REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiology www.sba.com.brREVIEW
ARTICLE
Effectiveness
of
combined
regional-general
anesthesia
for
reducing
mortality
in
coronary
artery
bypass:
meta-analysis
夽
Fabiano
Timbó
Barbosa
a,∗,
Rafael
Martins
da
Cunha
b,
Fernando
Wagner
da
Silva
Ramos
a,
Fernando
José
Camello
de
Lima
a,
Amanda
Karine
Barros
Rodrigues
a,
Ailton
Mota
do
Nascimento
Galvão
a,
Célio
Fernando
de
Sousa-Rodrigues
a,
Paula
Monique
Barbosa
Lima
aaUniversidadeFederaldeAlagoas,Maceió,AL,Brazil bHospitalUnimed,Maceió,AL,Brazil
Received22March2014;accepted13May2014 Availableonline21January2016
KEYWORDS
Generalanesthesia; Neuraxialanesthesia; Mortality;
Meta-analysis; Coronaryartery bypass
Abstract
Backgroundandobjectives: Neuraxialanesthesia(NA)hasbeenusedinassociationwithgeneral anesthesia(GA)forcoronaryarterybypass;however,anticoagulationduringsurgerymakesus questiontheviabilityofbenefitsbytheriskofepiduralhematoma.Theaimofthisstudywas toperformameta-analyzesexaminingtheefficacyofNAassociatedwithGAcomparedtoGA aloneforcoronaryarterybypassonmortalityreduction.
Methods:Mortality,arrhythmias, cerebrovascularaccident(CVA),myocardialinfarction(MI), lengthofhospitalstay(LHS),lengthofICUstay(ICUS),reoperations,bloodtransfusion(BT), qualityoflife,satisfactiondegree,andpostoperativecognitivedysfunctionwereanalyzed.The weightedmeandifference(MD)wasestimatedforcontinuousvariables,andrelativerisk(RR) andriskdifference(RD)forcategoricalvariables.
Results:17 originalarticlesanalyzed.Meta-analysis ofmortality(RD=−0.01, 95%CI=−0.03
to 0.01), CVA (RR=0.79, 95% CI=0.32---1.95), MI (RR=0.96, 95% CI=0.52---1.79) and LHS (MD=−1.94,95%CI=−3.99to0.12)werenotstatisticallysignificant.Arrhythmiawasless
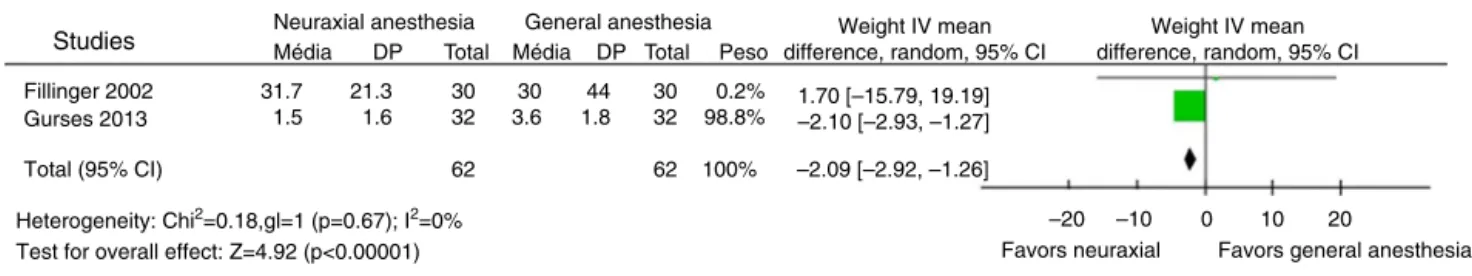
fre-quentwithNA(RR=0.68,95%CI=0.50---0.93).ICUSwaslowerinNA(MD=−2.09,95%CI=−2.92
to−1.26).
Conclusion: Therewasnosignificantdifferenceinmortality.CombinedNAandGAshowedlower incidenceofarrhythmiasandlowerICUS.
© 2014SociedadeBrasileirade Anestesiologia.Publishedby ElsevierEditoraLtda.Allrights reserved.
夽
Locationresearch:UniversidadeFederaldeAlagoas,Maceió,AL, Brazil.
∗Correspondingauthor.
E-mail:fabianotimbo@yahoo.com.br(F.T.Barbosa). http://dx.doi.org/10.1016/j.bjane.2014.05.012
PALAVRAS-CHAVE
Anestesiageral; Anestesianeuroaxial; Mortalidade;
Metanálise; Revascularizac¸ão miocárdica
Efetividadedaassociac¸ãodaanestesiaregionalàanestesiageralnareduc¸ão
damortalidadeemrevascularizac¸ãomiocárdica:metanálise
Resumo
Introduc¸ãoeobjetivos: Aanestesianeuroaxial(AN)vemsendoutilizadaemassociac¸ãocoma anestesiageral(AG)para revascularizac¸ãomiocárdica, entretantoaanticoagulac¸ãodurante acirurgiatornaquestionávelaviabilidadedosbenefíciosmedianteoriscodehematomade espac¸operidural.Oobjetivodesteestudofoiexecutarmetanálises analisandoaefetividade daANassociadaàAGcomparadaàAGisoladaparaacirurgiaderevascularizac¸ãomiocárdica relativaàreduc¸ãodamortalidade.
Métodos: Foramanalisados mortalidade,arritmias,acidentevascularcerebral(AVC),infarto miocárdico(IM),tempo deinternac¸ãohospitalar(TIH),tempo deinternac¸ãoem unidadede terapiaintensiva(TUTI),reoperac¸ões,transfusãosanguínea(TS),qualidadedevida,graude satisfac¸ãoedisfunc¸ãocognitivapós-opertória.Adiferenc¸amédia(DM)ponderadafoiestimada para as variáveiscontínuas erisco relativo (RR)e adiferenc¸a de risco (DR)para variáveis categóricas.
Resultados: Analisados 17 artigos originais. Metanálise da mortalidade (DR=−0,01; IC
95%=−0,03a0,01),AVC(RR=0,79;IC95%=0,32a1,95),IM(RR=0,96;IC95%=0,52a1,79)
eTIH(DM=−1,94;IC95%=−3,99a0,12)nãodemonstraramsignificânciaestatística.Arritmia
foimenos frequente comAN(RR=0,68;IC95%=0,50a0,93).OTUTIfoimenor nocomAN (DM=−2,09;IC95%=−2,92a−1,26).
Conclusão:Nãoseobservaramdiferenc¸asestatisticamentesignificantesquantoamortalidade. Acombinac¸ãodeANeAGmostroumenorincidênciadearritmiasemenorTUTI.
©2014SociedadeBrasileiradeAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Coronary artery bypass grafting occurs in approximately 800,000 patients annually.1 There is an increased
inter-est in the use of neuraxial anesthesia (NA), spinal and epidural anesthesia, associated with general anesthesia (GA) for coronary artery bypass, which is also a matter for further research worldwide.2 The risks and
bene-fits of NA in this setting have been reviewed in adult patients.2
One of the benefits of NA is tomitigate the response to surgical stress due to blockage of cardioaccelerator fibers, T1 to T5, and improved coronary response to vasodilators improving the balance between the supply and consumption of myocardial oxygen.2,3 Sympathetic
activationisconsideredthemainmechanismforthe occur-rence of new myocardial infarction in the postoperative period.3
Theuseof NAinheartsurgeryisstillcontroversialdue tothepossibilityofhematomaor abscessatthepuncture siteandthepossibilityofspinalcompression.4Thecurrent
dataavailableintheliteraturewereusedinmathematical modelsto estimatethe maximum risk of this eventafter fullheparinization,whichwasestimatedat1:2400withfull heparinization.4
The aim of this study wastoperforma meta-analyzes to evaluate the effectiveness of neuraxial anesthesia associated with general anesthesia compared to general
anesthesia alone for coronary artery bypass grafting regardingthereductionofmortality.
Method
Systematic review was performed following a protocol developed prioroftheperformingthisreview.This proto-col,aswellasthereviewperformance,followedthesteps suggestedbyThePreferredReportingItemsforSystematic ReviewsandMeta-Analysis(PRISMA)statement.5Thestages
ofthisresearchwere:systematicliteraturesearch,careful analysis for inclusionand exclusionof studies, analysis of thequalityofstudies,datacollectionofoutcomevariables, meta-analyticcalculations,analysisofsensitivityand homo-geneity,andtrialsequentialanalysis.Allstagesperformed aredescribedbelow.
Searchstrategy
The identification and systematic search for potentially relevant original articles was performed in the following databases:MedlineviaPubMedfromJanuary1966to Jan-uary 2014, Cochrane Central Registerof Controlled Trials (CENTRAL)n◦3(2014),ExcerptaMedicaDatabase(EMBASE) fromJanuary1974toJanuary2014,andLiteratura
Latino-AmericanaedoCaribeemCiênciasdaSaúde(Lilacs)from
studieswerealsoanalyzedforarticlesthathadthe poten-tialtobepartofthisreview,buttheywerenotidentifiedin theelectronicdatabases.Wesearchedforpublishedstudies comparingtheuseof NAassociatedwithGAandGAalone for coronary artery bypass grafting. The following terms wereusedindifferentcombinations:Anesthesia,General;
Anesthesias,Intravenous;neuraxialanesthesia,Anesthesia;
Epidural,anesthesia,spinal,thoracicsurgicalprocedures,
andclinicaltrialsastopic.Thesearchwaslimitedto
clini-caltrialsofrandomallocationthatincludedadultpatients (over18yearsold)whounderwentsurgeryonlyforcoronary arterybypass.Therewasnolanguagerestriction.
Inclusionandexclusioncriteriaofthestudies
Inclusioncriteriawereclinicaltrialswithrandomallocation that assessed patients undergoing coronary artery bypass and comparedthe NAtechniques associatedwith GA and GAalonewithorwithoutcatheter.
Exclusioncriteriawereoriginalarticlesofclinicaltrials withinadequatedescriptionofvariablesofinterestforthis review,whentheallocationforcoronaryarterybypass graft-ingwasassociatedwithanothertypeofsurgery,whenthe variableswerenotofinteresttothissystematicreview,and whenaninterventionother thanNAor GAwasusedinthe patientsstudied.
Studies initially identified by reading the titles and abstractsthatseemedrelevanttothisreviewweregrouped togetherfor fullreadingby tworeviewers. Disagreements wereresolvedbyconsensusmeetings.Ifthedisagreements werenotresolved,theparticipationofathird authorwas planned,butitwasnotnecessary.
Criticalanalysisofthestudies’quality andclassification
Theclassificationofstudieswascarriedoutindividuallyand independently by tworeviewers, who scored the original articlesaccordingtoitsmethodologicalquality,accordingto thecriteriaofJadad.6Theevaluatedcriteriawererandom
assignmentofsubjectstogroups,adequacyoftherandom allocation,concealmentofindividualsingroups,adequacy ofconcealmentofindividualsandthedescriptionoflosses andexclusions.Atotalof5pointscouldbeachievedwith goodqualityarticlesbeingconsideredthosethatreachmore than2points.Thiscriterionwasnotusedtoexcludeoriginal articlesofmeta-analyticreview.
TheAgreementKappaIndexwasusedtoassesswhether therehasbeenagreementamongthereviewers oriftheir analysiswereconsistentamongthemselves.Thisstatistical testwasusedconsideringastatisticalpowerof80%andtype Ierror probabilityof5%.The valuesof thistest mayvary between0and1with0beingtheabsenceofagreementand 1perfectagreementbetweenreviewers.Valuesabove0.8 wereconsideredasgoodagreementbetweenreviewers.
Outcomevariablesanddataextractionmethod
The primary outcome variable was mortality. The vari-able mortality was considered for the first 7 days of
hospitalization(immediate), between7 and30 daysafter surgery(early), and after1 year of follow-up (late). Sec-ondaryoutcomevariableswerearrhythmias,stroke,acute myocardialinfarction,lengthof hospitalstaymeasured in days,length ofintensivecare unitstay measuredin days, reoperationfrequency,blood transfusionmeasured bythe number of participants who received blood transfusion, quality of life, degree of satisfaction, and postoperative cognitivedysfunction.
Tworeviewersindependentlycollectedthedata.Oneof thereviewersenteredthedataintoacomputerprogramand later,inasecond stage,theotherreviewerwhocollected the data checked to prevent the insertion of exchanged numbersintothecomputerprogram.Themeta-analytic cal-culations were performed only after the checking by the secondreviewer.
Meta-analysis
The Review Manager software was used to perform the meta-analysiscalculations.7Itwasplannedtocalculatethe
magnitudeof theinterventions’ effectandthe respective 95%confidenceintervals(95%CI)fordichotomousvariables using relative risk (RR), however, if the event frequency wasabsent in an analyzed variable included in the origi-nalarticle,theriskdifference(RD)wasused.Theinterval variables were evaluated by mean differences (MD). The random-effectsmodelwasappliedformeta-analytic calcu-lations.Statistical heterogeneity wasquantified usingthe
I2 test. When thevalues ofI2 weregreater than 30%,the
resultswereconsideredheterogeneous.
Publication bias was investigated by the analysis of invertedfunnelplot.8Theoriginalarticlefromthepublished
study that has been identified as a source of publication biasfortheresultswasexcludedduringtheanalysisof sen-sitivityandhomogeneity.The original articlesused inthe calculations were indicated by the last name of the first authorfollowed by theyear ofpublicationtopresent the meta-analysisresults.
Analysisofsensitivityanduniformity
Thesensitivityanalysiswasperformed bycomparing sepa-ratelytheresultsofstudiesofgoodandpoormethodological quality.8 The search for statisticalheterogeneity was
per-formedbysuccessivemeta-analysis,withdrawingastudyat atimeuntiltheidentificationoftheheterogeneitysource. Theheterogeneity search wasperformed in meta-analysis withI2testgreaterthan30%.
Trialsequentialanalysis
Weplan touse the trial sequential analysis(TSA) for the variablemortality.9TSAprovideslimitsthatareintendedto
monitor thevalues for themagnitude ofthe effectbeing evaluated in an intervention, so that subsequent meta-analysiscan generate reliable results.9 A part of the TSA
The estimate calculation of how many patients would be needed to obtain viable conclusions was obtained by multiplyingthesamplesizecalculationresultforindividual searchesperformedinaconventionalmannerbyan adjust-mentfactorbasedontheexistingdiversity(heterogeneity) betweenthestudies.9Conventionalcalculationtoestimate
thesamplesizewasperformedbyconsideringconventional values(typeIerrorprobabilityof5%andstatisticalpowerof 80%).Thesecalculationswereperformedusingthelate mor-talityincidencevalue, seenintheGAgroup,foundinthis systematic review and aiming at a relativerisk reduction of25%.Theadjustmentfactorbasedondiversityusedwas 50%, considering that the statistical heterogeneity above thisvalueisconsideredhigh.
Results
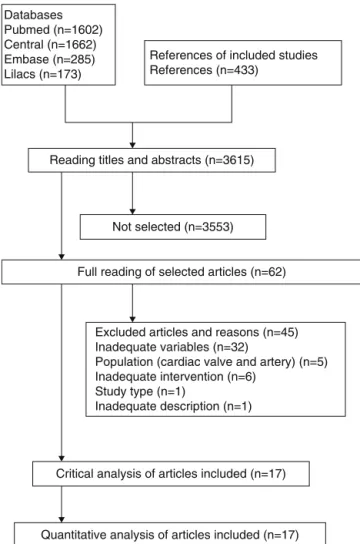
Weidentified3615titlesandabstractsbythesearch strat-egyandalsobyanalyzingthereferencesofstudiesthatwere selectedfor theassessmentof methodologicalquality.We identified17originalarticlesthat mettheinclusion crite-riaofthissystematicreview(Fig.1).10---26Thetotalnumber
ofpatients studied inthe 17articles identifiedwas2477. TheKappaIndexAgreementbetween reviewerswas0.92.
Databases Pubmed (n=1602) Central (n=1662) Embase (n=285) Lilacs (n=173)
References of included studies References (n=433)
Reading titles and abstracts (n=3615)
Not selected (n=3553)
Full reading of selected articles (n=62)
Critical analysis of articles included (n=17)
Quantitative analysis of articles included (n=17) Excluded articles and reasons (n=45) Inadequate variables (n=32)
Population (cardiac valve and artery) (n=5) Inadequate intervention (n=6)
Study type (n=1)
Inadequate description (n=1)
Figure 1 Flowchart of the included and excluded studies accordingtoPRISMAstatementrecommendation.
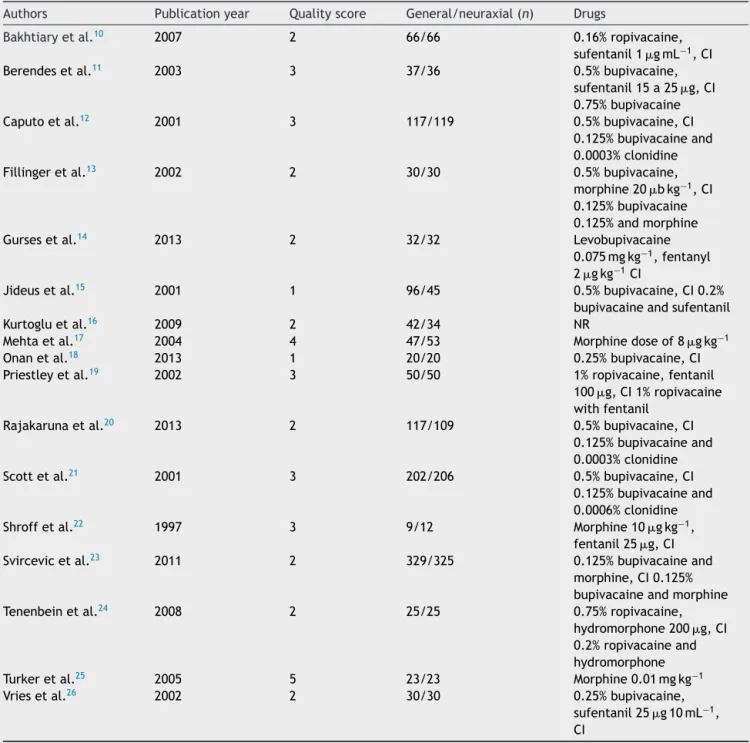
Table 1 shows a summary of the studies included in the meta-analysis.10---26
Primaryoutcome
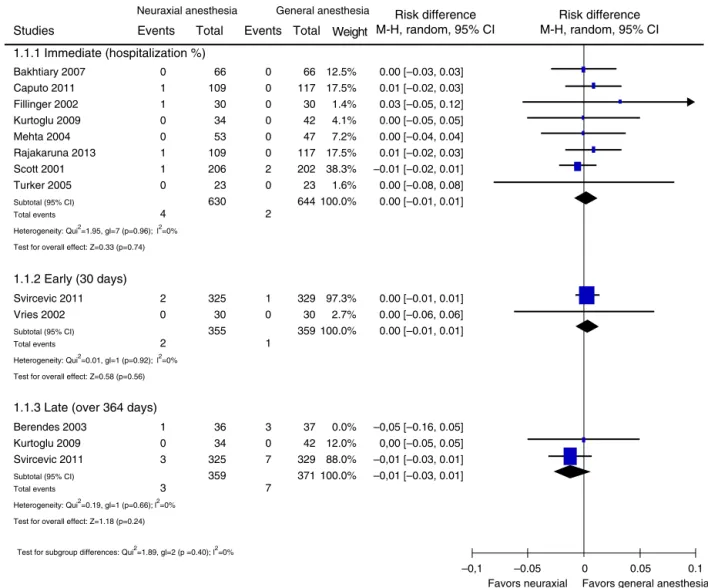
The primaryoutcome wasassessed in 11 original articles with different follow-up times.10---13,16,17,20,21,23,25,26
There-fore,thestudiesweregroupedforanalysisaccordingtothe follow-uptimeasimmediate(duringhospitalization),early (30days),andlate(over 364days).Therewasno statisti-callysignificant differenceintheassessedfollow-uptimes (Fig.2).
Theforestplotshowstheriskdifferenceandthe corre-sponding95%CIforeachstudy(Fig.2).Itisobservedthat all95%CIcrossedthelineofstatisticalinvalidity.The dia-mondplotinthevariousfollow-uptimeassessedalsocrossed the line of statistical invalidity. Considering the immedi-atemortalityap-value=0.74(RD=0.00;95%IC=−0.01to 0.01;1274participants).Consideringtheearlymortalitya
p-value=0.56 (RD=0.00; 95% IC=−0.01 to0.01; 714 par-ticipants). Considering the late mortality a p-value=0.24 (RD=−0.01;95%IC=−0.03to0.01;730participants).Itis concludedthattherewasnostatisticallysignificant differ-enceregarding the studiedparameter. It is observed that there was no statistical heterogeneity in the assessment of immediate mortality (I2=0%; p=0.96), early mortality
(I2=0%;p=0.92),andlatemortality(I2=0%;p=0.66).
Secondaryoutcomes
The secondary outcome arrhythmia was assessed in 11 originalarticles.10,19,21,24---26Theanalysisintheoriginal
arti-cles was performed only during the hospital stay. There was a significant difference in the parameter analyzed (Fig.3).
The forest plot shows the relative risk and the corre-sponding 95% CI for each study (Fig. 3). It is noted that the95%CIof3 studiesdidnotcrossthelineof statistical invalidityindicatingthatNAhasaprotectiveeffectforthe emergenceofarrhythmias.10,12,21Thediamondplotalsodid
notcrossthelineofstatisticalinvalidityshowinga protec-tiveeffectinfavor ofNA. Thisanalysisp-valuewasequal to0.02(RR=0.68;95%CI=0.50---0.93;1363participants).It is concludedthattherewasnostatisticallysignificant dif-ferenceinregardingthestudiedparameter.Itisnotedthat therewasstatisticalheterogeneity in thisvariable assess-ment(I2=35%;p=0.12).
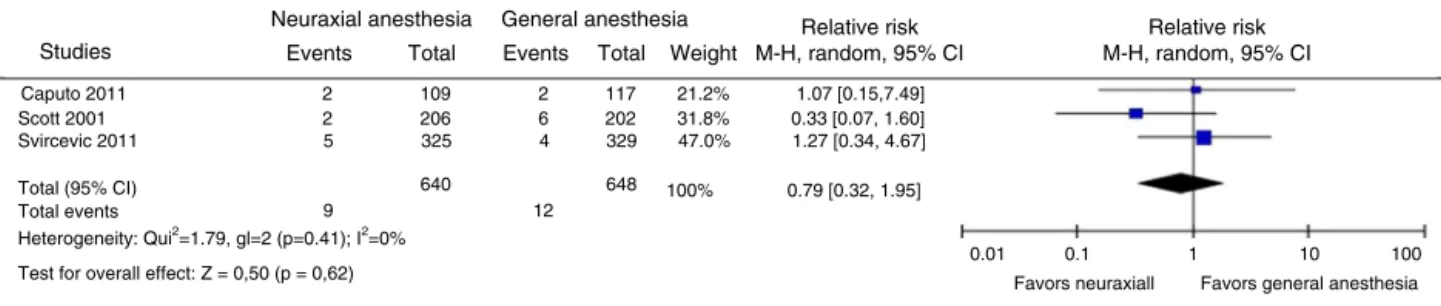
Thesecondaryoutcomestrokewasassessedinthree orig-inalarticles.12,21,23Theanalysisintheoriginalarticleswas
performedonlyduringthehospitalstay.Therewasno sta-tistically significant difference in the assessed parameter (Fig.4).
Table1 Summaryofstudiesincludedinmeta-analysis.
Authors Publicationyear Qualityscore General/neuraxial(n) Drugs
Bakhtiaryetal.10 2007 2 66/66 0.16%ropivacaine, sufentanil1gmL−1,CI
Berendesetal.11 2003 3 37/36 0.5%bupivacaine,
sufentanil15a25g,CI
0.75%bupivacaine
Caputoetal.12 2001 3 117/119 0.5%bupivacaine,CI
0.125%bupivacaineand 0.0003%clonidine
Fillingeretal.13 2002 2 30/30 0.5%bupivacaine,
morphine20bkg−1,CI
0.125%bupivacaine 0.125%andmorphine
Gursesetal.14 2013 2 32/32 Levobupivacaine
0.075mgkg−1,fentanyl 2gkg−1CI
Jideusetal.15 2001 1 96/45 0.5%bupivacaine,CI0.2%
bupivacaineandsufentanil
Kurtogluetal.16 2009 2 42/34 NR
Mehtaetal.17 2004 4 47/53 Morphinedoseof8
gkg−1
Onanetal.18 2013 1 20/20 0.25%bupivacaine,CI
Priestleyetal.19 2002 3 50/50 1%ropivacaine,fentanil
100g,CI1%ropivacaine
withfentanil
Rajakarunaetal.20 2013 2 117/109 0.5%bupivacaine,CI
0.125%bupivacaineand 0.0003%clonidine
Scottetal.21 2001 3 202/206 0.5%bupivacaine,CI
0.125%bupivacaineand 0.0006%clonidine
Shroffetal.22 1997 3 9/12 Morphine10
gkg−1,
fentanil25g,CI
Svircevicetal.23 2011 2 329/325 0.125%bupivacaineand
morphine,CI0.125% bupivacaineandmorphine
Tenenbeinetal.24 2008 2 25/25 0.75%ropivacaine,
hydromorphone200g,CI
0.2%ropivacaineand hydromorphone
Turkeretal.25 2005 5 23/23 Morphine0.01mgkg−1
Vriesetal.26 2002 2 30/30 0.25%bupivacaine,
sufentanil25g10mL−1,
CI
n,numberofparticipants;CI,continuousinfusion;NR,notreported.
theassessedparameter. Itisnotedthattherewasno sta-tistical heterogeneity in this variable assessment (I2=0%;
p=0.41).
Thesecondaryoutcomeacutemyocardialinfarctionwas assessedinthreeoriginalarticles.12,23,26Theanalysisinthe
original articles was performed only during the hospital stay.Therewasnostatisticallysignificantdifferenceinthe assessedparameter(Fig.5).
The forest plot shows the relative risk and the corre-sponding95%CIforeachstudy(Fig.5).Itisnotedthatall 95%CIofthethreeoriginalarticlescrossedthelineof statis-ticalinvalidityindicatingnobeneficialeffectintheNAand
GAcombination.Thediamondplotalsocrossedthelineof statisticalinvalidityshowingnoprotectiveeffectinfavorof NA.Thep-valueofthisanalysiswasequalto0.90(RR=0.96; 95%CI=0.52---1.79; 940participants). It is concludedthat therewasnostatisticallysignificantdifferenceregardingthe studiedparameter.Itisnotedthattherewasnostatistical heterogeneityinthisvariableassessment(I2=0%;p=0.61).
The secondary outcome hospital stay was assessed in threeoriginalarticles.14,18,26Theanalysisintheoriginal
Neuraxial anesthesia General anesthesia Risk difference
M-H, random, 95% CI
Risk difference M-H, random, 95% CI Events
Studies
1.1.1 Immediate (hospitalization %)
1.1.2 Early (30 days)
Total Events Total Weight
Bakhtiary 2007 0 66 0 66 12.5% 0.00 [–0.03, 0.03]
Caputo 2011 1 109 0 117 17.5% 0.01 [–0.02, 0.03]
Fillinger 2002 1 30 0 30 1.4% 0.03 [–0.05, 0.12]
Kurtoglu 2009 0 34 0 42 4.1% 0.00 [–0.05, 0.05]
Mehta 2004 0 53 0 47 7.2% 0.00 [–0.04, 0.04]
Rajakaruna 2013 1 109 0 117 17.5% 0.01 [–0.02, 0.03]
Scott 2001 1 206 2 202 38.3% –0.01 [–0.02, 0.01]
Turker 2005 0 23 0 23 1.6% 0.00 [–0.08, 0.08]
Subtotal (95% CI) 630 644 100.0% 0.00 [–0.01, 0.01]
Total events 4 2
Heterogeneity: Qui2=1.95, gl=7 (p=0.96); l2=0% Test for overall effect: Z=0.33 (p=0.74)
Svircevic 2011 2 325 1 329 97.3% 0.00 [–0.01, 0.01]
Vries 2002 0 30 0 30 2.7% 0.00 [–0.06, 0.06]
Subtotal (95% CI) 355 359 100.0% 0.00 [–0.01, 0.01]
Total events 2 1
Heterogeneity: Qui2=0.01, gl=1 (p=0.92); l2=0% Test for overall effect: Z=0.58 (p=0.56)
Berendes 2003 1 36 3 37 0.0% –0,05 [–0.16, 0.05]
Kurtoglu 2009 0 34 0 42 12.0% 0,00 [–0.05, 0.05]
Svircevic 2011 3 325 7 329 88.0% –0,01 [–0.03, 0.01]
Subtotal (95% CI) 359 371 100.0% –0,01 [–0.03, 0.01]
Total events 3 7
Heterogeneity: Qui2=0.19, gl=1 (p=0.66); l2=0% Test for overall effect: Z=1.18 (p=0.24) 1.1.3 Late (over 364 days)
M-H, Mantel-Haenszel; Random, random effect model; 95% CI, 95% confidence interval.
–0,1 –0.05 0 0.05 0.1
Favors neuraxial Favors general anesthesia
Test for subgroup differences: Qui2=1.89, gl=2 (p =0.40); l2=0%
Figure2 Evaluationofmortality.M---H,Mantel---Haenszel;random,randomeffectmodel;95%CI,95%confidenceinterval.
Neuraxial anesthesia General anesthesia Relative risk
M-H, random, 95% CI
Relative risk M-H, random, 95% CI Events
Studies Total Events Total Weight
M-H, Mantel-Haenszel; random, random effect model; 95% CI, 95% confidence interval.
Bakhtiary 2007 2 66 18 66 4.2% 0.11 [0.03, 0.46]
Caputo 2011 23 109 43 117 19.3% 0.57 [0.37, 0.89]
Fillinger 2002 7 30 7 30 8.5% 1.00 [0.40, 2.50]
Gurses 2013 4 32 5 32 5.5% 0.80 [0.24, 2.71]
Jideus 2001 13 45 29 96 15.8% 0.96 [0.55, 1.66]
Kurtoglu 2009 0 34 1 42 1.0% 0.41 [0.02, 9.74]
Priestley 2002 11 50 10 50 11.0% 1.10 [0.51, 2.36]
Scott 2001 21 206 45 202 17.8% 0.46 [0.28, 0.74]
Tenenbein 2008 6 25 9 25 9.2% 0.67 [0.28, 1.59]
Turker 2005 3 23 4 23 4.5% 0.75 [0.19, 2.98]
Vries 2002 4 30 2 30 3.4% 2.00 [0.40,10.11]
Total (95% CI)
Total events 94
650 173
713 100% 0.68 [0.50,0.93]
0.02 0.1 1 10 50
Favors neuraxial Favors general anesthesia
Heterogeneity: Qui2=15.27, gl=10 (p=0.12); I2=35% Test for overall effect: Z=2.38 (p=0.02)
Neuraxial anesthesia General anesthesia Events
Total Total Weight
Events
Relative risk M-H, random, 95% CI
Relative risk M-H, random, 95% CI Studies
Caputo 2011 2 109 2 117 21.2% 1.07 [0.15,7.49] Scott 2001 2 206 6 202 31.8% 0.33 [0.07, 1.60] Svircevic 2011 5 325 4 329 47.0% 1.27 [0.34, 4.67]
Total (95% CI) 640 12 9
648 100% 0.79 [0.32, 1.95] Total events
Heterogeneity: Qui2=1.79, gl=2 (p=0.41); I2=0% Test for overall effect: Z = 0,50 (p = 0,62)
0.01 0.1 1 10 100 Favors neuraxiall Favors general anesthesia
M-H, Mantel-Haenszel; random, random effect model; 95% CI, 95% confidence interval.
Figure4 Evaluationofstroke.M---H,Mantel---Haenszel;random,randomeffectmodel;95%CI,95%confidenceinterval.
General anesthesia Neuraxial anesthesia
Events Total
Events Total Weight
Relative risk M-H, random, 95% CI
Relative risk M-H, random, 95% CI
M-H, Mantel-Haenszel; random, random effect model; 95% CI, 95% confidence interval.
Caputo 2011 1 109 0 117 3.8% 3.22 [0.13, 78.17] Svircevic 2011 17 325 18 329 92.4% 0.96 [0.50, 1.82] Vries 2002 0 30 1 30 3.8% 0.33 [0.01, 7.87]
Total (95% CI) Total events
Heterogeneity: Qui2=0.98, gl=2 (p=0.61); I2=0% Test for overall effect: Z=0.13 (p=0.90)
19
476 100% 18
0.96 [0.52,1.79] 464
0.005 0.1 1 10 200 Favors neuraxial Favors general anesthesia
Studies
Figure5 Evaluationofacutemyocardialinfarction.M---H,Mantel---Haenszel;random,randomeffectmodel;95%CI,95%confidence interval.
Theforestplotshowsthemeandifferenceandthe corre-sponding95%CIforeachstudy(Fig.6).Itisnotedthattwo 95%CIofthethreeoriginalarticlescrossedthelineof statis-ticalinvalidityindicatingthattherewasabeneficialeffect intheNAandGAcombination.14,18 The diamondchartdid
notcrossthelineofstatisticalinvalidityshowingno protec-tiveeffectinfavorofNA.Thep-valueofthisanalysiswas equalto0.06(MD=−1.94;95%CI=−3.99to0.12;164 par-ticipants).Itwasconcludedthattherewasnostatistically significant differenceregarding theassessedparameter. It isnotedthattherewasstatisticalheterogeneityinthis vari-ableassessments(I2=95%;p<0.00001).
Thesecondaryoutcomelengthofintensivecareunitstay was assessed in two original articles.13,14 The analysis in
theoriginalarticleswasperformedonlyduringthehospital
stay.There wasa statisticallysignificantdifferenceinthe assessedparameter(Fig.7).
Theforestplotshowsthemeandifferenceandthe cor-responding95%CIforeachstudy(Fig.7).Itisobservedthat one95%CI fromthetwooriginal articlescrossedthe line ofstatistical invalidityindicating thattherewasa benefi-cialeffectin theNAand GAcombination.14 The diamond
plotcrossedthelineofstatisticalinvalidityindicatingthat therewas a protective effect in favor of neuraxial anes-thesia.The p-value of thisanalysiswas lessthan 0.00001 (MD=−2.09;95%CI=−2.92to−1.26;124participants).It wasconcludedthattherewasnostatisticallysignificant dif-ference regardingthe studied parameter. Itis notedthat therewasnostatisticalheterogeneityinthisvariable assess-ment(I2=0%;p=0.67).
Neuraxial anesthesia
Studies Mean
Gurses 2013 Onan 2013 Vries 2002
4.9 6.1 5.9
1.5 0.3 2.4
32 20 30
8.8 7.2 6.6
1.7 1.1 3.3
32 20 30
34.2% 35.3% 30.5%
–3.90 [–4.69, –3.11] –1.10 [–1.60, –0.60] –0.70 [–2.16, 0.76]
–1.94 [–3.99, 0.12]
–10
Favors neuraxial Favors general anesthesia
–5 0 5 10
100% 82 82
Total (95% CI)
Heterogeneity: Qui2=37.17,gl=2 (p<0.00001); I2
=95%
Test for overall effect: Z = 1.85 (p=0.06)
IV, interval variable; random, random effect model; 95% CI, 95% confidence interval.
SD Total Mean SD Total Weight
General anesthesia IV mean difference,
random, 95% CI
IV mean difference, random, 95% CI
Neuraxial anesthesia
Studies Média
31.7 1.5
21.3 1.6
30 32
30 3.6
44 1.8
30 32
0.2% 98.8%
62
62 100%
1.70 [–15.79, 19.19] –2.10 [–2.93, –1.27]
–2.09 [–2.92, –1.26]
Favors general anesthesia Favors neuraxial
–20 –10 0 10 20 Total (95% CI)
Fillinger 2002 Gurses 2013
Heterogeneity: Chi2=0.18,gl=1 (p=0.67); I2=0% Test for overall effect: Z=4.92 (p<0.00001)
IV, interval variable; random, random effect model; 95% CI, 95% confidence interval. DP Total Média DP Total Peso
General anesthesia Weight IV mean difference, random, 95% CI
Weight IV mean difference, random, 95% CI
Figure7 Evaluation of lengthof intensive care unitstay. IV, interval variable; random,random effect model;95% CI, 95% confidenceinterval.
Neuraxial anesthesia
Studies Events
32 35 Caputo 2011
Scott 2001
Total (95% CI)
Total events 67 50
100%
315 319
27 23 109 206
117 202
55.2% 44.8%
1.27 [0.82, 1.98] 1.49 [0.98, 1.90]
1.37 [0.98, 1.90]
Favors neuraxial Favors general anesthesia 0.05 0.2
1
5 20 Heterogenidade: Chi2=0.23,gl=1 (p=0.63); I2=0%
Test for overall effect: Z=1.87 (p=0,06)
M-H, Mantel-Haenszel; random, random effect model; 95% CI, 95% confidence interval.
Total Events Total Weight
General anesthesia Relative risk M-H, random, 95% CI
Relative risk M-H, random, 95% CI
Figure 8 Evaluation of blood transfusion. M---H, Mantel---Haenszel; random, random effect model; 95% CI, 95% confidence interval.
Thesecondaryoutcomebloodtransfusionwasassessedin twooriginalarticles.12,21Theanalysisintheoriginalarticles
wasperformedonlyduringthehospitalstay.Therewasno statisticallysignificantdifferenceintheassessedparameter (Fig.8).
The forest plot shows the relative risk and the corre-sponding95%CIforeachstudy(Fig.8).Itisnotedthatthe two95%CIoftheoriginalarticlesdidnotcrossthelineof statisticalinvalidityindicatingthattherewasnobeneficial effectintheNAandGAcombination.Thediamondplothas notcrossthelineofstatisticalinvalidityindicatingno pro-tective effectinfavor of NA. The p-value of thisanalysis wasequalto 0.06(RR=1.37; 95% CI=0.98---1.90; 634 par-ticipants). It is concluded that there was no statistically significant difference regarding the studied parameter. It isnotedthattherewasnostatisticalheterogeneityinthis variableassessment(I2=0%;p=0.63).
The secondary outcome qualityof lifewasanalyzed in oneestudy.12 The meta-analytic calculationscouldnotbe
performed. Individualdata from thisstudy show that the bestresultwasfoundintheNAgroupcombinedwithGA.
Thesecondaryoutcomesreoperationfrequency,degree of satisfaction, and postoperative cognitive dysfunction were not assessed in any study selected for quantitative analysisoftheresults.
Sensitivityanduniformityanalysis
The sensitivity analysis was performed for the primary outcome and for the following secondary outcome varia-bles:arrhythmia,stroke,acutemyocardialinfarction.The
variableslengthofhospitalstay,lengthofstayinintensive care unit, and blood transfusion could not be analyzed becausethestudieswereclassifiedinthesamecategory.
Therewasnostatisticallysignificantdifferencebetween studies of good and bad quality regarding the variable mortality. Considering the group of good quality studies,
p-value=0.55 (RD=0.01; 95% CI=−0.01 to0.03; 372 par-ticipants). Considering the group of bad quality studies,
p-value=0.40(RD=0.00;95%CI=−0.01to0.01;1208 par-ticipants).
Thearrhythmiavariableshowedthatthestudiesofgood quality are statistically significant, those of poor quality have no statistically significant difference, and the anal-ysis of all the articles does not change the end result, confirming that NA associated with GA reduces the inci-denceofarrhythmias.Consideringthegroupofgoodquality studies, p-value=0.004 (RR=0.60;95% CI=0.43---0.85; 780 participants).Consideringthegroupofbadqualitystudies,
p-value=0.63 (RR=0.91; 95% CI=0.62---1.33; 451 partici-pants).Considering allthe goodand poorquality studies,
p-value=0.002(RR=0.69;95%CI=0.55---0.87;1231 partici-pants).
The stroke variable showed no statistically significant difference between the studies of good and bad quality. Consideringthegroupofgoodqualitystudies,p-value=0.31 (RR=0.53; 95% CI=0.15---1.80; 634 participants). Consid-ering the group of bad quality studies, p-value=0.72 (RR=1.27;95%CI=0.34---4.67;654participants).
226 participants). Considering the group of bad quality studies, p-value=0.76 (RR=0.90; 95% CI=0.47---1.75; 714 participants).
Statisticalheterogeneityoccurredinthearrhythmiaand hospitalstayanalyzes.Inthearrhythmiavariableanalysis, the successive meta-analysis method allowed the identi-fication of a study as the source of heterogeneity.10 The
inverted funnel plotshowed thatthis study isresponsible for publication bias and its exclusion makes the analy-sis homogeneous without changing the beneficial effect of using the NA and GA combination. The meta-analysis resultwithoutthestudyresponsibleforthepublicationbias shows that, from this analysis, p-value=0.002 (RR=0.69; 95%CI=0.55---0.87;1231participants;I2=0%;p=0.46).The
originalarticleresponsibleforthesourceofstatistical het-erogeneity of thelength ofhospital stay variableanalysis wasidentified.14 The statisticalheterogeneity mayhave a
medical explanation, as a catheter was used in cervical spacewithcaudal-to-thoracicsegmentsintroduction,unlike other studies performingthoracic catheterinsertion. The analysiswithoutthestudyidentifiedasthesourceof statisti-calheterogeneityshowssignificantresults,p-value<0.0001 (MD=−1.06;95%CI−1.53to−0.59;100participants),and favorabletotheuseofNA.
Trialsequentialanalysis
TheTSAcouldnotbeperformedduetothelimitationofdata foundinthearticlesincludedinthissystematicreviewfor themortalityvariable.Thelowfrequencyoftheeventand thelimitednumberofparticipantslimitedthecalculation.
The numberof studiedpatientsrequired for the meta-analysisresultstobeconsideredreliablewasestimated.The eventrateinthecontrolgroup(GAgroup)ofthis system-aticreviewwas2%(7/371).The25%relativeriskreduction reduced this value to 1.5%. The sample size calculation withatypeIerror probabilityof5% andstatisticalpower of80%indicated theneedfor4664 participants.The sam-plesizewasmultipliedbytheadjustmentfactorbasedon thediversityamongstudies,leadingtoan estimated9264 moreparticipants tomake ourconclusion reliable for the mortalityvariable.
Discussion
Briefly, the results of this meta-analysis are: (a) lack of statistical significance between the two anesthetic tech-niquesusedforcoronaryarterybypass,regardingmortality; (b)lowerincidenceofarrhythmiaswhenNAwasused;(c) shorterlengthofstayintheintensivecareunitwhenNAwas used.
There are some limitations in this systematic review. First,wenotetheexistenceofheterogeneityamongstudies insomeanalyzes;however,thestrategyusedforthe analy-sisofsensitivityandhomogeneitywaseffectivetoidentify the source of statistical heterogeneity that was explored bythereviewers.Second,thearrhythmiavariableshowed statisticaldifferenceinfavorofNA,butexcludingthe stud-iesusingclonidineinneuraxialblockadeandnotusingitin the group receivingGA alone, thatstatistical significance does not occur demonstratingthat possiblythe beneficial
effectofusingNAforcoronaryarterybypassmayberelated tothe␣2-adrenergicagonisteffectofthisdrugwhenused via epidural route. Third, the number of studies used in the analysis of the length of stay in intensive care unit variablewas small,and the result may have occurred by chance.
Stroke, acute myocardial infarction, hospital stay,and bloodtransfusionvariableswerenotstatisticallysignificant consideringthedatafromthestudiesincludedin this sys-tematicreview. The analysis of thesevariables may have beenlimitedbythesmallnumberofidentifiedstudies,small numberofeventsreportedinstudies,andidentificationof studieswithsmallsamples.The lackofstatistically signif-icantdifferencemaybeduetothesmallstatisticalpower presentintheseanalyzes.
Thesensitivityanalysisthatevaluatedtheresultsofgood andpoorqualitystudieswasnotalimitationtothisresearch, astheseparation of studies toperformthe meta-analysis didnot change the final results or the conclusions drawn fromthe analyzes of the full set of original articles. The homogeneity analysis of the length of hospital stay vari-ableshowed that statistical significance occurs when the source of statistical heterogeneity is excluded from the meta-analysis,showing thatthe result for this variableis unbound.
Qualityof lifewasevaluatedina study.12 The variable
presencein only onestudy prevents the executionof the meta-analysiscalculations.8Thestudyinquestionalsocould
nothavebeenincluded intheanalysisbecauseitassessed onlytheparticipantswholivedinoneofthecountries par-ticipating inthe study,and thiscould beconsidered data measurementbias.8
Reoperation frequency, degree of satisfaction, and postoperativecognitivedysfunctionvariableswerenot eval-uatedintheincludedstudies,highlightingtheneedformore randomizedtrialswithadequatestatisticalpowerandgood methodological quality to evaluate the relevant clinical variables.Aclinicaltrialwithrandomallocationperformed individuallyshould consideranadequate statistical power foritsexecution.Consideringthe5%mortalityinthegroup undergoing GA, the 3% mortality in the NA alone group, a statistical power of 80%, and a type I error probabil-ityof 5%, it is needed 1500 participants in each analysis group.
Themaximumnumberofparticipantsassessedinthis sys-tematicreviewforthemortalityvariablewas1274,ofwhich 714for mortality upto30 daysafter surgeryand 730 for latemortality.TheexecutionofpartoftheTSAcalculation indicatedthatitnecessary toevaluate9264extra partici-pants.Consideringtheexecutionofthiscalculationandthe numberofstudyparticipants,wenotethatthenumberof participantswassmall,whichimpliestheexistenceofahigh probabilityforthepresenceoftypeIIerrorinthis system-aticreviewthatmayhavebeenresponsibleforthelackof statisticalsignificanceintheprimaryoutcome.
Asystematicreviewpublishedin2009evaluatedtheuse of spinal anesthesia in heart surgery, but concluded that theuseof NAwasunfavorable,considering themortality, myocardial infarction, and hospital stay variables.27 That
Asystematicreviewpublishedin2011evaluatedtheuse of epiduralanalgesia in heart surgery.28 The authors
con-cluded that the use of NA is beneficial, considering the reducedriskofpostoperativesupraventricular arrhythmias andrespiratorycomplications.Thatreviewdidnot individ-ualize data for coronary artery bypass. The authors used an instrumentnot validated to assess the methodological qualityoftheincludedstudies,contrarytothissystematic reviewthatusedanestablishedsystem fortheanalysisof thisitem.
Asystematicreviewpublishedin2012evaluatedtheuse ofepiduralanesthesiainheartsurgery.29Theonlyassessed
variable was the presence of atrial fibrillation, but the results showed marked heterogeneity whose source was notidentified by the authors, contrary tothis systematic review.
Ourstudy hasemerged asan attempt to optimizethe resultsthatwerefoundinothersystematicreviewsinthe lit-erature,individualizingthedataforcoronaryarterybypass andtoupdatetheknowledge basedonscientificevidence inthisareaofknowledgeinordertoassistthephysicianin makingdecisionsbeforethepatientwhenchoosingthe anes-thetictechnique.Fromthissystematicreview,weconclude thatthe combination of neuraxialanesthesia andgeneral anesthesiaforcoronaryarterybypassshowednostatistical differenceinmortalityandisassociatedwithalower inci-dence ofpostoperative arrhythmias andshorter length of stayintheintensivecareunit.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.NalysnykL,FahrbachK,ReynoldsMW,etal.Adverseeventsin coronaryarterybypassgraft(CABG)trials:asystematicreview andanalysis.Heart(BritishCardiacSociety).2003;89:767---72. 2.Frogel JK, GandretiN. Should thoracic epidural/spinal
anal-gesiabeusedforcoronaryarterybypassgrafting?In:Fleisher LA,editor.Evidence-basedpracticeofanesthesiology.3rded. Philadelphia:Saunders;2013.p.477---83.
3.Liu S,Carpenter RL, NealMJ.Epidural anesthesia and anal-gesia: their role in postoperative outcome. Anesthesiology. 1995;82:1474---506.
4.Ho AMH, Chung DC, Joynt GM. Neuraxial blockade and hematoma in cardiac surgery: estimating the risk of a rare adverse event that has not (yet) occurred. Chest. 2000;117:551---5.
5.MoherD,LiberatiA,TetzlaffJ,etal.Preferredreportingitems for systematicreviewsandmeta-analyses:thePRISMA state-ment.BMJ.2009,33dom9:b2535.
6.Jadad AR, Moore RA, Carroll D,et al. Assessing thequality ofreportsofrandomizedclinicaltrials:isblindingnecessary? ControlClinTrials.1996;17:1---12.
7.Review Manager (RevMan) [Computer program].
Ver-sion 5.1. Copenhagen: The Nordic Cochrane Centre,
The Cochrane Collaboration; 2011. Available from:
http://ims.cochrane.org/revman/[accessed05.02.14].
8.Higgins JPT, Green S. Cochrane Handbook for
System-atic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration; 2011. Available from: www.cochrane-handbook.org[accessed05.02.14].
9.Brok J, Thorlund K, Gluud C, et al. Trial sequential analy-sisreveals insufficient informationsize and potentially false positive results in many meta-analyses. J Clin Epidemiol. 2008;61:763---9.
10.BakhtiaryF,TherapidisP,DzemaliO,etal.Impactofhigh tho-racicepiduralanesthesiaonincidenceofperioperativeatrial fibrillation inoff-pump coronarybypass grafting: a prospec-tiverandomized study. JThorac Cardiovasc Surg. 2007;134: 460---4.
11.BerendesE,SchmidtC,VanAkenH,etal.Reversiblecardiac sympathectomybyhighthoracicepiduralanesthesiaimproves regionalleftventricularfunctioninpatientsundergoing coro-nary artery bypass grafting: a randomized trial. Arch Surg. 2003;138:1283---90.
12.CaputoM,AlwairH,RogersCA,etal.Thoracicepidural anesthe-siaimprovesearlyoutcomesinpatientsundergoingoff-pump coronary artery bypass surgery: a prospective, randomized, controlledtrial.Anesthesiology.2011;114:380---90.
13.FillingerMP,YeagerMP,DoddsTM,etal.Epiduralanesthesiaand analgesia:effectsonrecoveryfromcardiacsurgery.J Cardio-thoracVascAnesth.2002;16:15---20.
14.Gurses E,Berk D,Sungurtekin H, et al.Effects of high tho-racicepiduralanesthesia onmixed venousoxygensaturation in coronary artery bypass grafting surgery. Med Sci Monit. 2013;19:222---9.
15.JideusL,JoachimssonPO,StridsbergM,etal.Thoracicepidural anesthesia does not influence the occurrence of postopera-tive sustained atrial fibrillation. Ann Thorac Surg. 2001;72: 65---71.
16.KurtogluM,AtesS,BakkalogluB,etal.Epiduralanesthesia ver-susgeneralanesthesiainpatientsundergoingminimallyinvasive directcoronaryarterybypasssurgery.AnadoluKardiyolDerg. 2009;9:54---8.
17.MehtaY,KulkarniV,JunejaR,etal.Spinal(subarachnoid) mor-phineforoff-pumpcoronaryarterybypasssurgery.HeartSurg Forum.2004;7:E205---10.
18.OnanB,OnanIS,KilickanL,etal.Effectsofepiduralanesthesia onacuteandchronicpainaftercoronaryarterybypassgrafting. JCardSurg.2013;28:248---53.
19.PriestleyMC,CopeL,HalliwellR,etal.Thoracicepidural anes-thesiaforcardiacsurgery: theeffectsontracheal intubation timeandlengthofhospitalstay.AnesthAnalg.2002;94:275---82. 20.RajakarunaC,RogersC,PikeK,etal.Superiorhaemodynamic stabilityduringoff-pumpcoronarysurgerywiththoracic epidu-ral anaesthesia: resultsfrom a prospective randomized con-trolledtrial.InteractCardiovascThoracSurg.2013;16:602---7. 21.ScottNB,TurfreyDJ,RayDA,etal.Aprospectiverandomized
studyofthepotentialbenefitsof thoracicepidural anesthe-siaandanalgesiainpatientsundergoingcoronaryarterybypass grafting.AnesthAnalg.2001;93:528---35.
22.Shroff A, Rooke GA, Bishop MJ. Effects of intrathecal opi-oid on extubation time, analgesia, and intensive care unit stayfollowingcoronaryarterybypassgrafting.JClinAnesth. 1997;9:415---9.
23.SvircevicV,NierichAP,MoonsKG,etal.Thoracicepidural anes-thesiaforcardiacsurgery:arandomizedtrial.Anesthesiology. 2011;114:262---70.
24.Tenenbein PK, Debrouwere R, Maguire D, et al. Thoracic epidural analgesia improves pulmonary function in patients undergoingcardiacsurgery.CanJAnaesth.2008;55:344---50. 25.TurkerG,GorenS,SahinS,etal.Combinationofintrathecal
morphineandremifentanilinfusionforfast-trackanesthesiain offpumpcoronaryarterybypasssurgery.JCardiothoracVasch Anesth.2005;19:708---13.
surgery:theroleofepidural anesthesia.JCardiothoracVasc Anesth.2002;16:21---6.
27.ZangrilloA,BignamiE,Biondi-ZoccaiGG,etal.Spinalanalgesia incardiacsurgery: ameta-analysis ofrandomizedcontrolled trials.CardiothoracVascAnesth.2009;23:813---21.
28.SvircevicV,vanDijkD,NierichAP,etal.Meta-analysisof tho-racicepiduralanesthesiaversusgeneralanesthesiaforcardiac surgery.Anesthesiology.2011;114:271---82.