Journal
of
Coloproctology
w w w . j c o l . o r g . b r
Original
Article
Risk
factors
for
postoperative
endoscopic
recurrence
in
Crohn’s
disease:
a
Brazilian
observational
study
夽
Ivan
Folchini
de
Barcelos
a,
Rodolff
Nunes
da
Silva
a,
Fábio
Vieira
Teixeira
b,
Idblan
Carvalho
de
Albuquerque
c,
Rogério
Saad-Hossne
d,
Renato
Vismara
Ropelato
a,
Lorete
Maria
da
Silva
Kotze
a,
Márcia
Olandoski
e,
Paulo
Gustavo
Kotze
a,∗aColorectalSurgeryUnit,HospitalUniversitárioCajuru(SeCoHUC),PontifíciaUniversidadeCatólicadoParaná(PUC-PR),Curitiba,
PR,Brazil
bClínicaGastrosaúde,Marília,SP,Brazil
cInflammatoryBowelDiseasesOutpatientClinic,HospitalHeliópolis,SãoPaulo,SP,Brazil
dDigestiveSurgeryUnit,UniversidadeEstadualPaulistaJúliodeMesquitaFilho(UNESP),Botucatu,SP,Brazil eDepartmentofBiostatistics,PontifíciaUniversidadeCatólicadoParaná(PUC-PR),Curitiba,PR,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received24April2014 Accepted15May2014 Availableonline14June2014
Keywords:
Crohndisease Recurrence Riskfactors
a
b
s
t
r
a
c
t
Introduction:Postoperativeendoscopicrecurrence(PER)istheinitialeventafterintestinal resectioninCrohn’sdisease(CD),andafterafewyearsmostpatientspresentwith progres-sivesymptomsandcomplicationsrelatedtothedisease.Theidentificationofriskfactorsfor PERcanhelpintheoptimizationofpostoperativetherapyandcontributetoitsprevention.
Methods:Retrospective,longitudinal, multicenter,observationalstudy involvingpatients withCDwhounderwentileocolicresections.Thepatientswereallocatedintotwogroups accordingtothepresenceofPERandthevariablesofinterestwereanalyzedtoidentifythe associatedfactorsforrecurrence.
Results:Eighty-fivepatientswereincludedinthestudy.Themeanperiodofthefirst postop-erativecolonoscopywas12.8(3–120)monthsandPERwasobservedin28patients(32.9%). Therewasnostatisticaldifferenceinrelationtogender,meanage,durationofCD,family history,previousintestinalresections,smoking,Montrealclassification,bloodtransfusion, residualCD,surgicaltechnique,postoperativecomplications,presenceofgranulomasat histology,specimenextensionanduseofpostoperativebiologicaltherapy.Thepreoperative useofcorticosteroidswastheonlyvariablethatshowedasignificantdifferencebetween thegroupsinunivariateanalysis,beingmorecommoninpatientswithPER(42.8%vs.21%;
p=0.044).
Conclusions: PERwasobservedin32.9%ofthepatients.Thepreoperativeuseof corticoste-roidswastheonlyriskfactorassociatedwithPERinthisobservationalanalysis.
©2014SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.All rightsreserved.
夽
StudyconductedatTheColorectalSurgeryUnit,HospitalUniversitárioCajuru(SeCoHUC),PUC-PR,Curitiba,PR,Brazil. ∗ Correspondingauthor.
E-mail:pgkotze@hotmail.com(P.G.Kotze).
http://dx.doi.org/10.1016/j.jcol.2014.05.003
Fatores
de
risco
para
recorrência
endoscópica
pós-operatória
na
doenc¸a
de
Crohn:
um
estudo
observacional
brasileiro
Palavras-chave:
Doenc¸adeCrohn Recorrência Fatoresderisco
r
e
s
u
m
o
Introduc¸ão: Recorrênciaendoscópicapós-operatória(REP)éeventoinicialapósressecc¸ões intestinaisnadoenc¸adeCrohn(DC)egrandepartedospacientesprogridecomsintomas e complicac¸ões relacionados à doenc¸aem algunsanos. A identificac¸ão dos fatores de riscoparaREPpodeauxiliarnaotimizac¸ãodaterapiapós-operatóriaecontribuirparasua prevenc¸ão.
Método: Estudoretrospectivo,longitudinal,multicêntricoeobservacional,realizadocom pacientesportadoresdeDC,submetidosàressecc¸ãoileocólica.Ospacientesforamalocados emdoisgruposdeacordocomapresenc¸adeREPeasvariáveisdeinteresseforamanalisadas afimdeseidentificarosfatoresassociadosàrecorrência.
Resultados:Oitentaecincopacientesforamincluídosnoestudo.Otempomédiodaprimeira colonoscopiapós-operatóriafoide12,8(3-120)meseseREPfoiobservadaem28pacientes (32,9%).Nãohouvediferenc¸aestatísticaentreosgruposemrelac¸ãoa gênero,médiade idade,durac¸ãodaDC,históriafamiliar,ressecc¸ãointestinalprévia,tabagismo,classificac¸ão de Montreal, transfusão sanguínea, DC residual, técnica cirúrgica, complicac¸ões pós-operatórias,presenc¸adegranuloma,extensãodoespécimeeutilizac¸ãodebiológicosapós a cirurgia.Ousopré-operatóriode corticosteroidesfoia únicavariávelqueapresentou significativadiferenc¸anaanáliseunivariada,sendomaisfrequentenospacientesque apre-sentaramREP(42.8%vs.21%,p=0.044).
Conclusões: REPfoiobservadaem32.9%dospacientes.Autilizac¸ãopré-operatóriade corti-costeroidesfoioúnicofatorassociadoàREPnestaanáliseobservacional.
©2014SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda. Todososdireitosreservados.
Introduction
DespitetheprogressinthemedicaltherapyofCrohn’sdisease (CD),withbetterresultsaftertheuseofimmunosuppressive drugsandantagonistsoftumornecrosisfactor alpha (anti-TNFs),about70%ofpatientswillrequiresurgerythroughout their lives,often dueto complicationsassociated withthe disease,suchasfistulae,abscessesandfibroticstrictures.1–3
Onceundergoing intestinalresection, thesepatients are at increasedriskoffuturereoperationsand30–70%willrequire anewprocedureina10-yearinterval.1
Postoperativerecurrencecanbedefinedbydifferent find-ings,includingclinical,endoscopic,histological,radiological andsurgicalCharacteristics.4Thetimetorecurrencefollowsa
definitepattern,withendoscopicrecurrencebeingaprecursor ofsymptomatic(clinical)recurrence.5Uponendoscopic
recur-rence,about20%ofpatientshaveconcomitantclinicalrelapse within1yearandabove50%at5years.2,5,6
Besides preceding the symptoms, the severity of endo-scopiclesions predicts the likelihood ofsubsequent devel-opment of clinical recurrence and the need for another operation.7Accordingly,theuseoftheclassificationof
endo-scopic recurrence described by Rutgeerts et al.8 plays an
importantroleinthestandardizationofpostoperative endo-scopicfindings.
Some publications have suggested the stratification of postoperative endoscopic recurrence (PER) risk, based on patient-relatedcharacteristics,onsurgicalfindingsandonthe CDitself,inordertodeterminethebesttypeofpostoperative
prophylaxis.6,7Thefactorscommonlyusedforthis
stratifica-tionarethosewiththehighestlevelofevidence:priorbowel resection,penetratingdiseaseandsmoking.7,9,10
InBrazil,thereisscarcepublisheddataonfactors asso-ciatedwithpostoperativeendoscopicrecurrence.Thereisa needtodeterminewhichriskfactorsforPERrecognizedinthe internationalliteraturecanbeappliedtopatientsandat refer-ralcentersinourcountry,inordertoproperlystratifytherisks ofrecurrence,withsubsequentimprovementinpostoperative management.
Thus,theaimofthisstudywastoexamineratesofPER and determinewhichriskfactorswouldbeassociatedwith its occurrence inacohort ofBrazilian patientsundergoing ileocolicresectionsforCD.
Method
This study was approved by the Ethics Committee on Research, Center for Bioethics, Pontifícia Universidade Católica do Paraná (PUCPR), based on Opinion of Pre-sentation Certificate for Ethics Assessment (CAAE) nr. 19923413.1.0000.0020 (second version), performed by the
PlataformaBrasilwebsite.
Table1–DetaileddescriptionoftheRutgeerts’score (adaptedfromRutgeertsetal.)8.
Rutgeertsscore Endoscopicdescriptionoffindings i0 Nolesions
i1 ≤5aphthousulcerations
i2 >5aphthousulcerationswithnormalmucosa betweenthem,ornormalareasbetweenlarger ulcerations,orulcerationslimitedtotheileocolic anastomosis
i3 Diffuseaphthousileitiswithdiffuselyinflamed mucosa
i4 Diffuseinflammationwithlargeulcerations, nodulesorstenoses
Patients with CD, aged between 14 and 80 years, who underwentileocolicresectionwithprimaryanastomosisand with postoperative ileocolonoscopy during the evaluation period were included in the study. Patients with unde-termined inflammatory bowel disease, aged under 14 and over 80 years; patients undergoing other types of surgi-cal procedures (enterectomies, enteroplasties, colectomies, ileostomiesorotherprocedureswithoutanastomosis)orwho didnotundergopostoperativeileocolonoscopy;andpatients withnofollow-upaftersurgeryintheirrespectiveinstitution wereexcluded.
Collectionandprocessingofdata
PatientswerepreviouslyidentifiedindatabasesofIBD opera-tionsconductedatthefourreferralunits.Afterconfirmation oftheinclusioncriteria,datawerecollectedbyreviewing elec-tronicmedicalrecordsandfillingapre-establishedprotocol. Intheabsenceofdatarecordedinmedicalrecords,phonecalls topatients,whennecessarytosupplementtheinformation, wereperformed.
Definitionofrecurrenceandstudygroups
TheoccurrenceofPERwasassessedbythefirstpostoperative colonoscopicexaminationafterileocolicresection.The defi-nitionofPERwasbasedontheRutgeerts’score,8definedasi2,
i3ori4atileocolonoscopy.TheRutgeerts’scoreisillustrated inTable1.
Patientswereallocatedintotwogroupsaccordingtothe presenceorabsenceofendoscopicrecurrence:groupwithout recurrence(Rutgeertsi0/i1)andgroupwithrecurrence (Rut-geerts≥i2).Fromthesegroups,thevariablesofinterestwere
testedinordertoidentifypossiblefactorsassociatedwithPER, whichwouldbedesignatedasriskfactorsifstatistical signif-icancewasreached.
Statisticalanalysis
ForstatisticalanalysistheSPSSv.20softwarewasused.For qualitativevariables,weusedFisherexacttestorchi-squared test.For quantitativevariables,theStudent’st testor non-parametricMann–Whitneytestwasused.Univariateanalysis wasperformed todeterminethe association betweeneach independentvariableandthepresenceorabsenceofPER. Sta-tisticalsignificancewasdefinedasP<0.05.
Results
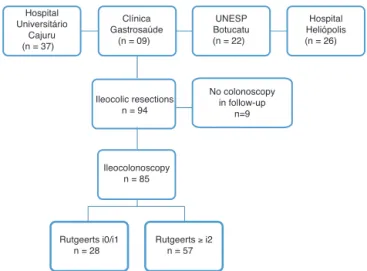
During the study period, 94 patients with CD underwent ileocolic resectionin thefour referral units. Ofthese, nine wereexcludedbecausetheyhadnotundergonecolonoscopy postoperatively. Thus, the series consisted of 85 patients (Fig.1).
Hospital Universitário
Cajuru (n = 37)
Clínica Gastrosaúde
(n = 09)
Ileocolic resections n = 94
Ileocolonoscopy n = 85
Rutgeerts i0/i1 n = 28
Rutgeerts ≥ i2 n = 57
UNESP Botucatu (n = 22)
Hospital Heliópolis (n = 26)
No colonoscopy in follow-up
n=9
Fig.1–Studydesignandgroupdivisionforevaluation accordingtothepresenceorabsenceofPER,definedas Rutgeerts’score≥i2.
The average time for the first postoperative ileo-colonoscopywas12.8(3–120)months.Consideringrecurrence asthe presenceofaRutgeerts’ score≥i2,thePER ratewas
32.9%(n=28).Table2illustratesindetailsthefindingsin rela-tiontotheRutgeerts’scoreindividually,showingthedivision ofthestudygroups.
Table2–Identificationofthegroupsaccordingtothe Rutgeerts’scoreatthefirstpost-operativecolonoscopyin 85patients.RecurrencedefinedasaRutgeertsscore≥i2.
Group Rutgeerts’ n(%) n(%) W/oPER i0 25(29.4) 57(67.1)
i1 32(37.6)
WithPER i2 10(11.8) 28(32.9) i3 15(17.6)
i4 3(3.5)
Total – 85(100) 85(100)
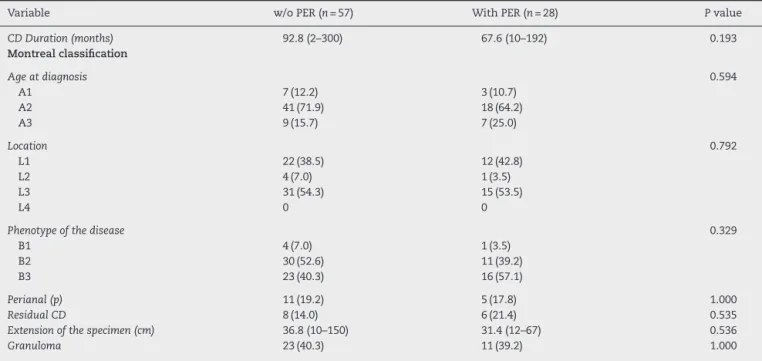
Patient-related factors were compared between groups (Table 3) and only the preoperative use of corticosteroids was statistically significant, being observed in a signif-icantly higher number of patients in the group with PER compared to the group without PER (42.8% vs. 21%
P=0.044).
Table3–UnivariateanalysisamongfactorsrelatedtopatientandstudygroupsregardingthepresenceofPER.Only preoperativeuseofcorticosteroidswasstatisticallysignificant.
Variable w/oPER(n=57) WithPER(n=28) Pvalue
Gender 0.487
Male 34(59.7) 14(50.0)
Female 23(40.3) 14(50.0)
Averageage(years) 32.8(14–63) 33.7(15–57) 0.753
FamilyhistoryofIBD 1(1.7) 2(7.1) 0.251
PreviousresectionsforCD 17(29.8) 8(28.5) 1.000
Smokingstatus 10(17.5) 7(25.0) 0.565
Preoperativemedications
Corticosteroids 12(21.0) 12(42.8) 0.044
AZA/6MP 30(52.6) 17(60.7) 0.498
Biologicals 15(26.3) 4(14.2) 0.129
Bloodtransfusion 8(14.0) 4(14.2) 1.000
Biologicalsinthepostoperativeperiod 39(68.4) 17(60.7) 0.627
Typeofpostoperativebiological 1.000
Adalimumab 20(35.0) 8(28.5) Infliximab 19(33.3) 9(32.1)
Table4–UnivariateanalysisamongfactorsrelatedtoCDandstudygroupsregardingthepresenceofPER.
Variable w/oPER(n=57) WithPER(n=28) Pvalue
CDDuration(months) 92.8(2–300) 67.6(10–192) 0.193
Montrealclassification
Ageatdiagnosis 0.594
A1 7(12.2) 3(10.7)
A2 41(71.9) 18(64.2)
A3 9(15.7) 7(25.0)
Location 0.792
L1 22(38.5) 12(42.8)
L2 4(7.0) 1(3.5)
L3 31(54.3) 15(53.5)
L4 0 0
Phenotypeofthedisease 0.329
B1 4(7.0) 1(3.5)
B2 30(52.6) 11(39.2)
B3 23(40.3) 16(57.1)
Perianal(p) 11(19.2) 5(17.8) 1.000
ResidualCD 8(14.0) 6(21.4) 0.535
Extensionofthespecimen(cm) 36.8(10–150) 31.4(12–67) 0.536
Granuloma 23(40.3) 11(39.2) 1.000
Discussion
The occurrence ofPER is not an uncommon event in CD, becauseoftherecurringnatureofthisdisease.Itisknownthat endoscopicrecurrenceprecedestheclinicalrecurrence,which inturn precedessurgicalrecurrence.About20%ofpatients withPERwillhavesymptomswithinayear,andover50%in fiveyears,makingthesepeoplevulnerabletofurther compli-cationsandpossiblyreoperations.6Basedonthesedata,the
mainissueinthecurrentmanagementofpostoperative recur-renceofCDistoidentifystrongpredictorsofrecurrence,in ordertoestablishifpatientswouldbenefitfrompostoperative prophylaxis.11
Thescarcityofnationaldataisanobstacletobetterdefine thebehaviorofpostoperativeCDinourcountry.Todate,this
isthefirststudyincludingalargenumberofBrazilianpatients withCD,whichsoughttoidentifyriskfactorsforendoscopic recurrence.
ThePERrateobservedinthisstudywas32.9%, notwith-standing the postoperative therapy used. Earlier studies showed PERratesover90% in1year.5 Currently,these
val-uesremainhigh,butwithgreatervariationsinreferralcenters (48–93%).5Inaretrospectivestudy,DeCruzetal.observedPER
in37.1%of70patientswhounderwentcolonoscopywithin1 yearaftersurgery,12afiguresimilartothenumberfoundin
this series.Standardizationinthe preventionof postopera-tiverecurrencetherapy,aswellastheuseofbiologicalagents, mayhavecontributedtothereductionofPERinmorerecent publications.
Table5–Univariateanalysisamongfactorsrelatedto surgicalproceduresperseandstudygroupsregarding
thepresenceofPER.
Variable w/oPER(n=57) WithPER(n=28) Pvalue Isolatedintestinal
resection
50(87.7) 23(82.1) 0.519
Typeofoperation 1.000
Open 49(85.9) 25(89.2) Laparoscopic 8(14.0) 3(10.7)
Anastomosis 1.000
stapled 43(75.4) 22(78.5) hand-sewn 14(24.5) 6(21.4)
Anastomosistype 0.274
side-to-side 42(73.6) 24(85.7) end-to-end 15(26.3) 4(14.2)
Earlycomplications 13(22.8) 8(28.5) 0.599 Abdominalsepsis 5(8.7) 4(14.2) 0.469 Anastomotic
dehiscence
4(7.0) 3(10.7) 0.679
thefollow-upofpatientsaftersurgicalresection.However,in somecasestheendoscopicexaminationwasperformedlater, whichmay have influenced thefinding ofluminal lesions, sincethelongerthewaitingtime,thegreatertheriskof endo-scopicrecurrence.2Themeanpostoperativeileocolonoscopy
timewasof12.8(3–120)months,andtheMann–Whitneytest adaptedanexclusion ofthe moredisparatefindingsofthe study,limitingthisbias.
Comparing observationally the groups with PER (n=27) versuswithout PER(n=58), itwasnoted thattherewasno statisticaldifferenceinrelationtogenderandageofpatients at surgery. Gender does not seem to be a risk factor for recurrence7,13;ontheotherhand,theagefactoratthetime
ofsurgerypresentsconflictingdata.2Ryanetal.,14ina
Cal-ifornian database, described an increased risk of surgical recurrence inpatients previously operatedwhen with less than20yearsold(RR=1.98,95%CI1.6–2.4).
DespitetheshorterdurationofCDinPERgroup,therewas nostatisticaldifferencebetweengroups; thus,this variable wasnotestablishedasariskfactorinthisobservationalstudy. CDofshorterdurationmayindicateamoreaggressive behav-ior,withrapidprogressiontocomplicationsandconsequent reoperations.SomestudiessuggestthatCDofshortduration isassociatedwithpostoperativerecurrence,15,16whileothers
havefailedtodemonstratesucharelationship.8,17Thislackof
consistencybetweenstudiesmaybelinkedtothedefinition oftheterm“short”duration,makingitdifficulttocompare studies.7
Despitethehigherproportionofsmokersinthegroupwith PER(25%, n=7),therewasnostatisticaldifference between groups. Although not associated with PER in this study, smokingistheonlymodifiableindependentfactorfor post-operativerecurrencedescribed with consistentevidence in theliterature.2,6,10Besidesincreasingtheriskofclinicaland
surgicalrecurrence,cigarettesmokingisresponsibleforthe elevationofPERrates.AccordingtoCottoneetal.18inastudy
involving182patients,PERwasdescribedin70%ofsmokers, comparedwith35%innonsmokers.Thus,itisessentialtostop smokinginpatientswithCDbecause,inadditiontoreducing
diseaseactivity,thismayalsoreducetheriskofendoscopic, clinicalandpostoperativesurgicalrecurrence.7
Anotherconsistentfactorassociatedwithrecurrenceisthe presenceofpreviousbowel resection.Inastudyconducted byNgetal.,19symptomaticrecurrencewasmorefrequentin
patientswithpreviousresection(p=0.06).Otherpublications alsodescribethisassociation,mostlywithclinicalandsurgical recurrence.20,21 In the presentstudy, therewas no
correla-tionbetweenthehistoryofpreviousintestinalresectionand endoscopicrecurrence.Approximately30%ofpatientsinboth groupshadpriorintestinalsurgery.Althoughthereis consis-tentdataintheliteratureonhighriskforclinicalandsurgical recurrence,previousbowelresectionswerenotconsidereda riskfactorforendoscopicrecurrence,maybeduetothelimited numberofpatientsinthissample.
Regarding theMontreal classification,noneofthe items showedstatisticaldifferencewithrespecttoPER. Neverthe-less, patients with PER presented mainly with penetrating CD (57.1%, n=16), which is considered one of the factors withscientificevidenceforpostoperativerecurrenceofCD. A meta-analysisbySimilliset al.22 described the
penetrat-ingphenotypeofthediseaseasassociatedwithclinicaland surgical recurrence, althoughsignificant heterogeneity was observedinthe13studiesincluded.Again,fewstudiesaddress thisbehaviorofCDasariskfactorforPER,thereisno con-sensusintheliterature,andinourstudythisvariablelacks statisticalsignificance.
Acohortstudyof907patientsinSwedenfoundan associ-ationofpostoperativerecurrencewithperianalCD(OR=1.6,
P=0.003) inpatients undergoing ileocolic resection.23 Yang
etal.24alsodemonstratedthisassociationwithclinical
recur-rence(P=0.007).However,otherstudiesfailedtodemonstrate this relationship, being few the trials published with high levelofevidencetosupportperianalCDasariskfactorfor recurrence.7,10 Inourstudy,arelationshipbetweenperianal
CDandPERalsowasnotidentified.
Regarding the medicationsusedbefore surgery,patients onimmunosuppressiveandbiologicdrugshadsimilarrates ofPER.On the otherhand, patientsoncorticosteroids had higherPERrates(21%)comparedtothosewithoutPER(42.8%), withstatisticalsignificance(P=0.044).Althoughreportedin somestudies,1,25 theuseofcorticosteroidsinthe
preopera-tiveperiodpresentsnoscientificevidenceasariskfactorfor recurrence,whichgoesagainsttheobservationalfindingsof this study.However,manypatientswithsurgicalindication aresteroid-dependents,despitetheimmunosuppressiveand biologictherapy,assuminganaggressivebehaviorand possi-blyestablishingahigherrateofrecurrence.Itisnotknown exactly whether this association is acoincidence (patients withamoreseveredisease,whofindincorticosteroidsa med-icationforstabilizationofsymptomsbeforetheiroperations), orrepresentapharmacologicaleffectofthismedicationon theoccurrenceofhigherratesofPER.
Therewasnodifferencebetweentheassociationof pro-cedureswithileocolic resection,aswell asthe presenceof residualCDonthefindingsofthisobservationalstudy.Few patients required procedures of stricturoplasty (n=3) and enterectomy(n=2),whichmayhavehamperedtheanalysis ofthisvariable.InasystematicreviewbyYamamotoetal.,26
inareaswithoutstricturoplastyandonlyin3%atthesitesof plasticprocedures.
ResidualCDwasobservedinahigherpercentage(21.4%)in thegroupwithPERcomparedtothosepatientswithoutPER (14%).Thisfindingiscloselyrelatedtoareasinwhichitwas decidedtoperformthestricturoplasty.However,studies sug-gestthattherecurrenceratesarelowafterthepermanenceof residualCDinareasofplasticprocedures.27,28Thereisno
evi-dencetosupportstricturoplastyandresidualCDasriskfactors forPER.
Regarding the surgical procedure per se, although the laparoscopicprocedures reducethe systemic inflammatory response,thereisnoevidencetosuggestareductionintherisk ofPER.Threeretrospectivestudies29–31andthreerandomized
clinicaltrials32–34showednodifferenceinratesofearlyorlate
recurrencebetweenopenand laparoscopicprocedures.The configurationandtypeofanastomosishavealsobeentested asariskfactor forPER.Ina randomizedclinicaltrial with ameanfollow-upof12months,theratesofPER and clini-calrecurrenceweresimilarbetweengroupswithside-to-side and end-to-endanastomoses.20 Asobservedin thecurrent
scientificevidence,inthepresentstudy,thedatarelatedto thesurgicaltechniqueusedwerenotconsideredasrisk fac-tors,consideringthatdifferencesbetweengroupsregarding PERwerenotidentified.
The presence of granulomas in the surgical specimens occurredinapproximately40%inbothgroups,withno asso-ciation with PER. Data regarding the predictive value of granulomasinthesurgicalspecimensareconflicting.2,7,13Ina
prospective20-yearstudy,Cullenetal.35foundanassociation
betweengranulomasandincreasedclinicalandsurgical recur-rence.Inameta-analysisincluding21studiesandatotalof 2236patientswithCD,thenumberofrecurrencesand reoper-ationswassignificantlyhigherinpatientswithversuswithout granulomas.36 However, other publications37,38 and more
recentlyaGermanstudydidnotrevealthisassociation.39
Krauseet al. followed 173 patients operated for CD for over 27 years.40 Extended resections with normalmargins
(10cm)wereassociatedwithlowerratesofreoperation, com-paredwitheconomicresections(31%vs.83%).Ontheother hand,Fazioetal.foundnodifferenceinpostoperative recur-renceinpatientsundergoingresectionwithlimited(2cm)or enlarged (12cm) macroscopicmargins.27 Theextent ofCD
influencesthe lengthofresection,but bothhavean indefi-niteimpactinthepostoperativerecurrence.7,10 Considering
thefactthatextendedsurgicalmarginsdonotrepresentclear benefitsinpreventingrecurrence,aneconomicresectionof themacroscopicallyaffectedsegmentmaybethebeststrategy inpatientswithCD,giventhelikelyneedforfuture reoper-ations,aswellastheriskofshortbowelsyndrome.7 Inour
study,themeanlengthofthespecimenwasslightlylarger inthegroupwithoutPER (36.8cmvs.31.4cm),but withno differencebetweengroups(P=0.536).
Itisknownthatbiologicaltherapycurrentlypresentsgood resultsinthepreventionofpostoperativerecurrenceandis indicatedforpatientsclassifiedashighriskforrecurrence.10
Accordingtotheliterature,thepostoperativeuseofanti-TNFs was not related to PER in the present study, and a lower utilizationratewasobservedinthegroupwithPER(60.7%), compared to the group without PER (68.4%), but with no
statistical differencebetween theiruse orthe typeofdrug (infliximaboradalimumab).
Thisstudyhasclearlimitations thatmustbetaken into accountinthedataanalysis.Insomepatientsthecolonoscopy wasperformed12monthsafterileocolicresection,afactthat influences the rate of PER, since the risk of postoperative recurrenceisdirectlyproportionaltothetimeof postopera-tivecolonoscopy.Inadditiontothelimitationsinherenttoa retrospective study,datafrom differentunitscaninfluence theresults,especiallybecausethisisanobservationalstudy, withnouseofafixedprospectiveprotocol.Althoughthe insti-tutionsinvolvedinthisstudyareconsideredreferralcenters in IBD, thereis somevariability inrelation tothe medical therapyandsurgicaltechniqueusedandintheinterpretation ofendoscopicfindingsbetweencenters.Ontheotherhand, thesmallnumberofpatientsanalyzedinsomevariablesand theabsenceofamultivariateanalysisalsocontributedtothe adoptionofacautiousinterpretationoftheresultsobtained inthisseries.
Insummary,inthisfirststudyonthesubjectonBrazilian patients,PERwasobservedin32.9%ofthepatients. Preopera-tivecorticosteroidusewastheonlyvariablethatwasrelatedto PER,establishingtheuseofthesedrugsasapossiblerisk fac-torfortheoccurrenceofendoscopicrecurrenceafterileocolic resection.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.SwogerJM,RegueiroM.Evaluationforpostoperative recurrenceofCrohndisease.GastroenterolClinNorthAm. 2012;41:303–14.
2.BuissonA,ChevauxJB,AllenPB,BommelaerG, Peyrin-BirouletL.Reviewarticle:thenaturalhistoryof postoperativeCrohn’sdiseaserecurrence.AlimentPharmacol Ther.2012;35:625–33.
3.Peyrin-BirouletL,LoftusEV,ColombelJF,SandbornWJ.The naturalhistoryofadultCrohn’sdiseaseinpopulation-based cohorts.AmJGastroenterol.2010;105:289–97.
4.SpinelliA,SacchiM,FiorinoG,DaneseS,MontorsiM.Riskof postoperativerecurrenceandpostoperativemanagementof Crohn’sdisease.WorldJGastroenterol.2011;17:3213–9.
5.RutgeertsP,GeboesK,VantrappenG,KerremansR, CoenegrachtsJL,CoremansG.Naturalhistoryofrecurrent Crohn’sdiseaseattheileocolonicanastomosisaftercurative surgery.Gut.1984;25:665–72.
6.MossAC.PreventionofpostoperativerecurrenceofCrohn’s disease:whatdoestheevidencesupport?InflammBowelDis. 2013;19:856–9.
7.DeCruzP,KammMA,PrideauxL,AllenPB,DesmondPV. PostoperativerecurrentluminalCrohn’sdisease:asystematic review.InflammBowelDis.2012;18:758–77.
8.RutgeertsP,GeboesK,VantrappenG,BeylsJ,KerremansR, HieleM.PredictabilityofthepostoperativecourseofCrohn’s disease.Gastroenterology.1990;99:956–63.
10.YamamotoT,WatanabeT.Strategiesforthepreventionof postoperativerecurrenceofCrohn’sdisease.ColorectalDis. 2013;15:1471–80.
11.NgSC,KammMA.ManagementofpostoperativeCrohn’s disease.AmJGastroenterol.2008;103:1029–35.
12.DeCruzP,BernardiMP,KammMA,AllenPB,PrideauxL, WilliamsJ,etal.PostoperativerecurrenceofCrohn’sdisease: impactofendoscopicmonitoringandtreatmentstep-up. ColorectalDis.2013;15:187–97.
13.CunninghamMF,DochertyNG,CoffeyJC,BurkeJP,O’Connell PR.PostsurgicalrecurrenceofilealCrohn’sdisease:anupdate onriskfactorsandinterventionpointstoacentralrolefor impairedhost-microflorahomeostasis.WorldJSurg. 2010;34:1615–26.
14.RyanWR,AllanRN,YamamotoT,KeighleyMR.Crohn’s diseasepatientswhoquitsmokinghaveareducedriskof reoperationforrecurrence.AmJSurg.2004;187:219–25.
15.SacharDB.Theproblemofpostoperativerecurrenceof Crohn’sdisease.MedClinNorthAm.1990;74:183–8.
16.PoggioliG,LauretiS,SelleriS,BrignolaC,GraziGL,StocchiL, etal.FactorsaffectingrecurrenceinCrohn’sdisease.Results ofaprospectiveaudit.IntJColorectalDis.1996;11:294–8.
17.ShivanandaS,Lennard-JonesJ,LoganR,FearN,PriceA, CarpenterL,etal.Incidenceofinflammatoryboweldisease acrossEurope:isthereadifferencebetweennorthandsouth? ResultsoftheEuropeanCollaborativeStudyonInflammatory BowelDisease(EC-IBD).Gut.1996;39:690–7.
18.CottoneM,RosselliM,OrlandoA,OlivaL,PuleoA,Cappello M,etal.SmokinghabitsandrecurrenceinCrohn’sdisease. Gastroenterology.1994;106:643–8.
19.NgSC,LiedGA,ArebiN,PhillipsRK,KammMA.Clinicaland surgicalrecurrenceofCrohn’sdiseaseafterileocolonic resectioninaspecialistunit.EurJGastroenterolHepatol. 2009;21:551–7.
20.McLeodRS,WolffBG,RossS,ParkesR,McKenzieM,
InvestigatorsoftheCASTTrial.RecurrenceofCrohn’sdisease afterileocolicresectionisnotaffectedbyanastomotictype: resultsofamulticenter,randomized,controlledtrial.Dis ColonRectum.2009;52:919–27.
21.ArdizzoneS,MaconiG,SampietroGM,RussoA,RadiceE, ColomboE,etal.Azathioprineandmesalaminefor preventionofrelapseafterconservativesurgeryforCrohn’s disease.Gastroenterology.2004;127:730–40.
22.SimillisC,YamamotoT,ReeseGE,UmegaeS,MatsumotoK, DarziAW,etal.Ameta-analysiscomparingincidenceof recurrenceandindicationforreoperationaftersurgeryfor perforatingversusnonperforatingCrohn’sdisease.AmJ Gastroenterol.2008;103:196–205.
23.BernellO,LapidusA,HellersG.Riskfactorsforsurgeryand recurrencein907patientswithprimaryileocaecalCrohn’s disease.BrJSurg.2000;87:1697–701.
24.YangRP,GaoX,ChenMH,XiaoYL,ChenBL,HuPJ.Risk factorsforinitialbowelresectionandpostoperative recurrenceinpatientswithCrohndisease.ZhonghuaWei ChangWaiKeZaZhi.2011;14:176–80.
25.YamamotoT.Factorsaffectingrecurrenceaftersurgeryfor Crohn’sdisease.WorldJGastroenterol.2005;11:3971–9.
26.YamamotoT,FazioVW,TekkisPP.Safetyandefficacyof strictureplastyforCrohn’sdisease:asystematicreviewand meta-analysis.DisColonRectum.2007;50:1968–86.
27.FazioVW,MarchettiF,ChurchM,GoldblumJR,LaveryC,Hull TL,etal.Effectofresectionmarginsontherecurrenceof Crohn’sdiseaseinthesmallbowel.Arandomizedcontrolled trial.AnnSurg.1996;224:563–71.
28.StebbingJF,JewellDP,KettlewellMG,MortensenNJ. Recurrenceandreoperationafterstrictureplastyfor
obstructiveCrohn’sdisease:long-termresults[corrected].BrJ Surg.1995;82:1471–4.
29.EshuisEJ,PolleSW,SlorsJF,HommesDW,SprangersMA, GoumaDJ,etal.Long-termsurgicalrecurrence,morbidity, qualityoflife,andbodyimageoflaparoscopic-assistedvs. openileocolicresectionforCrohn’sdisease:acomparative study.DisColonRectum.2008;51:858–67.
30.LowneyJK,DietzDW,BirnbaumEH,KodnerIJ,MutchMG, FleshmanJW.Isthereanydifferenceinrecurrenceratesin laparoscopicileocolicresectionforCrohn’sdiseasecompared withconventionalsurgery?Along-term,follow-upstudy.Dis ColonRectum.2006;49:58–63.
31.TabetJ,HongD,KimCW,WongJ,GoodacreR,AnvariM. LaparoscopicversusopenbowelresectionforCrohn’s disease.CanJGastroenterol.2001;15:237–42.
32.StocchiL,MilsomJW,FazioVW.Long-termoutcomesof laparoscopicversusopenileocolicresectionforCrohn’s disease:follow-upofaprospectiverandomizedtrial.Surgery. 2008;144:622–7.
33.MaartenseS,DunkerMS,SlorsJF,CuestaMA,PierikEG, GoumaDJ,etal.Laparoscopic-assistedversusopenileocolic resectionforCrohn’sdisease:arandomizedtrial.AnnSurg. 2006;243:143–9.
34.MilsomJW,HammerhoferKA,BöhmB,MarcelloP,ElsonP, FazioVW.Prospective,randomizedtrialcomparing
laparoscopicvs.conventionalsurgeryforrefractoryileocolic Crohn’sdisease.DisColonRectum.2001;44:1–8.
35.CullenG,O’TooleA,KeeganD,SheahanK,HylandJM, O’donoghueDP.Long-termclinicalresultsofileocecal resectionforCrohn’sdisease.InflammBowelDis. 2007;13:1369–73.
36.SimillisC,JacovidesM,ReeseGE,YamamotoT,TekkisPP. Meta-analysisoftheroleofgranulomasintherecurrenceof Crohndisease.DisColonRectum.2010;53:177–85.
37.GlassRE,BakerWN.Roleofthegranulomainrecurrent Crohn’sdisease.Gut.1976;17:75–7.
38.ChambersTJ,MorsonBC.ThegranulomainCrohn’sdisease. Gut.1979;20:269–74.
39.WelschT,HinzU,LöfflerT,MuthG,HerfarthC,SchmidtJ, etal.Earlyre-laparotomyforpost-operativecomplicationsis asignificantriskfactorforrecurrenceafterileocaecal resectionforCrohn’sdisease.IntJColorectalDis. 2007;22:1043–9.
40.KrauseU,EjerbladS,BergmanL.Crohn’sdisease.Along-term studyoftheclinicalcoursein186patients.ScandJ