www.jped.com.br
REVIEW
ARTICLE
Severe
forms
of
food
allergy
夽
Emanuel
Sarinho
a,b,c,∗,
Maria
das
Grac
¸as
Moura
Lins
a,daUniversidadeFederaldePernambuco(UFPE),Recife,PE,Brazil
bUniversidadeFederaldePernambuco(UFPE),ProgramadeResidênciaMédicaemAlergiaeImunologia,Recife,PE,Brazil cSociedadeBrasileiradePediatria,DepartamentodeAlergia,RiodeJaneiro,RJ,Brazil
dUniversidadeFederaldePernambuco(UFPE),ProgramadeResidênciaMédicaemGastropediatria,Recife,PE,Brazil
Received2May2017;accepted14June2017 Availableonline21September2017
KEYWORDS
Severeformsoffood allergy;
Foodanaphylaxis; Food-protein-induced enterocolitis
syndrome
Abstract
Objectives: To guide the diagnosticand therapeutic management ofsevere forms of food allergy.
Datasources:Search in the Medline database using the terms ‘‘severe food allergy,’’ ‘‘anaphylaxisandfoodallergy,’’‘‘generalizedurticariaandfoodallergy,’’and‘‘food protein-induced enterocolitis syndrome’’ in the lastten years, searching inthe title, abstract, or keywordfields.
Summaryofdata: Foodallergycanbeseriousandlife-threatening.Milk,eggs,peanuts,nuts, walnuts,wheat,sesame seeds,shrimp,fish,andfruit canprecipitate allergicemergencies. The severity ofreactions willdependonassociated cofactors suchas age,drug useatthe onsetofthereaction,historyandpersistenceofasthmaand/orsevereallergic rhinitis, his-toryofpreviousanaphylaxis,exercise,andassociateddiseases.Forgeneralizedurticariaand anaphylaxis,intramuscular epinephrineisthefirstandfundamental treatmentline.Forthe treatment inacutephaseoffood-inducedenterocolitissyndromeintheemergency setting, prompthydroelectrolyticreplacement,administrationofmethylprednisoloneandondansetron IVarenecessary.Itisimportanttorecommendtothepatientwithfoodallergytomaintainthe exclusiondiet,seekspecializedfollow-upand,inthosewhohaveanaphylaxis,toemphasize theneedtocarryepinephrine.
Conclusion: Severefoodallergymayoccurintheformofanaphylaxisandfood-protein-induced enterocolitis syndrome, which areincreasingly observed inthe pediatric emergency room; hence,pediatriciansmustbealertsotheycanprovidetheimmediatediagnosisandtreatment. ©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 4.0/).
夽
Pleasecitethisarticleas:SarinhoES,LinsMG.Severeformsoffoodallergy.JPediatr(RioJ).2017;93:53---9.
∗Correspondingauthor.
E-mail:emanuel.sarinho@gmail.com(E.Sarinho). https://doi.org/10.1016/j.jped.2017.06.021
PALAVRAS-CHAVE
Formasgravesde alergiaalimentar; Anafilaxiaalimentar; Síndromeda
enterocoliteinduzida pelaproteína alimentar
Formasgravesdealergiaalimentar
Resumo
Objetivos: Abordaromanejodiagnósticoeterapêuticodasformasgravesdealergiaalimentar.
Fontesdosdados: BuscaativanabasededadosMedlinedostermos‘‘severefoodallergies’’, ‘‘anaphylaxisandfoodallergy’’e‘‘foodprotein-inducedenterocolitis’’nosúltimosdezanose combuscanoscampostítulo,resumooupalavra-chave.
Síntesedosdados: Aalergiaalimentarpodesergraveeameac¸adoraàvida.Leite,ovo, amen-doim,castanha,noz,trigo,gergelim,crustáceo,peixeefrutaspodemprecipitaremergências alérgicas.Agravidadedasreac¸õesvaidependerdefatoresassociadostaiscomoidade,usode medicamentosnoiníciodareac¸ão,persistênciadeasmae/ourinitealérgicagrave,históriade préviaanafilaxia,exercícioedoenc¸asintercorrentes.Paraanafilaxia,aadrenalina intramuscu-laréumaindicac¸ãobemestabelecida.Paraotratamentodasíndromedaenterocoliteinduzida pela proteína alimentar nafase aguda nosetor de emergência,faz-se necessária a pronta reposic¸ãohidroeletrolítica,aadministrac¸ãodemetilprednisolonaeodansetronaIV.Importante recomendaraopacientecomodiagnósticodealergiaalimentargravequemantenhaadieta deexclusão,procureacompanhamentoespecializadoe,naquelesqueapresentaramanafilaxia, enfatizaranecessidadedeportaradrenalina.
Conclusão: Alergiaalimentargravepodesemanifestarcomoanafilaxiaousíndromeda ente-rocoliteinduzidaporproteínaalimentaremfaseagudaasquais,porseremcondic¸õescadavez maispresentesereconhecidasnosetordeemergênciapediátrica,demandam diagnósticoe tratamentoimediatos.
©2017SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4. 0/).
Introduction
Severe food allergy refers to the abnormal immune response to a certain food in a susceptible host, caus-inglife-threateningclinicalsyndromestothelatter.1These reactions arereproducibleeach timethefood isingested and,mostofthetime,aredose-independent.1They com-prise food-induced anaphylaxis, which is mediated by IgE andtheacuteformofthefood-protein-inducedenterocolitis syndrome(FPIES),thoughttobemediatedbycells.2
Anaphylactic reactions to eggs and fish have been describedsincethe16thand17thcenturies.Decadesago,it wasarareevent,butaprogressiveincreaseinitsprevalence hasbeenobserved;currently,severefoodallergyisthemain causeof emergencycare due toanaphylaxis.3 Milk, eggs, peanuts,nuts,walnuts,wheat,sesameseeds,crustaceans, fish,andfruit aresome ofthe foods that canprecipitate allergicemergencies.
In Brazil, a survey aimed at allergists indicated food allergyasthesecondcauseofanaphylaxis.Themainculprits werecow’smilkandeggwhitesininfantsandpreschoolers, andcrustaceansinolderchildren,adolescents,andadults.4 Inameta-analysisoftheliterature,theestimatedincidence of fatality in high-income countries due to food anaphy-laxisinchildrenunder19yearsofagewas3.25permillion persons/year.5The earlyestablishment ofthe correctand immediatediagnosisandtreatmentbytheemergency pedi-atriciancanpreventlethalityandeffectivelysavelives.
The objective of this article is to guide the physician in the diagnostic and therapeutic management of severe forms of food allergy, based on an active search in the Medlinedatabaseusingtheterms‘‘severefoodallergies,’’ ‘‘anaphylaxisandfoodallergy,’’and‘‘foodproteininduced
enterocolitis’’ within the lastten years; the search com-prisedthe title,abstract,and keywordfields.The review and recommendation articlesthat were useful, according totheauthors’evaluation,wereselectedforreadinginfull tosupportthearticlescope.
Thetwofoodallergysituationsthatleadthepatientto emergencycarearefoodanaphylaxisandFPIES,whichare clinical entities withdifferentpresentations and manage-ment and will be approached sequentially in thisarticle. However,inbothapproaches, theemphasiswillbeonthe pathophysiology and associated aspects in the diagnosis, emergencytreatment,andpatientguidance.
Anaphylaxis
due
to
food
allergy
Physiopathologyandassociatedaspects
Food anaphylaxis is the severe IgE-mediated reaction to food, in which generalized and life-threatening vasodila-tion occurs. The release of vasoactivemediators into the bloodstream can lead to vascular collapse, anaphylaxis, andshock.Vasodilationisaccompaniedbyhypotensionand hypoperfusion,whichcancompromisevitalorganssuchas thebrainandheart,resultinginischemiaanddeath.When cardiovascular symptoms,such ashypotension andshock, andneurologicalsymptoms,suchasmentalconfusion,loss ofconsciousness,andsphincterrelaxationarepresent,the riskofdeathishigh.Epinephrineadministrationandlower limbelevation,restoringvasculartonusandvenousreturn, arelife-savingmeasures.4
appearearlierandforetellapotentiallyfatal condition.It allstartswiththeexposuretoafoodallergen,whichforms abivalentbindingwiththespecificIgEthatisfixatedinthe high-affinityreceptorsofmastcells.Throughtheion chan-nels, this binding leads toreticular activation and to the releaseofmediatorssuchashistamine(themainmediator oferythemaandpruritus)andseveralotherpotentneo-and pre-formedvasodilators,whichcauseedemainthe superfi-cialanddeepdermisandsubcutaneouscelltissue,resulting in urticariaandangioedema.Inthe digestivesystem, this processcausesnausea,vomiting,anddiarrheaand,in the respiratorytract,intensecoryza,sneezing,coughing, bron-chospasm,laryngealedema,andevenapnea.4,6,7
The presence of generalized urticariaand angioedema are often the initial symptoms, indicating that vasodila-tionandbronchoconstrictionareimminentandthepatient mustbeidentifiedandtreatedurgentlytorestorethe vascu-lartonus.8,9Theassociationwithasthmaincreasesreaction severity,andresponsetotreatmentismuchmoredifficult. Ithasbeenobservedthatupto75%ofthepatientswithfatal anaphylaxishadconcomitantasthma.6,7,9
Sometimes,severefoodallergydevelopsduringexercise, in association witha specific food (up to4h after inges-tion), characterizing a food-dependent exercise-induced anaphylaxis. Exercise may promote increased absorption of the inadequately processed allergen and/or promote the degranulation of sensitized basophils and mast cells, or further promote an over-synthesis of arachidonic acid metabolites.10 In this case, anaphylaxis results from the association of food and exercise, while food or exercise, alone,arewelltolerated.Wheatisthemostcommon aller-gen,butothergrains,nuts,andotherfoodshavealsobeen implicated.4,10
Food-dependent exercise-induced anaphylaxis may be precipitated by associated factors, such as the consump-tionofanti-inflammatories,especiallyaspirin,andtheuse ofalcohol,whichiscommonamongadolescents.10,11
Theseverityoffoodallergicreactionswilldependonthe amountofingestedallergen,itsstabilityagainstdigestion, andepithelialpermeability.10,11Associatedfactors,suchas age,druguseat thereactiononset,persistenceofsevere allergicrhinitis, history ofprevious anaphylaxis, exercise, andconcomitantdiseases,mustbeconsidered.10,11Thedose andtypeoffoodallergenthatsensitizesandcausessevere foodallergy mayvarybetween individuals,and mayeven varyinthesameindividualondifferentoccasions.Whenthe foodallergenishidden,itcanresultindelayedidentification oftheculpritagentandgreaterriskforpatients.11
Adolescents are at increased risk of fatal anaphylaxis becauseofgreaterdifficultyinfollowingtheexclusiondiet. Acute infectious diseases facilitate mast cell degranula-tionandfavortheonsetofsevere foodanaphylaxisin the presenceofthespecificallergen.Similarly,excessivelyhot showersanduseoffevermedicationmaypredisposetomore severereactions,astheyalterintestinalpermeability.11
In infants, cow’s milk protein is the most common precipitating agent of food anaphylaxis, but egg, soy-bean, and other proteins may also be implicated.1,4 In schoolchildren and adolescents, allergies to crustaceans, fish,peanuts,walnuts,andcashewspredominateas poten-tially life-threatening situations.4 Wheat is the most common precipitant of exercise-dependent food-induced
anaphylaxis,throughaproteinfractionfoundingluten, 5-omegagliadin.10
Diagnosisoffoodanaphylaxis
The diagnosis of food anaphylaxis is relatively easy to attain. It is important to emphasize that, because it is a potentially fatal allergic reaction, it should be treated as a medical emergency with the immediate administra-tion of epinephrine; therefore, the diagnosis should be associatedwithprompttreatment, sothattheresults are favorable.6,7Foodanaphylaxisoccurssuddenly,withinafew minutesorafewhoursafterfoodintake,withintense pru-ritus and generalized erythematous plaques that tend to converge. This picture is often accompanied by lip, eye, or even tongue and uvula angioedema, followed by fur-ther involvement of at least one of the following organ systems: respiratory (dyspnea, wheezing/bronchospasm, stridor, hypoxemia), cardiovascular (hypotension, hypoto-nia,shock), gastrointestinal(nausea, vomiting, abdominal pain),andneurological(mentalconfusion,lipothymia,loss of consciousness).In up to20% of cases, anaphylaxis can occurwithtwoormoreoftheseaffectedorgansystems,but withoutcutaneousinvolvement,whichmakesthediagnosis muchmoredifficult.4,6Anaphylaxisshouldbemainly differ-entiatedfromvaso-vagalsyndrome(inthiscase,theskinis cold,pale,andmoist),fromanacutecrisisofsevereasthma, andfrompost-feeding generalizedacuteurticaria,which, aspreviously mentioned, canbe considered andmanaged asanaphylaxis.4,6,8,9,11
Althoughurticariaandangioedemaarecommonsignsof foodallergicreactions, especiallyduringanaphylaxis,itis importanttonotethattheirabsencedoesnotexcludethe possibilityofseverefoodallergy.Upto20%ofcasesoffood anaphylaxismaypresentwithoutcutaneoussymptoms,and theabsenceofthesesymptomsmayresultinlate identifi-cationandtreatmentdelay,aswellasincreasedlethality.8 Inadditiontoclassicalfoodanaphylaxis,itisimportant torecognizefood-dependentexercise-inducedanaphylaxis. The initial symptoms are fatigue, heat, redness, pruri-tus,andurticaria,whichcansometimes subsidewhenthe patient interrupts the physical activity and rests; other times, when the exercise continues, angioedema, gas-trointestinal symptoms, laryngeal edema, bronchospasm, hypotension,andshockmightoccur.10
Whenthereisdoubtregardingthediagnosisof anaphy-laxis,themeasurementoftryptaselevels(collectedduring orshortlyaftertheeventresolution),whenavailable,may beusedtosubsequentlyconfirmthediagnosis.The measure-mentoftheIgEspecific forthefoodallergen components shouldbeperformedlater.4
Emergencytreatmentoffoodanaphylaxis
withoutdelay.Whenindoubt,thedrugshouldbepromptly administeredtopreventfatalanaphylaxis;particularlyfor foodallergies,itisalife-savingdrugandreducesthe like-lihood of hospitalization.7 The action mechanism occurs throughthe alpha-adrenergic effectthat reverses periph-eral vasodilation, significantly reduces mucosal edema, upper airway obstruction (laryngeal edema), as well as hypotensionandshock,inadditiontoreducingsymptomsof urticaria/angioedema.Its-adrenergicpropertiesincrease myocardialcontractility,cardiacoutput,andcoronaryflow, andhavea potentbronchodilatoraction.4,6 The intramus-cularrouteispreferable,asitreachespeakconcentrations fasterthanthesubcutaneous route,andis tentimessafer thanthebolusintravenousroute;additionally,withoutany riskoflossoftime,therichvascularizationof thismuscle allowsthemedicationtobereadilyabsorbedwithan imme-diateeffect,eveninastateofcirculatoryinsufficiency.4,6,12
Table1showstheguidelinesformanagingfood anaphy-laxisinthe emergencyroom.Adrenalinshouldbeusedat adoseof0.01mg/kgintramuscularly(IM)uptoamaximum doseof0.3mg/kginchildren.Iftheinitialresponseis insuf-ficient, after5 to 15min, the dose may be repeatedone or more times. It is estimated that up to 20% of treated patients may require a second dose. Late administration mayleadtoanincreasedriskofhospitalization,insufficient cardiac perfusion, hypoxic-ischemic encephalopathy, and death. The pharmacologicalaction alsoincludes transient pallor, tremor, anxiety, and palpitations, which, although perceivedasanadverseeffect,issimilartothephysiological reactionofacutestress.7
TheuseofsecondarydrugsisdescribedinTable2. Anti-histaminesareknowntopreventpruritusandurticaria,but theydo not alleviate respiratory symptoms, hypotension, orshock.Thus,similarlytocorticosteroids, theyare adju-vantdrugsthatarenotindicatedfortheinitialtreatment. Corticosteroids may help prevent the secondary phase of
anaphylaxis, which might recur within 12---24h after the initial event, but this biphasic presentation is consider-ably less commonin food allergy anaphylaxis.In cases of asthmacrises,theuseofinhaledbeta-2agonistsshouldbe considered.7
Inpatientswithahistoryofverysevereanaphylaxis,it is recommendedtostarttreatment withepinephrinesoon aftertheprobableingestionandonsetofthefirstsymptom (evenwhentheyaremildsymptoms,suchasitchingofthe face/mouth, mild gastric discomfort,or nausea), because therapidprogressiontosevereanaphylaxisisexpectedand usual.7Thesameconductisprudentandrecommendedfor childrenatriskofdevelopingfoodanaphylaxiswith uncon-trolledasthma.11
Recommendationstopatientsafterhospital discharge
Once thepatienthasbeen treated,itisessentialto iden-tifythe possible foodculprits. A patientwithanaphylaxis should remainonobservation for 12---24h, asasecondary delayresponsemayoccur;thepatientshouldalsobeadvised toavoidexercisesfor thenextsevendays.Prescriptionof oralcorticosteroids(prednisoneorprednisoloneatadoseof 1---2mg/kg/day,withamaximumdoseof40mg/day)forfive tosevendaysandofsecond generationantihistaminesfor atleastsevendays(e.g.,fexofenadineatadoseof2.5mL twicedailyforchildrenunder6years,5mLtwicedailyfor thoseolderthan6years,or1120mgtablet,twicedailyfor adolescents).Itisalsoprudenttoavoidphysicalactivityin theweekfollowingtheepisode.4
Forfood-dependentexercise-inducedanaphylaxis,which occursprimarilyinadolescents,itisalsorecommendedto refer the patient toa specialist. At the outpatient level, itwillbeassessedwhethertheIgEspecifictothepossibly
Table1 Conductandmaintherapeuticagentsinanaphylaxistreatment. Conduct/Therapeutic
agent
Recommendations
Maintainvitalsigns CheckA(airway),B(breathing),C(circulation), andM(Mind-sensory)
Maintainadequateposition(dorsaldecubituswith elevatedLL).
Gettinguporsittingdownsuddenlyisassociated withfataloutcomes(‘‘emptyventricle
syndrome’’).
Epinephrine1:1000 (1mg/mL)
Children:0.01mg/kguptoamaximumof0.3mg IM,intheanterolateralthigh.
Adolescents:0.2---0.5mg(maximumdose)IM,in theanterolateralthigh.
Administerimmediatelyandrepeatifnecessary, every5---15min.Monitortoxicity(heartrate) Epinephrineatdilutionsof1:10,000or1:100,000 shouldbeadministeredonlyIVincasesof cardiorespiratoryarrestorprofoundhypotension thatdidnotrespondtovolumeexpansionor multipleIMinjectionsofepinephrine.
Volumeexpansion
Salinesolution Ringer’slactate
Children:5---10mL/kgIVinthefirst5minand 30mL/kginthefirsthour
Adolescents:1---2LrapidlyIV
Infusionrateisregulatedbypulseandblood pressure.
EstablishIVaccesswiththehighestcaliber possible.Monitorvolumeoverload
Oxygen(O2) Undernasalcannulaormask IfO2sat<95%,morethanonedoseofepinephrine
isnecessary
Table2 Secondarymedicationsinthetreatmentofanaphylaxis.
Agent Recommendation
ˇ2-Agonists
Salbutamolsulfate
Inhaledmedications:
Metered-doseinhalerwithaspacer(100 mcg/jet)
Children:50mcg/kg/dose=1jet/2kg; Maximumdose:tenjets
Adolescents:fourtoeightjets,every20min
Nebulizer:Solutionfornebulization:drops (5mg/mL)
Children:0.07---0.15mg/kgevery20minupto threedoses
Adults/Adolescents:2.5---5.0mg,every20min, forthreedoses
Maximumdose:5mg
Bronchospasmreversal
Antihistaminicagents
Promethazine Diphenhydramine
Ranitidine
Children:1mg/kgIVuptoamaximumof50mg
Adolescents:25---50mgIV
Children:1mg/kg
Adolescents:12.5---50mgIVinupto10min
Anti-H1agentsassociatedwithanti-H2maybe moreeffectivethananti-H1alone
Oraldosemaybesufficientformilderepisodes Secondaryrolethathasnotyetbeenwell determined.
Steroids
Methylprednisolone Prednisone
1---2mg/kg/dayIV
0.5---1mg/kg/day,OR,maximum40mg
Dosagestandardizationnotestablished Preventionofbiphasicreactions?
IV,intravenous;IM,intramuscular;OR,oralroute;anti-H1,antihistamineH1;anti-H2,antihistamineH2. AdaptedandmodifiedbyLockeyetal.12
involved food is positive, whether symptoms occur when thisfoodisingestedintheabsenceofphysicalactivity,and whethersymptomsoccurduringexercisewithoutingestion oftheimplicatedfood.10
The subsequent management of severe IgE-mediated foodallergyconsistsmainlyofanexclusiondietforagiven period.Theproposalofanallergen-specificimmunotherapy for food anaphylaxis,especially withbaked milk (as cake orcookies)aimingtopreventanaphylaxis,isstillan exper-imentaltreatmentundergoingevaluation.3,13
Animportantrecommendationtothefamilyofapatient whosufferedsevereanaphylaxisis theneedtocarry self-injectingepinephrine.Thesedevicesareavailableatfixed doses(0.15mgforchildrenupto30kg,0.3mgforolder chil-dren/adolescents)andareindicated,especiallyincasesof highrisk ofantigenic exposure.Unfortunately,the expira-tiondatesforthesedevicesarelimited,theircostishigh, andtheyarenotavailableinBrazilandinothercountries.4 Where self-injectable epinephrine is not available, doses of epinephrine prepared and assembled by the health careprovider according tothepatient’s weight,in insulin syringes, adequately protected from sunlight and well-conditioned, may be offered to the patient and/or appropriately-trainedfamilymembers.A schemethat can besimplyandsafelyusedintramuscularlyisasfollows:up to10kg,0.1mLIM;10---20kg,0.2mLIM;and>20kg,0.3mL IM.Similarly,cautionshouldbetakennottomissthedose whenhandlingthesyringe;patientsshouldbeinformedthat theyshouldbereplacedeverytwotothreemonths,toavoid lossofthedrug’seffectduetoenvironmentalexposure.7,14 Itisimportantthatfamily,teachers,andcommunityleaders
increasingly recognize the early signs and know how to handleanaphylaxiswithself-injectableepinephrineoreven arrangeandpracticetheuseofsyringecontainingthe medi-cation,whenthispresentationisnotavailable(Table3).14,15
Food
protein
induced
enterocolitis
syndrome
(FPIES)
Pathogenesisandassociatedaspects
The pathogenesis of non-IgE mediated food allergies has yet tobe clarified, becauseendoscopies and biopsies are notroutinelyperformed.FPIEShasbeenthemostassessed allergy;severalstudieshavesuggestedakeyroleofT-cells, withsecretionofproinflammatorycytokinesthatmayalter intestinalpermeability.2Although neutrophilia and throm-bocytosis occur in patients with acute FPIES, the role of thesecells inthepathogenicmechanism hasnotyet been established.TheIgEsagainstallergy-causingfoods arenot typicallydetected;however,inasubgroupofchildren,they maybepresentintheacutephaseorduringitsevolution.16 These patients tend to develop a longer course and, in somecases,progresstoIgE-mediatedallergy.2The neuroen-docrinepathwayappearstoplayaroleinthepathogenesis ofFPIES,basedontheefficacyofondansetron,aserotonin antagonistreceptor (5-HT3), in the managementof FPIES acutereaction.17,18
Table3 Preventiverecommendationsforfoodanaphylaxis forfamily,teachers,andcommunityleaders.
Recommendations
-Thefamily,theschoolandthecommunityshould collaboratetopreventpatientexposuretothefood allergen.
-Criteriaandtrainingforearlyrecognitionandmanagement ofsymptomsofprobableanaphylaxisisdesirableand feasibletobecarriedoutinthefamily,school,and community.
-Patientswithaprevioushistoryofanaphylaxisshouldcarry self-injectableepinephrine.
-Incasesofhighriskandnoavailableself-injectable epinephrine,carryingepinephrineinacappedinsulin syringeaftertrainingmaybeavalidconduct.
-Patientwithfood-dependent,exercise-inducedanaphylaxis shouldavoidphysicalactivityfor4haftertheinducerfood, whichiswheat,inmostcases.
-Patientswithfood-dependentexercise-inducedanaphylaxis shouldalsoavoidprecipitatingreactionfactorssuchas alcoholandnon-steroidalantiinflammatorydruguse, especiallyaspirin,wheningestingtheallergenfood. -Patientsatriskforanaphylaxisshouldhaveametalplaque intheirarmoracardidentifyingwhichfoodtheyare allergicto.
particularlyinyounginfantswithamoreseverephenotype (lessthan30%arechildrenolderthanoneyear).Theacute FPIESeventmaybethefirstmanifestationoritmayoccur whenthefoodallergenisintroducedafteraperiodof exclu-sioninpatientswiththechronicform;itwouldbeanepisode ofacuteFPIESoccurringinthechronicformofthedisease. ChronicFPIES shares clinical characteristics with food-induced enteropathy, such as malabsorption syndromes, anemia, diarrhea, and vomiting in children younger than ninemonthsofage;however,inthesepatients,diarrheaisa moreprominentsymptom,butitdoesnotleadtometabolic disturbancesandseveredehydrationasinacuteFPIES.FPIES alsooccursinolderchildrenandadults,duetoexposureto fishor shrimp.Incontrasttofoodprotein-induced procto-colitis,FPIESisrareinexclusivelybreastfedchildren.19
FPIES caused by solid foods typicallyoccurslater than thatcaused by cow’s milkand soy milk,probably related tothetimeoftheirintroductionintothechild’sdiet.Most FPIES patients respondto a singlefood (65---80%), usually cow’smilkorsoy.However,patientswithFPIEScausedby cow’smilk/soymightreacttosolids.IntheUnitedStates, upto50%of patientswithcow’s milk/soyallergyreactto bothfoods,andaboutone-thirdofpatientswithcow’smilk and/orsoyallergyreacttosolids.19
Most children with FPIES to solids respond to several foods; chiefly those with FPIES caused by rice, oats, or barleyhavesymptomsrelatedtoothergrains.Patientswith FPIEStomultiplefoodsarelesscommoninJapan,Australia, and Italy. These differences may reflect specific dietary habitsin each country, and reinforce the hypothesis that earlyintroductionofcow’smilkandsoybeansisariskfactor forFPIEScausedbytheseproteinsandfoodsatolderages.19
DiagnosisofFPIES
The diagnosis of FPIES is based onclinical history, recog-nition of clinical symptoms,exclusion ofother etiologies, and oral challenge test (OCT) under medical supervision. Although the OCT is the gold standard, most patients do notneedtoundergoconfirmation,especiallyiftheyhavea historyofseverereactionsandbecomeasymptomaticafter removalofthesuspectedprotein.However,challengetests are required todetermine FPIES resolution or toconfirm chronicFPIES.20 ThediagnosticcriteriaforFPIESareshown inTable4.
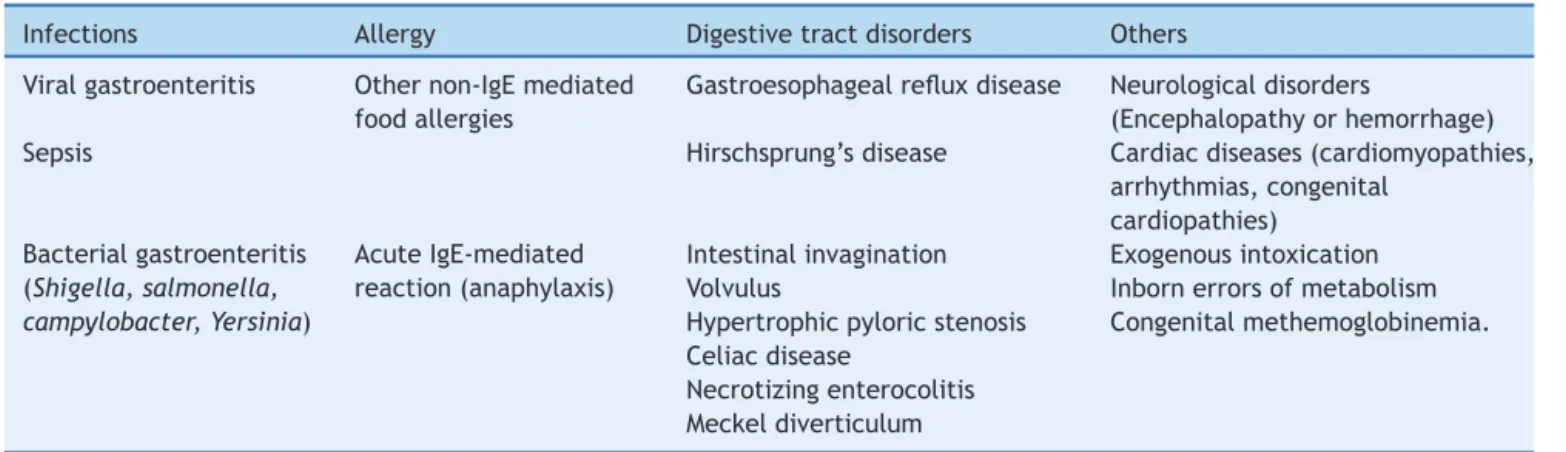
The differential diagnosis of FPIES is extensive and includes infectious diseases, other food allergies, and intestinalobstruction,aswellasneurologicalandmetabolic diseases(Table5).Theinitialepisodesareoftendiagnosed as acute, viral, or septic gastroenteritis, when profound lethargyandhypotensionoccurs,andthereisahigh leuko-cytecountwithaleftshift.Manyotherconditionscanalso be considered in the differential diagnosis, especially in infantswithrepeatedandprolongedepisodesofvomiting. Metabolic disorders arepresent and lead to dehydration, lethargy,aswellasmetabolicacidosis.21
EmergencytreatmentofacuteFPIES
EmergencytreatmentofacuteFPIESisbasedonthreemain points18,19:
1) Hydroelectrolytic resuscitation --- 10---20mL/kg body weightinbolus;
2) Administration of methylprednisolone --- 1mg/kg body weightIV,maximumof60---80mg;
3) OndansetronIVorIM---0.15mg/kgbodyweight.
Aftertheseinitialconducts inthe emergencyunit,the patientshouldremain hospitalized,maintainingthe veno-clysisforhydrationandlossreplacement,monitoringofvital signs(pulse,temperature,capillaryfillingtime,heartrate, andblood pressure).Additionaldosesofondansetron may benecessary,aswellascorrectionsofhydroelectrolytic
dis-Table4 CurrentcriteriausedforthediagnosisofFPIES. 1.Agelessthan2yearsoldonfirstpresentation(frequent butnotmandatory)
2.Exposuretosuspectedfoodstriggersprojectilevomiting, pallor,lethargyin2---4h
Symptomslastafewhoursandresolve,usuallywithin6h Diarrheamaybepresent,lessfrequent,andappearsin 5---10h
3.AbsenceofsymptomsthatsuggestanIgE-mediated reaction
4.Theexclusionfromthedietoftheinvolvedprotein resolvesthesymptoms
5.Re-exposureororalchallengetesttriggerssymptoms within2---4h
Twoexposuresarerequiredtoestablishthedefinitive diagnosiswithouttheneedtoperformthechallengetest
Table5 MainclinicalsituationsinthedifferentialdiagnosisofFPIES.
Infections Allergy Digestivetractdisorders Others Viralgastroenteritis Othernon-IgEmediated
foodallergies
Gastroesophagealrefluxdisease Neurologicaldisorders
(Encephalopathyorhemorrhage) Sepsis Hirschsprung’sdisease Cardiacdiseases(cardiomyopathies,
arrhythmias,congenital cardiopathies)
Bacterialgastroenteritis (Shigella,salmonella, campylobacter,Yersinia)
AcuteIgE-mediated reaction(anaphylaxis)
Intestinalinvagination Exogenousintoxication Volvulus Inbornerrorsofmetabolism Hypertrophicpyloricstenosis Congenitalmethemoglobinemia. Celiacdisease
Necrotizingenterocolitis Meckeldiverticulum
FPIES,foodprotein-inducedenterocolitissyndrome.
orders, basedonlosses. Complementary examsshould be requested:wholebloodcountwithplatelets,ionogram,and gasometry.
Patientguidanceafterhospitaldischarge
The management of non-IgEfood allergyis empiricaldue tothelimitedevidenceandthedivergencesinmanyareas of its pathophysiology. Food protein elimination diet is paramount.InFPIES,exclusivebreastfeedingmustbe pre-served. Protein hydrolysate formulas are generally well tolerated, although approximately 20% of patients may requireaminoacidformulas.20 Follow-upwithaspecialist isindicatedforspecificcare,especiallyfornutritional guid-anceandsymptomcontrolduringandshortlyafterhospital admission.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.CianferoniA, SpergelJM.Foodallergy:review, classification anddiagnosis.AllergolInt.2009;58:457---66.
2.Nowak-WegrzynA,Jarocka-CyrtaE,MoschioneCastroAP.Food protein-inducedenterocolitissyndrome.JInvestigAllergolClin Immunol.2017;27:1---18.
3.SampsonHA.Foodallergy:past,presentand future.Allergol Int.2016;65:363---9.
4.SarinhoE,AntunesA, Pastorino A, Ribeiro M,Porto Neto A, KuschnirFC,etal.Guiapráticodeatualizac¸ão:Departamento de Alergia da SBP. Available from: http://www.sbp.com.br/ src/uploads/2012/12/Alergia-GuiaPratico-Anafilaxia-Final.pdf [accessed08.05.17].
5.UmasuntharT, Leonardi-BeeJ, HodesM, Turner PJ,GoreC, HabibiP,etal.Incidence offatal foodanaphylaxisinpeople withfoodallergy:asystematicreviewandmeta-analysis.Clin ExpAllergy.2013;43:1333---41.
6.SichererSH,SimonsFE.Epinephrineforfirst-aidmanagement ofanaphylaxis.Pediatrics.2017;139:e20164006.
7.Wang J, Sicherer SH. Guidance on completing a writ-ten allergy and anaphylaxis emergency plan. Pediatrics. 2017;139:e20164005.
8.MansoorDK,SharmaHP.Clinicalpresentationsoffoodallergy. PediatrClinNorthAm.2011;58:315---26.
9.Zuberbier T, Aberer W, Asero R, Bindslev-Jensen C, Brzoza Z, Canonica GW, et al. The EAACI/GA(2) LEN/EDF/WAO guidelineforthedefinition,classification,diagnosis,and man-agement ofurticaria: the2013 revisionand update.Allergy. 2014;69:868---87.
10.Feldweg AM. Food-dependent, exercise-induced anaphylaxis: diagnosisandmanagementintheoutpatientsetting.JAllergy ClinImmunolPract.2017;5:283---8.
11.SmithPK,HourihaneJO,LiebermanP.Riskmultipliersforsevere foodanaphylaxis.WorldAllergyOrganJ.2015;8:30.
12.Lockey RF, Kemp SF, Lieberman PL, Sheikh A. Anaphylaxis. In:PawankarR,CanonicaGW,HolgateS,LockeyR,BlaissM, etal.,editors.WorldAllergyOrganization(WAO).Whitebook onallergy.Update2013.Wisconsin:WAO;2013.p.48---53. 13.ValentaR,HochwallnerH,LinhartB,PahrS.Foodallergies:the
basics.Gastroenterology.2015;148,1120---31.e4.
14.PepperAN,Westermann-ClarkE,LockeyRF.Thehighcostof epinephrineautoinjectorsandpossiblealternatives.JAllergy ClinImmunolPract.2017;5,665---8.e1.
15.NIAID-SponsoredExpertPanel,BoyceJA,Assa’adA,BurksAW, JoneSM,SampsonHA,etal.Guidelinesforthediagnosisand management of foodallergy in the UnitedStates: teportof the NIAID-sponsored expert panel. J Allergy Clin Immunol. 2010;126:S1---58.
16.Caubet JC, Ford LS, Sickles L, Järvinen KM, Sicherer SH, Sampson HA, et al. Clinical features and resolutionof food protein-inducedenterocolitissyndrome:10-yearexperience.J AllergyClinImmunol.2014;134:382---9.
17.MiceliSopoS,BattistaA,GrecoM,MonacoS.Ondansetronfor foodprotein.IntArchAllergyImmunol.2014;164:137---9. 18.HolbrookT,KeetCA,Frischmeyer-GuerrerioPA,WoodRA.Useof
ondansetronforfoodprotein-inducedenterocolitissyndrome. JAllergyClinImmunol.2013;132:1219---20.
19.FernandesBN,BoyleRJ,GoreC,SimpsonA,CustovicA.Food protein-inducedenterocolitissyndromecanoccurinadults.J AllergyClinImmunol.2012;130:1199---200.
20.Nowak-W˛egrzynA,ChehadeM,GroetchME,SpergelJM,Wood RA,Allen K,etal.International consensusguidelinesforthe diagnosisandmanagementoffoodprotein-induced enterocol-itissyndrome:executivesummary---workgroupreportofthe Adverse Reactions to Foods Committee, American Academy of Allergy, Asthma & Immunology. J Allergy Clin Immunol. 2017;139:1111---26.