www.jped.com.br
ORIGINAL
ARTICLE
Metabolic
risk
in
schoolchildren
is
associated
with
low
levels
of
cardiorespiratory
fitness,
obesity,
and
parents’
nutritional
profile
夽
Pâmela
Ferreira
Todendi
a,
Andréia
Rosane
de
Moura
Valim
a,
Cézane
Priscila
Reuter
a,
Elza
Daniel
de
Mello
b,
Anelise
Reis
Gaya
b,
Miria
Suzana
Burgos
a,∗aUniversidadedeSantaCruzdoSul(UNISC),SantaCruzdoSul,RS,Brazil bUniversidadeFederaldoRioGrandedoSul(UFRGS),PortoAlegre,RS,Brazil
Received29May2015;accepted13October2015 Availableonline17May2016
KEYWORDS
School;
Cardiorespiratory fitness;
Bodymassindex; Parents
Abstract
Objective: Verifytheassociationbetweenmetabolicriskprofileinstudentswithdifferentlevels
ofcardiorespiratory fitnessand body massindex, aswell as thenutritional status of their parents.
Methods: Across-sectionalstudycomprising1.254schoolchildrenagedbetweensevenand17
years.Themetabolicriskprofilewascalculatedbysummingthestandardizedvaluesofhigh densitylipoproteinsandlowdensitylipoproteins,triglycerides,glucoseandsystolicblood pres-sure.Theparents’nutritionalstatuswasevaluatedbyself-reportedweightandheightdata, forbodymassindexcalculating.Thebodymassindexofschoolchildrenwasclassifiedas under-weight/normalweightandoverweight/obesity.Thecardiorespiratoryfitnesswasassessedby 9-minuterunning/walktest,beingcategorizedasfit(goodlevels)andunfit(lowlevels).Data wereanalyzedusingprevalenceratiovalues(PR).
Results: Thedataindicatesahigheroccurrenceofdevelopingmetabolicriskinschoolchildren
whosemotherisobese(PR:1.50;95%CI:1.01,2.23),andevenhigherforthosewhosefather andmotherareobese(PR:2, 79,95%CI:1.41; 5.51).Studentswhohavelowlevelsof car-diorespiratoryfitnessandoverweight/obesityhavehigheroccurrenceofpresentingmetabolic riskprofile(PR:5.25;95%CI:3.31;8.16).
Conclusion: theoccurrenceofdevelopingmetabolicriskinschoolchildrenincreasewhenthey
have low levels of cardiorespiratory fitness and overweight/obesity, and the presence of parentalobesity.
©2016SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Thisisanopen accessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/licenses/by-nc-nd/ 4.0/).
夽 Pleasecitethisarticleas:TodendiPF,ValimAR,ReuterCP,MelloED,GayaAR,BurgosMS.Metabolicriskinschoolchildrenisassociated withlowlevelsofcardiorespiratoryfitness,obesity,andparents’nutritionalprofile.JPediatr(RioJ).2016;92:388---93.
∗Correspondingauthor.
E-mail:mburgos@unisc.br(M.S.Burgos).
http://dx.doi.org/10.1016/j.jped.2015.10.007
0021-7557/©2016SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-ND
PALAVRAS-CHAVE
Escolares; Aptidão
cardiorrespiratória; Índicedemassa corporal; Pais
Riscometabólicoemescolaresestáassociadocombaixosníveisdeaptidão cardiorrespiratória,obesidadeeperfilnutricionaldospais
Resumo
Objetivo: Verificarseháassociac¸ãoentreoperfilderiscometabólicoemescolarescom
difer-entesníveisdeaptidãocardiorrespiratóriaeíndicedemassacorporal,bemcomocomoperfil nutricionaldeseuspais.
Métodos: Estudotransversalconstituídopor1.254escolarescomidadeentresetee17anos.O
perfilderiscometabólicofoicalculadopormeiodasomadosvaloresestandardizadosde lipopro-teína dealta densidade elipoproteínade baixa densidade,triglicerídeos,glicosee pressão arterialsistólica.Operfilnutricionaldospaisfoiavaliadopelosdadosautorreferidosdepeso eestatura,calculando-seposteriormenteoíndicedemassacorporal.Oíndicedemassa cor-poraldoescolarfoiclassificadoembaixopeso/pesonormalesobrepeso/obesidade.Aaptidão cardiorrespiratóriafoi avaliada atravésdo testedecorrida/caminhada de9minutos,sendo categorizadaemapto(bonsníveis)einapto(baixosníveis).Osdadosforamanalisadosatravés dosvaloresderazãodeprevalência(RP).
Resultados: Osdadosapontammaiorocorrênciadedesenvolvimentoderiscometabólicoem
escolaresqueapresentammãecomobesidade(RP:1,50;IC95%:1,01;2,23)e,maiorainda, em escolaresquepossuem pai emãe obesos (RP:2,79; IC 95%: 1,41; 5,51).Escolares que apresentambaixosníveisdeaptidãocardiorrespiratóriaesobrepeso/obesidadepossuemmaior ocorrênciadeperfilmetabólicoderisco(RP:5,25;IC95%:3,31;8,16).
Conclusões: a ocorrência de desenvolvimento de risco metabólicoem escolaresaumentam
quandoestesapresentambaixosníveisdeaptidãocardiorrespiratóriaesobrepeso/obesidade, assimcomonapresenc¸adeobesidadedospais.
©2016SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Este ´eumartigo OpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/licenses/by-nc-nd/4. 0/).
Introduction
The rapid increase in the prevalence of overweight and obesityin Brazilianchildrenandadolescents1hasresulted in a growing interest about the role of lifestyle in the development of the metabolic risk profile (MRP) in chil-drenandadolescents.Basedontherecordsofthisalarming increaseinoverweightandobesity,theirconsequencesfor healthhavebeendemonstrated,suchastheoccurrenceof metabolicsyndrome(MS),whichrepresentsaconditionof adulthoodrelatedtocardiovascularmorbidity.However,MS hasalsobeenidentifiedinchildrenandadolescents, show-ingadirectassociationwithexcessweight.2---4Studieshave shown that metabolic risk develops during childhood and adolescence,leadingtoanincreasedriskofcardiovascular eventsandoccurrenceoftype2diabetes.2,3
Consequently, studies thataim toexplore therisk fac-torsofcardiovasculardiseasesinchildrenandadolescents are being emphasized, focusing on the centralization of prevention --- considering, in additionto the lifestyles of youngindividuals, theinfluenceoffamilyinvolvement.5 It hasthereforebeenverifiedthatadultswithlow cardiorespi-ratoryfitnessareassociatedwithcardiovascularriskfactors suchashypercholesterolemia,obesity,andtype2diabetes.6 However,theevidenceisnotyetclearinchildrenand ado-lescents,butsuggeststhattheassociationbetweenobesity andcardiovascularriskismediatedbyaerobicfitnesssince childhood.7Itcanalsobeobservedthatthecardiometabolic risk ishigher inchildren and adolescentswithoverweight andobesitywhoperformlightphysicalactivitythaninthose whopracticevigorousactivity.8
Severalstudieshaveshownthatlowcardiorespiratory fit-ness(CRF)isasignificantindependentriskfactorforfuture cardiometabolicdiseaseinadulthood.Nolessimportantly,it issuggestedthattheparentalnutritionalprofileisan impor-tant predictor of overweight and obesity in children and adolescents.9 Nevertheless, considering the consequences ofthisdisorder,thereisalreadyevidenceofanassociation betweentheparents’lifestyleandnutritionalprofile with anearlyriskofdevelopingametabolicriskprofile.10,11The possibilityofobeseparentsofhavingchildrenwithhigh car-diometabolicriskisexplainedbythelikelyinfluencenotonly of familyinvolvement, but also of geneticfactors, which accountforapproximately30%---40% of factorsresponsible for early development of diseases in childhood and ado-lescence.However,it isworth mentioningthe importance offocusingresearchonfactorsrelatedtolifestyle,bothof youngindividualsandtheirparents,inordertoobtaindata tobetterorganizeinterventions.
Theabovestatementsjustify theimportanceofstudies thatseektounderstandtheearlydevelopmentofMSin chil-drenandadolescentsandtheneedtoincludealargenumber ofpotentialassociatedfactors.Thus,itissuggestedthatlow cardiorespiratoryfitnessmaybeanindependentriskfactor for futurecardiometabolic disease in adulthood.12 Never-theless,whenpreventionisconsidered,somefactorshave been highlightedas beingboth importantand modifiable, resultsthatjustifytheneedtocomprehendtheassociation between obesity7 and parents’ nutritional profile11 vs. cardiorespiratoryfitnessinayoungBrazilianpopulation.
levelsofcardiorespiratoryfitness(CRF)andbodymassindex (BMI),aswellaswiththenutritionalstatusoftheirparents.
Methods
The population ofschoolchildren andadolescents consists ofapproximately20,540students,frompublicandprivate elementary and high Schools, of whom 11,679 are state-operated,6813aremunicipal,and2048areprivateschool locatedin themunicipality of Santa Cruz doSul,state of RioGrandedoSul,Brazil,stratifiedbyruralandurbanareas andthe latter by downtown and periphery:north, south, east,andwest.Datawerecollectedfromthe6thRegional Coordinatorof Education andtheMunicipal Secretariatof EducationofSantaCruzdoSul.Toberepresentativeofthe municipality,asample of approximately400students was estimated, based on a statistical power of 0.80, a level of significance of 5%, and the prevalence of overweight andobesityofapproximately30%forBrazilianchildrenand adolescents.1
This research is part of a longitudinal study called Schoolchildren’sHealth,consistingof arandomsampleby conglomerates of approximately 2000 schoolchildren and adolescents,aged 7---17 years, attending 19 schools (cen-ter,north,south,east, andwestof theruralarea)ofthe municipality ofSanta Cruz doSul-RS. Ofthese, 1254 par-ticipatedinthisstudy,consideringasinclusioncriterionthe students’complete dataregarding theselectedvariables, aswellastheirparents’.Thus,studentswhoseparentsdid notreporttheirweightandheight,thosewhodidnotallow thecollectionofblood,andthosewhohadaphysical prob-lemthatpreventedthemfromperformingthetesttoassess CRFwereremovedfromthesample.
After providingdetailed informationabout the project and explanations about the procedures to which the schoolchildren and adolescents would be submitted, all participantsprovidedtheinformedconsentsignedby par-ents/guardians,agreeingtoparticipateinthestudy,which was approved by the Ethics Committee of Universidade SantaCruzdoSul---UNISCunderNo.2525/10.
The nutritional profile of parents was self-reported throughasurveythatincludedtheirheightandweightfor subsequent BMI calculation, which was classified accord-ing tothe World Health Organization criteria13 asnormal BMI(18.50---24.99kg/m2),overweight(25.00---29.99kg/m2),
orobesity(≥30.00kg/m2).
Bloodwascollectedthroughvenipuncture bya trained technician after eight hours of fasting. Blood samples were centrifuged and the serum was stored in pre-labeled Eppendorf tubes at −20◦C until the time of the analysis. The biochemical analyses (glucose, high-density lipoprotein[HDL],andtriglycerides [TG])wereperformed using DiaSys commercial kits (DiaSys Diagnostic Systems, Germany),inaMiuraOnedevice(I.S.E.,Rome,Italy). Low-density lipoprotein (LDL) wascalculated according tothe Friedewald---Fredrickson---Levyformula.14
Forbloodpressureassessment,theparametersoftheVI BrazilianGuidelinesonHypertension15wereused,basedon theauscultatory method, withaneroiddevices calibrated forlessthanthreemonthsatthetimeoftheevaluations. The researchershadthreedifferent cuffsizes in orderto
selectthemostsuitablecuffforthecircumferenceofeach arm,whileconsideringawidth/lengthproportionof1:2.
CRFwasassessedbythedistancetraveledbythestudent (inmeters)usingthenine-minutewalk/runtestcarriedout on a race track, according to the protocol recommended by theSportBrazilProject.16 Subsequently, subjectswere categorizedinto goodlevels(fit) andlow levels(unfit) of cardiorespiratory fitness,according tothe cutoff point of PROESP-BR(ProjectSportBrazil),16consideringgenderand age.
BMIwasdefinedbyapplyingtheformula:BMI=weight/ height2 (kg/m2).Weightand heightwereevaluatedin the
early morning in fasting state, with the subject wear-inglightclothing andnoshoes.BMIclassificationfollowed theprotocolfor Brazilianchildrenandadolescents, estab-lishedbyCondeandMonteiro,17consideringthecategories underweight/normalweightandoverweight/obeseforthis study.
TheCRF/BMIassociationwasestablishedconsideringthe following categories: 1) fit/low weight-normal weight; 2) fit/overweight-obesity;3)unfit/lowweight-normalweight; 4)unfit/overweight-obesity.
The metabolic risk was calculated by the sum of the standardizedvalues(Z-score)ofeachoftheriskfactorsfor cardiovasculardisease:HDLandLDL,TG,glucose,and sys-tolicbloodpressure(SBP),notincludingtheBMI.TheZ-score ofHDLwasmultipliedby−1,asitindicatesaninverse
asso-ciationwithcardiovascularriskfactors.MRPwasconsidered when values were equal to or greater than one standard deviation,accordingtothecriteriaestablishedbyAndersen etal.18andusedbyMotaetal.19
DatawereanalyzedinthestatisticalprogramSPSS(IBM SPSS Statistics for Windows, Version 23.0. IBM Corp., NY, USA). Descriptive analyses are shown as mean/standard deviation and frequency for categorical variables. The prevalence ratio between the MRP and the independent variableswascalculatedusingbivariatelogisticregression models,consideringthehighMRPvaluesastheriskcategory tocalculatetheprevalenceratioThemodelincludedthe fol-lowingpredictingfactors:BMI/CRFandBMIoftheparents. The riskcategorieswereusedasreferencecategories.All modelswereadjustedforage.Knowingthatseveralfactors areassociatedwiththedevelopmentoftheMRP,such asso-ciationswereanalyzedbymultivariateanalysis,whereupon multiple variables are analyzed in a single association.20 Thus,differentregressionmodelswereassessed, consider-ingthepossibilityoferrorassociatedwithmulticolinearity between three variables: father’sBMI, mother’s BMI, and parents’BMI.A5%significancelevelwasconsideredforall analyses.
Results
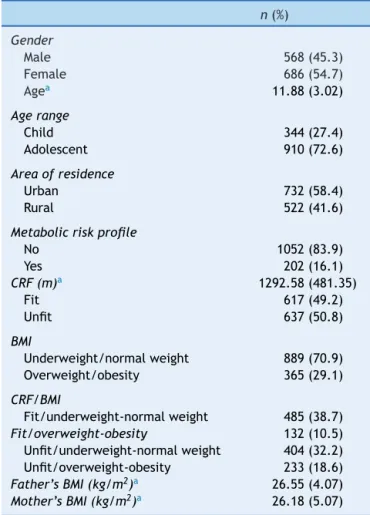
Table1 Descriptivecharacteristicsofthesubjects.
n(%)
Gender
Male 568(45.3)
Female 686(54.7)
Agea 11.88(3.02)
Agerange
Child 344(27.4)
Adolescent 910(72.6)
Areaofresidence
Urban 732(58.4)
Rural 522(41.6)
Metabolicriskprofile
No 1052(83.9)
Yes 202(16.1)
CRF(m)a 1292.58(481.35)
Fit 617(49.2)
Unfit 637(50.8)
BMI
Underweight/normalweight 889(70.9)
Overweight/obesity 365(29.1)
CRF/BMI
Fit/underweight-normalweight 485(38.7) Fit/overweight-obesity 132(10.5) Unfit/underweight-normalweight 404(32.2) Unfit/overweight-obesity 233(18.6) Father’sBMI(kg/m2)a 26.55(4.07)
Mother’sBMI(kg/m2)a 26.18(5.07)
CRF,cardiorespiratoryfitness;BMI,bodymassindex. a Dataexpressedasmean(standarddeviation).
Table2showsthreemodelsofbinarylogisticregression, takingintoaccountthattheindependentvariables,which representtheparents’characteristics,showahigh associ-ation witheach other (multicolinearity).All models were adjustedfor theareaofresidence,ageandgenderof the subject, and alsocontain thegrouped variables CRF/BMI. Theresultsshowhigherincidenceinstudentswhose moth-ershadobesity(PR:1.50;95%CI:1.01,2.23)---model1,and evenhigherinstudentswhohadanobesefatherandmother (PR:2.79;95%CI:1.41,5.51)---model3.Therewasno associ-ationbetweenthefathers’obesityandtheirchildren’sMRP --- model2.
AnassociationwasobservedinallmodelsfortheCRF/BMI variable, considering as reference category the fit/low weight-normal weight students. High metabolic risk was found both in unfit/overweight-obesity (PR: 5.29; 95% CI: 3.31,8.16) andfit/overweight-obesity students(PR: 3.42; 95%CI:1.24,2.38).Thisstudydidnotverifyanincreasedrisk inunfit/lowweight-normalweightincomparisontofit/low weight-normalweightstudents.
Regardingthe students’characteristics,girls(PR: 1.74; 95% CI: 1.24, 2.38) and residents of the rural area (PR: 1.77; 95% CI: 1.25, 2.37) had a higher incidence of MRP development. On the other hand, birth weight, time of breastfeeding,andagewerenotassociatedwithMRP.
Discussion
Thisstudyaimedtodeterminewhetherthereisan associ-ationbetween levels of CRF/BMI and parents’ nutritional profile with students’ MRP. It wasobserved that children andadolescentswithanobesefatherandmotherhadhigher incidenceofMRPincomparisontothosewhohadonlythe fatheror motherwithobesity.Itis noteworthythatthese resultswere independent fromthe CRF/BMI levelsof the youngindividuals.However,satisfactoryaerobicfitness lev-elswereshowntobeanimportantmediatoroftheriskof obeseyoungindividualstodevelopMRP.
Themultifactorialcausesofearlycardiovascularrisk fac-tordevelopmentin childhoodhave been demonstratedin recent years.21 In additionto the geneticcontribution to thedevelopmentofcardiovascularrisk factors,22 parental behavior has been strongly associated with the behavior adopted by their children.11 Studies indicate a significant associationof parentalnutritional profilewithoverweight andobesityintheirchildren.9,23Infact,theimportanceof parents’obesityasapredictorforobesityintheirchildren seemsclear.
A study by Efstathiou et al.10 carried out in Greece, includinga sample of children and adolescents and their parents,obtainedasthemain resultthepossibilityoflow weight,reducedheadsize,andfamilyhistoryofoverweight andobesityaspossiblefactorsassociatedwiththedetection ofchildrenwithchanceofdevelopingMRPinadolescence. It should be noted that this study used a metabolic risk scoresimilartothatusedinthisstudy;however,contraryto thepresentresults,lowbirthweightwasthemain predic-tor.Anotherstudyfoundthatobesityinchildhoodincreases thecardiometabolicrisk profile,but satisfactory levelsof cardiorespiratoryfitnesstendtoattenuate theassociation betweenobesityandcardiometabolicrisk.24
As a result of these statements, studies that indicate thechances of children and adolescentswhohave a par-entorbothparentswithoverweightandobesitydeveloping not only early overweight and obesity,but additionally a metabolicriskprofile,arehighlighted.10,11,25Inthepresent study,therewasahigheroccurrenceofstudents whohad an obese father and mother in the development of early metabolicriskprofile.Additionally,itwasfoundthatwhen analyzedindividually,onlythemothers’behaviorwas asso-ciatedwiththechildren’s,whilethefathers’behaviordoes notshowsuchassociation.InthestudybyJiangetal.,9the mothers’nutritionalprofileshowedastrongassociationwith theirchildren’sobesity.Asjustificationfortheseresults,the authorssuggestthepossibilitythatmothersareusuallymore involvedintheirchildren’sdailyactivitiesandfeedinghabits and,thus, can have a higherinfluence than the parents’ lifestyle.
Table2 AssociationbetweenCRF,BMI,mother’sBMI,father’sBMIandparents’BMIwithstudents’metabolicriskprofile.
Model1 Mother’sBMI
Model2 Father’sBMI
Model3 Parents’BMI
PR(95%CI) PR(95%CI) PR(95%CI)
Mother’sBMI
Normal 1
Overweight 1.09(0.75;1.50)
Obesity 1.50(1.01;2.23)
Father’sBMI
Normal 1
Overweight 0.96(0.69;1.41)
Obesity 0.90(0.57;1.42)
Parents’BMI
Normal 1
Overweight 1.07(0.65;1.74)
Obesity 2.79(1.41;5.51)
CRF/BMI
Fit/normalBMI 1 1 1
Fit/overweight-obesity 3.29(1.24;2.38) 3.45(2.01;5.92) 3.42(1.98;5.89)
Unfit/normalBMI 1.37(0.88;2.14) 1.37(0.88;2.14) 1.38(0.88;2.16) Unfit/overweight-obesity 5.25(3.31;8.16) 5.62(3.38;8.81) 5.29(3.36;8.32)
Areaofresidence
Urban 1 1 1
Rural 1.72(1.25;2.37) 1.74(1.26;2.40) 1.77(1.29;2.45)
Gender
Male 1 1 1
Female 1.72(1.24;2.38) 1.71(1.24;2.37) 1.74(1.25;2.42)
CRF,cardiorespiratoryfitness;BMI,bodymassindex;fit,goodlevelsofcardiorespiratoryfitness;unfit,lowlevelsofcardiorespiratory fitness.
Models1,2and3wereadjustedforage.
NagelkerkeRSquare:model1(7.4%),model2(7.1%)andmodel3(13.4%).
MRPofapproximately15%,confirmingtheneedtoinclude othervariablesthatmayexplainthisearlymetabolicrisk, togetherwithcertaingeneticcharacteristics.Nevertheless, itappearsimportanttosuggestthatobesity vs.lowlevels ofaerobicfitnessaddedtotheparents’obesity wereable toexplainalmost one-thirdofwhatis expectedtobethe non-genetic contribution to metabolic syndrome in young individuals.
Additionally,thepresentstudyobservedastrong associa-tionbetweenCRF/IMCwiththeMRPofthestudents,andthe occurrenceofMRPinunfitstudentswithoverweight/obesity washighercomparedthosewhowerefitandhadnormalBMI. However,contrarytowhatwasexpected,andinaccordance withwhatwassuggestedbyEisenmannetal.,7childrenand adolescentswithnormalBMI,butwithlowCRF,didnotshow ahigherincidenceofMRPinrelationtothosewithgood lev-elsofCRFandnormalBMI.Thatis,itappearsthatnormal weightinchildrenandadolescentsisconsideredaprevalent factorofcardiometabolicriskwhencomparedwiththerole ofaerobicfitness.
However,theoccurrenceofMRPamongchildrenand ado-lescents with overweight and obesity was attenuated by healthylevels of CRF. That is, while children and adoles-centswithoverweightandobesity whowereunfitshowed a5-foldhigheroccurrenceofMRPdevelopmentinrelation
tofitchildrenwithunderweight/normalweight,thosewith overweightandobesitythatwerefithadaloweroccurrence, approximatelythree-foldlower. Therefore,itis suggested that, in accordance withthe study by Eisenmann etal.,7 particularlyinchildrenandadolescentswithoverweightand obesity,maintainingahealthylevelofCRFseemstoprotect againsttheearlydevelopmentofriskfactorsfor cardiovas-culardisease.
Finally, the occurrence of metabolic risk development is higherin girls among studentsfrom ruralareas and,in fact,boththeparents’BMIandCRF/BMIratioareimportant predictors associated with risk factors for cardiovascular diseaseinstudents.Itisworthmentioningthetwo impor-tantfindingsofthisstudy:childrenwithobesefathersand mothers areat greater risk than their peerswithonly an obesemother or father and,furthermore, a high levelof cardiorespiratoryfitnessseemstobeaprotectivefactorin apopulationalreadyatrisk,asinthecaseofchildrenand adolescentswithoverweightandobesity.
However,itshouldbenotedthatthepresent studyhas somelimitations.Directassessmentoftheparents’weight andheight couldnotbeperformed due tothelarge sam-ple of students evaluated in the study; so we chose the self-reported information of these variables by the par-ents, allowing the calculation of BMI. Also, the students’ sexual maturation stage was not assessed, with sexual dimorphismbeingcapableofinfluencingtheanalyzed asso-ciations. Despite some limitations, this study reinforces theimportanceoftheassociationsfoundandsuggeststhat experimentalstudiesbeperformedtoestablisha cause-and-effectassociation.
Weconcludethattheparents’nutritionalprofile,aswell as obesity and low levels of cardiorespiratory fitness are riskfactorsforearlydevelopmentofmetabolicriskin chil-dren and adolescentsand should be considered in future interventionstudies.
Funding
UniversidadedeSantaCruzdoSul(UNISC).
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.FloresLS,GayaAR,PetersenRD,GayaA.Trendsofunderweight, overweight,andobesityinBrazilianchildrenandadolescents. JPediatr(RioJ).2013;89:456---61.
2.DamianiD,KubaVM,CominatoL,DamianiD,DichtchekenianV, MenezesFilhoHC.Metabolicsyndromeinchildrenand adoles-cents:doubtsaboutterminologybutnotaboutcardiometabolic risks.ArqBrasEndocrinolMetabol.2011;55:576---82.
3.RajM.Obesityandcardiovascularriskinchildrenand adoles-cents.IndianJEndocrinolMetab.2012;16:13---9.
4.FriendA,CraigL,TurnerS.Theprevalenceofmetabolic syn-dromeinchildren:asystematicreviewoftheliterature.Metab SyndrRelatDisord.2013;11:71---80.
5.ShaibiGQ,RyderJR,KimJY,BarrazaE.Exerciseforobeseyouth: refocusingattention from weightloss tohealth gains. Exerc SportSciRev.2015;43:41---7.
6.ErezA,KivityS,BerkovitchA,MilwidskyA,KlempfnerR,Segev S,etal.Theassociationbetweencardiorespiratoryfitnessand cardiovascularriskmaybemodulatedbyknowncardiovascular riskfactors.AmHeartJ.2015;169:916---23.
7.EisenmannJC,WelkGJ,WickelEE,BlairSN.Combinedinfluence ofcardiorespiratoryfitnessandbodymassindexon cardiovascu-lardiseaseriskfactorsamong8---18yearoldyouth:theaerobics centerlongitudinalstudy.IntJPediatrObes.2007;2:66---72.
8.Cárdenas-CárdenasLM,Burguete-GarciaAI,Estrada-VelascoBI, López-IslasC,Peralta-RomerocJ,CruzM,etal.Leisure-time physicalactivityandcardiometabolicriskamongchildrenand adolescents.JPediatr(RioJ).2015;91:136---42.
9.JiangMH,YangY,GuoXF,SunYX.Associationbetweenchild and adolescent obesity and parental weight status: a cross-sectionalstudyfromruralNorthChina.JIntMedRes.2013;41: 1326---32.
10.Efstathiou SP,Skeva II,Zorbala E,GeorgiouE,Mountokalakis TD. Metabolic syndrome in adolescence: can it be pre-dicted from natal and parental profile? The Prediction of MetabolicSyndromeinAdolescence(PREMA)study.Circulation. 2012;125:902---10.
11.KhanolkarAR,BybergL,KoupilI.Parentalinfluenceson cardio-vascularriskfactorsinSwedishchildrenaged5---14years.EurJ PublicHealth.2012;22:840---7.
12.Gualteros JA, Torres JA, Umbarila-Espinosa LM, Rodríguez-Valero FJ,Ramírez-VélezR. Alowercardiorespiratoryfitness isassociatedtoanunhealthystatusamongchildrenand adoles-centsfromBogotá,Colombia.EndocrinolNutr.2015;62:437---46. 13.WorldHealthOrganization.Obesity.Preventingandmanaging theglobalepidemic.ReportofaWHOconsultationonobesity. Geneva:WHO;1998.
14.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentrationoflow-densitylipoproteincholesterolinplasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499---502.
15.Sociedade Brasileira de Cardiologia; Sociedade Brasileira de Hipertensão;SociedadeBrasileiradeNefrologia.VIdiretrizes brasileirasdehipertensão.ArqBrasCardiol.2010;95:1---51. 16.PROESP-BR. Projeto esporte Brasil: manual; 2009 [accessed
12.03.15].Availablefrom:http://www.proesp.ufrgs.br. 17.CondeWL,MonteiroCA.Bodymassindexcutoffpointsfor
evalu-ationofnutritionalstatusinBrazilianchildrenandadolescents. JPediatr(RioJ).2006;82:266---72.
18.AndersenLB,WedderkoppN,HansenHS,CooperAR,FrobergK. BiologicalcardiovascularriskfactorsclusterinDanishchildren and adolescents:theEuropeanYouthHeartStudy. PrevMed. 2003;37:363---7.
19.Mota J, SantosR, Moreira C,Martins C,GayaA, SantosMP, et al.Cardiorespiratoryfitness and TVviewinginrelationto metabolicriskfactorsinPortugueseadolescents.AnnHumBiol. 2013;40:157---62.
20.HairFJ,BlackWC,BabinJB,AndersonER,TathamRL.Análise multivariadadedados.6thed.SãoPaulo:Bookman;2009.
21.GiussaniM,AntoliniL,BrambillaP,PaganiM,ZuccottiG, Valsec-chiMG,etal.Cardiovascularriskassessmentinchildren:role ofphysicalactivity,familyhistoryandparentalsmokingonBMI andbloodpressure.JHypertens.2013;31:983---92.
22.Rankinen T, Sarzynski MA, Ghosh S, Bouchard C. Are there geneticpathscommontoobesity,cardiovasculardisease out-comes, and cardiovascular risk factors? Circ Res. 2015;116: 909---22.
23.SvenssonV,JacobssonJA,FredrikssonR,DanielssonP,SobkoT, SchiöthHB,etal.Associationsbetweenseverityofobesityin childhoodandadolescence,obesityonsetandparentalBMI:a longitudinalcohortstudy.IntJObes(Lond).2011;35:46---52.
24.Brouwer IS, Stolk PR, Liem TE,Lemmink APK, CorpeleijnE. The role of fitness in the association between fatness and cardiometabolic riskfrom childhood to adolescence. Pediatr Diabetes.2013;14:57---65.
25.JuonalaM,MagnussenCG,BerensonGS,VennA,BurnsTL,Sabin MA,etal.Childhoodadiposity,adultadiposity,and cardiovas-cularriskfactors.NEnglJMed.2011;365:1876---85.