BrazJOtorhinolaryngol.2015;81(4):447---450
www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
CASE
REPORT
Primary
mantle
cell
lymphoma
of
the
nasopharynx:
a
rare
clinical
entity
夽
Linfoma
primário
de
célula
do
manto
da
nasofaringe:
uma
entidade
clínica
rara
Ji-Hun
Kang
a,
Young-Dae
Park
a,
Chang-Hoon
Lee
b,
Kyu-Sup
Cho
a,∗aDepartmentofOtorhinolaryngologyandBiomedicalResearchInstitute,PusanNationalUniversityHospital,Busan,
RepublicofKorea
bDepartmentofPathology,PusanNationalUniversitySchoolofMedicine,PusanNationalUniversityHospital,Busan,
RepublicofKorea
Received24January2015;accepted19February2015 Availableonline9June2015
Introduction
Mostnon-Hodgkin’slymphomas(NHL)intheheadandneck regiondevelop in the extranodallymphatic system of the Waldeyerring.1WithintheWaldeyerring,thenasopharynx
is thesecond most commonsite ofdisease afterthe ton-sil.Primarynasopharyngeallymphomaismuchlesscommon, occurringinonly8%ofallNHLoftheheadandneck,2and
diffuselargeB-celllymphoma(DLBCL)isthemostcommon histologictype.3 Mantlecelllymphoma(MCL) is adistinct
subtype of B-cell lymphoma andcomprises approximately 5---10%ofalllymphomas.4MCLischaracterizedbyan
aggres-sive clinical course, and there is a pattern of frequent relapse after conventional chemotherapy.4 MCLs involving
the nasopharynx and oropharynxare extremely rare, and havenotbeenreportedintheliterature,tothebestofthe
夽
Pleasecitethisarticleas:KangJ-H,ParkY-D,LeeC-H,Cho,K-S. Primarymantlecelllymphomaofthenasopharynx:arareclinical entity.BrazJOtorhinolaryngol.2015;81:447---50.
∗Correspondingauthor.
E-mails:choks@pusan.ac.kr,ckssmj@hanmail.net(K.S.Cho).
authors’knowledge.Thiscasereportdescribesarare clini-calpresentationofprimaryMCLarisinginthenasopharynx andextendingtotheoropharynx.Thisstudywasapproved bytheinstitutionalreviewboardofPusanNational Univer-sityHospital.
Case
report
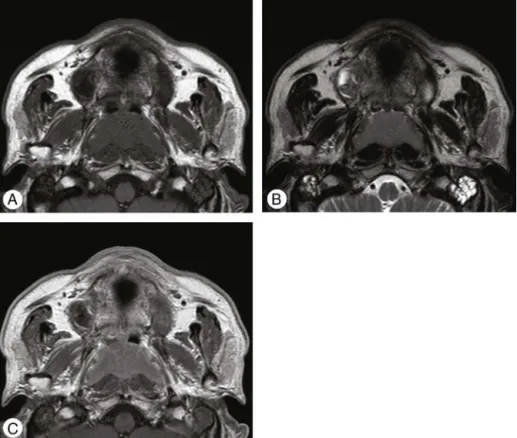
A 66-year-old male with both nasal obstruction and ear fullnessvisitedtheauthors’clinic.Hedeniedfever,chills, and weight loss. The endoscopic examination revealed obstructionofbothposteriorchoanaebyahuge nasopharyn-gealmass,accompanied bynecroticmaterial. Nocervical lymphadenopathies were felt. Paranasal sinus computed tomography (CT) showed a homogenous solid mass with mildenhancementinvolvingbothnasopharyngealwallsand extending to the upperoropharynx (Fig.1). On magnetic resonance (MR) images, the homogenous mass demon-stratedlowsignalintensityonT1-weightedimages(T1WIs), intermediate signal intensity on T2WIs, and moderate enhancement on gadolinium-T1WIs (Fig. 2). A transnasal endoscopicbiopsyofnasopharyngealmasswasperformed. Histopathologicexamination showeddiffuse infiltration of
http://dx.doi.org/10.1016/j.bjorl.2015.02.002
448 KangJ-Hetal.
Figure1 Computedtomography(CT)ofparanasalsinus.Contrast-enhancedCTimages showabilateral,homogenous, mildly-enhancedsolidmassfromnasopharynxextendingtoupperoropharynxonaxial(A),coronal(B),andsagittal(C)view.
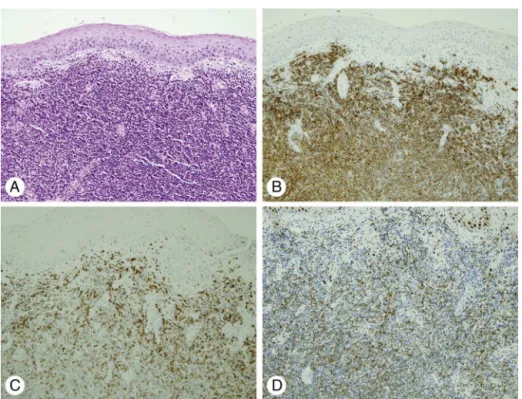
smalllymphocyticcellswithmildnuclearatypia(Fig.3A). Immunochemicalstainingrevealedthattheneoplastic lym-phocyteswerestronglypositiveforCD20,CD5,andcyclin D1(Fig.3B---D).ThesefindingswereconsistentwithMCL.An uppergastrointestinalendoscopy,bonescan,andCTscanof thechest,abdomen,andpelviswereallreportedasnormal.
Abonemarrowbiopsyshowednoabnormalities.Thepatient wasstaged IE according totheAnn Arborstaging system. The patientreceivedfourcyclesof R-CHOPchemotherapy and radiotherapy (total dose, 40Gy). After 24 months of post-therapyfollow-up,thepatientexhibitednoevidence ofresidualorrecurrentdisease.
PrimaryMCLofthenasopharynx 449
Figure3 Histopathologicfindingsofnasopharyngealmass.(A)Microscopicfindingshowsdiffuseinfiltrationofsmalllymphocytic cellswithmildnuclearatypia(H&E,×200).Immunohistochemicalstainingshowsstrongpositivitytoanti-CD20(B),anti-CD5(C),
andanti-cyclinD1(D)antibody(×200).
Discussion
MCL is a subtype of B-cell lymphoma, derived from CD5-positive antigen-naïve pregerminal center B-cells within the mantle zone that surrounds normal germinal center follicles.5MCLcellsgenerallyover-expresscyclinD1duetoa
t(11:14)chromosomaltranslocationinthedeoxyribonucleic acid.5,6The causeisunknown andnoinherited
predisposi-tionhasbeenidentified.Itaccountsfor about5%ofadult NHL inthe UnitedStates, andmoreover, theincidenceof MCL has been increasingover the last decade, especially among elderly patients.7 The population most commonly
affectedconsistsofmenwithamedianageof60years.7
Clinically,MCL usuallypresents withstageIII or IV dis-easeandextensivelymphadenopathy,hepatosplenomegaly, andbonemarrowinvolvement.One-quarterofpatientsare found to also have peripheral blood involvement.5
Extra-nodaldisease occurslessfrequently, butwhen present,it typically may be found in the gastrointestinal tract and Waldeyer’s ring.6 In the extremely rare cases when MCL
involvesthenasopharynx,itpresentswithanasopharyngeal mass.DescribedhereinisthefirstcasereportofMCLarising inthenasopahrynx.
MCL is diagnosed by examination of affected tissue, obtained from a biopsy of a lymph node, tissue, bone marrow,orbloodphenotype,whichshowsthetypical mor-phologyofmonomorphicsmall-tomedium-sizedlymphoid cellswithirregularnuclearcontours.8 Immunophenotyping
is commonly used with MCL cells that are CD20+, CD5+, and positive for cyclin D1, whereas negative for CD10 and Bcl-6.8 In most of patients with MCL, t (11:14) and
othergeneticchangescauseexcessproductionofcyclinD1, which is an early event in MCL.9 MCL is presently staged
by using a modified Ann Arbor system. This patient had stageI disease at presentation, withlesions of the naso-pharynxandoropharynx,whichwassuccessfullytreatedby immunochemotherapywithradiotherapy.
MostMCLpatientsreceivetreatmentfollowingdiagnosis andstaging.Anumberofchemotherapyandrituximab com-binations,suchasR-CHOP,areusedtotreatpatients with MCL.Althoughtheadditionofrituximab,amonoclonal anti-body,has significantly improved theoverall outcome, the five-yearoverallsurvivalisaslowas40%inMCLpatients.5,10
Conclusion
ThefirstcaseofprimaryMCLarisinginthenasopharynxand extendingtotheoropharynxhasbeendescribed,whichwas successfully treated by immunochemotherapy with radio-therapy.This entity shouldbe recognizedand adequately diagnosedbecauseit mayhave a moreaggressive clinical course than other types of NHL in the head and neck. A detailedmorphologicevaluationwiththorough immunophe-notypingisessentialforanaccuratediagnosis.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
450 KangJ-Hetal.
2.ChoKS,KangDW,KimHJ,LeeJK,RohHJ.Differential diag-nosisofprimarynasopharyngeallymphomaandnasopharyngeal carcinomafocusingonCT,MRI,andPET/CT.OtolaryngolHead NeckSurg.2012;146:574---8.
3.Allam W, Ismaili N, Elmajjaoui S, Elgueddari BK, Ismaili M, ErrihaniH.Primarynasopharyngealnon-Hodgkinlymphomas:a retrospective reviewof26Moroccanpatients.BMC Ear Nose ThroatDisord.2009;9:11.
4.ZhouY,WangH,FangW,RomaguerJE,ZhangY,DelasalleKB, etal.IncidencetrendsofmantlecelllymphomaintheUnited Statesbetween1992and2004.Cancer.2008;113:791---8.
5.KangBW,SohnSK,MoonJH,ChaeYS,KimJG,LeeSJ,etal. Clin-icalfeaturesandtreatmentoutcomesinpatientswithmantle celllymphomainKorea:studybytheconsortiumforimproving survivaloflymphoma.BloodRes.2014;49:15---21.
6.Chang CC,Rowe JJ,HawkinsP,SadeghiEM.Mantlecell lym-phoma of the hard palate: a case report and review of
thedifferential diagnosis based on thehistomorphology and immunophenotypingpattern. OralSurgOralMedOralPathol OralEndod.2003;96:316---20.
7.Aschebrook-Kilfoy B, Caces DB, Ollberding NJ, Smith SM, ChiuBC.Anupwardtrend intheage-specific incidence pat-ternsformantlecell lymphomaintheUSA.LeukLymphoma. 2013;54:1677---83.
8.Vose JM. Mantle cell lymphoma: 2013 update on diagnosis, risk stratification, and clinicalmanagement. Am JHematol. 2013;88:1082---8.
9.Pileri SA, Falini B. Mantle cell lymphoma. Haematologica. 2009;94:1488---92.