www.jped.com.br
REVIEW
ARTICLE
The
use
of
high-flow
nasal
cannula
in
the
pediatric
emergency
department
夽
Katherine
N.
Slain
a,b,
Steven
L.
Shein
a,b,
Alexandre
T.
Rotta
a,b,∗aUHRainbowBabies&Children’sHospital,DivisionofPediatricCriticalCareMedicine,Cleveland,UnitedStates
bCaseWesternReserveUniversity,SchoolofMedicine,DepartmentofPediatrics,Cleveland,UnitedStates
Received9May2017;accepted6June2017 Availableonline15August2017
KEYWORDS High-flownasal cannula; Children; Emergency department; Bronchiolitis
Abstract
Objectives: Tosummarizethecurrentliteraturedescribinghigh-flownasalcannulausein chil-dren,the components andmechanisms of action ofa high-flow nasal cannula system, the appropriateclinicalapplications,anditsroleinthepediatricemergencydepartment.
Sources: Acomputer-basedsearchofPubMed/MEDLINEandGoogleScholarforliteratureon high-flownasalcannulauseinchildrenwasperformed.
Datasummary: High-flownasalcannula,anon-invasiverespiratorysupportmodality,provides heatedandfullyhumidifiedgasmixturestopatientsviaanasalcannulainterface.High-flow nasalcannulalikelysupportsrespirationthoughreducedinspiratoryresistance,washoutofthe nasopharyngeal deadspace,reduced metabolicworkrelated to gasconditioning, improved airwayconductanceandmucociliaryclearance,andprovisionoflowlevelsofpositiveairway pressure.Mostdata describinghigh-flow nasalcannulauseinchildrenfocusesonthosewith bronchiolitis,althoughhigh-flow nasalcannulahasbeenusedinchildren withother respira-torydiseases.Introductionofhigh-flow nasalcannulaintoclinicalpractice, includinginthe emergencydepartment,hasbeenassociatedwithdecreasedratesofendotrachealintubation. Limitedprospectiveinterventionaldatasuggestthathigh-flownasalcannulamaybesimilarly efficaciousascontinuouspositiveairwaypressureandmoreefficaciousthanstandardoxygen therapyforsomepatients.Patientcharacteristics,suchasimprovedtachycardiaand tachyp-nea, havebeenassociated with alackofprogression toendotracheal intubation.Reported adverseeffectsarerare.
Conclusions: High-flownasal cannula shouldbeconsideredfor pediatric emergency depart-ment patients with respiratory distress not requiring immediate endotracheal intubation;
夽
Pleasecitethisarticleas:SlainKN,SheinSL,RottaAT.Theuseofhigh-flownasalcannulainthepediatricemergencydepartment.J
Pediatr(RioJ).2017;93:36---45.
∗Correspondingauthor.
E-mail:alex.rotta@uhhospitals.org(A.T.Rotta).
http://dx.doi.org/10.1016/j.jped.2017.06.006
0021-7557/©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-ND
prospective,pediatricemergencydepartment-specifictrialsareneededtobetterdetermine responsivepatientpopulations,idealhigh-flownasalcannulasettings,andcomparativeefficacy vs.otherrespiratorysupportmodalities.
©2017SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 4.0/).
PALAVRAS-CHAVE Cânulanasaldealto fluxo;
Crianc¸as; Departamentode emergência; Bronquiolite
Usodecânulanasaldealtofluxonodepartamentodeemergênciapediátrica
Resumo
Objetivos: Resumiraliteratura atualque descreve ouso dacânula nasal de alto fluxoem crianc¸as,os componentes emecanismosde ac¸ão dosistema decânula nasal dealto fluxo, as aplicac¸ões clínicas adequadas e o papel desse sistema no departamentode emergência pediátrico.
Fontes: Realizamosuma pesquisainformatizada naPubMed/MEDLINE e utilizamos oGoogle Acadêmicoparaencontrarliteraturasobreousodacânulanasaldealtofluxoemcrianc¸as.
Resumodosdados: Acânulanasaldealtofluxo,modalidadedesuporterespiratórionão inva-siva,fornecemisturasdegasesaquecidasetotalmenteumidificadasparapacientespormeio deumacânulanasal.Acânulanasaldealtofluxoprovavelmenteauxiliaarespirac¸ãopormeio dareduc¸ãodaresistênciainspiratória,eliminac¸ãodoespac¸omortoanatômiconasofaríngeo, reduc¸ãodotrabalhometabólicorelacionadoaocondicionamentodegás,melhorada condutân-ciadasviasaéreasetransportemucociliarefornecimentodebaixosníveisdepressãopositiva nasviasaéreas.Amaiorpartedosdadosquedescrevemousodacânulanasaldealtofluxoem crianc¸aséfocadaemcrianc¸ascombronquiolite,emboraacânulanasaldealtofluxotenhasido usadaemcrianc¸ascomoutrascausasdedoenc¸asrespiratórias.Aintroduc¸ãodacânulanasalde altofluxonapráticaclínica,incluindoodepartamentodeemergência,foiassociadaàreduc¸ão dosíndicesdeintubac¸ãoendotraqueal.Dadosintervencionistasprospectivoslimitadossugerem queacânulanasaldealtofluxopodesertãoeficazquantoapressãopositivacontínuanasvias aéreasemaiseficazdoqueaoxigenoterapiapadrãoemalgunspacientes.Ascaracterísticas dospacientes,comomelhoradataquicardiaetaquipneia,foramassociadasaumaausênciade progressãoparaintubac¸ãoendotraqueal.Foramrarososefeitosadversosrelatados.
Conclusões: Acânulanasaldealtofluxodeveserconsideradaparapacientesdodepartamento deemergênciapediátricocominsuficiênciarespiratóriaquenãoprecisamdeintubac¸ão endo-traqueal imediata,contudo,sãonecessáriosensaios clínicos prospectivosespecíficospara o departamentodeemergênciapediátricoparadeterminarmelhoraspopulac¸õesdepacientes querespondemaotratamento,asconfigurac¸õesideaisdacânulanasaldealtofluxoeaeficácia comparadaaoutrasmodalidadesdesuporterespiratório.
©2017SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4. 0/).
Introduction
High-flow nasal cannula (HFNC) is a non-invasive respira-torysupportmodalitythatprovidesconditioned(heatedand fullyhumidified)gasmixturestopatientsviaanasalcannula interface.Thereisnouniversallyaccepteddefinitionofthe minimumflowratethatdefines‘‘high’’flow.Inneonates, high-flowmaybedefinedasflowrates≥2L/min,whereas forolderchildren,flowrates≥4---6L/minarecommonly con-sideredhigh.1---3 Overthepastdecade,HFNC systemshave
gained increasedacceptance and arenow widely utilized
tosupportcritically-illpatientsacrosstheentireage
spec-trum,fromprematureneonatestoadults.Ithasalsofound
a role across various hospital sites, including the
neona-talintensivecareunit(NICU),pediatricintensivecareunit
(PICU),medicalandsurgicalintensivecareunits(ICU),
inter-mediate care units, and, more recently, the emergency
department(ED).Arecentrandomizedcontrolledtrialhas
shown that HFNC may be superior to standard low-flow
oxygendeliveryinpreventingtreatmentfailureinchildren
withbronchiolitis,4whileother trialssupportthatHFNCis
equivalentto more traditional modalities of non-invasive
ventilationsupport, suchascontinuousorbi-levelpositive
airwaypressure(CPAPorBiPAP).5,6
Inthisarticle,theauthorsreviewtherationalefor
utiliz-ingHFNCinchildren,thebasicanatomyofaHFNCsystem,
itsmechanismsofaction, clinicalapplication, anditsrole
inthepediatricED.
Rationale
for
using
HFNC
A
B
C
Gas blender
Humidifier
Heater
Cannula Heated circuit
Warm Water flow
Cross-section of tubing
Warm Water return Breathing gas
35 21 37
Figure1 Examplesofcommerciallyavailabledevicestodeliverhigh-flownasalcannula(HFNC)support.PanelA:HFNCsystem assembledfromcommonlyavailablecomponents,includingablender,heater/humidifier,heatedcircuit,andcannula.PanelB:the Airvo2HFNCsystemshownhereasamobileunitwithairandoxygencylinders(top),andacloseupofthedigitalconsoleindicating thesettemperature,flowandoxygenconcentrationoftheinspiredgas(bottom).PanelC:thePrecisionFlowHFNCsystem(top), theinternalhumidificationcartridgeandacutoutshowingthehollow-fiberconfiguration(middle),andacutoutofthecircuitwith adiagramofthewarmwaterinsulation system(bottom).ImagescourtesyofFisher&Paykel HealthcareLimited(AandB)and VapothermInc(C).
storedasadehydratedsubstance.Prolongedadministration ofsupplementaloxygencausesdrynessandirritationofthe mucusmembranesandadverselyaffectsmucociliary clear-ance, unlesshumidification is added.7 It is routinein the
hospitalsetting for a bubble humidifier filledwith sterile
watertobeusedforthispurpose.Thesesimpleand
afford-abledevicesprovidesomelevelofhydrationtodrymedical
gases,butthishumidificationisnotadequateforgasflows
greaterthan 5L/m.7,8 When highergas flowsareutilized,
it is imperative that the gas mixture be fully saturated
withwater vaporand heated closetobody temperature,
astheairway mucosais unabletoindependently transfer
sufficientheatandhumidityatthesesupraphysiologicflow
rates.
The deliveryof high-flowtherapy ispredicated onfour
importantfeatures.
(1) ‘‘Open’’system: gasflowshouldbedeliveredthrough
acannulainterfacethatdoesnotobstructthenostrils.
Thisisakeydistinctioncomparedtopressurizedmodes
of nasal ventilation, such as CPAP and BiPAP. There
should be ample opportunity for gas leakage around
the cannula, and a standard rule is to size the nasal
cannula’s prongs tooccupy no more than 50% of the
cross-sectionalareaofeachnostril.
(2) Conditioned gas:gasmixtures deliveredthroughHFNC
should be properly heated and humidified to prevent
desiccationoftherespiratorymucosa.
(3) Highflows:HFNCshoulddelivergasmixtureflowsthat
aregreaterthanthepatient’speakinspiratoryflow,so
astopreventsignificantentrainmentofambientair
dur-inginspiration.
(4) Highvelocity:gasdeliveredathighvelocitydeeply
pen-etratestheairway,movingthesourceoffreshgascloser
tothe carina andproviding some level of respiratory
support.
Basic
anatomy
of
an
HFNC
system
AlthoughthecompositionofanHFNCsystemvariesamong medicalequipmentmanufacturers,thebasicsetupincludes thesameessentialelements:(1)asourceofpressurized oxy-genandairregulatedbyaflow-meter/blender;(2)asterile waterreservoirattachedtoanefficientheaterhumidifier; (3)aninsulatedand/orheatedcircuitthatmaintains tem-peratureandrelativehumidityoftheconditionedgasasit travelstowardthepatient;and(4)anon-occlusivecannula interface.
An HFNC system can be assembled from items com-monlyusedinrespiratorycareandwidelyavailableinmost units. These systems (Fig. 1A) are composed of a water
reservoir heated by a plate heater,such asthoseused in
mechanical ventilators,ahigh-flowblendertocontrol gas
compositionandflow,andacircuitfittedwithaheatedwire
tomaintain gas temperatureand reduce condensation.In
deliveredthroughcommercialequipmentdesigned
specifi-callyforthispurpose,suchastheAirvo2(Fisher&Paykel
HealthcareLimited,Auckland,NewZealand)(Fig.1B)orthe
PrecisionFlowsystem(VapothermInc.,Exeter,New
Hamp-shire,UnitedStates)(Fig.1C).
TheAirvo2isaversatileHFNCdevice,capableof
deliv-ering a widerange of conditioned gas flows.It comprises
a humidifier chamber resting on a plate heater, a digital
consoleforsetting gasflow(2---60L/min)andtemperature
(31,34,or37◦C),abreathingcircuitwithdualspiralheating
elementsfittedwithanintegratedtemperaturesensor,and
contoured malleable cannulas with soft prongs for added
comfort and size options ranging from small neonates to
adults.Supplemental oxygencan beblended intothe
cir-cuit and regulated throughan external flow meter, while
abuilt-inultrasonicoxygensensoranalyzesthefractionof
inspiredoxygen(FiO2)anddisplaysitonthedigitalconsole.
ThePrecisionFlowisafullyintegrateddevicethatuses
adisposablehigh-efficiencyhollow-fibercartridge
humidifi-cationsystem.Gastransitsthroughthelumenofthehollow
fiberswhileheatedwatervaporisforcedthroughitssmall
particle(0.005m)pores.An intuitivesinglebutton
inter-facecontrolsgastemperature(33---43◦
C,adjustablein1◦
C
increments),FiO2(0.21---1,adjustablein0.01increments),
andgasflow(1---40L/min).Thecartridgedesignedfor
new-borns and infants has an operational flow rangebetween
1and8L/min,while thecartridgeforchildren andadults
operatesbetween5and40L/min;bothareclearedfor
30-days continuous use ona single patient. Conditioned gas
transitsfromthedevicetothecannulainterfacethroughthe
centerlumenofaheatedwater-insulatedtubethat
main-tainsgastemperatureandminimizescondensation.Awide
arrayofcannulasizesfittheentireagespectrum,including
asingleprongcannulatopreventocclusionofthenasal
pas-sagesinsmallneonateswhoalsorequireanasoenterictube.
Mechanisms
of
action
A growing body of evidence indicates that HFNC exerts potentiallybeneficialeffectsthoughseveraldifferent mech-anisms, whichinclude: (1)reduced inspiratoryresistance, (2)washoutofthenasopharyngealanatomicaldeadspace, (3)reducedmetabolicworkrelatedtogasconditioning,(4) improved airway conductance and mucociliary clearance, and(5)provisionoflowlevelsofpositiveairwaypressure.
(1) Reduced inspiratory resistance: The nostrils and the nasalpassagesarethepointsofhighestresistanceinthe humanairway.7,9Theuseofaflowthatmeetsorexceeds
an individual’s inspiratorydemand througha properly
positionednasal cannula helps offset that inspiratory
resistance by effortlessly delivering fresh gas further
down the airway, thus bypassing the area of highest
resistanceanddecreasingtheworkofbreathing.
(2) Washoutofthenasopharyngealanatomicaldeadspace:
During normal breathing, the nasopharynx contains
carbon-dioxiderichgas atthe endof exhalation.This
gasisthenrebreathedduringthenextrespiratorycycle,
which reduces the efficiency of gas exchange. When
an HFNC system is used, the fresh gas rapidly
occu-piesthenasalcavityandpharynx,washingoutcarbon
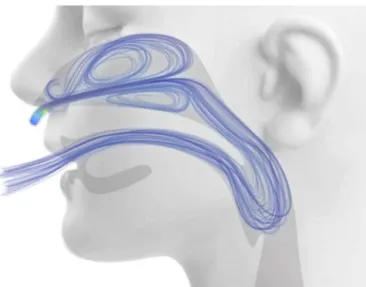
Figure2 Computationalfluiddynamicsmodelingof extratho-racicairwayflushduringhighflownasalcannulasupport.Image courtesyofThomasL.Miller,PhD.
dioxide-rich gas from the nasopharyngeal dead space viatheaforementioned‘‘open’’system(Fig.2).10 This
is equivalent to using the nasopharyngeal anatomical
dead spaceas a reservoir of fresh gas, thus reducing
rebreathingandeffectivelydecreasingthecontribution
oftheanatomicaldeadspacetobreathinginefficiency.
Therefore,apatientsupportedbyHFNCcanemploya
reduced respiratory effort and lower respiratory rate
tomaintainthesamelevelof alveolarventilationand
PaCO2.Thismechanismisparticularlyimportantinsmall
children,consideringthattheextrathoracicanatomical
deadspaceofanewbornisashighas3mL/kganddoes
notapproximatethatofanadult(0.8mL/kg)untilafter
6yearsofage.11
(3) Reduced metabolic work related to gas conditioning:
HFNCsuppliesfullyconditionedgastotheairway,thus
reducinginsensiblewaterlossesandtheenergycostof
heatingtheinspiredgastobodytemperature.10
(4) Improved airway conductance and mucociliary
clear-ance:Inhalationofheatedandhumidifiedgasprevents
desiccationofrespiratorysecretions,7decreases
dysp-neaandthesensation oforopharyngealdryness,12 and
haspotentiallysalutaryeffectsonthemucociliary
appa-ratusfunction.13,14
(5) Provision of low levels of airway pressure: HFNC
cre-ates a low level of positive pharyngeal pressure that
might assist in reducing the dynamic inspiratory
air-wayresistanceandprovidesomedegreeofcontinuous
positive airway pressure.10 The degree of observed
positive airway pressure is directly related to HFNC
flow rate, affected by mouth opening, and
depen-dentonthepressuremeasurementsite.10Threestudies
have used pressures measured in the nasopharynx as
a surrogate for lower positive end-expiration
pres-sures.Milésietal.15 studied21infants<6monthswith
bronchiolitis and found that increasing HFNC to
6---7L/minleads topharyngealpressures thatincrease
to∼6cmH2Oandareweight-dependent,withflowsof
≥2L/kg/minrequiredtoachieveapharyngealpressure
8
6
4
2
0 0 0
–2
3,0 2,5
0 2 1,5 1,0
Gas Flow (L/kg/min)
Pharyngeal Pressure (cm
H2
O)
0,5
Figure3 Relationshipbetweenpharyngealpressureandgas flowduringHFNCsupport.AdaptedfromMilésietal.15
pharyngeal pressuresof ∼3cmH2Oin 25patients with
bronchiolitis on 6---8L/min, and pressures were even
lowerifthesubject’smouthwasopen.Spentzasetal.17
reported nasopharyngeal pressures of 4---5cmH2O in
infants on 8---12L/min and pressures of ∼2cmH2O in
older patients on 20---30L/min. Pressures measured
throughanasopharyngealprobearepotentiallyaffected
by directimpression ofthe inspiredgas jetand likely
overestimatetheactualpressuretransmittedtothe
dis-tal intrathoracic airway, leading other authors touse
anesophagealballooncathetertomeasureesophageal
pressure (Pes).18---20 In one study of 11 infants with
bronchiolitis, end-expiratory Pes was ∼7cmH2O on
8L/min.20 Inanotherstudy of24infantswith
bronchi-olitisorrecoveringfromcardiacsurgery,end-expiratory
Peswas∼4cmH2Oon2L/kg/minandnotsignificantly
differentthanPesmeasuredon2L/minofflow.19
Simi-larly,astudyof25critically-illchildrenwithavarietyof
respiratorydiseasesfoundthatend-expiratoryPeswas
∼5cmH2Oon5---8L/min,only∼1cmhigherthan
mea-surementsobtainedwhileonastandardnasalcannulaat
2L/min.18 Consideredtogether,theavailableevidence
supports thetheorythat HFNC generatesverymodest
increasesinpositiveend-expiratorypressurerelativeto
standard nasalcannula,althoughtheactual amountis
dependentontheHFNC flowandpatientsize.
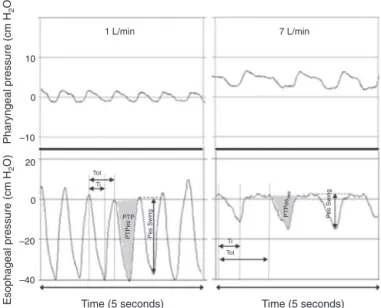
Regard-lessofmechanism,HFNChasbeenshowntosignificantly
reducetheworkofbreathing,mostlybyattenuatingthe
negativeintrathoracicinspiratorypressureasevidenced
byadecreasedesophagealpressureswings(Fig.4)and
electricalactivityofthediaphragm.15,19
Clinical
application
When initiating HFNC therapy, the clinician must control threemainvariables:gastemperature,FiO2,andflowrate. Atour institution, temperatureis typicallyset at approx-imately 1---2◦C below body temperature, and adjusted as
needed for patient comfort. In the authors’ experience, olderchildrenandyoungadultsdescribeanuncomfortable andsomewhatclaustrophobicfeelingwhengastemperature isatorabovebodytemperature,akintowhatisexperienced
1 L/min 7 L/min
10
0
–10
20
0
Tot PTP
Tot
Ti Ti
–20
–40
Time (5 seconds)
Pharyngeal pressure (cm
H2
O)
Esophageal pressure (cm
H2
O)
Time (5 seconds)
Pes Swing
PTPe
s PTPe
s
Pes Swing
Figure 4 Simultaneous recordings of pharyngeal (top) and esophageal(bottom)pressuresfromaninfantreceiving1L/min (left) and 7L/min (right) through a nasal cannula. Although there is a notable increase in pharyngeal pressure during higher flow conditions, virtually no increase is observed in end-expiratory pressure measured atthe thoracic level. The applicationof7L/minflowsignificantlydecreasedthe intratho-racicpressure swingsthroughanattenuationofthenegative inspiratorypressure.AdaptedfromMilésietal.15
while breathinginsideasteam saunaoronaveryhotand
humidsummerday.
HFNC is usually initiated with an FiO2 of 0.6 for the
hypoxemicpatient,providedtherearenophysiologic
con-traindications to the use of these high concentrations of
supplemental oxygen (e.g.,patients recovering from
Nor-woodstageIpalliationforhypoplasticleftheartsyndrome).
FiO2isthenrapidlyadjustedupordownoverthenextfew
minutestoachievethetargetoxygensaturation(SPO2),
typ-ically92%---97%.AlthoughmostpatientstreatedwithHFNC
receiveagasmixtureenrichedwithsupplementaloxygen,
thisisnotnecessarilythecaseforallpatients.Patientswith
respiratorydistresswithouthypoxemiacanstillbenefitfrom
theeffectsofHFNConrespiratorymechanicswhilereceiving
conditionedairwithouttheadditionofoxygen.
Thechoiceofgasflowrateisbasedonpatientsizeand
the perceived magnitude of respiratory support needed.
Ingeneralterms, older/largerpatientsandmoredyspneic
patientswillrequirehigherflows.Thereisnoconsensuson
idealHFNCflows.Someauthorsreportusingage-based
pro-tocols,suchas2L/minforpatients<6months,4L/minfor
6---18 monthsand 8L/min for thoseaged18---24 months21;
or 8---12L/min for infants and 20---30L/min for children.17
Othersreportweight-baseddosing,suchas1L/kg/min22or
2L/kg/min,23 and emergingdata supportthat the effects
of HFNC are dependent on weight.15 Modest support can
beinitiallyprovidedwith0.5---1.0L/kg/min,andincreasing
the flow to up to 1.5---2.0L/kg/min may further
atten-uate intrathoracic pressure swings and reduce the work
of breathing.24 Flows>2L/kg/minmaynotbe additionally
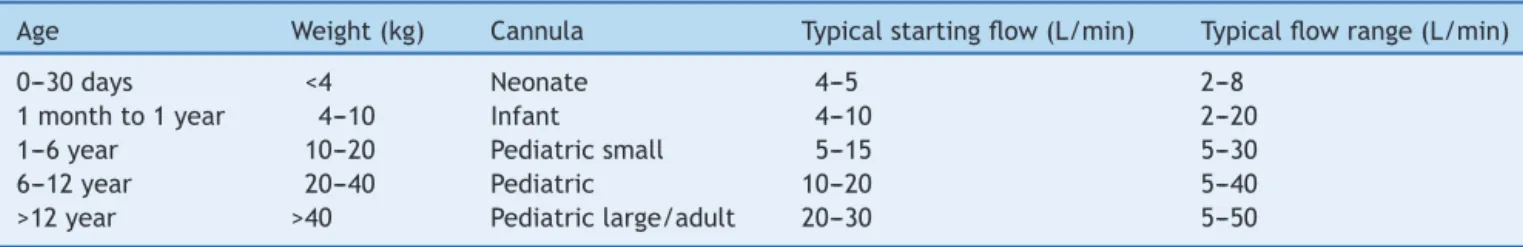
Table1 TypicalstartingflowsforinitiationofHFNCandclinicalflowrangesaccordingtoagegroupandsize.
Age Weight(kg) Cannula Typicalstartingflow(L/min) Typicalflowrange(L/min)
0---30days <4 Neonate 4---5 2---8
1monthto1year 4---10 Infant 4---10 2---20
1---6year 10---20 Pediatricsmall 5---15 5---30
6---12year 20---40 Pediatric 10---20 5---40
>12year >40 Pediatriclarge/adult 20---30 5---50
L,liters;min,minutes.
startedwithflowsof4---5L/min,whileayoungchildstarts with a flow of 5---15L/min (Table 1). Initial flow rates of
50L/min have been used in prospective studies of
criti-callyilladultsandmaybereasonableforadult-sizedPICU
patients.5
HFNC
in
the
pediatric
ED
Considering the success of HFNC in the treatment of critically-illneonates,children,andadults---especiallythe reported reduction in the need for intubation of infants with bronchiolitistreated in the PICU --- the natural next stepforclinicianswastoconsiderearlierinitiationofHFNC in patients while stillin the ED. With its broad range of potentially appropriate patient populations, ease of use, portability,andfavorablepatientsafetyandcomfortprofile, HFNCisrapidlybecominganimportantadjunctmodalityin thetreatmentof acuterespiratoryfailureinthepediatric
ED.25,26 While there is a paucity of robust pediatric
ED-specificdata, theauthorsrecommendconsidering theuse
ofHFNCininfantsandchildrenwithacutehypoxemic
res-piratoryfailurewhoneedsupportbeyondastandardnasal
cannulabutdonotrequireendotrachealintubation.HFNC
may be initiated following a failed trial of regular nasal
cannulaorasaprimaryrespiratorysupportmodality.
TheburgeoningliteraturedescribingHFNCuseinchildren
focusesprimarilyonthosewithbronchiolitis,althoughHFNC
usehasalsobeenreportedinchildrenwithothercausesof
respiratory distress, including pneumonia, asthma, croup,
andotherformsofupperairwayobstruction;neuromuscular
disease;andconvalescencefromcardiacsurgery.25---29
Sev-eralstudieshave evaluatedwhetherintroduction ofHFNC
intoclinical care wasassociated witha reducedneed for
invasive mechanical ventilation. Two small retrospective
studiesof PICUpatientswithmoderate tosevere
bronchi-olitisreportedthat makingHFNCavailable forclinicaluse
wasassociated witha decreased overall need for
intuba-tionandmechanicalventilation.27,30AlargerstudyofPICU
patientswithvariousetiologiesofrespiratorydistress
simi-larlyshowedreducedintubationratesafterintroductionof
HFNC.31 Whilethesestudiesarelimitedbytheir
retrospec-tive design and use of historical controls, similar results
werefound whenHFNC wasimplementedinthepediatric
ED.25Wingetal.studied848childrenwithacuterespiratory
insufficiencyrequiringPICUadmission.25 Overallintubation
rates decreasedfrom15.8% to8.1% (p=0.006)with
intro-ductionofHFNC andestablishmentof aguidelinefor use,
includingadecreasefrom21%to10%(p=0.03)among
chil-drenwithbronchiolitis.25 Theoverall decreasewaslargely
accountedforbyadecreasedintubationrateinthepediatric
ED,from10.5%to2.2%(p<0.001),whileratesofintubation
aftertransfertothePICUremainedsteady.25
Otherstudieshavecomparedintubationratesofchildren
treatedwithHFNCorCPAP.Inoneprospectiverandomized
controlledtrialof PICUpatients youngerthan6monthsof
agewithbronchiolitis,nodifferencewasobserved
regard-ingneedforinvasivemechanicalventilationamongsubjects
treatedwithHFNCat2L/kg/minwhencomparedwiththose
treated with CPAP at 7cmH2O, although HFNC was
asso-ciated with more frequent worsening of dyspnea.32 In a
prospectiverandomized controlledtrial of children under
5 years of age with pneumonia, subjects treated with
HFNChadsimilarratesofclinicaldeterioration,intubation,
anddeathwhencomparedwiththosetreatedwithCPAP.33
Retrospectivestudies of PICU patientswithbronchiolitis22
and varied forms of respiratory failure28 report similar
intubationrates between subjects treated withCPAP and
those receiving HFNC. However, there are no published
prospective interventional trials of pediatric ED patients
specificallydesignedtotestwhetherHFNCreducestheneed
formechanicalventilation,sothesedatashouldbe
gener-alizedtoEDpatientswithcaution.Nevertheless,duetoits
relativesafety,comfortand easeof use,the authors
rec-ommendconsideration of HFNC as a mode of respiratory
supportforchildrenpresentingtotheEDwithmoderateto
severerespiratorydistress.
Withthisstrategy,children whohavenotresponded to
HFNCandrequireahigherlevelofrespiratorysupportmust
be quickly identified. Several small retrospective studies
conducted in the pediatric ED and PICU have sought to
identifydemographicandphysiologicfactorsthatcould
dis-criminatebetweenHFNCsuccessandfailureinchildrenwith
bronchiolitis.23,26,27,34 Predictorsofsuccessincludea
signif-icantdecreaseinheartratefrombaselinewithin60minof
HFNCinitiation,23,27andsimilarlysignificantimprovementin
respiratoryrate27,34(Fig.5).Infantsandchildrenwhofailed
HFNC,variablydefinedasaneedforPICUadmission,or
esca-lationtononinvasiveorinvasiveventilation,wereyounger,26
smaller,34experiencednoimprovementinheartrate23,27or
respiratoryrate34;theywerefoundtobesickerupon
pre-sentation,withworseinitialrespiratoryrate,26 respiratory
acidosis,26,34andseverityofillnessscores.27,34
Forlessillchildren,HFNChasbeencomparedwith
stan-dardnasal cannula(NC). Inone prospectiveobservational
study of pediatric ED patients with bronchiolitis,18
chil-drenweretreatedwithHFNCand18childrenweretreated
withstandardNCbecausenoHFNCsystemwasavailable.35
Although the groups had similar baseline characteristics,
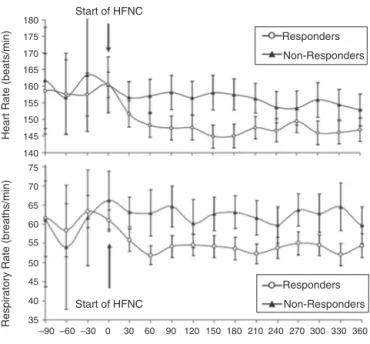
180 175 170 165 160 155 150 145 140 75 70 65 60 55 50 45 40 35 90 Time (minutes) 360 330 300 270 240 210 180 150 120 60 30 0 –30 –60 –90 Responders Non-Responders Responders Non-Responders
Start of HFNC Start of HFNC
Heart Rate (beats/min)
Respiratory Rate (breaths/min)
Figure5 Heartrate(top)andrespiratoryrate(bottom)over timeininfantswithacuteviralbronchiolitis.Anotable reduc-tion in heart rate and respiratory rate at 60min following initiation of HFNC support separates responders from non-respondersinthiscohort.AdaptedfromSchibleretal.27
andshorterdurationofhospitalization.35 Inanother
obser-vationalstudyof94bronchiolitispatientsinitiatedonHFNC
intheED,need forPICUtransferwasfour-foldlowerthan
33contemporarycontrolsreceivingstandardNCtherapy.23
Therehave alsobeenseveralinterventionaltrialsofHFNC
vs.standardNC.Inonestudy,childrenunder18monthsof
ageundergoingextubation followingcardiac surgerywere
randomizedtoHFNC at 2L/kg/minor 2L/minof standard
NC.36 HFNCwasassociated withincreasedPaO
2:FiO2 ratio
and less need for non-invasive positive pressure
ventila-tion,butnodifferenceinPaCO2orre-intubation.36Asmall
prospective pilot study of 19 children with bronchiolitis
foundnodifferenceindurationofoxygentherapyor
hospi-talizationwithHFNCvs.head-boxoxygen.37Inamuchlarger,
open,randomizedcontrolledtrialcomparingHFNCand
stan-dardNCinchildrenwithmoderatebronchiolitisadmittedto
thegeneralward,Kepreotesetal.4alsofoundnodifference
inlengthofhospitalization,durationofoxygentherapy,or
estimatedroomcostsbetweenthetwogroups.However,the
authorsestimatedthepragmatictrialdesign,whichallowed
childreninthestandardNCoxygengroupwhoexperienced
treatmentfailuretoescalatetoHFNC therapywhile
stay-ingonthegeneralcareward,wasultimatelycost-effective.
This is important, given that hospital charges associated
withbronchiolitisarerisingandeffortstowardlimitingcosts
arerecommended.38
A key factor in the cost of HFNC therapy is the
loca-tionin thehospitalin which itis provided.Many hospital
systemsonlyuse HFNC inthe EDand PICU.Other centers
have reported HFNC use on the general wards with
rea-sonablesafetyprofiles.21,23,37,39---41AllowingHFNCuseonthe
generalwardwasassociatedwithdecreasedmedianlength
of hospitalizationand totalhospital chargesin one
retro-spectivestudyofchildrenwithbronchiolitisinitiallytreated
with HFNC in the PICU.21 Reducing hospital costs by
pro-viding HFNC onthegeneral wards must bebalanced with
patient safety concerns, especially given a ∼10% rate of
eventual intubation reportedin several studies ofvarying
patientpopulations.17,21,22,26,27,30,33,34,40
When HFNC is started in the ED, consideration should
also be given tothe availabilityof portable HFNC
equip-ment, soas to avoid the need to interrupt therapy (and
the associated risk of clinical deterioration) while
trans-portingapatientfromtheEDtoaninpatientunit.Although
someofthesepatientsmight toleratethedeliveryof
non-heatednon-humidifiedgasthroughasimplecannulaoreven
interruptionofHFNCdeliveryforashortperiodoftime
dur-ing transport,theauthors prefertodeploy self-contained
portabletransportHFNCdevicesintheEDsothatpatients
can betransportedtothe inpatientsitewithout
interrup-tionsintreatment,whenneeded.
Assessment
of
clinical
response
to
HFNC
As more hospitalsand more sites withinahospital utilize HFNC,itisimperativethatusageguidelinesbedeveloped, includinghow,onwho,andwhentoinitiateHFNC,protocols fortitrationandweaning,frequencyandtypeofserial clin-icalassessment,andcleardefinitionsastowhatconstitutes treatmentfailurewiththeneedtoescalatetootherforms ofnon-invasiveventilation(CPAPorBiPAP)orendotracheal intubation.
Theclinical impactof HFNCis subjectivelyobviousthe patientwithinminutesofitsinitiation,asevidencedbythe reportsofreduceddyspneaandimprovedcomfortexpressed by adult patients and verbalchildren. Standard objective signs of clinical response, such asheart rate, respiratory rate, nasal flaring, accessorymuscle use, and SpO2, used individually or aspart of arespiratory distress score,are often used togauge clinical response to treatment. Sev-eralstudiesshowthatinitiationofHFNCisassociatedwith improvementsinrespiratoryeffortasmeasuredby improve-ments in vital signs, clinical respiratory scores, and gas exchange.17,19,30,35,39---41In theauthors’clinicalexperience,
responders can usually be discerned fromnon-responders
within 60min of initiating HFNC, and often even sooner
than that.Somecentershave attemptedtoasseswork of
breathingina moreobjectivewaythanmeredirect
clini-calobservationbymeasuringintrathoracicpressureswings
during the respiratory cycle througha pressure sensor or
balloon placed in the mid-distal intrathoracic portion of
theesophagus.15,18,24 Whenconsideredinconjunctionwith
thepatient’srespiratoryrate(pressure/rateproduct),
esti-matesofintrathoracicpressuremeasuredintheesophagus
canbeavaluabletooltoevaluateclinicalresponsetoHFNC
andevenhelptitratesupport.15,18,24However,theneedfor
insertion of the esophageal transducer and special
pres-suretransducingequipmentmostlyrelegatesthismonitoring
techniquetouseinresearch.
Patientswhoshownoclinicalimprovementorcontinue
to deteriorate despite initiation of HFNC should be
con-sidered for elective escalation of therapy (i.e., BiPAP or
cardiorespiratorycollapse. Conversely, patients who show
significantclinicalimprovementstillwarrantclose
observa-tionin amonitored environment dueto thecyclic nature
ofmanyrespiratoryconditions(i.e.,bronchiolitis)andthe
possibilitythattheimprovementobservedafterinitiationof
HFNCmightonlybetemporary.
Adverse
events
HFNC is generally safe, provided it is used within its acceptedclinicalparameters.Adverseeventsaregenerally mild, such asepistaxis, skin irritation caused by the can-nulainterface, or aerophagia. Seriousadverse events are extremelyrare,butpneumocephalushasbeenreportedin a premature neonate,42 and cases of pulmonary air leak
(i.e., pneumothorax or pneumomediastinum)43 have been
reportedin older children receiving HFNC support. These
adverse events underscore the importance of delivering
HFNCthroughan‘‘opensystem’’withaproperlysized
non-occlusivecannula thatallowsfor amplegas leakbetween
the prongs and the surrounding nostrils. An open system
ensures that the nasal cannula prongs are non-occlusive,
thus reducingtherisk of suddenincreasesin airway
pres-sureasaresultofinadvertentobstruction.Itis important
tonotethattheincidenceofpulmonaryairleakobservedin
randomizedcontrolledtrialsinvulnerablepretermneonates
wasnotdifferent between patientstreated withHFNC or
nasalCPAP.6Furthermore,theincidenceofskinbreakdown
inpatientstreatedwithHFNC wassignificantlylowerthan
inpatientstreatedwithanasalCPAPinterfacethatrequires
pressureontotheskinsurfacetocreateanocclusiveseal.6
Feeding
patients
on
HFNC
It is notuncommon for patients withrespiratory distress, especially infants with viral bronchiolitis, to have inade-quateoral intakein thehoursor evendaysleading upto theEDvisit.Inaddition,thediscomfortfromhungeroften contributes toa patient’s agitation, which can aggravate respiratory distress. Forthesereasons and thehigh value ofresumingadequatenutrition,considerationisoftengiven astowhetherornotapatientreceivingHFNCcanbefed. AlthoughthisconcernmightnotbepertinenttotheED envi-ronmentininstitutionswherepatientsonHFNCarequickly transitionedtothePICU,delaysindefinitiveplacementof apatientonHFNCmight takemany hoursor evendaysin othercenters.
Although somepractitionersconsiderHFNC usetobea contraindicationfororal feeding,ithasbeen theauthors’ personal experience that adults can swallow liquids and solids without difficulty when subjected to flows as high as40L/min. Thisgroup andothershave shownthat feed-ing selected patients on HFNC can be done safely and with few adverse events.44,45 In this institution, patients
on HFNC who have experienced significant and sustained
clinicalimprovement oftheirrespiratory distressare
gen-erallyfeed,regardlessoftheHFNCflowrate.Theauthors’
practicehasbeentodisregardHFNCasafactorinthe
deci-sion toinitiate enteralfeedsand apply thesame criteria
that wouldbe usedfor anypatient inrespiratory distress
(withorwithoutHFNC):apatientwhohasshownsufficient
improvementofvariousmarkersofrespiratorydistresswill
be tried on enteral feeds regardless of HFNC flow, while
enteralnutritionwillbewithheldfromapatientwho
con-tinuestostruggle andis at risk of requiring escalation of
support and/or aspiration. The authors believe that the
combination of HFNC supportand the comfort of enteral
feeding(for patients who meetthe criteriafor such)can
goalongwaytowardreducingthedistressexperiencedby
infants withacute viralbronchiolitis beingtreated in the
acutein-hospitalsetting.
Conclusion
HFNChasfoundawell-definedroleinthetreatmentof chil-drenwithacutehypoxemicrespiratoryfailure,bridgingthe gapbetweenthedeliveryoflow-flowsupplementaloxygen andtraditionalnon-invasiveventilation(i.e.,CPAP,BiPAP). Consideringitseaseofuse,comfort,andthegrowingbody of clinical evidence supporting its clinical equivalence to othernon-invasiveventilationmodalities,theuseofHFNC isexpectedtocontinuetoexpandbeyondtheconfinesofthe neonatalandpediatricICUs.Retrospectivedataand anec-dotalreportsshowingareductionintheneedforintubation andmechanicalventilationwhenHFNCisinitiatedintheED areencouraging,andmoredefinitivedatafromlarge ran-domizedclinicaltrialsareeagerlyawaitedtodeterminethe exactroleofHFNCinvariouspatientsubsetspresentingto thepediatricEDinrespiratorydistress.46
Conflicts
of
interest
Dr.Rottahasreceivedhonorariaforthedevelopmentof edu-cationalmaterialsandforlecturessponsoredbyVapotherm, Inc.andbyBD/Carefusion.Healsoreceivesroyaltiesfrom Elsevierforeditorialworkonapediatriccriticalcare text-book.Theotherauthorsdeclarenoconflictsofinterest.
References
1.LeeJH,RehderKJ,WillifordL,CheifetzIM,TurnerDA.Useof high flownasal cannulaincriticallyill infants,children, and adults:acriticalreviewoftheliterature.IntensiveCareMed. 2013;39:247---327.
2.Beggs S, WongZH, Kaul S, OgdenKJ, Walters JA. High-flow nasalcannulatherapyforinfantswithbronchiolitis.Cochrane DatabaseSystRev.2014:CD009609.
3.MayfieldS,Jauncey-CookeJ,HoughJL,SchiblerA,GibbonsK, BogossianF.High-flownasalcannulatherapyforrespiratory sup-portinchildren.CochraneDatabaseSystRev.2014:CD009850.
4.KepreotesE,WhiteheadB,AttiaJ,OldmeadowC,CollisonA, SearlesA,etal.High-flowwarmhumidifiedoxygenversus stan-dardlow-flownasalcannulaoxygenformoderatebronchiolitis (HFWHORCT):anopen,phase4,randomisedcontrolledtrial. Lancet.2017;389:930---9.
5.FratJP,ThilleAW,MercatA,GiraultC,RagotS,PerbetS,etal. High-flowoxygenthroughnasalcannulainacutehypoxemic res-piratoryfailure.NEnglJMed.2015;372:2185---96.
7.WardJJ.High-flowoxygenadministrationbynasalcannulafor adultandperinatalpatients.RespirCare.2013;58:98---122.
8.MyersTR,AmericanAssociationforRespiratoryCare.AARC Clin-icalPracticeGuideline:selectionofanoxygendeliverydevice forneonatalandpediatricpatients---2002revision&update. RespirCare.2002;47:707---16.
9.ShepardJWJr,BurgerCD.Nasalandoralflow-volumeloopsin normalsubjectsandpatientswithobstructivesleepapnea.Am RevRespirDis.1990;142:1288---93.
10.Dysart K, Miller TL, Wolfson MR, Shaffer TH. Research in high flow therapy: mechanisms of action. Respir Med. 2009;103:1400---5.
11.NumaAH,NewthCJ.Anatomicdeadspaceininfantsand chil-dren.JApplPhysiol(1985).1996;80:1485---9.
12.RocaO,RieraJ,TorresF,MasclansJR.High-flowoxygentherapy inacuterespiratoryfailure.RespirCare.2010;55:408---13.
13.ReaH,McAuleyS,JayaramL,GarrettJ,HockeyH,StoreyL, etal.Theclinicalutilityoflong-termhumidificationtherapyin chronicairwaydisease.RespirMed.2010;104:525---33.
14.Hasani A, Chapman TH, McCool D, Smith RE, Dilworth JP, AgnewJE. Domiciliary humidificationimproveslung mucocil-iaryclearanceinpatientswithbronchiectasis.ChronRespirDis. 2008;5:81---6.
15.MilesiC,BaleineJ,MateckiS,DurandS,CombesC,NovaisAR, et al. Is treatmentwitha high flow nasal cannulaeffective inacuteviralbronchiolitis?Aphysiologicstudy.IntensiveCare Med.2013;39:1088---94.
16.Arora B, Mahajan P, Zidan MA, Sethuraman U. Nasopharyn-geal airway pressures in bronchiolitis patients treated with high-flow nasalcannulaoxygen therapy.Pediatr EmergCare. 2012;28:1179---84.
17.SpentzasT,MinarikM,PattersAB,VinsonB,StidhamG.Children withrespiratorydistresstreatedwithhigh-flownasalcannula. JIntensiveCareMed.2009;24:323---8.
18.RubinS,GhumanA,DeakersT,KhemaniR,RossP,NewthCJ. Effortofbreathinginchildrenreceivinghigh-flownasalcannula. PediatrCritCareMed.2014;15:1---6.
19.PhamTM,O’MalleyL,MayfieldS,MartinS,SchiblerA.Theeffect ofhighflownasalcannulatherapyontheworkofbreathingin infantswithbronchiolitis.PediatrPulmonol.2015;50:713---20.
20.HoughJL,PhamTM,SchiblerA.Physiologiceffectofhigh-flow nasal cannulain infantswithbronchiolitis.Pediatr Crit Care Med.2014;15:e214---9.
21.RieseJ, FierceJ,Riese A,Alverson BK.Effectofa hospital-widehigh-flownasalcannulaprotocolonclinicaloutcomesand resource utilizationofbronchiolitis patientsadmittedtothe PICU.HospPediatr.2015;5:613---8.
22.MetgeP,GrimaldiC,HassidS,ThomachotL,LoundouA,Martin C,etal.Comparisonofahigh-flowhumidifiednasalcannulato nasalcontinuouspositiveairwaypressureinchildrenwithacute bronchiolitis:experienceinapediatricintensivecareunit.Eur JPediatr.2014;173:953---8.
23.MayfieldS,BogossianF,O’MalleyL,SchiblerA.High-flownasal cannula oxygen therapy for infants with bronchiolitis: pilot study.JPaediatrChildHealth.2014;50:373---8.
24.WeilerTW,KamerkarA, HotzJ,RossPA,NewthCJ,Khemani R.High-flownasalcannulaoffersgreaterreductionofeffortof breathing inchildrenoflowerweight. AmJRespirCritCare Med.2016;193:A6347.
25.Wing R, James C,Maranda LS, ArmsbyCC. Useof high-flow nasalcannulasupportintheemergencydepartmentreducesthe needforintubationinpediatricacuterespiratoryinsufficiency. PediatrEmergCare.2012;28:1117---23.
26.KellyGS,SimonHK,SturmJJ.High-flownasalcannulausein childrenwithrespiratorydistressintheemergencydepartment: predictingtheneedforsubsequentintubation.PediatrEmerg Care.2013;29:888---92.
27.SchiblerA,PhamTM,DunsterKR,FosterK,BarlowA,Gibbons K,etal.Reducedintubationratesforinfantsafterintroduction ofhigh-flownasalprongoxygendelivery.IntensiveCareMed. 2011;37:847---52.
28.tenBrinkF,DukeT,EvansJ.High-flownasalprongoxygen ther-apyornasopharyngealcontinuouspositiveairwaypressurefor childrenwithmoderate-to-severerespiratorydistress?Pediatr CritCareMed.2013;14:e326---31.
29.MikalsenIB,DavisP,OymarK.Highflownasalcannulain chil-dren:aliteraturereview.ScandJTraumaResuscEmergMed. 2016;24:93.
30.McKiernan C, Chua LC, Visintainer PF, Allen H. High flow nasalcannulaetherapyininfantswithbronchiolitis.JPediatr. 2010;156:634---8.
31.KawaguchiA,YasuiY,deCaenA,GarrosD.Theclinicalimpact ofheatedhumidifiedhigh-flownasalcannulaonpediatric res-piratorydistress.PediatrCritCareMed.2017;18:112---9.
32.MilesiC,Essouri S, PouyauR, LietJM,AfanettiM,Portefaix A,etal.Highflownasalcannula(HFNC)versusnasal continu-ouspositiveairwaypressure(nCPAP)fortheinitialrespiratory management of acute viral bronchiolitis in young infants: a multicenterrandomizedcontrolledtrial(TRAMONTANEstudy). IntensiveCareMed.2017;43:209---16.
33.ChistiMJ,SalamMA,SmithJH,AhmedT,PietroniMA,Shahunja KM,etal.Bubblecontinuouspositiveairwaypressurefor chil-drenwithseverepneumoniaandhypoxaemiainBangladesh:an open,randomisedcontrolledtrial.Lancet.2015;386:1057---65.
34.AbboudPA,RothPJ,SkilesCL,StolfiA,RowinME.Predictorsof failureininfantswithviralbronchiolitistreatedwithhigh-flow, high-humidity nasal cannulatherapy. Pediatr Crit Care Med. 2012;13:e343---9.
35.MilaniGP,PlebaniAM,ArturiE,BrusaD,EspositoS,Dell’EraL, etal.Usingahigh-flownasalcannulaprovidedsuperiorresults tolow-flowoxygendeliveryinmoderatetoseverebronchiolitis. ActaPaediatr.2016;105:e368---72.
36.TestaG,IodiceF,RicciZ,VitaleV,DeRazzaF,HaibergerR,etal. Comparativeevaluationofhigh-flownasalcannulaand conven-tionaloxygentherapyinpaediatriccardiacsurgicalpatients:a randomizedcontrolledtrial.InteractCardiovascThoracSurg. 2014;19:456---61.
37.HilliardTN,Archer N,LauraH,HeraghtyJ,CottisH,MillsK, etal.Pilotstudyofvapothermoxygendeliveryinmoderately severebronchiolitis.ArchDisChild.2012;97:182---3.
38.HasegawaK,TsugawaY,BrownDF,MansbachJM,CamargoCA Jr.TrendsinbronchiolitishospitalizationsintheUnitedStates, 2000---2009.Pediatrics.2013;132:28---36.
39.Bressan S, Balzani M,Krauss B, Pettenazzo A, Zanconato S, BaraldiE.High-flownasalcannulaoxygenforbronchiolitisina pediatricward:apilotstudy.EurJPediatr.2013;172:1649---56.
40.KallappaC, Hufton M,Millen G, Ninan TK. Use ofhigh flow nasalcannulaoxygen(HFNCO)ininfantswithbronchiolitisona paediatricward:a3-yearexperience.ArchDisChild.2014;99: 790---1.
41.DavisonM,WatsonM,WocknerL, KinnearF.Paediatric high-flow nasal cannula therapy in children withbronchiolitis: a retrospectivesafetyandefficacystudyinanon-tertiary envi-ronment.EmergMedAustralas.2017;29:198---203.
42.JasinLR,KernS,ThompsonS,WalterC,RoneJM,YohannanMD. Subcutaneousscalpemphysema,pneumo-orbitisand pneumo-cephalusinaneonateonhighhumidityhighflownasalcannula. JPerinatol.2008;28:779---81.
43.HegdeS, Prodhan P. Seriousair leak syndrome complicating high-flownasalcannulatherapy:areportof3cases.Pediatrics. 2013;131:e939---44.
45.SochetAA, McGeeJA,OctoberTW.Oralnutritioninchildren withbronchiolitisonhigh-flownasalcannulaiswelltolerated. HospPediatr.2017;7:249---55.
46.FranklinD,DalzielS,SchlapbachLJ,BablFE,OakleyE,Craig SS,etal.Earlyhighflownasalcannulatherapyinbronchiolitis,