REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
Official Publication of the Brazilian Society of Anesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Reducing
sore
throat
following
laryngeal
mask
airway
insertion:
comparing
lidocaine
gel,
saline,
and
washing
mouth
with
the
control
group
Mehryar
Taghavi
Gilani
a,
Iman
Miri
Soleimani
a,
Majid
Razavi
a,∗,
Maryam
Salehi
baCardiacAnesthesiaResearchCenter,Imam-RezaHospital,SchoolofMedicine,
MashhadUniversityofMedicalScience,Mashhad,Iran
bSocialMedicineDepartment,SchoolofMedicine,MashhadUniversityofMedicalScience,Mashhad,Iran
Received19June2013;accepted11July2013 Availableonline26October2013
KEYWORDS
Sorethroat; Laryngealmask airway; Lidocaine; Washingmouth; Saline
Abstract
Background: Laryngealmaskairwayisstillaccompaniedbycomplicationssuchassorethroat. Inthisstudy,effectsofthreemethods ofreducingpostoperativesorethroatwerecompared withthecontrolgroup.
Methods:240patients withASAI, IIcandidates forcataractsurgerywererandomlydivided intofoursamegroups.Nosupplementarymethodwasusedinthecontrolgroup.Inthesecond, thirdandfourthgroups,lidocainegel,washingcuffbeforeinsertion,andwashingmouthbefore removinglaryngealmaskairwaywereapplied,respectively.Anesthesiainductionwasdonewith fentanyl,atracurium,andpropofolandmaintainedwithpropofolinfusion.Theincidenceofsore throatwasevaluatedduringtherecovery,3---4hlaterandafter24husingverbalanalogscale. Thedatawereanalyzedbyt-test,analysisofvarianceandchi-squareusingSPSSV11.5.
Results:Age,gender,durationofsurgeryandcuffpressurewerethesameinallthefourgroups. Incidenceofsorethroatatrecoveryroomwashighestinthecontrolgroup(43.3%)andlowest inthewashingmouthgroup(25%).However,nosignificantstatisticaldifferencewasobserved betweenthesefour groups(recovery,p=0.30;discharge,p=0.31;examination,p=0.52).In thisstudy,increaseddurationofoperationhadasignificantrelationshipwiththeincidenceof sorethroat(p=0.041).
Conclusion:Sorethroatisacommonpostoperativeproblem,butnospecialmethodhasbeen foundcompletelyefficientyet.Inthisstudy,cuffwashing,lidocainegel,andmouthwashing beforeremovinglaryngealmaskairwaywerenothelpfulforsorethroat.
©2013SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:razavim@mums.ac.ir(M.Razavi).
0104-0014/$–seefrontmatter©2013SociedadeBrasileiradeAnestesiologia.PublishedbyElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Dordegarganta; Máscaralaríngea; Lidocaina; Lavagemdaboca; Salina
Reduc¸ãodadordegargantaapósainserc¸ãodemáscaralaríngea:comparac¸ãodegel delidocaína,salinaelavagemdabocacomogrupocontrole
Resumo
Justificativa: Amáscaralaríngeaaindaérelacionadaacomplicac¸õescomoadordegarganta. Neste estudo, os efeitosde três métodos para reduzir ador de garganta, no período pós-operatório,foramcomparadoscomogrupocontrole.
Métodos: Duzentose quarenta candidatos,comestadofísico ASA I-II, foramaleatoriamente divididosemquatrogruposiguaisparaacirurgiadecatarata.comestadofísicoASAI-II, can-didatos paraacirurgia decatarataforamaleatoriamentedivididosem quatrogruposiguais. Nenhummétodocomplementarfoiusadonogrupocontrole.Nosegundo,terceiroequarto gru-pos,osmétodosutilizadosforam:Aplicac¸ãodegeldelidocaína,lavagemdomanguitoantesda inserc¸ãoelavagemdabocaantesderemoveramáscaralaríngea,respectivamente.Aanestesia foiinduzidacomfentanil,atracúrioepropofolemantidacompropofol.Aincidênciadedorde gargantafoiavaliadadurantearecuperac¸ão,3-4hdepoiseapós24husandoumaescalaverbal analógica. Teste-t,análisedevariânciaetestedoqui-quadradoforamusadosparaaanálise dosdadospormeiodoprogramaestatísticoSPSSV11.5.
Resultados: Idade,gênero,tempo decirurgiaepressãodomanguitoforamsemelhantesem todososquatrogrupos.Nasaladerecuperac¸ão,aincidênciadedordegargantafoimaiorno grupocontrole(43,3%)emaisbaixanogrupolavagemdaboca(25%).Noentanto,nãohouve diferenc¸a estatisticamente significanteentre os quatro grupos (recuperac¸ão, p=0,30; alta,
p=0,31; exame,p=0,52).Neste estudo,otempomaislongodecirurgiaapresentourelac¸ão significativacomaincidênciadedordegarganta(p=0,041).
Conclusão:Dordegargantaéum problemapós-operatóriocomum,masnenhummétodoem especialfoiconsideradototalmenteeficiente.Nesteestudo,alavagemdomanguito,aaplicac¸ão degeldelidocaínaealavagemdebocaantesderemoveramáscaralaríngeanãoforamúteis paraevitaradordegarganta.
©2013SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Although anesthesiologists frequently use laryngeal mask airway because of its easy insertion and fewer complications,itisstillassociatedwithcomplicationssuch as sore throat, which sometimes reduce patients’ satis-faction and limit post-discharge activities. Occasionally, sorethroatpresentsasdysphonia,dysphagia,andmucosal dryness.Sorethroatismorecommonaftertracheal intuba-tion;however,somestudieshavereportedequalincidence ratesof sorethroatfollowing laryngealmask andtracheal intubation.1 This complication has evenbeen reportedin
patients ventilated by mask.2 Incidence of sore throatin
laryngeal mask airways has been reported from 5.8% to
34%.3---5
Physical damagehas been mentioned asthe main
rea-sonofsorethroatandvariousmethodshavebeenproposed
forreducingsorethroatfollowingtheuseoflaryngealmask
airways.Assumingthatphysicaltraumaduringinsertionof
laryngeal mask airways causes pressureonsalivary glands
leadingtodecreasedsalivaproductionandsorethroat,we
washed patients’ mouths with 20mL saline before
laryn-geal mask airway removaland comparedthe results with
othermethodssuchasapplyinglidocaineandsalinebefore
insertionandthecontrolgroup.
Methods
Aftertheapprovalof theDeputyfor ResearchofMashhad
UniversityofMedicalSciences,thisstudywasconductedin
OphthalmologyHospital on240 patientswithASAI---II who
hadundergonecataractsurgery.Thisstudywasprospective,
randomized, anddouble-blind. Exclusioncriteria included
ageunder15,addiction,obesity,severeasthmaorchronic
obstructive pulmonary disease, failure of laryngeal mask
airwayinsertion, sensitivity tolidocaine, sore throatand
commoncoldsymptoms.
Aftervenouscatheterizationandinjectionof5mL/kgof
saline,1g/kgfentanyl,0.2mg/kgatracurium,and2mg/kg
propofolwereusedforinductionofanesthesia.After2min,
laryngeal mask airways were inserted. Patientswere
ran-domlydividedintofourgroups,eachwith60patients,using
randomizedblock method.Inthecontrol group,laryngeal
mask airway wasinserted without lubricants. In the
lido-cainegroup,lidocainegelwasused,andinthesalinegroup,
laryngealmaskairwaywaswashedwithsalinebefore
inser-tion.In the fourth group, patients’ mouths were washed
with20mLofsalinebeforelaryngealmaskairwayremoval.
Laryngealmaskairways wereinserted bythesameperson
using90-degreerotationmethodandsemi-fullcuff.Inthis
method,laryngealmaskairwayisenteredfromtherightside
ofthemouth and,after passingthe tongue,it isrotated.
Then,thecuffwasfilledwithair,basedonthesize(20cm3
forno.3and30cm3forno.4)andcuffpressurewas
mea-sured.Anesthesiawasmaintainedwith100---150g/kg/min
propofoland50%O2andN2O.Attheendofthesurgery,after
returnofbreath, neostigmineandatropine wereinjected
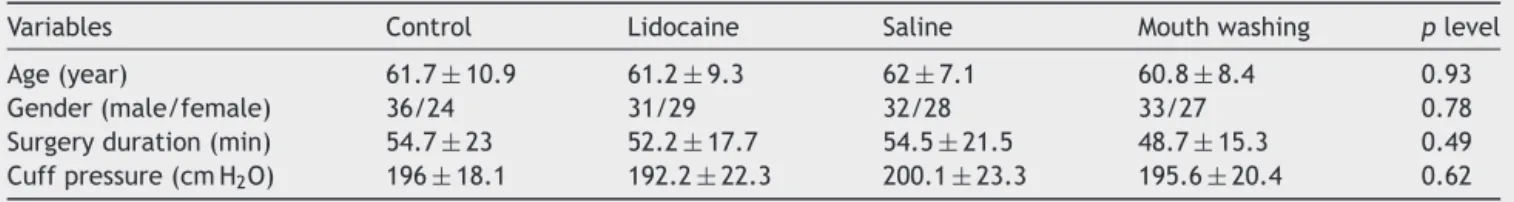
Table1 Demographicinformation,cuffpressure,andsurgeryduration.Mean±SD.
Variables Control Lidocaine Saline Mouthwashing plevel
Age(year) 61.7±10.9 61.2±9.3 62±7.1 60.8±8.4 0.93
Gender(male/female) 36/24 31/29 32/28 33/27 0.78
Surgeryduration(min) 54.7±23 52.2±17.7 54.5±21.5 48.7±15.3 0.49 Cuffpressure(cmH2O) 196±18.1 192.2±22.3 200.1±23.3 195.6±20.4 0.62
Table2 Incidenceofsorethroatduringrecovery(VAS=verbalanalogscale),N(%).
Variables Control Lidocaine Saline Mouthwashing
Withoutpain 34(56.7) 39(65) 39(65) 45(75)
VAS≤4 17(28.3) 13(21.7) 14(23.3) 8(13.3)
4<VAS≤7 9(15) 8(13.3) 7(11.7) 7(11.7)
Table3 Incidenceofsorethroatbeforedischarge(VAS=verbalanalogscale),N(%).
Variables Control Lidocaine Saline Mouthwashing
Withoutpain 36(60) 40(66.7) 41(68.4) 46(76.7)
VAS≤4 16(26.7) 13(21.7) 11(18.3) 8(13.3)
4<VAS≤7 8(13.3) 7(11.6) 8(13.3) 6(10)
During recovery, before discharge (around 3---4h) and nextexamination(24hlater),incidenceandseverityofsore throatwere evaluated in patients by verbal analog scale (VAS).Then,theyweredividedtofourcategories(nopain, score≤4,4<score≤7andscore>7).Whenscorewashigher than7,intramuscularopioidwasinjectedandthe patient wasdischargedlater.If scorewasless than7, we recom-mendedoralanalgesic(suchasacetaminophen500mg)and mouthwashing withsalineifneeded afterdischarge. The personwhoevaluatedsorethroatinrecoveryandbefore dis-chargefromthehospitalwasnotawareofpatients’group assignmentinthestudy.Becauseoftheoutpatientnatureof thesurgeryanduseoforalanalgesicsafterdischarge,sore throatevaluationwasdifficultafterdischargefromhospital. The gathered data were analyzed using SPSS V11.5. Parametricdatawithnormalvariationwereanalyzedwith analysisofvarianceandt-test.Non-parametricresultswere comparedby Mann---Whitneyand Kruskal---Wallistests and nominaldatawithchi-squaretest.p<0.05wereconsidered significant.
Results
Demographicinformationsuchasage,genderandtheother information like surgery duration and cuff pressure after fillingareshowninTable1.Therewasnostatistically
sig-nificant differencebetween these parameters in thefour
groups.
Sore throat was most common in the control group
(43.3%)andleastcommoninthemouthwashinggroup(25%).
Incidenceofsorethroatinthelidocaineandsalinegroups
wasthe same(35%). Nostatisticallysignificant difference
wasobservedbetween fourgroups for sorethroat(during
recovery p=0.30; during discharge p=0.31). Incidence of
sorethroatduringrecoveryandbeforedischargewasnot
dif-ferentsignificantly.Sincepainscorewasnotmorethan7,no
patientstookopioidanalgesic.Incidenceofsorethroat
dur-ingrecoveryandbeforedischargeisshowninTables2and3.
Only2patientsincontrolandsalinegrouphadpainafter24h
withscorelessthan4(p=0.52).
Therewasnocorrelationbetweenage,gender,andcuff
pressurewithsorethroat.Therewasasignificant
relation-shipbetween meansurgicaltimeandsorethroat(nopain
48.1±17.1minvs.withpain58.7±21.2min)(p=0.041).
Discussion
Sorethroatisoneofthemostcommonpostoperative
com-plaints,whichfollowstrachealintubation,useoflaryngeal
mask airway, oral airway insertion, andeven mask
venti-lation.Incidence of sore throatcaused bylaryngeal mask
airwayhasbeenreportedtoberelatedtoinsertionmethod
and techniques, users’experience,laryngeal mask airway
size,and cuffpressure.In thepresent work,incidence of
sorethroatrangedfrom25%inthemouthwashinggroupto
43.3% inthecontrol group;however,nosignificant
differ-encewasobservedbetweenthegroups.
Nospecialmedicationorprocedurehasbeencompletely
useful for pain control. For reducing of physical trauma,
various insertion methods such as classic method,
rota-tionmethod,andjawthrustmethodhavebeenutilized.6---8
contradictory results.12---14 In addition, various compounds
and methods have been used for reducing sore throat,
including lidocaine gel,9 benzydamine hydrochloride,10
washing laryngeal mask airway, local and systematic
steroids,11etc.
Multiple techniques are usedfor insertion of laryngeal
maskairways.Theclassicmethodisdonebyputtinga
fin-ger inthe patient’s mouth inordertofacilitate laryngeal
mask airwaypassage.However,somespecialistsuseother
methodslike180-degreerotationoflaryngealmaskairway
to avoid passing finger through the patient’s mouth.8 In
thisstudy,90-degree rotationmethodwasused;however,
no comparison wasmade between this method and
clas-sic methodfor laryngeal mask airwayinsertion. In classic
method,the cuffshould beevacuated, but insome
stud-ies,fullandsemi-fullcuffs havebeen comparedwiththis
method.1Therewaslessbloodinthemethodwithfullcuff
thaninclassictechnique(0%vs.15.3%)andsorethroatwas
remarkablylessprevalent(4.1%vs.21.4%).Weuseda
semi-fullcuff,i.e.thecuffwasfilledandthenitwasdrainedto
barometricpressure.
Studyoftherelationshipbetweencuffpressureand
inci-denceofsorethroathasproducedcontradictoryresultsin
differentreports.Inonestudy,highandlowpressuresofcuff
werecomparedandnosignificantdifferencewasobservedin
theincidenceofsorethroat(40%and50%,respectively).12
The investigation by Brimacombe etal. showed thathigh
cuff pressure increased dysphagia and sore throat.13 In
another study, however, maintenance of cuff pressure at
lessthan60cmH2Oreducedsorethroatrateby5.8%.14 In
ourstudy,thecuffwasfilledwithstandardvolumeandcuff
pressure was measured and no significant difference was
observed for cuff pressure between thegroups (p=0.62).
Norelationshipwasfoundbetween cuffpressureandsore
throat; it is notable however that the cuff pressure was
high.
Using lubricants has been widely studied in inserting
laryngealmaskairways.InastudybyKelleretal.,lidocaine
gelwascomparedtosaline anditwasdemonstrated that
lidocaine increased complications by 2%.14 Benzydamine
hydrochloride spray has also reduced postoperative sore
throat(from34%to4%).10Patternofventilationofpatients
(spontaneousormechanical)andinductiondrugshavebeen
considered tohave a roleinincidenceof sorethroat.15---17
Muscle relaxantshave shown noimpact onincidence and
intensity of throatproblems.18 In ourinvestigation, there
was no significant difference between lidocaine, saline,
mouthwashing,andcontrolgroups.
Conclusion
Inthisstudy,fourmethodsofusingcuffwithoutlubricants,
usinglidocainegel,usingsaline,andmouthwashingbefore
removing laryngealmask airwayswerecomparedfor their
impactontheincidenceof sorethroatfollowinglaryngeal
maskairwayinsertion.Theincidenceofsorethroatwasmost
commoninthecontrolgroup(43/3%)andleastinthemouth
washinggroup(25%),butnostatisticallysignificant
differ-ence was obtained. High incidence of sore throat in this
work might bedue to inadequate experienceof the user
(anesthesiaresidentwith1.5yearsofexperience),highcuff
pressure,orthe90-degreerotationmethod.Thelimitations
ofthisstudycanbeearlydischargeofpatients,uncontrolled
consumption oftranquilizers andlack of longer
investiga-tion.
Authorship
contribution
Mehryar Taghavi Gilani contributed towards the
concep-tion and design and for the data acquisition. Iman Miri
Soleimanicontributedtowards theresearchand data
col-lection.MajidRazavicontributedtowardstherevisionand
thefinalapproval.MaryamSalehicontributedtowardsthe
methodologyandthedataanalysis.
Funding
Deputy for Research of Mashhad University of Medical
Sciences.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.WakelingHG,ButlerPJ,BaxterPJ.Thelaryngealmaskairway: acomparisonbetweentwoinsertiontechniques.AnesthAnalg. 1997;85:687---90.
2.McHardyFE,ChungF.Postoperativesorethroat:cause, preven-tionandtreatment.Anaesthesia.1999;54:444---53.
3.HigginsPP,ChungF,MezeiG.Postoperativesorethroat after ambulatorysurgery.BrJAnaesth.2002;88:582---4.
4.JoshiGP,InagakiY,WhitePF,etal.Useofthelaryngealmask airwayasanalternativetothetrachealtubeduringambulatory anesthesia.AnesthAnalg.1997;85:573---7.
5.DingleyJ,WhiteheadMJ,WarehamK.Acomparativestudyof theincidenceofsore throatwiththelaryngeal maskairway. Anaesthesia.1994;49:251---4.
6.Krishna HM,KamathS, ShenoyL. Insertion ofLMA ClassicTM
with and without digital intraoral manipulation in anes-thetizedunparalyzedpatients.JAnaesthesiolClinPharmacol. 2012;28:481---5.
7.ChooCY,KoayCK,YoongCS.Arandomisedcontrolledtrial com-paringtwoinsertiontechniquesfortheLaryngealMaskAirway FlexibleTMinpatientsundergoingdentalsurgery.Anaesthesia.
2012;67:986---90.
8.KoayCK, YoongCS, KokP.Arandomizedtrialcomparingtwo laryngealmaskairwayinsertiontechniques.AnaesthIntensive Care.2001;29:613---5.
9.HungNK,WuCT,ChanSM,etal.Effectonpostoperativesore throatofsprayingtheendotrachealtubecuffwithbenzydamine hydrochloride,10%lidocaine,and2%lidocaine.AnesthAnalg. 2010;111:882---6.
10.KatiI,TekinM,SilayE,etal.Doesbenzydaminehydrochloride appliedpreemptivelyreducesorethroatduetolaryngealmask airway?AnesthAnalg.2004;99:710---2.
11.SumathiPA,ShenoyT,Ambareesha M,etal.Controlled com-parisonbetweenbetamethasonegelandlidocainejellyapplied overtrachealtubetoreducepostoperativesorethroat,cough, andhoarsenessofvoice.BrJAnaesth.2008;100:215---8.
13.BrimacombeJ,HolyoakeL,KellerC,etal.Pharyngolaryngeal, neck,andjawdiscomfortafteranesthesiawiththefacemask andlaryngealmaskairwayathighandlowcuffvolumesinmales andfemales.Anesthesiology.2000;93:26---31.
14.KellerC,SparrHJ,BrimacombeJR.Laryngealmaskairway lubri-cation.Acomparativestudyofsalineversus2%lignocainegel withcuffpressurecontrol.Anaesthesia.1997;52:592---7.
15.Figueredo E, Vivar-Diago M, Mu˜noz-Blanco F. Laryngo-pharyngealcomplaintsafteruseofthelaryngealmaskairway. CanJAnaesth.1999;46:220---5.
16.ChiaYY,LeeSW,LiuK.Propofolcauseslesspostoperative pha-ryngealmorbiditythanthiopentalaftertheuseofalaryngeal maskairway.AnesthAnalg.2008;106:123---6.
17.KellerC,BrimacombeJ.Spontaneousversuscontrolled respi-rationwiththelaryngealmaskairway.Areview.Anaesthesist. 2001;50:187---91.