revbrashematolhemoter.2015;37(5):292–295
w w w . r b h h . o r g
Revista
Brasileira
de
Hematologia
e
Hemoterapia
Brazilian
Journal
of
Hematology
and
Hemotherapy
Original
article
Monoclonal
B-cell
lymphocytosis
in
individuals
from
sporadic
(non-familial)
chronic
lymphocytic
leukemia
families
persists
over
time,
but
does
not
progress
to
chronic
B-cell
lymphoproliferative
diseases
Daniel
Mazza
Matos
∗,
Felipe
Magalhães
Furtado,
Roberto
Passetto
Falcão
UniversidadedeSãoPaulo(USP),RibeirãoPreto,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received5March2015 Accepted8May2015 Availableonline30June2015
Keywords:
MonoclonalB-celllymphocytosis Chroniclymphocyticleukemia Flowcytometry
Bcells
First-degreerelatives
a
b
s
t
r
a
c
t
Background:MonoclonalB-celllymphocytosisisclassifiedas‘high-countorclinical’ mono-clonalB-celllymphocytosisand‘low-countorpopulation’monoclonalB-celllymphocytosis. Previously, 167 first-degreerelatives pertaining to sporadic (non-familial)chronic lym-phocyticleukemia familieswerestudied and thepresence ofsevenmonoclonal B-cell lymphocytosisindividualswasreported.
Objective:Theaimofthisreportistodescribetheoutcomesoffiveoftheoriginalmonoclonal B-celllymphocytosisindividuals.
Methods:Flowcytometryanalysiswasperformedonmononuclearcellspreviouslyisolated fromperipheralbloodsamples.Astrategyofsequentialgatingdesignedtoidentifythe populationofCD19+/CD5+B-lymphocyteswasusedand,subsequently,themonoclonal B-celllymphocytosiscellswerecharacterizedbytheCD20weak/CD79bweak/negativephenotype. Results:ThemonoclonalB-celllymphocytosiscloneshowedconsistentstabilityovertime withlittlevariationsinsize.Afteramedianfollow-upof7.6years,noneofthefive mono-clonalB-celllymphocytosisindividualsprogressedtochroniclymphocyticleukemiaorother B-celllymphoproliferativedisease.
Conclusions:Thedataofthisstudysuggestthatchroniclymphocyticleukemia-like mon-oclonal B-cell lymphocytosis detected in the context of sporadic chronic lymphocytic leukemiafamiliesisnotpronetoclinicalevolutionandcouldbejustasignofimmune senescence.
©2015Associac¸ãoBrasileiradeHematologia,HemoterapiaeTerapiaCelular.Published byElsevierEditoraLtda.Allrightsreserved.
∗ Correspondingauthorat:DepartamentodeClínicaMédica,EscoladeMedicinadeRibeirãoPreto,UniversidadedeSãoPaulo(USP),
AvenidaBandeirantes3900,14049-900RibeirãoPreto,SP,Brazil. E-mailaddress:dmazza@usp.br(D.M.Matos).
http://dx.doi.org/10.1016/j.bjhh.2015.05.006
revbrashematolhemoter.2015;37(5):292–295
293
Introduction
MonoclonalB-celllymphocytosis(MBL)isdefinedasthe pres-ence of low levels of circulating abnormal B-cells in the peripheral blood of apparently healthy subjects, identified bymeansofimmunophenotypiccharacterizationperformed byflowcytometry.Phenotypically,MBL presentsaschronic lymphocytic leukemia (CLL)-like MBL, atypical MBL and non-CLL MBL. Moreover, MBL is classified into two cate-gories:‘high-countorclinicalMBL’,inwhichindividualshave absolutelymphocytosis, but with B-cell countslower than 5×109cells/Land‘low-countorpopulationMBL’casesfound
byscreeningindividualswithoutlymphocytosis.1
Notwithstanding the same phenotype, high-count and low-count CLL-like MBL are biologically different entities regarding specific immunoglobulin heavy chain variable (IGHV)genes,thesizeofB-cellcompartment,theprevalence ingeneralpopulationand,mainly,theriskofevolutiontoCLL requiringtreatment.Thus,high-countCLL-likeMBLisreallya pre-malignantconditioncharacterizedbytheriskof progres-siontoovertCLLin1–5%ofcasesperyear.2Ontheotherhand,
themainstudyonlow-countCLL-likeMBLpublishedsofar3
showedthattheconditionpersistsinapproximately90%of subjects,withsomecasesregressingovertime.
Previously,atotalof167first-degreerelativesofsporadic (non-familial)CLLpatientspertainingto42families(sporadic CLL families)were studied bythe current authors and the presenceofsevenMBLindividualsinthisparticular epidemi-ologicalsettingwasreported.4Thus,takingadvantageofthe
previousfindings,thisstudydescribestheoutcomesandthe sizeofB-cellclonesinthisveryparticulargroupofsubjects.
Methods
ThefollowingcriteriawereusedtodiagnoseMBL:(a)a disease-specificimmunophenotypeoranoverallkappa/lambdaratio >3:1or <0.3:1,(b) stablemonoclonalB-cell populationover a three-month period, (c) absence of lymphadenopathy, organomegaly,andautoimmuneorinfectiousdiseases,and (d)B-lymphocytecounts<5×109/L.5
Flow cytometry studies were performed as previously described.4 Briefly, mononuclear cells were isolated from
peripheralbloodsamplesbyFicollHypaque(Sigma–Aldrich,St Louis,MO,USA)densitygradientcentrifugation.Thediluted blood sample(1:1) was carefullylayeredon FicollHypaque (5mL)previouslyaddedtoacentrifugetube.Thesamplewas centrifuged at400×g for 30–40min. Using a clean Pasteur
pipette,themononuclearcellsweretransferredtoaclean cen-trifugetube.Thefinalconcentrationwasadjustedto1.0×106
cellspertube.Antibodiesforthefollowingantigenswereused: CD5(APC),CD19(PerCP-Cy5.5),CD20(FITC),CD79b(PE),anti-
(FITC),anti-(PE),polyclonalanti-(FITC),andpolyclonal anti-(PE).AllmonoclonalantibodieswerepurchasedfromBecton
Dickinson(BD,SanJose,CA,USA)exceptpolyclonalanti-and
anti-(DakoDenmarkA/S,USA).Allsampleswereanalyzed
usingaFACSCaliburflowcytometer(BD,SanJose,CA,USA).A totalof300,000eventspertubewereacquired.
Flowcytometryanalysiswasperformedasfollows:after the identification of the whole lymphocyte population (R1 gate)thesequentialgatingstrategywasdesignedto specif-icallyidentifythepopulationofCD19+/CD5+B-lymphocytes
(R2 gate) and,subsequently, the MBL cells were character-izedfortheCD20weak/CD79bweak/negativephenotype(R3gate)
(Figure1).ThepercentageofMBLcellswascalculatedbased
onthepopulationofCD19+/CD5+B-lymphocytesinperipheral
blood.
Aspreviouslydescribed,MBLwasdetectedinseven first-degreerelativesfromfivefamiliesinatotalof167subjects studied.4 FiveofthesesevenMBLindividualswerefollowed
up. Two individualsrefusedclinical surveillance. Theother fiveindividualswerefollowedupatUniversidadedeSãoPaulo (USP) in Ribeirão Preto with annual medical consultations includinghistory,physicalexamandcompletebloodcount. AllMBLsubjectshadnolymphocytosisatdiagnosisandwere initiallyclassifiedas‘low-countMBL’,althoughthese individ-ualsdidnotcomefromthegeneralpopulation(seeDiscussion section).
Results
Theclinicalandlaboratorialcharacteristicsoftheseven orig-inallydescribedMBLindividualsareshowninTable1.After
1000 10
4
10
3
10
2
10
1
10
0
10
4
10
3
10
2
10
1
10
0
104 103 102 101
100 100 101 102 103 104
800
600
SSC-H
FSC-H CD19 PerCP-Cy5,5 CD20 FITC
CD79b PE
CD5 APC
400
200
0
1000
R2
R3 R1
800 600 400 200 0
Figure1–Gatingstrategy.Leftdot-plot:R1gate(red)representsthetotallymphocytes.Centraldot-plot:R2gate(green) representstheCD19+/CD5+B-lymphocytes.Rightdot-plot:R3gate(red)representstheMBLcells
294
revbrashematolhemoter.2015;37(5):292–295 T able 1 – Clinical and labor a tor ial char acter istics of monoclonal B-cell lymphoc ytosis indi viduals at diagnosis. Name Ag e/g ender Leucoc ytes ( × 10 9/L) Lymphoc ytes ( × 10 9/L) MBL imm unophenotype : ratio Extended phenotyping PCR for IGHV P1 46/F 5.4 1.8 CD5 +/CD20 +bright /CD79b +dim 0.08:1 CD11a +bright /CD23 +/CD38 −/ CD49c − /CD49d +/CD54 +/FMC7 + Monoclonal P2 75/M 5.6 1.7 CD5 +/CD20 +dim /CD79b +dim 0.25:1 CD11a +bright /CD23 +/CD38 −/ CD49c +/CD49d +/CD54 +/FMC7 − Ne g ati v e P3 72/M 4.5 1.3 CD5 +/CD20 +dim /CD79b +dim 1.28:1 CD11a +dim /CD23 +/CD38 +/CD49c +/ CD49d +/CD54 +/FMC7 − Monoclonal P4 53/M 8.1 1.2 CD5 +/CD20 +dim /CD79b +dim 1.12:1 CD11a +dim /CD23 +/CD38 − /CD49c +/ CD49d −/CD54 +/FMC7 − Monoclonal P5 62/M 9.1 1.8 CD5 +/CD20 +dim /CD79b +dim 1.35:1 CD11a +dim /CD23 +/CD38 − /CD49c +/ CD49d −/CD54 +/FMC7 − Monoclonal P6 75/M 5.1 1.1 CD5 +/CD20 +dim /CD79b +dim 4.35:1 Not P erformed Not performed P7 61/F 8.4 4.0 CD5 +/CD20 +dim /CD79b +dim 4.94:1 CD11a +dim /CD23 +/CD38 − /CD49c +/ CD49d −/CD54 +/FMC7 − Ne g ati v e MBL: monoclonal B-cell lymphoc ytosis; PCR: pol ymer ase chain reaction; IGHV : imm uno globulin hea vy chain va ri abl e re g ion g enes; F: female; M: male . 4A
B
P1 P2 P3 P4 P5 3 2% MBL Cells
1
0
2007 2008 2012 2013
Year
2014
Monoclonal
B-c
ell lymphocytosis
cel
ls (%)
Individual
20
07
2008
201
2
201
3
201
4
P1 2.04
2.92 3.01
P2 0.51
0.62 0.86
P3
0.71
0.37
P4
0.53
1.14
0.69
P5
0.64
0.56
0.5
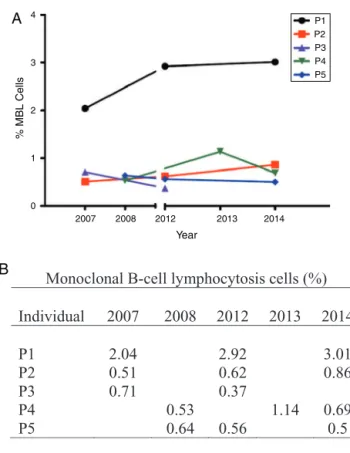
Figure2–(A)MonoclonalB-celllymphocytosisclonesize variation.(B)PercentageofmonoclonalB-cell
lymphocytosiscellsofeachindividual(P1,P2,P3,P4,P5) overtime.
a median follow-up of 7.6 years (range: 6.6–8.1 years) no individualprogressedtoCLLorotherchronicB-cell lympho-proliferativedisease,sinceallofthempersistedwithaB-cell countlowerthan5×109cells/L.
TheMBLcloneshowedconsistentstabilityovertime,with littlevariationsinsize(Figure2).Itisworthnotingthatonly onepatient(P1–Figure2)hadalittleincreaseofclonesize.At diagnosisin2006,thisindividualpresentedwithamonoclonal population(/=0.08:1)characterizedbyanatypicalMBL
phe-notype(CD5+/CD20bright).Atthelastfollow-upin2014,flow
cytometryanalysisshowedthatthemonoclonal+population
persistedwithoutanexpressiveincrease.
Discussion
CLL-likeMBLisclassifiedintotwosubgroups:‘high-countor clinicalMBL’,usuallydiagnosedinaclinicalsetting,and ‘low-countorpopulationMBL’,foundbyscreeninghealthy individ-ualsinthegeneralpopulation.6Itisnoteworthythatourgroup
ofsubjects,fromanepidemiologicalperspective,doesnot per-taineithertoclinicalorpopulationMBL,becausetheycame from specificsporadic(non-familial)CLL families.However, withregardtothesizeoftheabnormalB-cellcompartment, ourgroupissomehowrelatedtolow-countCLL-likeMBL.The resultsofthisstudy recallthoseofFazietal.3 thatshowed
revbrashematolhemoter.2015;37(5):292–295
295
ruralvalleycommunity.Furthermore,theLeedsgroup reeval-uated42MBLcasesdiagnosedinhospitaloutpatientsaftera medianfollow-upof4.3years.Theabsolutelymphocytecount wasnormalin38/42,with4/42developinglymphocytosis,of whichthreewerediagnosedwithhigh-countCLL-likeMBL.2
AsstatedbyGhiaetal.,7probablythemostimportant
ques-tion concerning population MBL is whether, given enough time, all these cases will become clinical MBL and, sub-sequently, every clinical MBL will become overt CLL. This question hasyetmorerelevance withregard toMBL cases diagnosedinsidesporadicCLLfamilies.Infact,thebest epi-demiological data confirmgenetic susceptibility to CLL, as first-degreerelatives ofCLL caseswere foundto beat sig-nificantlyincreasedriskforCLL [relativerisk(RR)=7.5;95% confidenceinterval(95%CI):3.63–15.56].8Thus,thedataofthis
study,thoughlimitedduetosamplesize,butwithamedian follow-upof7.6years,suggestthat‘sporadicCLLfamily-MBL’ isnotpronetoclinicalevolutionandthattheseabnormal B-cellexpansionscouldbejustasignofimmunesenescence. Thus,clonalexpansionsamongsomesubsetsofTcells,as commonlyseenintheelderly,closelyresembleCLL-likeMBL inhealthyindividuals,withthefrequencyofwhichbeing age-related.9,10
Conclusions
CLL-likeMBLdetectedinthecontextofsporadicCLLfamilies isapparentlystableovertime,similartootherlow-countMBL casesdiagnosedinpopulation-screeningsurveys.Thisentity isprobablynotapre-leukemicconditionandcouldjustbea signalofimmunerepertoirerestrictionsoccurringwithagein healthyindividuals.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
TheauthorsthankAglairB.GarciaandDeniseA.P.Gallofor thetechnicalassistance.
r
e
f
e
r
e
n
c
e
s
1.MatosDM,FalcãoRP.MonoclonalB-celllymphocytosis:abrief
reviewforgeneralclinicians.SaoPauloMedJ.
2011;129(3):171–5.
2.RawstronAC.MonoclonalB-celllymphocytosis–whatdoesit
reallymean?CurrHematolMaligRep.2013;8(1):52–9.
3.FaziC,ScarfòL,PecciariniL,CottiniF,DagklisA,JanusA,etal.
Generalpopulationlow-countCLL-likeMBLpersistsover
timewithoutclinicalprogression,althoughcarryingthesame
cytogeneticabnormalitiesofCLL.Blood.2011;118(25):6618–25.
4.MatosDM,IsmaelSJ,ScrideliCA,deOliveiraFM,RegoEM,
FalcãoRP.MonoclonalB-celllymphocytosisinfirst-degree
relativesofpatientswithsporadic(non-familial)chronic
lymphocyticleukaemia.BrJHaematol.2009;147(3):339–46.
5.MartiGE,RawstronAC,GhiaP,HillmenP,HoulstonRS,KayN,
etal.DiagnosticcriteriaformonoclonalB-celllymphocytosis.
BrJHaematol.2005;130(3):325–32.
6.DagklisA,FaziC,SalaC,CantarelliV,ScielzoC,MassacaneR,
etal.Theimmunoglobulingenerepertoireoflow-count
CLL-likeMBLisdifferentfromCLL:diagnosticimplications
forclinicalmonitoring.Blood.2009;114(1):26–32.
7.GhiaP,Caligaris-CappioF.MonoclonalB-celllymphocytosis:
righttrackorredherring?Blood.2012;119(19):4358–62.
8.GoldinLR,CaporasoNE.Familystudiesinchronic
lymphocyticleukaemiaandotherlymphoproliferative
tumours.BrJHaematol.2007;139(5):774–9.
9.VardiA,DagklisA,ScarfòL,JelinekD,NewtonD,BennettF,
etal.ImmunogeneticsshowsthatnotallMBLareequal:the
largertheclone,themoresimilartoCLL.Blood.
2013;121(22):4521–8.
10.GhiaP,MelchersF,RolinkAG.Age-dependentchangesinB
lymphocytedevelopmentinmanandmouse.ExpGerontol.