www.jped.com.br
REVIEW
ARTICLE
Magnesium
sulfate
infusion
for
acute
asthma
in
the
emergency
department
夽
Jose
Enrique
Irazuzta
a,b,∗,
Nicolas
Chiriboga
a,baWolfsonChildren’sHospital,Jacksonville,UnitedStates
bUniversityofFlorida,Jacksonville,UnitedStates
Received2May2017;accepted26May2017 Availableonline26July2017
KEYWORDS
Magnesiumsulfate; Highdoseinfusion; Severeasthma; Pediatric; Emergency department; Cost-effective
Abstract
Objectives: Todescribetheroleofintravenousmagnesiumsulfate(MgSO4)astherapyforacute
severeasthmainthepediatricemergencydepartment(ED).
Source: PublicationsweresearchedinthePubMedandCochranedatabasesusingthefollowing
keywords:magnesiumANDasthmaANDchildrenANDclinicaltrial.Atotalof53publications were retrieved using thiscriteria.References ofrelevant articles were also screened.The authorsincludedthesummaryofrelevantpublicationswhereintravenousmagnesiumsulfate wasstudiedinchildren(age<18years)withacuteasthma.TheNAEPPandGlobalInitiativefor Asthmaexpertpanelguidelineswerealsoreviewed.
Summaryofthedata: ThereisalargevariabilityintheEDpracticesontheintravenous
admin-istrationofMgSO4forsevereasthma.ThepharmacokineticsofMgSO4isoftennottakeninto
accountwithaconsequentimpact initspharmacodynamicsproperties. Thecumulative evi-dencepointstotheeffectivenessofintravenousMgSO4inpreventinghospitalization,ifutilized
inatimelymannerandatanappropriatedosage(50---75mg/kg).Foreveryfivechildrentreated intheED, onehospitaladmissioncouldbeprevented.Anotheradministrationmodalityisa high-dose continuous magnesiumsulfateinfusion(HDMI)as 50mg/kg/h/4h (200mg/kg/4h). TheearlyutilizationofHDMIfornon-infectiousmediatedasthmamaybesuperiortoaMgSO4
bolusinavoidingadmissionsandexpeditingdischargesfromtheED.HDMIappearstobe cost-effectiveifappliedearlytoaselectedpopulation.IntravenousMgSO4hasasimilarsafetyprofile
thanotherasthmatherapies.
Conclusions: TreatmentwithintravenousMgSO4reducestheoddsofhospitaladmissions.The
use ofintravenous MgSO4 in the emergency room was not associated with significant side
夽
Pleasecitethisarticleas:IrazuztaJE,ChiribogaN.Magnesiumsulfateinfusionforacuteasthmaintheemergencydepartment.JPediatr (RioJ).2017;93:19---25.
∗Correspondingauthor.
E-mail:Jose.Irazuzta@jax.ufl.edu(J.E.Irazuzta). http://dx.doi.org/10.1016/j.jped.2017.06.002
effectsor harm.The authors emphasizetherole ofMgSO4as anadjunctive therapy,while
corticosteroidsandbetaagonistremaintheprimaryacutetherapeuticagents.
©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 4.0/).
PALAVRAS-CHAVE
Sulfatodemagnésio; Altadosedeinfusão; Asmagrave;
Pediátrico; Servic¸ode emergência; Custo-benefício
Infusãodesulfatodemagnésioparaasmaagudanoservic¸odeemergência
Resumo
Objetivos: Descreveropapeldosulfatodemagnésiointravenoso(MgSO4)comoterapiapara
asmagraveagudanoservic¸odeemergênciapediátrica(SE).
Fonte: Aspublicac¸ões forampesquisadas nobanco dedadosPubMed eCochrane utilizando
asseguintespalavras-chave:magnésioEasmaEcrianc¸asEensaioclínico.Foiencontradoum totalde53publicac¸õesutilizandoessescritérios.Asreferênciasdeartigosrelevantestambém foramexaminadas.Incluímosoresumodepublicac¸õesrelevantesquandoosulfatodemagnésio intravenosofoiestudadoemcrianc¸as(idade<18anos)comasmaaguda.Revisamostambémas diretrizesdoProgramaNacionalparaaEducac¸ãoePrevenc¸ãodaAsma(NAEPP)edopainelde especialistasdaIniciativaGlobalparaAsma.
Resumodosdados: Háuma grande variabilidadenaspráticas do SEna administrac¸ão
intra-venosado MgSO4 para asma grave.A farmacocinética doMgSO4 normalmentenão leva em
contaumimpactoposterior emsuaspropriedadesfarmacodinâmicas.Acomprovac¸ão cumu-lativaapontaparaaeficáciadoMgSO4intravenosonaprevenc¸ãodainternac¸ão,seutilizado
quandonecessário e em uma dosagemadequada (50-75mg/kg). Uma internac¸ãohospitalar podeserevitadaparacadacincocrianc¸astratadasnoSE.Outramodalidadedeadministrac¸ão éainfusãoprolongadadealtadosedesulfatodemagnésio(HDMI)a50mg/kg/hora/4horas (200mg/kg/4horas).OusoprecocedaHDMI,paraasmanãoinfecciosamediada,podeser supe-rioraumMgSO4embolusparaevitarinternac¸õeseanteciparasaltasdoSE.AHDMIparece
terbomcusto-benefícioseaplicadaprecocementeemumapopulac¸ãoselecionada.OMgSO4 intravenosopossuiumperfildeseguranc¸asemelhanteaoutrasterapiasdeasma.
Conclusões: OtratamentocomMgSO4 intravenosoreduzaschancesde internac¸ões
hospita-lares.OusodeMgSO4intravenosonoprontosocorronãoéassociadoaefeitoscolateraisou
danossignificativos.EnfatizamosopapeldoMgSO4comoumaterapiaadjuvante,aopassoque
oscorticosteroideseasbeta-agonistascontinuamosagentesterapêuticosagudosprimários. ©2017SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4. 0/).
Introduction
Asthma is a reversible, diffuse lower airway obstruc-tioncausedby airwayinflammationand edema,bronchial smooth-musclespasm,andmucousplugging.Thecomposite effectleadstoexpiratoryairflowobstruction.1Asthmacould belife-threateningand mustbe promptlytreated.Severe asthma is oftendefined asfailureto improveafter 2h of conventional emergency department (ED) treatment, and commonlypresentwithmoderatehypoxemia.Thepresence ofhypoxemiashouldbeassessednon-invasivelywithapulse oximeter.Bloodgas,serologicalorradiological studiesare notnecessarytodefineordetermineitsseverity.
Perspectiveonahealthchallenge
Asthmais theleadingcause ofchronic illness inchildren; 19---24% of Brazilian children have been diagnosed with asthmaatsome timeintheirlives.2 Itisthethirdleading causeofhospitalizationsamongchildren undertheageof 15years.Severeasthmaisoneofthemostcommonsevere,
reversibleconditionsin EDs.1,2 Whileasthma-related mor-talitymaybeimproving, one-thirdofthe deathsoccurred beforemedicalattentionwasprovided.3EDmanagementto reverstheprogressiontowardrespiratoryfailureshouldbe structuredandaggressive,asinvasive mechanical ventila-tion is fraught with many complications and an elevated mortality.4 Due to the enormous health care burden of asthma, all medical treatments need to be scrutinized regardingtheircost-effectiveness.
Pathophysiology
exposestheterminalnervestoexcessivecholinergic stimu-lation,exacerbatingsmoothmusclecontraction.5
The progression of this physiopathology results in widespread lung heterogeneity with severe bronchocon-striction. Lung areas with mucus plugging and atelectasis alternatewithareasof hyperinflationduetoairtrapping. Thecombinedeffectsoftheaforementionedprocesseslead to ventilation perfusion mismatch (V/Q mismatch), with the clinical expression of hypoxemia. Air trapping puts the diaphragm in a disadvantageous position, losing its areaofappositionandproducinganineffectiveeffort.The respiratory work load increases dramatically, and inspira-tory substernal retractionsare observed, progressingto a paradoxicalthoraco-abdominalbreathingpattern.Insevere cases,thecardiacoutputiscompromised,witha combina-tionof dehydration,increasedpulmonary venous pressure creating a dynamic decreased venous return to the right atrium,andashiftoftheintraventricularseptum,impinging theleftventriclepreload.
Clinicalpresentation
Themajorityofsevereasthmaexacerbationsoccurafteran exposuretoallergictriggersorinthesettingofaviralupper respiratory infection. Most children present with cough, wheezing,prolongedexpiratoryphase,andincreasedwork of breathing while under mild hypoxemic conditions and dehydration. The degree of wheezing does not correlate well with severityof the disease. Clinical asthma scoring systems,suchastheWoodsscore,lackgranularity,butare helpfulinpatientfollow-up.6Thisandotherclinicalscores express categorical variables (mild/moderate/severe) as a number,1---3 which facilitates the trending of acuity on a single patient; nonetheless, any statistical analysis of theseresultsshouldbeperformedascategoricalvariable. Peakexpiratoryflowrate(PEFR),incooperative previously-trained patients, provides a more granular assessment. However,itis aneffort-dependent techniqueanddifficult toperformwhileinrespiratorydistress,unlessthe investi-gatorsarepreviouslytrainedtoperformspirometrytesting.7 Thepresenceofpulsusparadoxusdenotesseverity,butitis difficulttoberepeatedlyassessedinabusyED.
InitialEDmanagement
AnorganizedandresoluteEDinitialmanagementisneeded, due to the compounded facts that severe asthma is: (a) a condition witha high incidence,(b) has a potentialfor reversibility,(c)hastherisktoprogresstowardrespiratory failure,and(d) theED needstojudiciouslymanage hospi-taladmission.Theprimarygoalistostabilizepatientsand rapidly identify thosein whom the process is not rapidly reversibleorwhoareatahighriskofdeterioration.
Theinitialtreatmentsincludeoxygen,intravenousfluids, intravenousor oral corticosteroid,repeatedor continuous nebulizationofa2adrenergic(i.e.,salbutamol),nebulized
muscarinic anticholinergic (i.e., ipratropium), and intra-venousMgSO4.
Failure to improve after the aforementioned regimen, assessedaspersistenceofrespiratorydistressuponclinical exam,isdefinedassevereasthma(orstatusasthmaticus).
Methylxanthines and subcutaneous or intravenous  -agonists are not routinely utilized as a first line therapy in the United States. However, a study from Porto Ale-gre that assessed the effects of intravenous salbutamol in ED, observed a decrease in the 2 adrenergic
nebu-lizationrequirementssubsequenttothepatients’hospital admission.8 Thatstudy only addressedchanges in respira-toryrateanddidnotcontrolforalterationsinotherclinical findings.Italsodidnot statewhether vitalsigns monitor-ingwasperformedinablindedfashion.Helioxmayimprove the aerosol delivery of 2 adrenergic to the lower air-way;nonetheless, it is expensive and does not appear to offer a consistent and significant clinical benefit.9,10 and cost-effective studies are required. BIPAP support in the ED appears to stabilize patients with status asthmaticus beforethehospitaladmission;however,thecumulativedata (two publications) is scarce torecommend it as standard therapy.11,12
Inturn,theuseofintravenousMgSO4hasemergedasa proven strategyto reduce hospital admissions. This study aimedtoreview thedifferent regimens for MgSO4 admin-istrationanditscontributioninthemanagementofsevere asthma.
MgSO4mechanismofactionandkinetics
The primary mechanism of action of intravenous MgSO4
is thought to be secondary to its spasmolytic proper-ties. Supra-physiologic unbound serum magnesium (Mg), directlyrelated toionized Mg,produces atransient block ofthe N-methyl-d-aspartatereceptor-gated calcium
chan-nels with subsequent muscle relaxation. Blocking the Ca entryintotheairwaysmoothmuscleinterfereswithsmooth muscle contraction, inducing bronchodilation.13---15 While other mechanisms modulating the inflammatory reaction, such the attenuation of the neutrophil respiratory burst, have putative beneficial effects, their degree of contri-bution in the therapeutic management of acute asthma is less clear.16 The Mg2+ ion, due to its effects on Ca, alsoinhibitsthereleaseofacetylcholinefrommotornerve terminals, inhibiting histamine release from mast cells and decreasing the production of mucus in the secretory glands.17
ExperienceintheuseofintravenousMgSO4in asthmaticchildren
MgSO4 is inexpensive,has minimal adverse effects at the
dosesindicated,andiswidelyavailable.Theonsetofaction of intravenous MgSO4 is rapid (within minutes), a
neces-sityinemergencysettings.Sinceitsoriginaldescriptionin 1936,theoptimaldoseofIVMgSO4asabolushasnotbeen
established,leadingtotheutilizationofawidedoserange, from25to>100mg/kg.18---22Multicenterstudieshavefailed todemonstrateaconsistentdecreaseinhospitaladmissions orearlydischarge.23---25
These inconsistent results could bein part due to: (a) failuretotakeintoconsiderationtheMgSO4 pharmacokine-tics,(b)failuretoconceptualizeMgSO4asatime-sensitive therapy,(c)theinherentchallengesoftheaforementioned ‘‘outcomevariables’’inasthma,or(d)enrollmentof indi-vidualswithcurrentinfectiousprocess,withongoingstimuli forbronchoconstrictionanddamagetotheairway.
Someclinical studiesindicatethe needfor higher-dose regimens.22,26Ciaralloetal.reportedpositiveresultsintwo clinicaltrials, separatedbya periodof fouryears,where thedosewasincreasedfrom25mg/kgto40mg/kg, adminis-teredover20min.22Aretrospectivepharmacokineticstudy involving 54children suggested theneed for 50---75mg/kg bolustoattainaMglevelnear4mg/dL(1.64mmol/L).19In astudyconductedinIndiawith47children,Devietal.used 100mg/kg over 35min with a co-administration of intra-venous aminophylline. The results show an improvement in clinical and PEFR scores; the graphic display implied beneficial effects in oxygenation starting in the first few hoursand continuing for 10---12h.27 Nevertheless, the co-administrationofaminophyllineinthisstudyleadstodoubts aboutwhetherMgSO4alonecausedthiseffect.
The prompt initiation of therapy may be correlated with its efficacy. A study performed in Argentina indi-cated that early administration in the ED wasassociated with fewer patients, later on, requiring mechanical ven-tilation in a pediatric intensive care unit (PICU).25 Of note, the control group comprised younger subjects and mayhave included infantswithbronchiolitis.A large ran-domized clinical trial with 100 patients in India, using a modifiedasthma clinicalseverityscore,demonstratedthe superiorityofanearlyintravenousMgSO4bolusover terbu-talineoraminophyllineinfusions20;ofnote,manyofthese patients were very young and infection-mediated asthma was not identified. Another randomized trial in a Brazil-ianED demonstratedthesuperiorityof intravenousMgSO4 overplacebo,withalmostidenticaleffects tointravenous Salbutamol while using surrogate variables of efficacy in patients that were later hospitalized.8 An earlier meta-analysisconductedbyCheuketal.includingfivetrialsthat assessedMgSO4versusplacebodemonstratedMgSO4 effec-tivenessinpreventinghospitalization.28Amorerecentand stricter meta-analysisinvolving three trials(115 children) concludedthatthe true estimatedreduction inadmission wasbetween86%and26%,duetothewideconfidence inter-val(oddratio:0.32, 95%CI: 0.14---0.74).Nevertheless, an numberneededtotreat(NNT)of5couldbeascribedtothe useofintravenousMgSO4intheEDtopreventonehospital admission.29
The need to return to the ED after discharge has not been well documented. One study with 47 children reports a reducedlength ofstay of 5.3h on patientswho were admitted.28 This is an elusive variable as, once the patient is admitted, discharge may not be solely depen-dentonthepatient’sconditionbutratherontheavailability of medical personnel, time of the day, and day of the week.
High-doseMgSO4continuousinfusion(HDMI)
Much of the magnesium in serum is attached to albu-min, while ionized Mg (IoMg; the free form) is the pharmacologically active form in asthma. IoMg makes up 55% of extracellular Mg; however, the relation of Mg/IoMg is adversely altered in asthma and critically ill patients.24,25,27 Animal studies indicate that IoMg concen-trations≥1mmol/Larerequiredtoproducesmoothmuscle relaxation.15
These and other factors lead the authors to study high-dose MgSO4 continuous infusion (HDMI) in children in the setting of severe asthma and status asthmaticus. HDMI has been used in patients with pulmonary hyper-tension, brain injury, and subarachnoid hemorrhage, as well as extensively in preeclampsia.30---33 In these scenar-ios, the strategy is to maintain a consistent therapeutic level to compensate for MgSO4’s rapid elimination. This approach has been rarely adopted in asthma cases.28,34 The obstetrics and gynecology literature targets Mg infu-siontoclinicalsignsofweakening,butnotlosing,patellar reflexes as reflection of adequate spasmolysis. This usu-ally represents serum Mg of 4.8---8.4mg/dL with IoMg 0.9---1.6mmol/L.15,35,36
AretrospectivestudybyGloveretal.oncontinuous intra-venousMgSO4useinchildrenattemptedtoassesssafety,but hadmanyconfoundingvariables.Thoseauthorsdescribeda heterogeneousgroup withalarge variationin dosage and regimen duration, bolus of 35.3±12.7mg/kg, infusion of 21.6±6mg/kg/hfor93.8h±89.2h,withoutsignificantside effects.26
Inthispractice,thepresentauthorsretrospectively ana-lyzedtheuseofHDMI inthesettingofstatusasthmaticus within the confines of the pediatric intensive care unit (PICU).37 The HDMI regimens consisted of an initial bolus thatwasweight-dependent:50mg/kg(>30kg)or75mg/kg (≤30kg)overaperiodof30---45min;followedbya continu-ousinfusionof50mg/kg/h,for4h.Serummagnesiumlevels were 4.4±0.8mg/dL, and IoMg 0.95±0.2mmol/L at the endoftheinfusion,withinthetargetrange.In12patients, troponinlevelsandelectrocardiogramswereallnormal.37
0%
11% 11%
47%
0% 10% 20% 30% 40% 50%
Bolus
HDMI
12
hrs.
24
hrs.
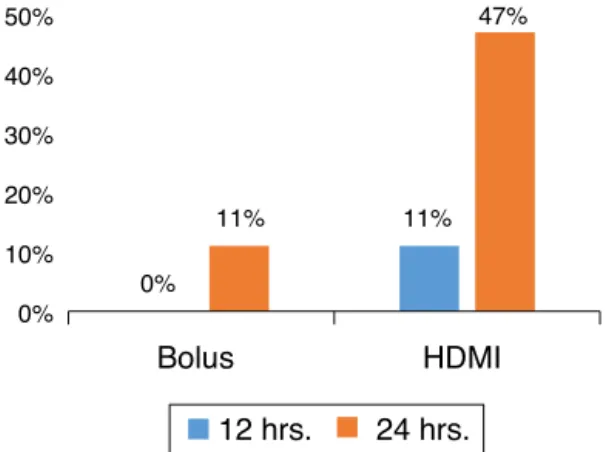
Figure1 PercentageofpatientsdischargedhomefromtheED bygroup.Bolus,50mg/kg/1h;HDMI,200mg/kg/4h.Columns representpatientsdischarged,bygroup.HDMI,high-dose mag-nesiuminfusion.
MgSO4HDMIvs.Bolus
Ina prospective,randomizedEDstudy for severeasthma, withpatientswithoutunderlyingco-morbidityorinfectious etiology,theauthorsdeterminedthatHDMIwassuperiorto MgSO4bolus(Fig.1)inshorteningtheEDlengthofstaywhile
reducingcosts.40
PatientswererandomizedtoreceiveintravenousMgSO4 50mg/kg bolus (over 1h) or HDMI (50/mg/kg/h for 4h), diluted in 0.9% saline solution at a concentration of 10mg/mL. The HDMI group presented a lower length of stay (HDMI, 34±19h; bolus, 48±19h; p=0.031; 95% CI: 1.3---26.5).Moreover,at24h,nineoutof19patients(47%) in the HDMI groupwere discharged,versus twoout of 21 (10%)in the bolus group(p=0.012), withan absoluterisk reduction(ARR)37%(95%CI:11---63).HDMIwassuperiortoa bolusasanearlyadjunctivetreatment,withaNNTof3(95% CI:1.6---9.5)tofacilitateadischargeat24hfromtheED.39 Interimanalysisat 12and36h presentedthesametrends favoringtheHDMIgroup;two-thirdsofthepatientsinthis groupweredischargedat36h(p=0.009;ARR:42%;95%CI: 14---70%;NNT: 3;95% CI:1.4---7.3).The useof HDMIin the EDmanagementofasthmawascost-effectiveinthepresent institution.39
Sideeffectsandpotentialchallenges
MgSO4-inducedmuscleweakness,withtheconsequentrisk
of respiratory failure, and potential vasodilatation, with subsequenthypotension, areof concerns whenutilizedin the context of asthma.41,42 Although many earlier studies showedminimalornoadverseeffects,thefearoftheseside effectsispervasive.Minorsideeffectsweredescribedin16% ofpatients:epigastricwarmth,tingling,numbness,andpain at thesiteof infusion,allof themappearingwithin5min of theinitiationand disappearingshortly afterwards.27 Of note,thatstudyappearstohaveusedabolusof100mg/kg over35min.27 Schuhetal.foundcontradictorybehaviorin anonlinesurveyofEDphysicians.Whilemorethan80%of respondersagreedthatthereweredata tosupportuseof MgSO4,itwasutilizedinlessthan20%ofthetime;24%of surveyedphysiciansrecalledobservingatleastoneepisode
of hypotension requiring intervention, and 23% had con-cernsaboutitssideeffects.Anonlinesurvey,amethodology thatsuffers fromself-selection bias and subjective recall bias,emphasizedthegeneralpredispositionofphysiciansto developopinionswhenthereislackofdata.34
In four HDMI studies, no significant side effects were observed, except for one patient reporting nausea, two painattheinjectionsite,andtwogeneralizedflushing.No patientexperiencedsignificantmuscleweaknessortheneed forrespiratorysupport.Lowdiastolicbloodpressureshould beexpectedduringHDMIifmeasuredbyautomated sphyg-momanometer.Theauthorsobservednormaltroponinlevels of 0.05±0.01ng/mL and no EKG changes during HDMI.38 Ofnote,inanon-invasivemethod,thechangesintonality betweenthe4thtothe5thKorotkoffdeterminethediastolic bloodpressure.43Automatedsphygmomanometershave dif-ficultelucidating this change when patients arereceiving ahigh dose 2 adrenergic or HDMI. A study withinvasive intra-arteriallinemaybeabletorefinethispoint.
A contemporary problem is that an increased propor-tionofpatientswithasthmaareobese,44,45whichrequires adjustmentsin theintravenous dose.In thispractice,the authorsadjustthedosagetoidealbodyweightwhenBMIis ≥25.Furtherstudiesinthisareaarealsoneeded.
InhaledMgSO4inasthma
Thelargeefficacyofthenebulized-agonistsinthe treat-ment of asthma makes their role undisputed. However, inhaledmedicationsaredifficulttodelivertotheaffected bronchi,even underidealconditions. Studies have shown thatonlyabout10%ofbronchodilatorsreachthelungand arelargelyaffectedbyrespiratoryrate,tidalvolumes,dead spaceventilation(Vd/Vt), bronchoconstriction,methodof delivery, mouth breathing, and particle size and deposi-tion.
The use of inhaled magnesium sulfate has presented inconsistentresults.Asystematicreviewshowedthat clin-ical trials that assessed the use of inhaled MgSO4 failed to find a beneficial effect, and its use is not widely recommended.46
Conclusions
Improvements in the ED management of severe asthma, aleading diagnosis for admissionto hospitals,could have asignificant economic impact, in particular in areas with lowersocioeconomic resources. A preplanned, organized, anddecisiveEDinitialmanagementisparamounttoreverse a condition that can evolve toward respiratory failure. The authors emphasize the role of MgSO4 as an
adjunc-tive therapy in the initial management of asthma, while
2adrenergicandcorticosteroidsremaintheprimary
ther-apy.Itispossiblethattheinconsistentresultsfromprevious MgSO4 studies weredue to a failureto achieve sustained
serummagnesiumandspasmolyticeffectsfor2adrenergic
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Kelly HW. The new National Asthma Education and Preven-tion Program’s guidelines onthe diagnosis and management of asthma and childhood asthma treatment. J Allergy Clin Immunol.2008;20:263---8.
2.SoléD,RosárioFilhoNA,SarinhoES,Camelo-NunesIC,Barreto BA,MedeirosML,etal.Prevalenceofasthmaandallergic dis-easesinadolescents:nineyearfollowupstudy(2003---2012).J Pediatr.2015;91:30---5.
3.PrietschSO,ZhangL,CatharinoAR,VauchinskiL,RodriguesFE. AsthmamortalityamongBrazilianchildrenupto19yearsold between1980and2007.JPediatr.2012;88:384---8.
4.Bratton SL, Newth CJ, ZuppaAF, MolerFW, Meert KL, Berg RA, et al. Critical care for pediatric asthma: wide care variability and challenges for study. Pediatr Crit Care Med. 2012;13:407---14.
5.BelvisiM.Overviewoftheinnervationofthelung.CurrOpin Pharmacol.2002;2:211---5.
6.HsuP,LamLT,BrowneG.Thepulmonaryindexscoreasaclinical assessmenttoolforacutechildhoodasthma.AnnAllergyAsthma Immunol.2010;105:425---9.
7.Silverman RA,FlasterE, EnrightPL,SimonsonSG. FEV1 per-formanceamong patientswithacute asthma:resultsfrom a multicenterclinicaltrial.Chest.2007;131:164---71.
8.Santana JC,Barreto SS,PivaJP, GarciaPC.Controlled study onintravenousmagnesiumsulfateorsalbutamolinearly treat-ment of severe acute asthmaattack in children. J Pediatr. 2001;77:279---87.
9.Bigham M. Helium/oxygen-driven albuterol nebulization in themanagement ofchildrenwithstatusasthmaticus: a ran-domized, placebo-controlled trial. Pediatr Crit Care Med. 2010;11:356---61.
10.BraunFilhoLR.Useofhelium-oxygenmixture(Heliox®)inthe treatmentofobstructive lowerairway diseaseina pediatric emergencydepartment.JPediatr.2010;86:424---8.
11.BasnetS,ManderG,AndohJ,KlaskaH,VerhulstS,KoiralaJ. Safety,efficacy,andtolerabilityofearlyinitiationof noninva-sivepositivepressureventilationinpediatricpatientsadmitted withstatusasthmaticus.PedCritCareMed.2012;13:393---8. 12.KorangSK,FeinbergJ,WetterslevJ,JakobsenJC.Non-invasive
positive pressure ventilation for acute asthma in children. CochraneDatabaseSystRev.2016;9:CD012067.
13.DelCastilloJ,EngbaekL.Thenatureoftheneuromuscularblock producedbymagnesium.JPhysiol.1954;124:370---84. 14.GourgoulianisKI,ChatziparasidisG,ChatziefthimiouA.
Magne-siumasarelaxingfactorofairwaysmoothmuscles.JAerosol Med.2004;14:301---7.
15.YoshiokaH,HirotaK,SatoT,HashimotoY,IshiharaH,MatsukiA. Spasmolyticeffectofmagnesiumsulfateonserotonin-induced pulmonaryhypertensionandbronchoconstrictionindogs.Acta AnaesthesiolScand.2001;45:435---40.
16.CairnsCB,KrafiM.Magnesiumattenuatestheneutrophil respi-ratory burst in adult asthmatic patients. Acad Emerg Med. 1996;3:1093---7.
17.Middleton E. Antiasthmatic drug therapy and calcium ions: review of pathogenesis and role of calcium. J Pharm Sci. 1980;69:243251.
18.ChesleyLC,TepperI.Someeffectsofmagnesiumloadingupon renalexcretionofmagnesiumandcertainotherelectrolytes.J ClinInvest.1958;37:1362---72.
19.RowerJE,LiuX,YuT,MundorffM,SherwinCM,JohnsonM. Clin-icalpharmacokineticsofmagnesiumsulfateinthetreatment ofchildrenwithsevereacuteasthma.EurJClinPharmacol. 2017;73:325---31.
20.SinghiS,GroverS,BansalA,ChopraK.Randomisedcomparison of intravenous magnesium sulphate, terbutaline and amino-phyllineforchildrenwithacutesevereasthma.ActaPaediatr. 2014;103:1301---6.
21.MorrisI,Lyttle MD, O’SullivanR, SargantN,Doull IJ, Powell CV.Whichintravenousbronchodilatorsarebeingadministered tochildrenpresentingwithacuteseverewheezeintheUKand Ireland.Thorax.2014;70:88---91.
22.CiaralloL,BrousseauD,ReinertS.Higher-doseintravenous mag-nesiumtherapy for children withmoderate to severe acute asthma.ArchPediatrAdolescMed.2000;154:979---83.
23.ScarfoneRJ,LoiselleJM,JoffeMD,MullCC,StillerS,Thompson K,etal. Arandomizedtrialofmagnesiumintheemergency departmenttreatmentofchildrenwithasthma.AnnEmergMed. 2000;36:572---8.
24.GoodacreS,CohenJ,BraidburnM,BengerJ,CoatsT.The3Mg trial:arandomisedcontrolledtrialofintravenousornebulised magnesiumsulphateversusplaceboinadultswithsevereacute asthma.HealthTechnolAssess.2014;18:1---168.
25.TorresS.Effectivenessofmagnesiumsulfateasinitialtreatment ofacutesevereasthmainchildren:arandomized,controlled trial.ArchArgentPediatr.2012;110:291---7.
26.GloverML,MachadoC,TotapallyBR.Magnesiumsulfate admin-isteredviacontinuousintravenousinfusioninpediatricpatients withrefractorywheezing.JCritCare.2002;17:255---8. 27.DeviPR,Kumar L,SinghiSC, PrasadR, SinghM. Intravenous
magnesiumsulfateinacutesevereasthmanotresponding to conventionaltherapy.IndianPediatr.1997;34:389---97. 28.CheukDK.Ameta-analysisonintravenousmagnesiumsulphate
fortreatingacuteasthma.ArchDisChild.2005;90:74---7. 29.GriffithsB,KewKM.Intravenousmagnesiumsulfatefor
treat-ingchildrenwithacuteasthmaintheemergencydepartment. CochraneDatabaseSystRev.2016;4:CD011050.
30.SibaiBM,GrahamJ,MccubbinJH.Acomparisonofintravenous andintramuscularmagnesiumsulfateregimensin preeclamp-sia.AmJObstetGynecol.1984;150:728---33.
31.NataleJE, GuerguerianAM, JosephJG,McCarter R, ShaoC, SlomineB,et al.Pilot studytodetermine thehemodynamic safetyand feasibility of magnesium sulfate infusion in chil-drenwithseveretraumaticbraininjury.PediatCritCareMed. 2007;8:1---9.
32.RaimondiF,MigliaroF,CapassoL,AusanioG,BiscegliaM, Gilib-ertiP,etal.Intravenousmagnesiumsulphatevs.inhalednitric oxideformoderate,persistentpulmonaryhypertensionofthe newborn:a multicentre, retrospective study.J Trop Pediatr. 2007;54:196---9.
33.Ma L, Liu W, Zhang J, Chen G, Fan J, Sheng H. Magne-siumsulphateinthemanagementofpatientswithaneurysmal subarachnoidhaemorrhage:ameta-analysisofprospective con-trolledtrials.BrainInj.2010;24:730---5.
34.SchuhS, MaciasC,FreedmanSB,PlintAC,ZorcJJ,BajajL, etal.NorthAmericanpracticepatternsofintravenous magne-siumtherapyinsevereacuteasthmainchildren.AcadEmerg Med.2010;17:1189---96.
35.AaliBS, KhazaeliP,GhasemiF.Ionizedand totalmagnesium concentrationinpatientswithseverepreeclampsia-eclampsia undergoingmagnesiumsulfatetherapy.JObstetGynaecolRes. 2007;33:138---43.
36.Handwerker SM, Altura BT, Chi DS, Altura BM. Serum ionized magnesium levels during intravenous MGSO4 ther-apy of preeclamptic women. Acta Obstet Gynecol Scand. 1995;74:517---9.
withstatusasthmaticus. JPediatr PharmacolTher. 2012;17: 150---4.
38.Egelund TA, Wassil SK, Edwards EM, Linden S, Irazuzta JE. High-dosemagnesiumsulfateinfusionprotocolforstatus asth-maticus:asafetyandpharmacokineticscohortstudy.Intensive CareMed.2012;39:117---22.
39.IrazuztaJE, ParedesF,PavlicichV, DominguezSL. High-dose magnesiumsulfateinfusionforsevereasthmaintheemergency department.PediatrCritCareMed.2016;17:29---33.
40.VaiyaniD,Irazuzta JE. Comparisonof twohigh-dose magne-siuminfusionregimensinthetreatmentofstatusasthmaticus. JPediatrPharmacolTher.2016;21:233---8.
41.KellyHW.Magnesiumsulfateforsevereacuteasthmain chil-dren.JPediatrPharmacolTher.2003;8:4045.
42.FasslerCA.Magnesiumtoxicityasacauseofhypotensionand hypoventilation.ArchInternMed.1985;145:1604---6.
43.MeyC,SchroeterV,ButzerR,RollS,BelzG.Methodspecificity ofnon-invasivebloodpressuremeasurement:oscillometryand fingerpulsepressurevsacousticmethods.BrJClinPharmacol. 1995;40:291---7.
44.BeutherDA,WeissST,SutherlandER.Obesityandasthma.Am JRespCritCareMed.2006;174:112---9.
45.FariaAG,Ribeiro MA,Marson FA, SchivinskiCI, SeverinoSD, RibeiroJD,etal.Effectofexercisetestonpulmonaryfunction ofobeseadolescents.JPediatr.2014;90:242---9.