jcoloproctol(rioj).2016;36(4):240–243
w w w . j c o l . o r g . b r
Journal
of
Coloproctology
Case
Report
Submucosal
lipoma
simulating
a
malignant
tumor
of
the
left
colon:
a
case
report
Victor
Minari
Campos
a,∗,
Sergio
Mazzola
Poli
de
Figueiredo
a,
Rodrigo
Salmeron
de
Toledo
Aguiar
a,
Augusto
Canton
Gonc¸alves
a,
Thiago
Manzione
b,
Fang
Chia
Bin
baFaculdadedeCiênciasMédicasdaSantaCasadeSãoPaulo(FCMSCSP),SãoPaulo,SP,Brazil
bIrmandadedeMisericórdiadaSantaCasadeSãoPaulo,DepartmentodeColoproctologia,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received1February2016 Accepted20April2016 Availableonline30June2016
Keywords: Lipoma Colontumor Benigntumor Colon
Descendingcolon
a
b
s
t
r
a
c
t
Intestinallipomascanoccuranywhereinthegastrointestinaltract,andthesetumorsare morefrequentinthecolon.Bybeinglargelyasymptomatic,colonic lipomasareusually foundincidentally,asfindingsincolonoscopyexaminations,inassociationwithbiopsy. Endoscopicorsurgicalresectionisthetherapeuticoption,dependingonthesizeofthe tumor,itslocation,andthepresenceorabsenceofsymptoms.Inthisstudy,wepresenta caseofa59-yearoldwoman,withadescendingcolonlipomahistologicallydiagnosedonly aftersurgicalresectionofthelesion.Theapproachwasadoptedaccordingtothepatient’s clinicalpicture(intestinalbleeding,vomitingandweightloss),inadditiontotheocclusion of80%ofthecoloniclumenobservedinacolonoscopy.
©2016SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.This isanopenaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
Lipoma
submucoso
simulando
tumor
maligno
de
cólon
esquerdo:
relato
de
caso
Palavras-chave: Lipoma Tumordecolon Tumorbenigno Colon
Colondescendente
r
e
s
u
m
o
Oslipomasintestinaispodemocorreremqualquerpartedotratogastrointestinal,sendo maisfrequentenocólon.Porserememgrandeparteassintomáticos,oslipomas colôni-cossãousualmenteencontradosacidentalmentecomoachadosdeexamedecolonoscopia associadaà biópsia.Como opc¸õesdetratamento,háaressecc¸ão endoscópicaou cirúr-gica,adependerdotamanhodotumor,sualocalizac¸ãoepresenc¸a(ounão)desintomas. Nesserelato,éapresentado umcasodeumamulher de59 anoscomlipomade cólon
∗ Correspondingauthor.
E-mail:victormcampos@hotmail.com(V.M.Campos).
http://dx.doi.org/10.1016/j.jcol.2016.04.014
jcoloproctol(rioj).2016;36(4):240–243
241
descendente,diagnosticadohistologicamenteapenasapósressecc¸ãocirúrgicadalesão.A condutafoiadotadapeloquadroclínicodeenterorragia,vômitoseperdaponderal,alémda oclusãode80%daluzdocólonobservadaemexamedecolonoscopia.
©2016SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
Introduction
Colonic lipomas are benign tumors arising from the con-nective tissue of the intestinal wall,1 representing 2.6% of
non-malignanttumorsofthegastrointestinaltract.2Although
this is the most frequent non-malignant intramural mes-enchymaltumorofthe gastrointestinaltract and the third in frequency, coming after adenomatous and hyperplastic polyps, are few the cases described inthe literature.2–4 In
mostcases,thetumorisasymptomatic,1,3,5generallybeing
anaccidentalfindingofimagingstudies,3–7butthesetumors
mayshowsymptomssuchasabdominalpain,rectal bleed-ing,changeinbowelhabits,abdominalbloating,anorexia,and weightloss.3–6,8
Case
report
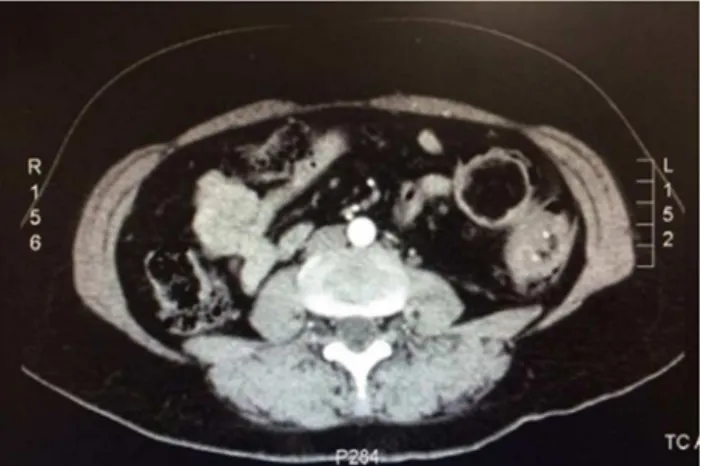
Ourpatientwasa59-yearoldbrown-coloredfemaleseenat theColoproctologyoutpatientclinicofatertiaryhospitalwith ahistoryofhypogastric colicpain fora year,accompanied byvomiting,diarrhea, and rectalbleeding. Inaddition, the patientmentionedaweightlossof5kginayear.Thispatient ishypertensive,withlactoseintolerance andhasnofamily historyofgastrointestinaldisease.Onphysicalexamination, theabdomenwasflat,flaccid,andpainlesstopalpationand withhydro-aerialsoundspresent.Theproctologic examina-tionrevealedanormalstaticanddynamicinspectionandthe digitalrectalexaminationwaswithoutpalpablelesions.Three colonoscopieswereperformed;thefirsttwowereperformed inotherservices,indicatingabenigntumorofapproximately 5cm, at the transition between the descending colon and thesigmoid,occluding40% ofthe coloniclumen. However, the biopsies produced unspecificresults. Between the first andthelastcolonoscopy,7monthshavepassed,anditwas noted a substantial increase of 80% in the colonic lumen occlusion.Thelastcolonoscopywasperformedinourservice, inordertoattainabetterdirectvisualizationofthelesion, in an attempt for the histological diagnosis, and also for tattooing the lesion found, in order to facilitatethe intra-operativemanagementoftheinjury.ACTscanshowedleft colonthickening(Fig.1).Thelaboratoryworkupshowedno changes,withCEA=1.8before surgery.Tumorexcision and primaryanastomosisoftheresectedcolonicportionwere car-ried out.Postoperatively, there were no complications and thepatientwasdischargedinagoodcondition.The patho-logicalexaminationshowedapolypoid-likelesionmeasuring 4.5cm×3.5cm,withayellow,softtocut,tissue(Figs.2and3). Amucosawithreducedwrinklingandagrayareaandwith parietalinfiltrationwasalsoobserved.Theadiposetissuewas
Fig.1–AbdominalCTwithleftcolonthickening.
Fig.2–Surgicalspecimen.
242
jcoloproctol(rioj).2016;36(4):240–243lobedandwithoutspecialfeatures.Thediagnosisofintestinal submucosallipomawasconfirmed,withprocess-freesurgical margins.
Discussion
Ourpatientisa59-yearoldfemale,whichcorrespondstothe mostfrequentgenderand agegroup ofpatients diagnosed withlipoma:womenbetweenthefifthandsixthdecade of life.1,6,7
Intestinallipomasarecommonlydiagnosedthrough find-ingsincolonoscopyprocedures indicatedforthetreatment ofotherdiseasesorforscreeningpurposes,consideringthat these tumorsare more prevalent inthe colon than inthe smallintestine,2,5,7,8beingasymptomaticinmostcases.1,3,5,7
Clinicalmanifestationsareevidentinapproximately 6–25% ofdiagnoses.1,5 However, the case atissue corresponds to
agiantlipoma, anatomopatologicallyprovenbythe sizeof thesurgicalspecimen,a piecemeasuringover 4cm. Inthe faceoftumorsofsuchsize,thepercentageofsymptomatic cases is75%.5,6 The patient complained ofan hypogastric
pain,episodesofrectalbleeding,diarrheaandamildweight loss–normalfindingsinsymptomaticcasesoflipoma.4–6,8in
addition,thepatienthadvomitepisodes,whichisnotoften describedintheliterature.
Colonoscopyistheprimarymethodfordiagnosisofcolonic lipomas. The characteristic findings are the presence of a wide-basetumor,withayellowishtintduetothe underly-ingfattytissue.Furthermore,a“tentingsign”anda“cushion sign”arealsoobserved:thefirstsignaliselicitedifonepulls themucosaoverlyingthelipoma,whichdetachesitself eas-ily, asseenin othersubmucosal lesions;the secondsignal consistsintouching the lipomawitha biopsy fórceps;the lipomaisdepressed easilyand quicklyreturns toits origi-nalform.3,4,6,9Aftertheestablishmentofthediagnosis,one
mustconsiderasurgicalapproach.Tumorresectionis indi-cated in casesof a symptomaticlipoma, particularly with obstruction or bleeding; if the mass measures more than 2.5cm; or if the injury is mimicking malignancy.1,2,5,6,8 In
the case reported, with the first two consecutive colonos-copies a 4-cm diameter protruding injury with a 40% of occlusion of the lumen of the descending colon – site of 20% ofcoloniclipomas –was diagnosed.1,4–7 Atthis point,
asurgerycould havebeen performed,bothconsideringthe clinical manifestations and the tumor size. However, this was not done due to the irregular follow-up in another service. After 7 months, a new colonoscopy showed a 6-cmlesion with80% ofocclusion; thistime, the lesionwas resected,despitetheabsenceofahistologicaldiagnosiswith the colonoscopy examinations performed prior to surgery. Thus, alaparotomy wasperformed, along witha segmen-talleft colectomywithprimaryanastomosis.Lipomaswith a less than 2-cm diameter can be removed endoscopi-cally;on the other hand,larger lesions must be surgically resected.4
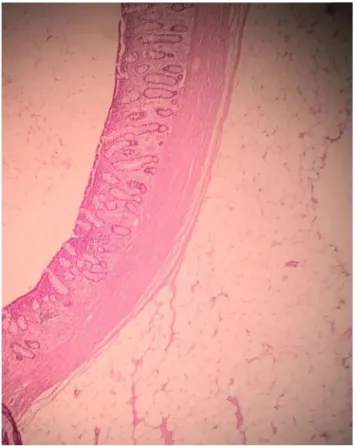
The pathological examination of the surgical specimen confirmed a description macro- and microscopically con-sistent with a diagnosis of intestinal submucosal lipoma, which isin accordance withthe highestfrequency among
Fig.4–Histologyoflesioncompatiblewithsubmucosal lipoma.
its subtypes. Submucosal lipomas are more frequent than subserosal andmixed lipomas.1,4 Histologically,the lipoma
showsadenseaccumulationofenlargedandroundedfatcells with cytoplasmand nucleus inthe cell periphery (Fig. 4).1
Grossly, the tumor may present itself in different forms: rounded,sessileorcoveredbyafibroustissuecapsule branch-ingovertheadiposetissuemass,whichresultsintheirlobate appearance.1,4
Conclusion
Lipomasarerarebenigntumors.Inmostcases,thesetumors are asymptomatic and are accidentallydiagnosed, particu-larly by colonoscopy.Their treatment isbased on the size of the lesion, presence of symptoms, and if there is sus-picion of malignancy, and the evaluated criteria point to an endoscopic or surgical resection. The gender and age group ofour patient were the mostprevalent for this dis-ease,andherswasagiantandsymptomatictumor;however, it tumor was not localized in the most frequent position in the colon. For all thesereasons, wechoseto performa surgery.
Conflicts
of
interest
jcoloproctol(rioj).2016;36(4):240–243
243
r
e
f
e
r
e
n
c
e
s
1.AndreiLS,AndreiAC,UsureluDL,PuscasuLI,DimaC,PredaE, etal.Rarecauseofintestinalobstruction–submucouslipoma ofthesigmoidcolon.Chirurgia(Bucur).2014;109:142–7.
2.AminianA,NoaparastM,MirsharifiR,BodaghabadiM, MardanyO,AliFAH,etal.Ilealintussusceptionsecondaryto bothlipomaandangiolipoma:acasereport.CasesJ. 2009;2:7099.
3.DultzLA,UlleryBW,SunHH,HustonTL,EachempatiSR,Barie PS.Ileocecalvalvelipomawithrefractoryhemorrhage.JSLS. 2009;13:80–3.
4.KatsinelosP,ChatzimavroudisG,ZavosC,PilpilidisI,Lazaraki G,PapaziogasB,etal.Cecallipomawithpseudomalignant features:acasereportandreviewofliterature.WorldJ Gastroenterol.2007;13:510–3.
5.MorimotoT,FuKI,KonumaH,IzumiY,MatsuyamaS,OguraK, etal.Peelingagiantileallipomawithendoscopicunroofing andsubmucosaldissection.WorldJGastroenterol.
2010;16:1676–9.
6.RehmanA,AhluwaliaJP.Largetubularcolonicmasswith hematocheziaandalteredbowelhabits.AmFamPhysician. 2012;86:451–3.
7.JiangL,JiangL-S,LiF-Y,YeH,LiN,ChengNS,etal.Giant submucosallipomalocatedinthedescendingcolon:acase reportandreviewoftheliterature.WorldJGastroenterol. 2007;13:5664–7.
8.PaˇskauskasS,LatkauskasT,Valeikait ˙eG,Parˇseli ¯unasA, Svag ˇzdysS,Salad ˇzinskasZ,etal.Colonicintussusception causedbycoloniclipoma:acasereport.Medicina(Kaunas). 2010;46:477–81.