REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Comparison
of
propofol
and
midazolam
on
patients
undergoing
spinal
surgery
with
intraoperative
wake-up
test:
randomized
clinical
trial
Ozgur
Canbay
a,
Basak
Altiparmak
b,∗,
Nalan
Celebi
a,
Heves
Karagoz
a,
Fatma
Saricaoglu
aaDepartmentofAnesthesiologyandReanimation,HacettepeUniversityFacultyofMedicine,Ankara,Turkey bBigaStateHospital,Canakkale,Turkey
Received27March2013;accepted17October2013 Availableonline11November2013
KEYWORDS Wake-uptest; Propofol; Midazolam; BIS;
Spinesurgery
Abstract
Backgroundandobjectives: Instrumentationincorrectionoperationsforspinaldeformities
car-riesa0.5---5%riskofinjuringthespinalcord.Thewake-uptestisusedforearlydetectionof theseinjuries.Inthisstudywecomparedtheeffectsofpropofolandmidazolamduringwake-up testinscoliosissurgery.
Methods:Thirty patients were randomly assigned as group P andgroup M. Anesthesia was
induced with propofol 2.5mgkg−1 for group P or midazolam 0.5mgkg−1 for group M with
remifentanil0.5gkg−1andcisatracurium0.15mgkg−1forbothgroups.Atthemaintenanceof
anesthesiaO2/airandinfusionsofremifentanilandcisatracuriumwereused.IngroupP,
propo-fol6---10mgkg−1h−1andingroupM,midazolam0.5mgmgkg−1werepreferred.Approximately
15min beforethewake-uptest,alldrugswerediscontinued. Atthewake-uptest, anesthe-siologistasked thepatientstoopentheir eyesandsqueezehis/herhandatevery30s until thepatientsresponded.Thenpatientsweretoldtowiggletheirtoes.Hemodynamic parame-ters,timeofeye-opening,appropriatemovementuponverbalcommandwereevaluated.BIS frequencythroughouttheoperationwasrecorded.
Results:Theeyeopeningtimewas9±2.15miningroupPand7±3.15miningroupM.Motor
movementtimewas12±2.55miningroupPand21.25±3.93miningroupM.
Conclusion:Propofol providedbetterwake-up conditionsandconductedabetterneurologic
assessmentwithinthesameBISvaluesthanmidazolam.
©2013SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:basakugurlu@me.com(B.Altiparmak).
PALAVRAS-CHAVE Testededespertar; Propofol;
Midazolam; BIS;
Cirurgiadecoluna
Comparac¸ãodepropofolemidazolamempacientessubmetidosàcirurgiadecoluna vertebralcomtestededespertarnointraoperatório:estudoclínicorandomizado
Resumo
Justificativaeobjetivos: Ainstrumentac¸ãoemcirurgiasdecorrec¸ãodedeformidadesdacoluna
vertebraltem riscode0,5a5%delesionaramedulaespinhal.Otestededespertaréusado para adetecc¸ão precoce dessaslesões. Neste estudocomparamosos efeitosde propofole midazolamduranteotestededespertaremcirurgiadeescoliose.
Métodos: TrintapacientesforamdesignadosdeformaaleatóriaparaosgruposPeM.Aanestesia
foiinduzidacompropofol(2,5mgkg−1)nogrupoPoumidazolam(0,5mgkg−1)nogrupoM,com
remifentanil (0,5gkg−1) ecisatracúrio (0,15mgkg−1)em ambos os grupos.A manutenc¸ão
daanestesiafoifeitacomO2/areinfusõesderemifentanilecisatracúrio.NosgruposPeM,
respectivamente,dosesdepropofol(6-10mgkg−1h−1)edemidazolam(0,5mgmgkg−1)foram
preferidas.Aproximadamente15minantesdotestededespertar,todososmedicamentosforam interrompidos.Notestededespertar,oanestesiologistapediaaopacientequeabrisseosolhose apertassesuamãoacada30satéqueopacienterespondesse.Depois,opacienteerasolicitado amexerosdedosdospés.Osparâmetroshemodinâmicos,otempodeaberturadosolhoseo movimentoapropriadosobcomandoverbalforamavaliados.AfrequênciadoBISfoiregistrada durantetodaacirurgia.
Resultados: Otempodeaberturadosolhosfoide9±2,15minnogrupoPede7±3,15minno
grupoM.Otempodemovimentomotorfoide12±2,55minnogrupoPede21,25±3,93min nogrupoM.
Conclusão:Propofolproporcionoumelhorescondic¸õesdedespertarepossibilitouumamelhor
avaliac¸ãoneurológicadentrodosmesmosvaloresdoBISquemidazolam.
©2013SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Instrumentationincorrectionoperationsforspinal deformi-tiesasvertebralfusion,congenitalandtraumaticscoliosis, carriesa0.5---5%riskofinjuringthespinalcordduringspinal surgery.1Thesecomplicationsaregenerallyresultsof com-plexfactors such asdirect effects of compression on the spinal cord, distraction,the effects of spinal ischemiaor arterial hypotension.2---4 The intraoperative monitoring of spinal cord function is necessary to prevent these series complications.Thewake-uptestisoneofthemethodsused forearlydetectionandpossiblypreventionofthesespinal cordinjuries5andwasperformedforthefirsttime success-fullybyVauzellaandStagmarain1973.6
Somatosensorial evoked potentials (SSEPs) and motor evokedpotentials (MEPs) aremore recentmethods which giveanideaaboutthespinalcordfunctionsintraoperatively. Butmanyfactorsmayaffectthesekindsofneuromonitoring andyielderroneousresultswhichnecessitatethewake-up testtopreventlong-termcomplications.Awake-uptestis recommendedfor allcases in which thresholdmonitoring changes occur because spinal cord injury may exist even whenmonitoredvariablesreturntobaseline.7
Thepurposeofthewake-uptestistomonitorvoluntary motorfunctionofthelowerlimbsoncethevertebraehave been instrumentedanddistracted. The depth of anesthe-sia is gradually lightened up tothe point where patients are able to respond to verbal commands. As the volun-tary movement oflowerextremities isdemonstrated, the depthofanesthesiais increasedtocompletethesurgery.8 Thatiswhyduringthewake-uptestmonitoring thedepth of anesthesia carries additional importance. BIS values between85and90mayalsosupportsuperficialanesthesiaor
wakefulnessatwhichstagereliableneurologicalassessment canbemade.
Nitrous oxide and halogenated anesthetics are known to have restraining effects on the MEPs from the lower extremities. TIVA (total intravenous anesthesia) has been recommendedinthecorrectionofscoliosisforseveralyears becauseitmayprovide optimalconditionstomonitor the spinalcordfunction reliablywithrapid emergence during thewake-uptest.9,10
Inthisstudyouraimistocomparetheeffectsoftwo dif-ferentintravenous anesthetic agents during wake-up test in patients undergoing scoliosis surgery. Although TIVA is recommended,thereis nostudycomparingthe effectsof propofolandmidazolamtogetherwithremifentanilinfusion duringwake-uptestunderBISmonitoring.
Materials
and
methods
table. Propofol or midazolam would be used as hypnotic agentforgroupsPorMrespectively.Nopreoperative med-icationwasgiven.
In the operating room, following preoxygenation for 3min, anesthesia was induced with propofol 2.5mgkg−1 for group P or midazolam 0.5mgkg−1 for group M with remifentanil 0.5gkg−1 (over 30---60s) and cisatracurium
0.15mgkg−1 for both groups. At the maintenance of anesthesiaO2/air (50%/50%) and infusions of remifentanil 0.025---0.2gkg−1min−1, cisatracurium 1---2gkg−1min−1
were used in both group. In the group P, propo-fol 6---10mgkg−1h−1 and in the group M, midazolam 0.5mgkg−1h−1werepreferredformaintenanceof anesthe-sia.Intraoperativemonitoringconsistedofpulseoximetry, electrocardiogram,invasivearterialbloodpressure,central venouspressure,end-tidalcarbondioxide,nasopharyngeal temperatureandbispectralindex.AdisposableBisSensor (Aspect Medical Systems) was applied to patients’ fore-head prior to induction of anesthesia. Then the patients areplaced in prone position. Anesthesia depth was mon-itored withBIS and hypnoticdoses were titrated tokeep BISfrequencyapproximatelybetween 40and60. To mini-mizebloodloss,controlledhypotensiontomaintainamean bloodpressureof60---70mmHgwasattemptedinallofthe patientswithinfusionofNitroglycerin0.1---4gkg−1min−1.
Themeanarterialpressureandheartratewererecordedat sixdifferenttimesas:beforeinduction,afterinduction,at intubation,beforesurgicalincision,atthebeginningofthe testandattheendofthetest.
Forthewake-uptest, approximately15minbeforethe predicted test time, all the drugs were discontinued. At the time of the wake-up test, anesthesiologist asked the patienttoopen his/hereyesandsqueezehis/herhand at every30suntilthepatientresponded.Thenpatientwastold towigglehis/hertoes.Hemodynamicparameters,timeof eye-opening,appropriatemovementuponverbalcommand wereevaluated.BISfrequencybefore,duringandattheend ofthewake-uptest wererecorded.The wake-uptest was endedaftertheappropriatemotorresponseswereobtained andthepatients werereanesthetizedwithrepeatedbolus propofolormidazolamdosesforgroupsPandMrespectively and anesthesia was maintained with the pretest medi-cations. At the end of the surgical procedure, infusions were stopped and neuromuscular blockage was reversed withneostigmine 0.05mgkg−1. Patients were transported toPACUandextubatedthere. Neurologicexaminationwas performeduponrecovery.Postoperativeanalgesiawas pro-videdby intravenousmorphine PCA withbasalinfusion of 0.1mgkg−1 and bolus of 0.1mgkg−1 with 15min lockout period.Recallandpainduringwake-uptestwerequestioned atthesecondpostoperativedaybyananesthesiologistblind tothestudy.
Mann---Whitney U test was used for the comparison of numericalvalues between groups andChi squaretest for thecomparisonofqualitativedatabetweengroups.
Results
Patientdemographicsweresimilarbetweengroups(p>0.05) (Table1).Throughouttheoperation andduringthe wake-uptestshemodynamicparametersweresimilaringroupP
Table1 Patientandsurgicalcharacteristics.
GroupP GroupM Age(year) 17±7 14±2.6 Gender(F/M) 9/3 9/3 Weight(kg) 49.6±15.3 44.0 Height(cm) 148.5±5 143.4±4 Meanoperationtime(min) 214.1±65.0 284.1±93.9
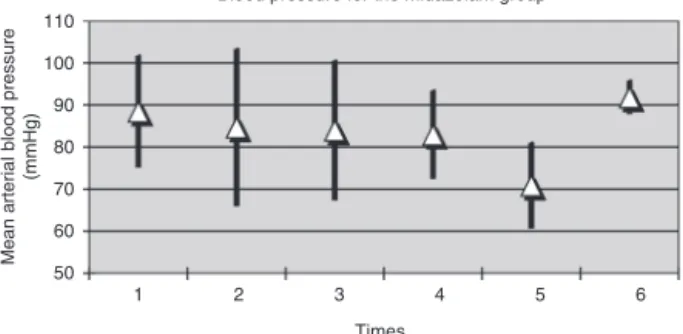
andgroupM.Therewerenosignificantdifferencesatmean arterialpressureandheartrateateachtimepointsbetween groups(Figs.1---4).
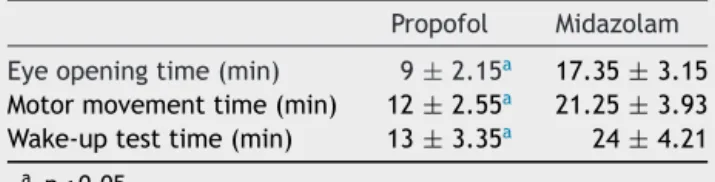
The mean time fromthe start of wake-up test to eye opening and motor movement upon verbalcommand (the wake-uptime)wassignificantlyloweringroupPthangroup M(Table2).
Neurologic deficits were revealed in two patients dur-ingtheirfirstwake-uptestsandthedeficitswerefoundto be reversedin the second wake-up tests performed after looseningofscrews.
Therewasstatisticallysignificantdifferenceforrecallof thewake-uptestbetweenthepropofolandthemidazolam groups(p<0.05).Nineofthepatientsinthepropofolgroup had memory of the wake-up test, but norecall of intra-operative pain whereas no patient had any memory of thewake-uptestinmidazolamgroup.Otherintraoperative
50 55 60 65 70 75 80 85 90 95 100
1 2 3 4 5 6
Mean arterial blood pressure
(mmHg)
Times
Blood pressure for the propofol group
Figure 1 Mean arterialblood pressure values for Propofol Group(Times,1:beforeinduction,2:afterinduction,3:at intu-bation,4:beforesurgicalincision,5:atthebeginningofthetest and6:attheendofthetest)(mean±SD).
50 60 70 80 90 100 110
6 5 4 3 2 1
Mean
ar
ter
ial
blood
pressure
(mmHg)
Times
Blood pressure for the midazolam group
40 60 80 100 120 140
6 5
4 3
2 1
Heart rate (bpm)
Times
Heart rate for propofol group
Figure 3 Heart rate (beat per minute)for Propofol Group (Times, 1:before induction,2: after induction,3: at intuba-tion,4:beforesurgicalincision,5:atthebeginningofthetest and6:attheendofthetest)(mean±SD).
40 60 80 100 120 140
6 5
4 3
2 1
Heart
rate
(
bp
m)
Times
Heart rate for midazolam group
Figure4 Heartrate(beatperminute)forMidazolamGroup (Times,1:beforeinduction,2:afterinduction,3:atintubation, 4:beforesurgicalincision,5:atthebeginningofthetestand 6:attheendofthetest)(mean±SD).
Table2 Meantimeforeyeopening,motormovementand
wake-uptestforpatientsingroupPandgroupM. Propofol Midazolam Eyeopeningtime(min) 9±2.15a 17.35±3.15
Motormovementtime(min) 12±2.55a 21.25
±3.93 Wake-uptesttime(min) 13±3.35a 24±4.21
a p<0.05.
eventsbeforeandafterthewake-uptestswerenotrecalled byanypatientsinneitherofthegroups.
Discussion
Spinalcordinjuryisoneof themostfearedcomplications of scoliosis surgery. Neurologic complications during the repair ofspinal deformitiesmay resultfromcomplex fac-torssuchasdirecteffectofcompressiononthespinalcord, distraction, spinal ischemia or arterial hypotension. Dur-ing‘‘Harringtonrod’’instrumentation andposteriorspinal fusiontocorrectscoliosis,excessivetractiononthespinal cordcan directly lead tovascular spasmor neuropraxia.2 Prevention or early detectionof neurologiccomplications necessitate neuromonitoringwhetherornot theyare sup-portedwithintraoperativearousaltests.
As one of the intraoperative neuromonitoring modali-ties, somatosensorial evoked potentials (SSEPs) show the posterior spinal cord function, but anesthetic agents
(inhaledagents,thiopental,etomidatandnarcotics), hypo-hyperthermia, hypotension, hypoxia, anemia and surgical stimulusdecrease theamplitude of SSEPsand extendthe latentperiod.Meanarterialpressure,particularlydecrease below60mmHg,can resultinsignificant changesin SEPs, which may or may not be indicative of motor deficit.11 Althoughmotorevokedpotentials(MEPs)giveabetter esti-mateofspinalcordfunctionthanSSEPs,theyarealsoknown tohaveadecreasedamplitudewithanesthesia.12 Itis rec-ommendedtoperformwake-uptest evenifmonitoring of theevokedpotentialsreturnstobaselinefollowing interven-tionsuponanysignofdeteriorationofspinalcordfunctions.7 With knownlimitations of these neuromonitoring modali-tiesweusedwake-uptestforallourpatientstodetectany intraoperativespinalcordinjury.
TIVAhasbeen commonlyusedinthecorrection of sco-liosisfor wake-upteststoenablearapidpatientrecovery andan immediateneurologicalexamination.The develop-mentofpropofolandremifentanilasshort-actinginjectable anestheticsprovidesan opportunitytomakean intraoper-ativewake-uptestmorereliable.13Aspropofolhasarapid onsetandrapidemergence,ithasbeencommonlypreferred forshortprocedures.InastudyconductedbyDoganetal., propofolwasusedinelectroconvulsive therapyandinthis study eye opening time wasfound as 7.95±1.27min and timeneededforobeyingcommandswas13.10±1.97min.14 Inourstudy,inthepropofol/remifentanilgroup,eye open-ingtime was9±2.15min and motor movement time was 12±2.55min.Theseresultsareverysimilarwiththestudy conductedby Blussé van Oud-Alblasetal. who compared composite auditory evoked potential index and BIS dur-ing wake-up test.15 In this study, propofol/remifentanil infusionwasusedvia conventionalinfusionpump technol-ogyfor maintenanceofanesthesiaandthewake-uponset was reported as 9.4±2.4min. On the other hand, Grot-tke et al. reported shorter wake-up time than both of thesestudies.Intheirstudy,propofol/remifentanil, propo-fol/sufentanil and desflurane/remifentanil combinations werecompared.16 Inthepropofol/remifentanilgrouptime needed for head elevation was 9.3±2.2min and motion offeet took9.4±2.4min.Although the onsetofwake-up time seems similar in two studies, motor motion time is shorterinthestudyofGrottkeetal.Thedelayinourstudy mayresultfromthecontinuousinfusion ofneuromuscular blockingagentthroughout theoperation.Inanotherstudy conductedbyImanietal.,propofol/remifentaniland propo-fol/alfentanilinfusionswerecomparedforposteriorspinal fusion including wake-up test.17 In propofol/remifentanil group, responding to verbal command was found only 4.1±2minwhereastherewasanextrapreparationperiod (fromdiscontinuation of anesthesiauntil start of sponta-neousventilation)forwake-uptestinthisstudy.
wake-uptimeforpropofolgroupwasshorterthan midazo-lamgroupandpropofol/fentanilinfusionprovidedabetter quality of neurologic assessment during wake-up tests.18 On the other hand, in 2011 Kuruefe et al. conducted a studyinwhichtheycomparedmidazolam/remifentaniland midazolam/alfentanil in 38 patients undergoing scoliosis surgery with intraoperative wake-up test.19 In this study, in the midazolam/remifentanil group wake-up test time was5.8±0.91min and inthe midazolam/alfentanilgroup 5.5±0.68min.Bothresultsaresignificantlyshorterthanour study.Inourstudymidazolamwasinfusedbasedonafixed dose(0.5mgkg−1h−1)until15minbeforethewake-uptest, althoughinthestudybyKuruefeetal.midazolaminfusion wasarrangedin adifferentmanner.Inthisstudy,scoliosis operationwasdividedinto6differentstagesandmidazolam infusionwasdecreasedgraduallyaccordingtothesestages. Differencebetweenthewake-uptesttimesmayresultfrom differentwaysofmidazolaminfusion.
In our study, no patient reported recall of wake-up test in midazolam group, although nine of the patients in propofol group had memory of the wake-up test. This significant difference between groups is probably due to the amnestic effect of midazolam. Likewise in the study of Kuruefe et al., only one patient out of 38 (2.6%) had recall of wake-up test.19 In an other study conducted by McCannetal.,34patientswerepremedicatedwith midazo-lambeforeoperationandallpatientsreceivedintermittent doses of midazolam before the wake-up test.20 The inci-denceofexplicitrecallwasfoundin17.6%(6patients)which wasa smaller incidence than expected based onanother voluntaryadultstudy.21 Inthisstudy McCannetal.stated thatBISin thesetting of acomplex surgicalprocedure in whichvasoactivedrugs wereusedtomodifyhemodynamic responsesandinwhichmovementduringanintraoperative wake-uptestandpostoperativerecallcouldbeusedas dis-creteendpoints.Theydemonstratedasignificantincrease inBISduringtheintraoperativewake-uptest witha small incidenceofexplicitrecall,whichwasindependentof anes-thetictechnique.20 As it is reportedbefore, thedepth of anesthesiaassessment withBIS monitoring providesus an abilitytoinformthesurgeonintimeandtoconductamore reliabletest.22Inourstudyweperformedwake-uptestswith effective results at the BIS values between 80 and 90. It alsohelpedustogivemorespecificinformationtothe sur-geonabout thereliabilityof the test. Withthesefindings wesuggest that especiallyinwake-up test BISmonitoring seems to be more useful than the other clinical signs of wakefulness.
Inourstudytherewasnostatisticaldifferencebetween thehemodynamicstabilityofthegroups.Nitroglycerin infu-sionwasneeded tomaintaincontrolledhypotensionfor 4 patientsingroupPand5patientsingroupM.The continu-ousremifentanilinfusioninbothofthegroupsmayprobably leadtothehemodynamicstabilityineachgroup.
Inconclusion,propofolprovidedbetter wake-up condi-tionsandconductedabetterneurologicassessmentwithin the same BIS values than midazolam. We suggest that using propofol/remifentanil infusion combined with BIS monitorizationfordepthofanesthesiaincreasesthesuccess ofwake-uptest inspinalsurgery.However,itis necessary toconductstudieswithmorecasesandalsotoevaluatethe costs.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.MacEwen GD, Bunnell WP, Sriram K. Acute neurological complications inthe treatmentof scoliosis. A reportof the Scoliosis Research Society. J Bone Joint Surg Am. 1975;57: 404---8.
2.Wilson-Holden TJ, Padberg AM, Lenke LG, Larson BJ, Brid-well KH, Bassett GS. Efficacy of intraoperative monitoring for pediatric patients with spinal cord pathology undergo-ingspinal deformitysurgery.Spine (PhilaPa 1976).1999;24: 1685---92.
3.Nuwer MR, Dawson EG, Carlson LG, Kanim LE, Sherman JE. Somatosensory evoked potential spinal cord monitoring reducesneurologicdeficitsafterscoliosissurgery:resultsofa largemulticentersurvey.ElectroencephalogrClinNeurophysiol. 1995;96:6---11.
4.WilberRG,ThompsonGH,ShafferJW,BrownRH,NashJrCL. Postoperativeneurologicaldeficitsinsegmentalspinal instru-mentation.Astudyusingspinalcordmonitoring.JBoneJoint SurgAm.1984;66:1178---87.
5.AshkenazeD,MudiyamR,Boachie-AdjeiO,GilbertC.Efficacyof spinalcordmonitoringinneuromuscularscoliosis.Spine(Phila Pa1976).1993;18:1627---33.
6.VauzelleC,StagnaraP,JouvinrouxP.Functionalmonitoringof spinalcordactivityduringspinalsurgery.ClinOrthopRelatRes. 1973;93:173---8.
7.NoonanKJ,WalkerT,FeinbergJR,NagelM,DidelotW,Lindseth R.Factorsrelatedtofalse-versustrue-positiveneuromonitoring changesinadolescentidiopathicscoliosissurgery.Spine(Phila Pa1976).2002;27:825---30.
8.DorganJC,AbbottTR,BentleyG.Intra-operativeawakeningto monitorspinalcordfunctionduringscoliosissurgery. Descrip-tionofthetechniqueand reportoffourcases.JBoneJoint SurgBr.1984;66:716---9.
9.OnakaM,YamamotoH,AkatsukaM,MoriH.Continuoustotal intravenous anesthesia is recommended for wake-up test. Masui.1999;48:897---9.
10.YamaguchiK,SumitomoM.Anestheticmanagementwithtotal intravenousanesthesiaforintraoperativewake-uptestin pedi-atricscoliosissurgery.Masui.2010;59:1522---5.
11.Owen JH. Theapplication of intraoperative monitoring dur-ing surgery for spinal deformity. Spine (Phila Pa 1976). 1999;24:2649---62.
12.Kawaguchi M, Furuya H. Motor evoked potentials. Masui. 2006;55:294---301.
13.RussellD,WilkesMP,HunterSC,GlenJB,HuttonP,KennyGN. Manualcomparedwithtarget-controlledinfusionofpropofol. BrJAnaesth.1995;75:562---6.
14.DoganZ,SenogluN,YildizH,etal.Comparisonofenfluraneand propofolinelectroconvulsivetherapy,arandomizedcrossover open preliminary studyon seizure duration and anaesthetic recovery.RevBrasAnestesiol.2011;61:582---90,319---23. 15.BlussevanOud-AlblasHJ,PetersJW,deLeeuwTG,etal.A
com-parisoninadolescentsofcompositeauditoryevokedpotential indexand bispectralindexduringpropofol-remifentanil anes-thesiafor scoliosissurgerywithintraoperativewake-up test. AnesthAnalg.2008;107:1683---8.
17.Imani F, JafarianA, Hassani V, Khan ZH. Propofol-alfentanil vspropofol-remifentanil for posterior spinal fusion including wake-uptest.BrJAnaesth.2006;96:583---6.
18.ErogluA,UzunlarSM,OzenHI.Midazolamversuspropofol anes-thesiaforvertebral columnsurgery withwakeuptests.Turk AnestReanCemMecmuası.1999;27:417---22.
19.KuruefeR,OzcanYAB.Comparisonofremifentaniland alfen-tanil infusions during scoliosis surgery with wake-up test. AnesteziDergisi.2011;19:99---105.
20.McCann ME, Brustowicz RM, Bacsik J, Sullivan L, Auble SG, LaussenPC.Thebispectralindexandexplicitrecallduringthe
intraoperativewake-uptestforscoliosissurgery.AnesthAnalg. 2002;94:1474---8(tableofcontents).
21.Glass PS,Bloom M, Kearse L, RosowC, Sebel P,Manberg P. Bispectralanalysismeasuressedation andmemory effectsof propofol,midazolam,isoflurane,andalfentanilinhealthy vol-unteers.Anesthesiology.1997;86:836---47.