rev bras hematol hemoter. 2 0 1 5;37(6):423–425
w w w . r b h h . o r g
Revista
Brasileira
de
Hematologia
e
Hemoterapia
Brazilian
Journal
of
Hematology
and
Hemotherapy
Letter
to
the
Editor
Diagnostic
approach
to
hemolytic
anemias
in
the
adult
DearSir,
Eventhoughhemolyticanemias(HAs)arenotverycommon, their diagnosis remains a big challenge for hematologists and clinicians.Wehopethat this summarywillcontribute withvaluableinformationaboutasubjectthathasbeen lit-tledescribedinthemedicalliterature,andwillhelptoclarify thediagnosticapproachtoguidespecifictreatmentdepending onthecausativecondition.
ItisknownthatHAsare agroupofdisorders character-izedbyaprematureredbloodcell(RBC)destruction(lessthan 120days),1,2 thatexceedsthecompensatorycapacityofthe bonemarrowtoincreaseRBC productionandkeepupwith the loss.1–3 Usually HAs are diagnosed through laboratory tests,however, the patient’shistory and physical examina-tionarecrucialastheyprovideimportantinformationabout the presenceof hemolysis and its probable etiology.3,4 For example,ifinaddition tothe classicsymptomsofanemia (paleness, fatigue, dyspnea, palpitations), findings such as familialorpersonalhistoryofjaundice,exposuretotoxics,leg ulcers,lymphadenopathies,hepatomegaly or splenomegaly mayhelptoelucidatethecauseoftheanemia.1,3,4
Regardingtheetiology,HAscanbeclassifiedasinherited oracquiredandwhenconsideringthesiteofhemolysis,RBCs canbedestroyedinthecirculation(intravascular)orwithin macrophagesinthespleenorliver(extravascular).Fromthe clinicalperspective,HAscanbeacuteorchronicandaccording tothelocationoftheabnormalityresponsibleforthe hemoly-sis,theymaybeduetointrinsic(intracorpuscular)orextrinsic (extracorpuscular)defects.2–4Itisimportanttomentionthat mostintrinsicdefectsareinherited,andmostextrinsicones areacquired,2however,therearesomeexceptionstothisrule. Forexample,paroxysmalnocturnalhemoglobinuria(PNH)is anacquiredHAproducedbyanintrinsicdefect4and glucose-6-phosphatedehydrogenase(G6PD)deficiencyisaninherited intrinsicdefectthatistriggeredbyanexternalfactor.2
Althoughtherearedifferentwaysofapproachingthe diag-nosisofHAs,itisfirstnecessarytoidentifythepatientwithHA andcollectdataonhemolysis.ThedestructionofRBCsinHAs ischaracterizedbyanincreasedbreakdown ofhemoglobin
whichresultsinunconjugatedhyperbilirubinemiaclinically evidencedbyjaundice,increasedlactatedehydrogenase (cel-lular destruction), and reticulocytosis, which is a normal compensatory response of the bone marrow to the RBC loss.Additionally,decreasedlevelsofplasmahaptoglobin,a markerofRBC destruction, areevidenced1–3 regardlessthe site ofhemolysis(intravascularor extravascular).5 Incases ofsevere acute intravascular HAs, the haptoglobin-binding capacityreachesitssaturationpoint,andfreehemoglobinis filteredbytheglomerulusandhemoglobinuriaisseen.3,6Also, hemosiderinuriamaybepresentinlong-termintravascular hemolysis.3,6Ontheotherhand,ifthehemolysisis extravas-cular,urobilinogenmayappearintheurineorfeces.6
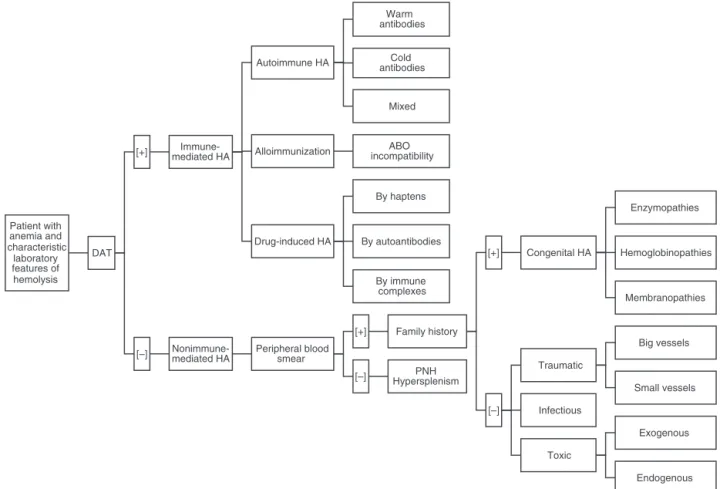
Oncewehaveapresumptivediagnosis,amulti-step pro-cedureisrequired,4beginningwithadirectantiglobulintest (DAT) or direct Coombs test.6,7 This isthe exam ofchoice becauseitwillclassifythehemolysisintoanimmuneor non-immune etiology.6,7 AlthoughDAT helps tocategorize HAs into twogroups,resultsmustbeinterpretedinthe context oftheclinicalconditionsassomeconditionsmaybe incor-rectlyclassified.7,8 Thisiswhythe DATshould befollowed byaperipheralbloodsmear(PBS)andaninvestigationofthe familyhistory.6AsimpleapproachtoidentifyandclassifyHAs basedontheworksofGonzálezMesonesetal.6andothers3,4,8 ispresentedinFigure1.
424
rev
bras
hema
tol
hemoter.
2
0
1
5;
3
7(6)
:423–425
Table1–Themostcommoncausesofhemolysisclassifiedbytype.
Defect
Intrinsic Inherited
Enzymopathies
Hemoglobinopathies
Membranopathies
Immune-mediated
Acquired
Traumatic
Infectious
Toxic
Entrapment
Endogenous Exogenous Small Vessels
Big Vessels Drug-induced Alloimmunization
Autoimmune hemolytic anemia
hemolytic anemia Extrinsic
Etiology Abnormality Examples
G6PD deficiency, pyruvate kinase deciciency
Thalassemia, sickle cell anemia Hereditary spherocytosis, elliptocytosis
Nocturnal paroxysmal hemoglobinuria Warm antibodies [IgG]
Idiopathic, lymphoproliferative (CLL, NHL), SLE, non-lymphoid
malignancies Cold antibodies [IgG]
mononucleosis, lymphoproliferative (Waldenstroms), paroxysmal cold hemogloburina
Mixed [warm and cold antibodies] Idiopathic, SLE, lymphoma ABO incompatibility
By haptens
By autoantibodies
By immune complexes
Quinidine, hydrochlorothiazide, sulfonamides, tetracycline Prostheses
diclofenac
Valves, TIPS
Microangiophatic hemolytic anemia TTP, HUS, HELLP, DIC Bartonella, Babesia, Plasmodium
Clostridium
Arsenic, lead or copper poisoning Snake or spider bite
Wilson disease
Hypersplenism
Alpha-methyldopa, L-dopa, ibuprofen, Penicillin, cephalosporin
Idiopathic, M. pneumoniae, •
•
•
•
•
•
•
•
Site of hemolysis
EV
EV IV
IV
IV
EV IV
EV
IV
IV
IV
IV
IV EV
EV
EV (also EV)
or EV
G6PD:glucose-6-phosphatedehydrogenase;CLL:chroniclymphocyticleukemia;NHL:non-Hodgkinlymphoma;SLE:systemiclupuserythematous;TIPS:
transjugularintrahepaticportosystemicshunt;TTP:thromboticthrombocytopenicpurpura;HUS:hemolyticuremicsyndrome;HELLP:hemolysis,elevated
revbrashematolhemoter.2015;37(6):423–425
425
Patient with anemia and characteristic laboratory features of hemolysis
DAT
[+] mediated HA
Immune-Autoimmune HA
Warm antibodies
Cold antibodies
Mixed
Alloimmunization incompatibilityABO
Drug-induced HA
By haptens
By autoantibodies
By immune complexes
[–] Nonimmune-mediated HA Peripheral blood smear
[+] Family history
[+] Congenital HA
Enzymopathies
Hemoglobinopathies
Membranopathies
[–]
Traumatic
Big vessels
Small vessels
Infectious
Toxic
Exogenous
Endogenous PNH
Hypersplenism [–]
Figure1–Asimpleapproachtoidentifyandclassifyhemolyticanemias.DAT:directantiglobulintest;HA:hemolytic
anemia;PNH:paroxysmalnocturnalhemoglobinuria.
acongenitalHAincludingdisordersofenzymes(G6PD defi-ciency,pyruvatekinasedeficiency)hemoglobin(thalassemia, sicklecellanemia)or ofthe membrane(hereditary sphero-cytosis,elliptocytosis).Likewise,traumatichemolysis(ofbig orsmallvessels),infectious(Bartonella,Babesia,Plasmodium)or toxic(exogenousorendogenous)pathologiesshouldbetaken intoaccountifthereisanabnormalPBSintheabsenceof fam-ilyhistory.Incontrast,ifthePBSisnormal,hypersplenismor PNHshouldbeconsidered.Adetailedlistofthemostcommon causesofhemolysisclassifiedbytypeispresentedinTable1.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.EvansER.Diagnosisofthehemolyticanemias.CalifMed. 1951;75(4):271–5.
2.UcarK.Clinicalpresentationandmanagementofhemolytic anemias.Oncology(WillistonPark).2002;169(Suppl10):163–70.
3.DhaliwalG,CornettPA,TierneyLMJr.Hemolyticanemia.Am FamPhysician.2004;69(11):2599–606.
4.GuillaudC,LoustauV,MichelM.Hemolyticanemiainadults: maincausesanddiagnosticprocedures.ExpertRevHematol. 2012;5(2):229–41.
5.ShihAW,McFarlaneA,VerhovsekM.Haptoglobintestingin hemolysis:measurementandinterpretation.AmJHematol. 2014;89(4):443–7.
6.GonzálezMesonesB,GonzálezdeVillambrosiaA,BatlleA, InsunzaA.Protocolodiagnósticodelasanemiashemolíticas. Medicine.2012;11(20):1246–9.
7.ZantekND,KoepsellSA,TharpDRJr,CohnCS.Thedirect antiglobulintest:acriticalstepintheevaluationofhemolysis. AmJHematol.2012;87(7):707–9.
8.BassGF,TuscanoET,TuscanoJM.Diagnosisandclassification ofautoimmunehemolyticanemia.AutoimmunRev. 2014;13(4–5):560–4.
EloyF.Ruiz∗, MiguelA.Cervantes
UniversidadPeruanaCayetanoHeredia,Lima,Peru
∗Correspondingauthorat:Av.ElPolo740,EdificioC,Oficina313,
SantiagodeSurco,Lima,Peru.
E-mailaddress:eloy.ruiz.m@upch.pe(E.F.Ruiz).
Received26June2015 Accepted19August2015 Availableonline9October2015
http://dx.doi.org/10.1016/j.bjhh.2015.08.008