercategorizesthechildinto1of 5categories:respiratorydistress,respiratoryfailure,shock, centralnervoussystemormetabolicdisorder,and cardiopul-monaryfailure.Thespecificcategorythendictatesthetype andurgencyofintervention.2,6
In 2005, an Emergency Medical Services for Children (EMSC) task force was convened to review definitions andassessmentapproachesfornational-levelpediatriclife support programs and courses. Representatives from the AAP, the American College of Emergency Physicians, the
AmericanHeartAssociationEmergencyNurses Association, the National Association of EMTs, the Children’s National MedicalCenter,andtheNewYorkCenterforPediatric Emer-gency Medicine met to adopt consensus definitions and approaches to pediatric emergency care. The group con-cluded thata standard algorithmfor pediatric emergency assessmentshouldstartwiththePAT.5
Sinceits creation as a rapid assessment tool, the PAT hasbeentaughttoandusedinternationallybyhealth pro-fessionalsinvariousdifferentsettings,althoughtherehave beenveryfewvalidationstudies.
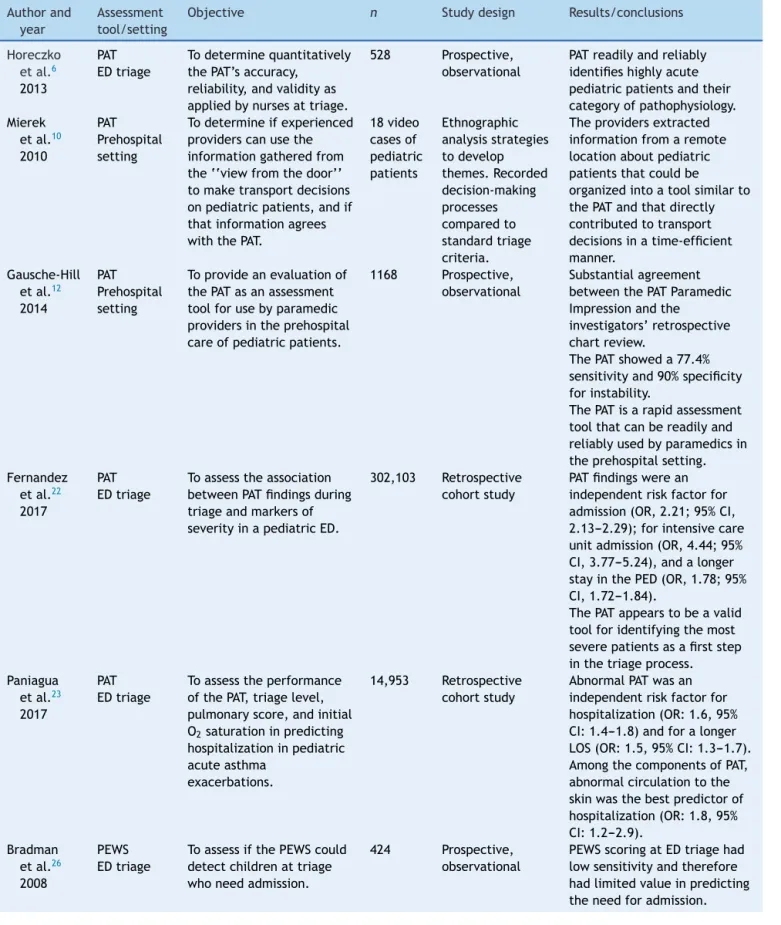
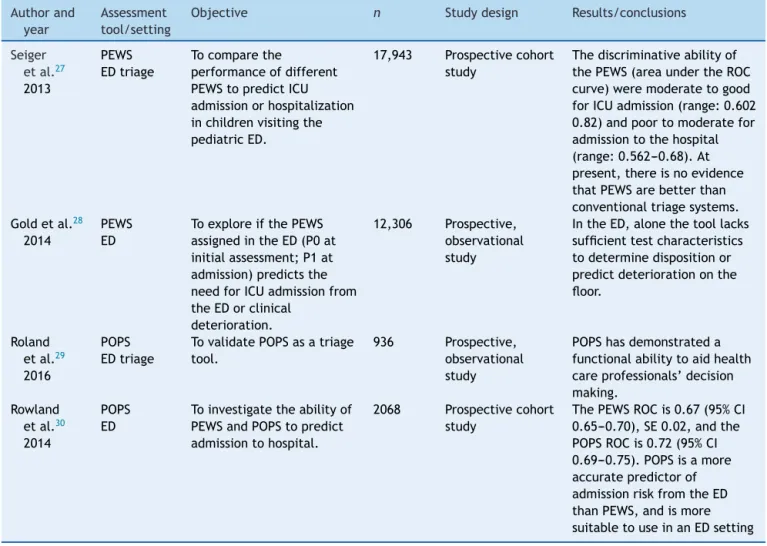
This non-systematicreview aims toupdate the profes-sionals involved in thecare of children in EDsin relation totheliteratureavailableregardingtheclinicaluseofthe PAT.Itwascarriedoutusingthekeywords‘‘pediatric assess-menttriangle,’’‘‘pediatrictriage,’’‘‘pediatricassessment tools,’’ and ‘‘pediatric emergency department’’ in the PubMed®,MEDLINE®,andEMBASE® databases,searchingfor articlespublishedbetween1999---2016(Table1).
PAT
as
a
teaching
tool
The tool has been incorporated, as an essential instru-mentforassessingsickchildren,intodifferentlifesupport courses, including the Advanced Pediatric Life Support (APLS), Emergency Nursing Pediatric Course, Pediatric Advanced Life Support (PALS), Pediatric Education for Prehospital Professionals (PEPP), Special Children’s Out-reachandPrehospitalEducation,andTeachingResourcefor InstructorsinPrehospitalPediatrics.5
TheAPLScourseaimstoimprovetheearlymanagement ofacutelyillandinjuredchildrenthroughtrainingand edu-cationofhealthcareprofessionals.Itisavaluableresource forpediatricresidentsanditispartoftheprogramof con-tinuingeducationofpediatriciansandemergencyphysicians intheUnitedStates.7
The first APLScourse was implemented in 1984 in the UnitedStates.The firsteditionoftheAPLScoursestudent manualwaspublishedbytheAAPandACEPin1989.All edi-tionswereguidedbytheAPLSJointTaskForce,andallwere builtonthefoundation laidby Dr.Brushore-Fallisandher colleagues.8
Table1 Pediatricassessmenttools.
Authorand
year
Assessment tool/setting
Objective n Studydesign Results/conclusions
Horeczko
etal.6
2013
PAT EDtriage
Todeterminequantitatively thePAT’saccuracy,
reliability,andvalidityas appliedbynursesattriage.
528 Prospective, observational
PATreadilyandreliably identifieshighlyacute pediatricpatientsandtheir categoryofpathophysiology. Mierek
etal.10
2010
PAT Prehospital setting
Todetermineifexperienced providerscanusethe informationgatheredfrom the‘‘viewfromthedoor’’ tomaketransportdecisions onpediatricpatients,andif thatinformationagrees withthePAT.
18video casesof pediatric patients
Ethnographic analysisstrategies todevelop themes.Recorded decision-making processes comparedto standardtriage criteria.
Theprovidersextracted informationfromaremote locationaboutpediatric patientsthatcouldbe organizedintoatoolsimilarto thePATandthatdirectly contributedtotransport decisionsinatime-efficient manner.
Gausche-Hill etal.12
2014
PAT Prehospital setting
Toprovideanevaluationof thePATasanassessment toolforusebyparamedic providersintheprehospital careofpediatricpatients.
1168 Prospective, observational
Substantialagreement betweenthePATParamedic Impressionandthe investigators’retrospective chartreview.
ThePATshoweda77.4% sensitivityand90%specificity forinstability.
ThePATisarapidassessment toolthatcanbereadilyand reliablyusedbyparamedicsin theprehospitalsetting. Fernandez
etal.22
2017
PAT EDtriage
Toassesstheassociation betweenPATfindingsduring triageandmarkersof severityinapediatricED.
302,103 Retrospective cohortstudy
PATfindingswerean independentriskfactorfor admission(OR,2.21;95%CI, 2.13---2.29);forintensivecare unitadmission(OR,4.44;95% CI,3.77---5.24),andalonger stayinthePED(OR,1.78;95% CI,1.72---1.84).
ThePATappearstobeavalid toolforidentifyingthemost severepatientsasafirststep inthetriageprocess. Paniagua
etal.23
2017
PAT EDtriage
Toassesstheperformance ofthePAT,triagelevel, pulmonaryscore,andinitial O2saturationinpredicting
hospitalizationinpediatric acuteasthma
exacerbations.
14,953 Retrospective cohortstudy
AbnormalPATwasan independentriskfactorfor hospitalization(OR:1.6,95% CI:1.4---1.8)andforalonger LOS(OR:1.5,95%CI:1.3---1.7). AmongthecomponentsofPAT, abnormalcirculationtothe skinwasthebestpredictorof hospitalization(OR:1.8,95% CI:1.2---2.9).
Bradman etal.26
2008
PEWS EDtriage
ToassessifthePEWScould detectchildrenattriage whoneedadmission.
424 Prospective, observational
Table1(Continued)
Authorand
year
Assessment tool/setting
Objective n Studydesign Results/conclusions
Seiger
etal.27
2013
PEWS EDtriage
Tocomparethe
performanceofdifferent PEWStopredictICU admissionorhospitalization inchildrenvisitingthe pediatricED.
17,943 Prospectivecohort study
Thediscriminativeabilityof thePEWS(areaundertheROC curve)weremoderatetogood forICUadmission(range:0.602 0.82)andpoortomoderatefor admissiontothehospital (range:0.562---0.68).At present,thereisnoevidence thatPEWSarebetterthan conventionaltriagesystems. Goldetal.28
2014
PEWS ED
ToexploreifthePEWS assignedintheED(P0at initialassessment;P1at admission)predictsthe needforICUadmissionfrom theEDorclinical
deterioration.
12,306 Prospective, observational study
IntheED,alonethetoollacks sufficienttestcharacteristics todeterminedispositionor predictdeteriorationonthe floor.
Roland etal.29
2016
POPS EDtriage
TovalidatePOPSasatriage tool.
936 Prospective, observational study
POPShasdemonstrateda functionalabilitytoaidhealth careprofessionals’decision making.
Rowland etal.30
2014
POPS ED
Toinvestigatetheabilityof PEWSandPOPStopredict admissiontohospital.
2068 Prospectivecohort study
ThePEWSROCis0.67(95%CI 0.65---0.70),SE0.02,andthe POPSROCis0.72(95%CI 0.69---0.75).POPSisamore accuratepredictorof admissionriskfromtheED thanPEWS,andismore suitabletouseinanEDsetting
PAT,PediatricAssessmentTriangle;PEWS,PediatricEarlyWarningScore;POPS,PediatricObservationPriorityScore;ED,emergency department.
Inaddition, morethan 80% of respondents indicated that theyalwaysusethePATapproachintheirclinicalpractice. AlmostallrespondentsbelievedthattheAPLScourseshould beincludedinthepediatricresidency-trainingprogramand thatitshouldbearequirement.9
PAT
in
the
prehospital
setting
ThePATwasinitiallydesignedtobeusedintheprehospital setting.Thus,firstattemptstovalidatethetoolwerecarried outinthissetting.In2010,Miereketal.publishedastudyin which12EMSproviderswererecruitedtoobservetwovideos ofpediatricpatientsandmakeatransportdecisionbasedon theirobservations. Aftereachcase, theparticipantswere interviewed to determine why they made their decision. Interviewswere thentranscribed and analyzedseparately bythreeresearchers.Theyconcludedthatproviderscould extract information from a remote location about pedi-atric patients that could be organized into a tool similar to the PAT. This remotely-obtained information directly contributedtotransportdecisionsandsupported thatthe toolwasatime-efficientmethodoftriagingpatients.They
statedthatthePAT couldbetaughtwithmoreconfidence andgreateremphasis,andultimately,appliedmorebroadly toprehospitalmedicine.10
In2011,Horeczkoetal.publishedanarticlepresenting thePATtoprehospitalprovidersasatoolfortherecognition andtreatmentoftheacutelyillorinjuredchild.11
When categorized as stable vs. unstable agreement betweenthePATParamedicImpressionandPATInvestigator Impression,agreementwasalso‘‘substantial’’(=0.66,95% CI:0.62---0.71).ThePATParamedicImpressionforinstability demonstrateda sensitivityof 77.4% (95%CI:72.6---81.5%), aspecificityof90.0%(95%CI:87.1---91.5%),withapositive likelihoodratio(LR+)of7.7(95%CI:5.9---9.1)andanegative likelihoodratio(LR-)of0.3(95%CI:0.2---0.3).The authors concludedthatparamedicsconstructedandappliedthePAT reliably,accuratelypredicting theinstabilityandstability. Further,thePATasusedbyparamedicswasconsistentwith theperformanceofappropriateprehospitalinterventions.12
PAT
and
triage
The aim of triage is to identify patients who are more urgent. Urgency incorporates concepts of risk of deterio-rationandtimelinessinmedicalassessmentandtreatment. Becauseurgencymaydifferbetweenpatientswiththesame diagnosis,triageshouldfocusonthepatient’sconditionat presentation insteadofthe diagnosis. Toidentifypatients withsuchacuteconditions,easyandquickassessmenttools mustbeincorporatedintriagesystems.13
Currently,themostcommonlyusedstructuredtriage sys-tems begin the patient’s classification by an assessment of this general impression regardless of the presenting problem.14---16 Systems such as the Manchester triage
sys-temwidelyusedinEuropeanEDswhichdonotincludethis initialassessment, haveshowntobelessaccuratefor the classificationofthepediatricpatient.17---21
Toassessthisgeneralimpression,knowledgeand experi-encearenecessarybutnotsufficient.Theotherfactorfound tobeimportantisgutinstinctorthesixthsense.15 Aswas
said before, the PAT somehow summarizes ‘‘gut feeling’’ findings,andthismakesittheidealacademictooltoteach thisinitialassessment.
The PAT also appears to be a potentially idealtool to guidetriagedecisionsbecauseitcanbeappliedeasilyand quickly, stratifyingstable andunstable patientsto differ-entcare pathways. The pediatric versionof theCanadian TriageandAcuityScale(PaedCTAs)usesthePATastheinitial assessmenttool.16
Horeczko etal. demonstratedfor the firsttime that a structuredassessment basedonPAT, performed bynurses during patienttriage, rapidlyand reliablyidentifies clini-callyurgentpediatricpatientsandtheirpathophysiological status. They conducted aprospective observational study wheretriagenursesperformedthePATonallpatients pre-senting tothe pediatricED of anurban teachinghospital. Researchersperformedblindedchartreviewusingthe physi-cian’sinitialassessmentandfinaldiagnosisasthecriterion standard for comparison. In their study, the PAT accu-ratelyand reliablyidentifiedacutely illor injuredinfants andchildren intriage, asevidenced bya lownegativeLR for instability. Furthermore, the PAT reliably categorized unstablechildrenbypathophysiology,asevidencedbyhigh positiveLRsfordisease,thusaidinginidentifyingpriorities ofmanagement.6
Inaddition,thePATalsohelpstoidentifythosepatients who, after complete diagnosis and treatment in the ED, have more serious health conditions and are eventually
admittedtothehospital.Inalargesingle-center retrospec-tivestudyincludingaround300,000episodesclassifiedusing thePaedCTAS,Fernandezetal.analyzedthepercentageof children hospitalizedrelated tothe PAT findings made by nursesatthetimeoftriage.As secondaryoutcomes,they alsoanalyzed thepercentage of patientsadmitted tothe pediatricintensivecareunit(PICU),thelengthofstay(LOS) inthepediatric ED(<3hand≥3h),andthepercentageof patientsinwhichbloodtestswereobtainedinrelationtoPAT findingsattriage.ThepresenceofabnormalPATfindingsat triagewasassociatedwithahigherprobabilityof hospital-ization(oddsratio[OR],5.14;95%CI,4.97---5.32)especially inthe case of appearance (OR, 7.87; 95% CI,7.18---8.62). In the multivariate analysis, abnormal PAT findings were confirmedtobeindependentriskfactorsforhospitalization. Regardingsecondaryoutcomemeasures,abnormalPAT find-ings,mainlyappearance,andcombinationsofmorethanone componentof thePAT wereassociatedwithlongerLOS in thepediatricED,andhigherprobabilityofadmissiontothe PICU(ORforabnormalPAT12.75;95%CI,10.86---14.97).22
Morerecently,thesamegroupassessedtheperformance ofthePAT along withthetriagelevel givenby PaedCTAS, a clinical score of asthma (pulmonary score), and oxy-gen saturation, as predictors of admission to a pediatric ED for children with asthma exacerbations. The presence of abnormal PAT findings was an independent risk factor for hospitalization (OR: 1.6, 95% CI: 1.4---1.8) and for a longer LOS (OR: 1.5, 95% CI: 1.3---1.7). Among the com-ponentsof PAT, abnormal circulation tothe skin was the bestpredictorofhospitalization(OR:1.8,95%CI:1.2---2.9), whereasincreasedwork of breathing wasassociated with longerLOS(OR:1.4,95%CI:1.3---1.6).Norelationship was foundbetweenabnormalPATfindingsandPICUadmission. TheauthorsconcludedthatthePATidentifiespatientswho requiremoreurgenttreatment,helpingtooptimizepatient flowwithinthepediatricED,andalsothosemorelikelytobe eventuallyadmittedorrequiringalongerstay.EDmanagers coulduse thisinformation in realtimeto make decisions regardingtheneedforadditionalresources.23
Other more complex initial assessment tools, such as the Pediatric Early Warning Score (PEWS) and the Paedi-atricObservationPriorityScore(POPS),havebeenassessed in the first stepof the triageprocess. These tools incor-poratemeasurementofvitalsigns.Traditionally,vitalsigns wereconsideredanintegralcomponentoftheinitialnursing assessmentandwereoftenusedasadecisionmakingtool, butnewertriagemodelsadvocateselectiveuseof physio-logicalparametersat triage.Vitalsignmeasurementsmay beoperatordependent, andthedefinitionofnormalvital signsvaries according to the referenceconsulted. This is especiallytrueforinfancyandchildhood,periodsof enor-mousphysiologicalanddevelopmentalchange,particularly intheearlymonthsandyears.Thereisalackofconsensusin theliteratureregardingnormalpediatricvitalsign param-eters,and furthermore, most references for normal vital signsderive fromstudies of healthy children. Even under thebest conditions,vital signsare not always reliable or accurate.1,24,25
status.Thetoolwasdevelopedtodetectclinical deteriora-tioninchildrenadmittedtohospital,ultimatelytoprevent cardiopulmonaryarrest.Currently,severalPEWSarebeing usedin Europe,all ofthembasedonthemeasurementof physiologicalparameters,withlittledifferencebetweenthe scoringsystems.In2008Bradman&Maconochiestudiedthe use ofa PEWS-system asa triage tooltopredict hospital admission from the pediatric ED. They found that PEWS scoring in theED hada low sensitivity andtherefore had alimitedvalueinpredictingtheneedforadmission, proba-blybecausethephysiologicalparametersmeasuredcanbe raisedsecondarilytopain,pyrexia,andanxiety,allcommon presentationsinapediatricED.26
In 2013,Seiger etal. publisheda study comparingthe validityof differentPEWsin a pediatricED. Although the authorsfoundthatPEWScouldidentifypatientsatriskinthe EDforICUadmissionand,toalesserextent,couldidentify patientsatriskforhospitalization,theydidnotadviseusing warningscoresastriagetoolstoprioritizepatients,because atpresent,thereisnoevidencethatPEWSarebetterthan conventionaltriagesystems.27
In2014,Goldetal.exploredwhetherthePEWSutilized inanEDofanurban,tertiarycarechildren’shospital pre-dictedthe need forICU admission fromtheED or clinical deteriorationin admitted patients. Theirstudy confirmed that,actually,anelevatedPEWSisassociatedwithneedfor ICU admissiondirectly fromthe ED and asa transfer,but lacksthenecessarytestcharacteristicstobeused indepen-dentlyintheEDenvironment.Usingtheoptimalcutoffscore topredictdispositionfromtheEDwouldresultinatwo-to four-foldincreaseinintensivecareunitadmissionrate,as wellasincorrectlyplaceroughly25%ofICUpatientsonthe floor.The EDisadynamicenvironment,withpatients fre-quentlyhavingalterationsinphysiologicparametersdueto theacuityof illness or injury,medication,pain,fear,and anxiety.SuchfactorswouldresultinelevatedPEWSscores thatdonotreflectactualillness.28
ThePOPSincludes,inadditiontovitalsigns,subjective observation criteria, and has proven to be more suitable tousein anEDsetting thanPEWS.ThePOPSisabespoke assessmenttoolforuse inpediatricEDsincorporating tra-ditionalphysiologicalparametersalongsidemoresubjective observationalcriteria.Itisaphysiologicalandobservational scoringsystemdesignedforusebyhealth care profession-alsofvaryingclinicalexperience.POPShasdemonstrateda functionalabilitytoaidhealthcareprofessionals’decision makingandhasbeenshowntobeamoreaccuratepredictor ofadmissionriskfromtheEDthanPEWS.29,30
PAT
and
clinical
practice
Beyondthe clinical application of the PAT in triage, arti-clesonitsusefulnessinmedicalpracticewerenotfound.In theaforementionedstudypublishedbyBenitoetal.,most participants in the APLS courses acknowledged that they usedthe PAT approachin clinical practiceand morethan a half assured that their management of the critically-ill patientshadimprovedaftercoursecompletion.Inaddition, 82%statedthatthePATandABCDE(Airway,Breathing, Cir-culation,Disability, Exposure) approaches helped them in thediagnosisandindicationofthemostappropriateinitial
treatment.9Althoughthisstudydoesnotgiveevidenceon
thedirectimpactofthePATinclinicalpractice,theopinion ofproviderswhohave introducedthistoolinthe manage-mentoftheirpatientsappearstosupportitsusefulness.
Conclusions
The PAT has been incorporated, as an essential instru-mentforassessingsickchildren,intodifferentlifesupport courses,although littlehasbeen written aboutthe effec-tivenessofteachingit.
The PAT has demonstrated to be useful to assess sick children in the prehospital setting and tomake transport decisions.
IntheED,thePATisusefultoidentifychildrenattriage who require more urgent care, and recent studies have assessed and proved theefficacy of the PAT toalso iden-tify those patients having more serious health conditions whoareeventuallyadmittedtothehospital.Littlehasbeen published about performance of the PAT administered by pediatriciansor emergency physiciansin theinitial evalu-ationattheED.
The PAT is quickly spreading internationally and its clinical applicability is very promising. Nevertheless, it is imperativetopromoteresearchforclinicalvalidation.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.HohenhausS,TraversD,MechamN.Pediatrictriage:areviewof emergencyeducationliterature.JEmergNurs.2008;3:308---13. 2.DieckemannRA.Pediatricassessment.In:FuchsS,Yamamoto L,editors.Emergencymedicineresource.5thed.Burlington, MA:Jones&BarlettLearning;2012.p.2---37.
3.RoyalCollegeofPaediatricsandChildHealth.Availablefrom: http://www.rcpch.ac.uk/training-examinationsprofessional-development/postgraduate-training/sub-specialty-training/ paedia-3[cited01.04.17].
4.AlmondC.Issues inpaediatrictriage. AustralEmerg NursJ. 2000;3:12---4.
5.Dieckmann RA, Brownstein D, Gausche-Hill M. The pediatric assessmenttriangle:anovelapproachfortherapidevaluation ofchildren.PediatrEmergCare.2010;26:312---5.
6.HoreczkoT,EnriquezB,McGrathNE,Gausche-HillM,LewisRJ. ThePediatricAssessmentTriangle:accuracyofitsapplication bynurses in thetriage of children. JEmerg Nurs.2013;39: 182---9.
7.American Academy of Pediatrics, and American College of
EmergencyPhysicians.Continuingmedicaleducation.American
Academy of Pediatrics; 2017. Available from: http://www.
aap.org/en-us/continuing-medical-education/life-support/ Pages/Life-Support.aspx[cited30.03.17].
8.American Academy of Pediatrics, and American College
of Emergency Physicians. History of the APLS. Jones &
Bartlett Learning LL; 2012. Available from: http://www.
aplsonline.com/about/abouthome.aspx[cited30.03.17].
9.BenitoJ,Luaces-CubellsC,MintegiS,ManriqueMartínezI,De
laTorreEspíM,MiguezNavarroC,etal.Evaluationandimpact
ofpediatricemergenciesinSpain.PediatrEmergCare.2017,
http://dx.doi.org/10.1097/PEC.0000000000001038.
10.MierekC,NaccaN,ScottJM,WojcikSM,D’AgostinoJ,Dougher K,etal.Viewfromthedoor:makingpediatrictransport deci-sionsbasedonfirstimpressions.JEMS.2010;35:68---9,71,73, 75,77,79,81.
11.HoreczkoT,Gausche-HillM.Thepaediatricassessmenttriangle: apowerfultoolfortheprehospitalprovider.JParamedPract. 2011;3:20---5.
12.Gausche-Hill M,Eckstein M,Horeczko T, McGrathN, Kurobe A,Ullum L,et al.Paramedicsaccuratelyapplythepediatric assessmenttriangletodrivemanagement.PrehospEmergCare. 2014;18:520---30.
13.FitzGerald G, Jelinek GA, Scott D, Gerdtz MF. Emer-gency department triage revisited. Emerg Med J. 2010;27: 86---92.
14.Australian Government, Department of Health and Ageing.
Paediatrictriage. In: Emergency triageeducation kit:triage
workbook. Canberra: Commonwealth of Australia; 2009.
p. 63---71. Available from: https://acem.org.au/getmedia/
a2ee0153-51ac-4480-81e4-428fe2d2d2ca/Triage-Workbook.pdf.
aspx[cited01.04.17].
15.GilboyN,TanabeT,TraversD,RosenauA.Introductiontothe emergencyseverityindex.In:EmergencySeverityIndex(ESI): atriagetoolforemergencydepartmentcare,Version4. Imple-mentationHandbook2012ED.AHRQpublicationNo12-0014. Rockville, MD: Agency for HealthcareResearch and Quality; 2011.p.15---25.
16.Canadian Paediatric Triage and Acuity Scale.
Implementa-tion guidelines for emergency departments. Available from:
http://www.cjem-online.ca/v3/n4/PaedCTAS[cited25.03.17]. 17.vanVeenM,SteyerbergEW,RuigeM,vanMeursAH,Roukema J, vander Lei J, et al. Manchester triage system in paedi-atricemergency care:prospective observational study.BMJ. 2008;337:a1501.
18.vanVeenM, SteyerbergEW, Van’t KloosterM, RuigeM, van MeursA, vanderLeiJ,etal.TheManchestertriagesystem: improvementsfor paediatricemergency care.Emerg MedJ. 2012;29:654---9.
19.SeigerN,vanVeenM,AlmeidaH,SteyerbergEW,vanMeursAH, CarneiroR,etal.ImprovingtheManchestertriagesystemfor pediatricemergencycare:aninternationalmulticenterstudy. PLOSONE.2014;9:e83267.
20.SeigerN,vanVeenM,SteyerbergEW,RuigeM,vanMeursAH, MollHA.UndertriageintheManchestertriagesystem:an assess-mentofseverityandoptionsforimprovement.ArchDisChild. 2011;96:653---7.
21.van Ierland Y, Seiger N, van Veen M, Moll HA, Oostenbrink R. Alarmingsignsinthe Manchestertriagesystem:a toolto identifyfebrile childrenat riskof hospitalization. JPediatr. 2013;162:862---6.
22.FernandezA,AresMI,GarcíaS,Martínez-IndartL,MintegiS, BenitoJ.ThevalidityofthePediatricAssessmentTriangleas thefirst stepinthetriageprocessin apediatric emergency department.PediatrEmergCare.2017;33:234---8.
23.PaniaguaN,ElosegiA,DuoI,FernandezA,MojicaE, Martinez-Indart L, et al. Initial asthma severity assessment tools as predictors of hospitalization. J Emerg Med. 2017. pii:S0736-4679(17)30233-0.
24.GilboyN,TanabeT,TraversD,RosenauA.Theroleofvitalsigns inESItriage.In:EmergencySeverityIndex(ESI):atriagetoolfor emergencydepartmentcare,Version4.Implementation hand-book2012 ED. AHRQ publicationNo 12-0014. Rockville, MD: AgencyforHealthcareResearchandQuality;2011.p.41---7.
25.SmythRL.Lessonsfromnormalheartandrespiratoryratesin children.Lancet.2011;37:974---5.
26.BradmanK,MaconochieI.Canpaediatricearlywarningscore beusedasatriagetoolinpaediatricaccidentandemergency? EJEM.2008;15:359---60.
27.Seiger N, Maconochie I, Oostenbrink R. Validityof different pediatricearlywarningscoresintheemergency department. Pediatrics.2013;132:e841---50.
28.Gold DL, Mihalov LK, Cohen DM. Evaluating the Pediatric Early Warning Score (PEWS) system for admitted patients in the pediatric emergency department. Acad Emerg Med. 2014;21:1249---56.
29.RolandD,LewisG,FieldingP,HakimC,WattsA,DaviesF.The paediatricobservationpriorityscore:asystemtoaiddetection ofseriousillnessandassistinsafedischarge.OpenJEmergMed. 2016;4:38---44.