w w w . r b o . o r g . b r
Update
article
Stress
fractures:
definition,
diagnosis
and
treatment
夽
Diego
Costa
Astur
∗,
Fernando
Zanatta,
Gustavo
Gonc¸alves
Arliani,
Eduardo
Ramalho
Moraes,
Alberto
de
Castro
Pochini,
Benno
Ejnisman
UniversidadeFederaldeSãoPaulo,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received5January2015 Accepted5February2015
Availableonline30December2015
Keywords:
Stressfracture/epidemiology Stressfracture/physiopathology Stressfracture/diagnosis Stressfracture/classification Stressfracture/treatment
a
b
s
t
r
a
c
t
StressfractureswerefirstdescribedinPrussiansoldiersbyBreithauptin1855.Theyoccur astheresultofrepeatedlymakingthesamemovementinaspecificregion,whichcanlead tofatigueandimbalancebetweenosteoblastandosteoclastactivity,thusfavoringbone breakage.Inaddition,whenaparticularregionofthebodyisusedinthewrongway,a stressfracturecanoccurevenwithouttheoccurrenceofanexcessivenumberoffunctional cycles.Theobjectiveofthisstudywastoreviewthemostrelevantliteratureofrecentyears inordertoaddkeyinformationregardingthispathologicalcondition,asanupdatingarticle onthistopic.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
Fraturas
por
estresse:
definic¸ão,
diagnóstico
e
tratamento
Palavraschave:
Fraturasporestresse/epidemiologia Fraturasporestresse/fisiopatologia Fraturasporestresse/diagnóstico Fraturasporestresse/classificac¸ão Fraturasporestresse/tratamento
r
e
s
u
m
o
AfraturaporestressefoidescritainicialmenteemsoldadosprussianosporBreithauptem 1855eocorrecomooresultadodeumnúmerorepetitivodemovimentosemdeterminada regiãoquepodelevarafadigaedesbalanc¸odaatuac¸ãodososteoblastoseosteoclastose favorecerarupturaóssea.Alémdisso,quandousamosumadeterminadaregiãodocorpo demaneiraerrônea,afraturaporestressepodeocorrermesmosemqueocorraumnúmero excessivodeciclosfuncionais.Oobjetivodesteestudoérevisaraliteraturamaisrelevante dosúltimosanosparaagregarasprincipaisinformac¸õesarespeitodessapatologiaemum artigodeatualizac¸ãodotema.
©2015SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevierEditora Ltda.Todososdireitosreservados.
夽
WorkperformedattheSportsTraumatologyCenter,EscolaPaulistadeMedicina,UniversidadeFederaldeSãoPaulo,SãoPaulo,SP, Brazil.
∗ Correspondingauthor.
E-mail:mcastur@yahoo.com(D.C.Astur). http://dx.doi.org/10.1016/j.rboe.2015.12.008
Introduction
Stressfractures werefirst described inPrussian soldiersby Breithauptin1855.1–3Theywerenamed“marchfractures”and
theircharacteristicswereconfirmed40 yearslaterwiththe adventofradiography.1,2In1958,Devasmadethefirstreport
onstressfracturesinathletes.1–3
Thisinjuryoccurs asaresultofhighnumbersof occur-rences of cyclical overloading of intensity lower than the maximumbonestrength,onnon-pathologicalbonetissue.4–6
Thesefracturesmaybethefinalstageoffatigueor insuf-ficiencyofthe boneaffected.6 Fatiguefractures occur after
formationandaccumulationofmicrofracturesinnormalbone trabeculae.Ontheotherhand,fracturesresultingfrombone insufficiencyoccurinbonethatismechanicallycompromised and generally presents low bonemineral density.6 In both
situations,imbalancebetweenthebonethatisformedand remodeledandthebonethatitreabsorbedwillresultin dis-continuityofthe boneatthe siteaffected.7,8 Theaimhere
wastopresentanupdatingarticleonthistopicandcondense themaininformationobtainedthroughthemostimportant studiespublishedoverthelastfewyears.
Epidemiology
Population
Runners,soldiersanddancersarethemainvictimsofstress fractures.6,9,10
Anatomicalregion
All the bonesofthe humanbody are subject tofracturing causedby stress.Thisstress isclosely related tothe daily practicethatathletesundertake.Thepredominanceofstress fracturesinthelowerlimbs,overfracturesintheupperlimbs, reflectsthecyclical overloadingthatistypicallyexertedon bonesthatbearthebodyweight,incomparisonwithbones thatdonothavethisfunction.3Stress fracturesaremostly
commonlydiagnosedinthetibia,followedbythemetatarsals (especially the second and third metatarsals) and by the fibula.3,11Stressfracturesintheaxialskeletonareinfrequent
andaremainlylocatedintheribs,parsinterarticularis,lumbar vertebraeandpelvis.11–13
Typesofsport
Runnerspresentgreatestincidenceofstressfracturesinlong bonessuchasthetibia, femurand fibula,andalsopresent fracturesinthebonesofthe feetandsacrum.11,12 Typesof
sport inwhichthe upperlimbsare used, suchasOlympic gymnastics,14 tennis,baseball andbasketballmay resultin
fracturesduetostress.Thebonemostaffectedistheulna, especiallyinitsproximalportion,whilethedistalextremity ofthe humerusisalsoaffected.6,11,13Stress fracturesoccur
mainlyintheribsingolfersandrowers11,13Jumpers,bowlers
anddancerspresentgreatestriskofinjurytothelumbarspine andpelvis.11
Sex
Amongathletes,thedifferenceintheincidenceofstress frac-turesbetweenmenandwomenisminimal.Itisbelievedthat theintensityandtypeofcontrolledtrainingforeachathlete andthephysicalpreparationthatalreadyexistsdiminishthe impactofthetrainingprogram.9,15Inthemilitarypopulation,
theincidenceofstressfracturesamongfemalesisgreaterthan amongmen.16,17
Physiopathology
Sixtoeightweeksafterasuddenandnon-gradualincrease intheintensityofanathlete’sornewpatient’sphysical activ-ity,thiscyclicalandrepetitivephysiologicaloverloadingmay leadtotheappearanceofmicrofracturesandmaynotallow thebonetissuetohavesufficienttimetoundergo remodel-ing andadapt tothe newcondition, andthustorepairthe microlesion.4–6,10,18,19 Theload appliedis considered to be
insufficienttocauseanacutefracture,butthecombinationof overloading,repetitivemovementsandinadequaterecovery timemakethisachronicinjury.11Elasticdeformationoccurs
initially,andthisprogressestoplasticdeformityuntilitfinally resultsinmicrofracturing.Ifthisisnottreated,itwillevolve tocompletefracturingoftheboneaffected.10Thebonerepair
processinstressfracturesdiffersfromtheprocessincasesof commonacutefracturesandonlytakesplacethroughbone remodeling,i.e.reabsorptionoftheinjuredcellsand replace-mentwithnewbonetissuetakeplace.19
Markeyalsoproposedthatthemusclemassactstoward dispersing and sharing impactloads on the bonetissue.20
Therefore,whenfatigue,weaknessormuscleunpreparedness occur,thisprotectiveactionislostandtheriskofbonetissue lesionsincreases.16,20
Risk
factors
The factors associatedwith increasedrisk ofdevelopment ofstress fracturescan bedividedinto extrinsicand intrin-sic factors. This makes stress fractures multifactorial and difficult to control.8,9,20–23Extrinsic factors relate to sports
movements,nutritionalhabits,equipmentusedandthetype ofground.8,9,14,20–23
Abruptincreasesintheintensityandvolumeoftraining areoftenenoughforlesionstodevelop.6,9–11Equipmentsuch
asfootwearthathaslowimpactabsorption,iswornout(more thansixmonthsofuse)orisabadfitfortheathlete’sfootmay causeinjuries.8,23 Thequalityofthetrainingtrackmayalso
beariskfactor,whenitisuneven,irregularorveryrigid.17,24
Lastly,iftheathlete’sfitnesslevelisinsufficientforthesports movement orfunctionaltechnique,thismayleadtoinjury, sometimes withoutthe number ofrepetitions having been veryhigh.8,25
Theintrinsicfactors relatetopossibleanatomical varia-tions,muscleconditions,hormonalstates,gender,ethnicity orage.8,9,20–22
reality,hormonal,nutritional,biomechanicalandanatomical alterationsarethetruefactorsthatfavorappearanceofstress fracturesinwomen.11,24
Agealsocannotbeconsideredtobeariskfactorin isola-tionforstressfractures.11,23,27StudiesconductedintheUnited
States have attempted to evaluate the incidence of these injuriesamongwhite andblackathletes,withoutobserving anysignificantdifferences.11,13 Inamilitarypopulation,the
incidenceamongwhiteswastwiceashighasamongblacks, withoutanydifferencebetweenthesexes.Thiswasattributed tobonedensityanditsbiomechanics.24
There is an inverse relationship between bone mineral densityandtheriskofstressfractures.8,10,28Inadequate
nutri-tional intake may alter bone metabolism and predispose towardappearanceofstressfractures.8,10,29
Lowlevelsofphysicalandmuscleconditioningarealsoan importantriskfactorforthegenesisofthisproblem.6,8,10,30,31
Furthermore,rigidpescavus,discrepancyofthelowerlimbs, shorttibia,genuvalgum,increasedQangle,bodymassindex lowerthan21kg/m2 andshortstature shouldalsobetaken
into consideration in analyzing the risk factors for stress fractures.6,8,9,21,32
Somestudieshavealsosuggestedthatstiffnessofthefeet, alterationstotheplantararchandlimitationsofdorsiflexion duetoshorteningofthesuraltricepsmayberiskfactors.8,10,33
Runnerswhosehindfootpresentseversion,particularlywith excessive pronation, and athletes witha pronounced high archhaveariskofdevelopingstressfracturesthatisup to 40%higher.10,21,33,34Moreover,hyperpronationoftheforefoot
predisposestowardincreasedriskofstressfracturesinthe fibula.35Stressfracturesinthesecondmetatarsalhavebeen
correlatedwithpresenceofMorton’sneuroma, hypermobil-ityofthefirstmetatarsalandarelativeincreaseinthelength ofthesecondmetatarsal.20,33Althoughuseoforthosesand
footwearthatismoreappropriatetheoreticallydecreasesthe incidenceofstress fractures,the number ofstudies inthe literatureremainsinsufficienttosustainthistheory.10,34
Otherauthorshavealsoconsideredthatthefollowingare riskfactors:smoking,physicalactivityoffrequencylessthan threetimesaweekandconsumptionofmorethan10doses ofalcoholicdrinkperweek.6
Physical
examination
Physicalexaminationofstressfracturesisverysensitivebut unspecific.20,36Patientspresentincreasedsensitivity,painand
edemaatthelesionlocationafteranabruptand/orrepetitive increaseinphysicalactivitywithinsufficientrestintervalsfor physiologicaltissuerecovery.6Initially,thepainisreducedand
alleviatedthroughrestandthisallowsunimpairedphysical activity.However,iftheaggressivemovementismaintained, the injury will progress, thus resulting in increased pain andlimitationofpracticingthis movement.9,20 Information
regardinganypreviousfractures,weight,height,bodymass indexand its changes over the last 12 months, menstrual andpubertyhistoryandnutritionalevaluationsisimportant foridentifyingpossibleintrinsicriskfactorsforinjuryduring physicalexaminations.10
Clinical testssuchasuse oftherapeuticultrasound and tuningforksare alsouseful indiagnosticinvestigations on stressfractures.3Whenuseddirectlyonthesiteofthe
sus-pectedlesion,theymaytriggerorworsenthepainbecause of the great local osteoclastic reabsorption, which results in injury to the periosteum.3,37 In addition, the skipping
rope test (hop test) can be used: this consists of asking the patient to hop on the spot while putting weight on the limb that is under investigation. The test is positive whenit triggersstrong orincapacitatingpainintheregion injured.6,38
Somelaboratorytestsmaybeusefulininvestigatingstress fractures:serumlevelsofcalcium,phosphorus,creatinineand 25(OH)D3. Nutritional markers should be requested in the presenceofclinicalconditionsofweightlossandanorexia. Hormonal levels(FSHand estradiol)shouldbeinvestigated whenthereisahistoryofdysmenorrhea.10
Imaging
examinations
Imagingexaminationsarefundamentalfordiagnosing, prog-nosingandfollowingupstressfractures.6
Simpleradiography (X-ray) isthe initialimaging exami-nationbecauseofitseaseofaccessandlowcost.4,13,36,38–42
However, it has a high false-negative rate, given that the alterations caused bystress fractures onlyappearon such examinationsatalatestage(twotofourweeksafterthestart ofthepain),whichmaydelaythediagnosis.6,14,18,43Initially,a
subtleweakradiolucentareacanbeobserveddirectlyonthe bonetissueaffected and/orsclerosis,periostealthickening, corticalchangescomprisingdiminishedcorticalbonedensity (gray cortex) and/or appearance ofa delicate fracture line. Finally, an attempt bythe organism toform abone callus isobserved,withendostealthickeningandsclerosis,which arethecommonestfindings.6,10,14,38,44Thesignknownasthe
dreadedblacklineoccursintheanteriorcorticalboneofthe tibiaandsuggeststhepresenceofafracturewithapoor prog-nosisandahighprobabilityofevolutiontoacompletefracture becauseofitslocationinaregionofbonetensionandpoor vasclarization.44
Computed tomography (CT)is used mainly when there is a contraindication against using magnetic resonance imaging.43–46 Chronic and quiescent lesions may be more
evident in this examination than on magnetic resonance imagingorbonescintigraphybecausetheypresentlowbone turnover.46SinglephotonemissionCT(SPECT)hasbeen
par-ticularlymoreusefulininvestigatingstressfracturesinvolving the dorsal spine, and specifically in pars interarticularis (spondylolysis).6,45,46
Nuclear medicine using triple-phase scintigraphy (technetium-99m)presents significant sensitivity(74–100%) toboneremodelingandshowsimagingalterationsthreeto fivedaysafterthestartofsymptoms.3,6,41,42,47The
radiophar-maceutical becomes concentrated in the regions affected anddetectsareasofboneremodeling,microfracturesofthe trabecular bone,periosteal reactionand formation ofbone callus.46
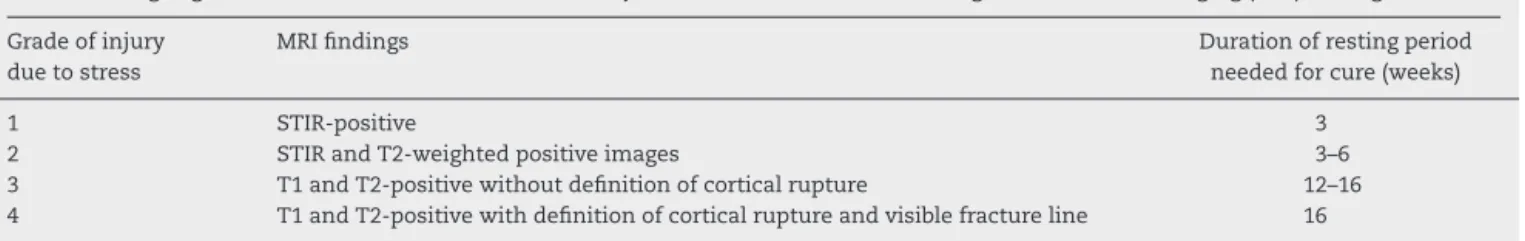
Table1–ClassificationofArendtandGriffiths.
Stages/gradesofArendtandGriffithsforboneinjuriesduetostress,basedonmagneticresonanceimaging(MRI)findings
Gradeofinjury duetostress
MRIfindings Durationofrestingperiod
neededforcure(weeks)
1 STIR-positive 3
2 STIRandT2-weightedpositiveimages 3–6
3 T1andT2-positivewithoutdefinitionofcorticalrupture 12–16
4 T1andT2-positivewithdefinitionofcorticalruptureandvisiblefractureline 16
fractures. It is recommended by the American College of Radiology as the preferred examination in the absence of radiographic alterations.6 The abnormalities caused bythe
fracturecanbeidentifiedonetotwodaysafterthestartof thesymptoms,6,10,12,38,41,43,46,48withearlydetectionofedema
in the bone tissue and adjacent areas.10,41,46 This
exami-nationmakesitpossibletodifferentiatemedullarydamage from cortical,endosteal and periostealdamageallows gra-dationofthelesionsregardingtheirseverityandprognosis.6
Intramedullaryendosteal edemaisoneofthefirstsigns of boneremodelingandmaycontinuetobepresent forup to sixmonthsafterthefracturehasbeendiagnosedandtreated, whilethecorticalmaturationandremodelingtakeplace.16,48
Medullaryedemaorsignsofbonestressmayalsobepresentin asymptomaticphysicallyactivepatients,withoutany correla-tionwithincreasedincidenceofstressfractures,especiallyin thetibiainmarathonrunners.46Thefracturelineisless
com-monlyvisible.10Itpresentssensitivityslightlygreaterthanor
equaltothatofscintigraphy,butitisconsideredtobeamore specificexamination.6,38,41
Classification
Fracturescanandshouldbeclassifiedsothattheprognosis andtreatmentcanbemeasuredandthusgiverisetoabetter resultforthepatient.
Arendt and Griffiths apud Royer et al.11 used imaging
parametersobtainedthroughMRItodividestressfractures intofourstages.Theaimofthisclassificationistodefinethe lengthofrestingtimethat isneededforareturn tosport, according to the patient’s current stage. These stages can alsobeusedforreevaluationduringfollow-upofthelesion.7
Lesionstreatedatstage1requireanaverageof3.3weeksof resting,whilethoseatstage4require14.3weeks7(Table1).
Table2–Classificationoflow-riskstressfractures.
Low-riskstressfractures
Upperlimbs Clavicle,scapula,humerus,olecranon,ulna, radius,scaphoid,metacarpals
Lowerlimbs Femoraldiaphysis,tibialdiaphysis,fibula, calcaneus,metatarsaldiaphyses
Thorax Ribs
Dorsalspine Parsinterarticularis,sacrum Pelvis Ischiopubicrami
Table3–Classificationofhigh-riskstressfractures.
High-riskstressfractures Femoralneck(superolateral) Anteriorcorticalboneofthetibia Medialmalleolus
Navicularbone
Baseofthesecondmetatarsal Talus
Patella
Sesamoids(hallux) Fifthmetatarsal
Stressfracturescanalsobeclassifiedashighandlow-risk fractures. The bone location, the prognosis for consolida-tionandtraitsascertainedthroughimagingexaminationsare someofthecharacteristicsthatdefinewhetherthereishigher riskthatastressfracturemightnotevolvesatisfactorilyduring thetreatment6,11(Tables2and3).
Fredericson proposed a stress fracture classification throughusingthe alterationsseenonMRI.Theprogressive stagesoflesionseverityareassessedaccordingtoperiosteal involvement,followedbymedullaryinvolvementandgoing asfarasthepointatwhichthecorticalbonealsobecomes compromised10,41(Table4).
Treatment
Inordertoadequatelytreatstressfractures,itisessentialto identifyriskfactorsthatleadtodisease.Treatmentsforstress fractures are based on preventionofnewepisodes and on recoveryoftheinjuredarea.6,10,20
Table4–Fredericsonclassification.
MRIfindingsaccordingtoFredericson
Lesionstage
0 Normal
1 Periostealedema
2 PeriostealandmedullaryedemaonT2-weighted images
3 PeriostealandmedullaryedemaonT1and T2-weightedimages
Preventionofnewepisodesisachievedthrough modify-ingactivities,correctingsportsmovements,changingsports equipment,changingtraininglocationsthatmightbe favor-ingboneoverloading,changingnutritionalhabits,recognizing hormonal,anatomical andmuscle strength alterationsand recognizinglowcardiomuscularconditioning.20Theidealtype
of footwear for each type of sports practice is the exter-nal factor that has been studied most with regard to the genesisofstressfractures.20Somestudieshaveshownthat
thereislowerincidenceofinjurieswhenrunningonasphalt isreplacedbyrunning onsoftersurfaces,suchasathletics tracks.Nonetheless,otherauthorshavereportedintheir stud-iesthat therewasno relationshipbetweenthesefactors.20
Voloshin49believedthattherewasinterferencebetweenthe
differentshock-absorbingsurfaces:thestressonthebone tis-sueisnotduesolelytothereactionforcesfromtheground. Thecombinedforcesgeneratedbymuscleactionthroughthe athlete’smovementandhisadaptationtothetrainingsurface mayalsobeconsideredtoberiskfactorsforagiventypeof injury.20,49
Thetreatmentsfortheseinjuriescomprisediminutionof theoverloadingonthesiteaffected,medicationforpain con-trolandphysiotherapeuticrehabilitation.6,10,20
Analgesics are used for pain relief.6 Anti-inflammatory
drugs, if used, should be prescribed cautiously and only for short periods. Studies on animals have demonstrated thattheremaybenegativeinterferenceinthebonehealing process.6However,reviewsoftheliteratureconductedmore
recentlyhavereportedthatthereisnoconclusiveevidence regardingthisnegativeaction.50–52
The time taken for fracture consolidation is generally betweenfourand12weekswhenthefracturesarelow-risk.6
Forthemetatarsals,atimeofthreetosixweeksisexpected, whilefor the posteromedial region of the tibial diaphysis, the femurand the pelvis, sixto12 weeks isexpected.10,11
Thepatientshouldbereexaminedeverytwotothreeweeks, tomonitor the changesto the symptoms and pain during restingandrehabilitationperiods.6,53–56INordertomaintain
flexibility,strengthandcardiovascularphysicalconditioning duringthe restingperiod, thepatient needstobeengaged inaphysiotherapy program6,53,54 and acontrolled exercise
program.57
Immobilizationisonlyrarelyusedfortreatingstress frac-turesbecauseofitsdeleteriouseffectsonmuscles,tendons, ligamentsandjoints.5However,therearesomespecifictypes
of fracture for which immobilization is fundamental for obtainingappropriateconditionsforacure:thisisthecase forthenavicularbone,sesamoids,patellaandposteromedial regionofthetibia.5
High-riskfracturescommonlyevolvetonon-consolidation of the bone and surgical intervention by an orthopedist becomesnecessary.6 Stress fractures ofthe lateral cortical
bone(duetotension)atthefemoralneckisassociatedwith catastrophicresults,suchascomplete displacement ofthe femoral head and osteonecrosis, when this is not treated surgically.20,53 Fracturesoftheanterior corticalboneofthe
middle third ofthe tibialdiaphysis are another type that, ifnottreatedsurgically,mostlypresentsanextremelypoor prognosis.20Fracturesofthebaseofthefifthmetatarsaland
ofthenavicularbonecanalsobecitedastypesthatcommonly
requiresurgicalinterventioninordertoachieveasatisfactory resultfromtheirtreatment.20
New
types
of
therapy
Somenewtypesoftherapyforstressfracturesarebeing stud-ied with the aim ofachieving faster consolidation and an earlierreturntophysicalactivities.Thesecanbedividedinto biologicalandphysicalmethods.50
Oxygensupplementationtherapy(hyperbaricoxygen therapy)
In vitro studies have demonstrated that administration of 100%oxygeniscapableofstimulatingosteoblastsand conse-quentlyboneformation.50However,thereisstillnoconsensus
in the literature regarding its benefits for treating stress fractures.50,54
Bisphosphonates
Bisphosphonatessuppressbonereabsorptionandinactivate osteoclasts through their bonding withcalcium phosphate crystals.20,50Theirhighcostandvarioussideeffectsmaybe
thedecidingfactorwithregardtochoosingandattemptingto usethistherapeuticmethod.50,55Thereisnotyetanyscientific
basisfortheirprophylacticuse.50,56
Growthfactorsandgrowthfactor-richpreparations
Growth factorsareapplieddirectlytodiseasedtissueswith the aim of accelerating and promoting their repair. The preliminary results from muscles, tendons and ligaments have been encouraging.50,57 There are only a few studies
on treating stress fractures. Some of them have reported thatwhenthesefactorsare usedduringsurgicaltreatment ofhigh-riskfractures,theymayaccelerateand improvethe recovery.50
Bonemorphogenicproteins
Bonemorphogenicproteinscontainbioactivefactorsthatare responsibleforinducingbonematrixactivitywithan osteoin-ductive function.50 Their primary activity is in relation to
differentiationofmesenchymalcellsintoboneandcartilage tissue-formingcells,throughdirectandosteochondral ossi-fication.Theyhaveanimportantfunctioninrepairingbone lesions.Studiesonanimalshavedemonstratedacceleration of the injury cure process in cases of traumaticfractures, but little can be concluded regarding their use in stress fractures.50
Recombinantparathyroidhormone
Parathormone actstoward regulating serum calcium levels through gastrointestinal absorption, calcium and phospho-rusreabsorptioninthekidney,andcalciumreleasefromthe skeletal tissue.50 Although this initially promotes
isdone intermittentlyin acontrolledmanner, it givesrise toanabolic stimulationofosteoblastsandresultsin forma-tionofbonewithincreasedstrengthanddensity,followedby remodeling.50Studieshavedemonstratedthatthishormone
stimulatesbonerepairthroughbothendochondraland mem-branousmechanisms.50
Low-intensitypulsatileultrasonography
High-frequencysoundwavesthatareabovetheaudiblelimit of human beings interact with bone tissue and the adja-centsofttissuesand generatemicrostressandtensionthat arecapableofstimulatingconsolidation.6,13,50However,their
exactmechanismofactionremainsunknown.19Somestudies
havedemonstrateditsefficacyintreatingstressfractures.50,58
Otherstudieshavecompletelysupporteditsusefortreating thesefractures.6
Applicationofmagneticfields
Magneticfieldscanbeappliedbymeansofadirectcurrentat thefocusofthefracturethroughsurgicalplacementof elec-trodes,useofanelectricalcapacitationfielddeviceoruseof electromagneticfieldpulses.50Thereisstillnoconcrete
evi-denceregardingitsuseinstressfractures.20,50
Criteria
for
return
to
sport
Thetimetakenfromdiagnosis tocureand untilthereturn tosportdependsonmultiplefactorssuchastheinjurysite, sportsactivity, severityoftheinjury andpossibility of cor-rectingriskfactorsthatareintrinsictothepatient.20Low-risk
stressfracturesandnon-surgicaltreatmentusuallymakeit possibleforthepatienttoreturntohisactivitiesfourto17 weeksaftertheinjury.6
Thecriteriathat can beusedforallowing anathlete to returntohispracticemayinclude:totalabsenceofpainat thesiteaffected,especiallyduringsportsmovements;absence ofsymptomsduringpainprovocationtestsattheinjurysite; absenceofabnormalitiesinimagingexaminations;and,above all,comprehensionbythepatient,trainersandtechnicalteam ofthesportregardingtheriskfactorsandconditionsthatled totheinjury,sothatcorrectionscanbemadesoastoprevent recurrenceandreappearanceofinjuries.10
Thegradualdefinitivereturntosportsactivityshouldbe startedafterthepatienthasbeenfreefrompainfor10–14days, with10%increasesintrainingintensityperweek.20,50
Forma-tionofabonecallusandobliterationofthefracturelineon simpleradiographsand,especially,oncomputedtomography scansarethefactorsthatdeterminewhetherthecureprocess forthestressfracturehasbeenadequate.50
Prevention
Althoughseveralmethodsforpreventingstressfractureshave been proposed,onlysomeofthem presentproven validity thatcanjustifytheirrecommendations.6Thepossiblerisk
fac-torsthatcontributetoappearanceofthesefracturesneedto
becarefullystudied,modifiedandfollowedup.6,10 Constant
controlandmodificationofphysicalactivity,withadequate recovery time,are extremelyimportant.6,10 Itisconsidered
thatdailyintakeof2000mgofcalciumand800IUofvitamin D maybeprotectionfactors.6,9 Thekinematicsand
biome-chanicalfactorspredisposingtowardsuchfracturesneedto bemonitoredandcorrected,throughcorrectunderstanding ofthesportsmovements,equipment,orthoses,training sur-faceandalltheotherfactorsthatmaybeinvolvedinsports practice.6,10,50 Some studies have investigated prophylactic
use ofbisphosphonatesforpreventing stressfractures, but thereisstillnoevidenceregardingitsbenefitsinprevention ofthistypeofinjury.6
Complications
Themaincomplicationsoccurincasesofhigh-riskstress frac-tures.Inappropriatemanagementmaycauseprogressionof the fracture to acomplete and displaced fracture line and thus give rise to delayed consolidation, avascularnecrosis and pseudarthrosis.6,20 Furthermore,bisphosphonatesused
intreatingstressfractures mayweaken someboneregions when usedoverthe longterm and maypredisposetoward appearanceoffracturesduetoinsufficiencyandapotential teratogeniceffectamongpregnantpatients.6
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.BreithauptMD.Zurpathologiedesmenschlichenfusses.To thepathologyofthehumanfoot.MedZeitung.1855;24:169. 2.DevasMB.Stressfracturesofthetibiainathletesof‘shin
soreness.JBoneJointSurgBr.1958;40(2):227–39. 3.SchneidersAG,SullivanSJ,HendrickPA,HonesBDGM,
McmasterAR,SugdenBA,etal.Theabilityofclinicalteststo diagnosestressfractures:asystematicreviewand
meta-analysis.JOrthopSportsPhysTher.2012;42(9):760–71. 4.FayadLM,KamelIR,KawamotoS,BluemkeDA,FrassicaFJ,
FishmanEK.Distinguishingstressfracturesfrompathologic fractures:amultimodalityapproach.SkeletRadiol. 2005;34(5):245–59.
5.NivaMH,MattilaVM,KiuruMJ,PihlajamäkiHK.Bonestress injuriesarecommoninfemalemilitarytrainees:a
preliminarystudy.ClinOrthopRelatRes.2009;467(11):2962–9. 6.CarmontRC,Mei-DanO,BennellLK.Stressfracture
management:currentclassificationandnewhealing modalities.OperTechSportsMed.2009;17:81–9. 7.PatelDS,RothM,KapilN.Stressfractures:diagnosis,
treatment,andprevention.AmFamPhysician. 2011;83(1):39–46.
8.EvansRK,AntczakAJ,LesterM,YanovichR,IsraeliE,Moran DS.Effectsofa4-monthrecruittrainingprogramonmarkers ofbonemetabolism.MedSciSportsExerc.2008;4011 Suppl.:S660–70.
10.BennellKL,MalcolmSA,ThomasSA,WarkJD,BruknerPD. Theincidenceanddistributionofstressfracturesin competitivetrackandfieldathletes.Atwelve-month prospectivestudy.AmJSportsMed.1996;24(2):211–7. 11.RoyerM,ThomasT,CesiniJ,LegrandE.Stressfracturesin
2011:practicalapproach.JointBoneSpine.2012;79Suppl. 2:S86–90.
12.SnyderRA,KoesterMC,DunnWR.Epidemiologyofstress fractures.ClinSportsMed.2006;25(1):37–52.
13.IwamotoJ,TakedaT.Stressfracturesinathletes:reviewof196 cases.JOrthopSci.2003;8(3):273–8.
14.DaffnerRH,PavlovH.Stressfractures:currentconcepts.AmJ Roentgenol.1992;159(2):245–52.
15.JohnsonAW,WeissCBJr,WheelerDL.Stressfracturesofthe femoralshaftinathletes–morecommonthanexpected:a newclinicaltest.AmJSportsMed.1994;22(2):248–56. 16.JonesBH,BoveeMW,HarrisJM,CowanDN.Intrinsicrisk
factorsforexercise-relatedinjuriesamongmaleandfemale armytrainees.AmJSportsMed.1993;21(5):705–10.
17.PesterS,SmithPC.Stressfracturesinthelowerextremitiesof soldiersinbasictraining.OrthopRev.1992;21(03):
297–303.
18.BolinD,KemperA,BrolinsonG.Currentconceptsinthe evaluationandmanagementofstressfractures.CurrRep SportMed.2005;4(6):295–300.
19.MoriS,BurrDB.Increasingintracorticalremodelling followingfatiguedamage.Bone.1993;14(2):103–9. 20.RaaschWG,HerganDJ.Treatmentofstressfractures:the
fundamentals.ClinSportsMed.2006;25(1):29–36. 21.KorpelainenR,OravaS,KarpakkaJ,SiiraP,HulkkoA.Risk
factorsforrecurrentstressfractureinathletes.AmJSports Med.2001;29(3):304–10.
22.JoyEA,CampbellD.Stressfracturesinthefemaleathlete. CurrSportsMedRep.2005;4(6):323–8.
23.GardnerLIJr,DziadosJE,JonesBH,BrundageJF,HarrisJM, SullivanR,etal.Preventionoflowerextremitystress fractures:acontrolledtrialofashockabsorbentinsole.AmJ PublicHealth.1988;78(12):1563–7.
24.MilgromC,FinestoneA,LeviY,SimkinA,EkenmanI, MendelsonS,etal.Dohighimpactexercisesproducehigher tibialstrainsthanrunning?BrJSportsMed.2000;34(3):195–9. 25.PatelRD.Stressfractures:diagnosisandmanagementinthe
primarycaresettings.PediatrClinNAm.2010;81:9–27. 26.ShafferRA,RauhMJ,BrodineSK,TroneDW,MaceraCA.
Predictorsofstressfracturesusceptibilityinyoungfemale recruits.AmJSportsMed.2006;34(1):108–15.
27.MilgromC,FinestoneA,ShlamkovitchN,RandN,LevB, SimkinA,etal.Youthisariskfactorforstressfracture:a studyof783infantryrecruits.JBoneJointSurgBr. 1994;76(1):20–2.
28.ValimakiVV,AlfthanH,LehmuskallioE,LoyttyniemiE,Sahi T,SuominenH,etal.Riskfactorsforclinicalstressfractures inmalemilitaryrecruits:aprospectivecohortstudy.Bone. 2005;37(2):267–73.
29.MyburgKH,HutchinsJ,FataarAB,HoughSF,NoakesTD.Low bonedensityisanetiologicfactororstressfracturesin athletes.AnnInternMed.1990;113(10):754–9.
30.NievesJW,MelsopK,CurtisM.Nutritionalfactorsthat influencechangeinbonedensityandstressfracturerisk amongyoungfemalecross-countryrunners.PMR. 2010;2(8):740–50.
31.PoppKL,HughesJM,SmockAJ,NovotnySA,StovitzSD, KoehlerSM,etal.Bonegeometry,strength,andmusclesize inrunnerswithahistoryofstressfracture.MedSciSports Exerc.2009;41(12):2145–50.
32.GiladiM,MilgromC,SimkinA,DanonY.Stressfractures: identifiableriskfactors.AmJSportsMed.1991;19(6):647–52.
33.ManioliA2nd,GrahamB.Thesubtlecavusfoot:theunder pronator:areview.FootAnkleInt.2005;26(3):256–63. 34.PohlMB,MullineauxDR,MilnerCE,HamillJ,DavisIS.
Biomechanicalpredictorsofretrospectivetibialstress fracturesinrunners.JBiochem.2008;41(6):1160–5.
35.MaitraRS,JohnsonDL.Stressfractures.Clinicalhistoryand physicalexamination.ClinSportsMed.1997;16(2):
259–74.
36.FredericsonM,WunC.Differentialdiagnosisoflegpaininthe athlete.JAmPodiatrMedAssoc.2003;93(4):321–4.
37.RomaniWA,PerrinDH,DussaultRG,BallDW,KahlerDM. Identificationoftibialstressfracturesusingtherapeutic continuousultrasound.JOrthopSportsPhysTher. 2000;30(8):444–52.
38.IshibashiY,OkamuraY,OtsukaH,NishizawaK,SasakiT,Toh S.Comparisonofscintigraphyandmagneticresonance imagingforstressinjuriesofbone.ClinJSportMed. 2002;12(2):79–84.
39.SterlingJC,EdelsteinDW,CalvoRD,WebbR.Stressfractures intheathlete.Diagnosisandmanagement.SportsMed. 1992;14(5):336–46.
40.BennellK,BruknerP.Preventingandmanagingstress fracturesinathletes.PhysTherSport.2005;6:171–80. 41.FredericsonM,BergmanAG,HoffmanKL,DillinghamMS.
Tibialstressreactioninrunners.Correlationofclinical symptomsandscintigraphywithanewmagneticresonance imaginggradingsystem.AmJSportsMed.1995;23(4): 472–81.
42.StrauchWB,SlomianyWP.Evaluatingshinpaininactive patients.JMusculoskeletMed.2008;25:138–48.
43.ShinAY,MorinWD,GormanJD,JonesSB,LapinskiAS.The superiorityofmagneticresonanceimagingindifferentiating thecauseofhippaininenduranceathletes.AmJSportsMed. 1996;24(2):168–76.
44.DixonS,NewtonJ,TehJ.Stressfracturesintheyoungathlete: apictorialreview.CurrProblDiagnRadiol.2011;40(1): 29–44.
45.ZukotynskiK,CurtisC,GrantFD,MicheliL,TrevesST.The valueofSPECTinthedetectionofstressinjurytothepars interarticularisinpatientswithlowbackpain.JOrthopSurg Res.2010;5:13.
46.SofkaCM.Imagingofstressfractures.ClinSportsMed. 2006;25(1):53–62.
47.BruknerP,BennellK.Stressfracturesinfemaleathletes. Diagnosis,managementandrehabilitation.SportsMed. 1997;24(6):419–29.
48.FredericsonM,JenningsF,BeaulieuC,MathesonGO.Stress fracturesinathletes.TopMagnResonImaging.
2006;17(5):309–25.
49.VoloshinKW.Dynamicloadingduringrunningonvarious surfaces.HumanMovSci.1992;11:675–89.
50.MehalloCJ,DreznerJA,BytomskiJR.Practicalmanagement: nonsteroidalanti-inflammatorydrug(NSAID)useinathletic injuries.ClinJSportMed.2006;16:170–4.
51.WheelerP,BattME.Donon-steroidalanti-inflammatory drugsadverselyaffectstressfracturehealing?Ashortreview. BrJSportsMed.2005;39(2):65–9.
52.BurnsAS,LauderTD.Deepwaterrunning:aneffectivenon weightbearingexerciseforthemaintenanceoflandbased runningperformance.MilMed.2001;166(3):253–8. 53.JohanssonC,EkenmanI,TornkvistH,ErikssonE.Stress
fracturesofthefemoralneckinathletes:theconsequenceof adelayindiagnosis.AmJSportsMed.1990;18(5):524–8. 54.BennetMH,StanfordR,TurnerR.Hyperbaricoxygentherapy
forpromotingfracturehealingandtreatingfracturenon union.CochraneDatabaseSystRev.2005;25(1):
55.ShimaY,EngebretsenL,IwasaJ,KitaokaK,TomitaK.Useof bisphosphonatesforthetreatmentofstressfracturesin athletes.KneeSurgSportsTraumatolArthrosc. 2009;17(5):542–50.
56.EkenmanI.Donotusebisphosphonateswithoutscientific evidence,neitherinthetreatmentnorprophylactic,inthe treatmentofstressfractures.KneeSurgSportsTraumatol Arthrosc.2009;17(5):433–4.
57.HammondJW,HintonRY,CurlLA,MurielJM,LoveringRM. Useofautologousplateletrichplasmatotreatmusclestrain injuries.AmJSportsMed.2009;37(6):1135–42.