Work developed in the Program of Post-Graduate Studies in Speech-Language, Pathology and Audiology, Pontifícia Universidade Católica de São Paulo – PUC-SP – São Paulo (PUC-SP), Brasil, with scholarship granted by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
(1) Department of Otorhinolaryngology,Irmandade da Santa Casa de Misericórdia de São Paulo – São Paulo (SP), Brazil.
(2)Program of Post-Graduate Studies in Human Communication Disorders, Pontifícia Universidade Católica de São Paulo – PUC-SP – São Paulo (SP), Brazil. Conflict of interest: No
Author’s contributions: JHSM principal investigator, development of research, development schedule, survey of literature, collection and analysis of data, article writing, article submission and procedures; BCACN guiding, developing the research, development schedule, data analysis, correcting the wording of article, approval of the final version.
Correspondence adress: Juliana Habiro de Souza Miguel. R. Camarajé 88/143, Mandaqui, São Paulo (SP), Brazil, CEP: 02416-060. E-mail: juhabiro@yahoo.com.br
Received: 7/31/2012; Accepted: 7/29/2013
Hearing rehabilitation in children: adhesion to treatment
and use of hearing aids
Reabilitação auditiva na criança: adesão ao tratamento e ao uso
do aparelho de amplificação sonora individual
Juliana Habiro de Souza Miguel1, Beatriz Cavalcanti de Albuquerque Caiuby Novaes2
ABSTRACT
Purpose: Early diagnosis of hearing loss in children, as well as fast intervention, have been shown to be determining factors for hearing and language development, with important implications for the social inclu-sion process and communicative performance. The present study aims to analyze alternatives that guarantee adhesion to use of Hearing Aids and greater family participation in the initial steps of the intervention. Methods: The study comprehended parents/caregivers of 16 hearing impaired children who attended the process of ADAPTI (Hearing Aid Fitting and Initial Therapy) during one year, who had formally applied for the Hearing Care Service. The parents were divided in three groups: Previously Determined (Families that attend both the speech therapy and the Family Adhesion Group (GrAF) from the first day set for the begin-ning of sessions, to the last day); Continuous Flow (Families that started attending the group from the moment they arrived for the ADAPTI); and Control (Families that only attended speech therapy, but not the GrAF). Results: The study verified the effectiveness of parent adhesion to their children’s treatment with more than 66% of attendance in the proposed activities (therapeutic intervention and/or GrAF). The statistical analysis allowed the composition of three children groups regarding the datalog usage (hours a day), family participation and degree of hearing loss. Conclusion: The systematic use of hearing aids was the only variable closely related to hearing and language skills. Degree of hearing loss and age at the beginning of amplification have not explained the development of the children in the study.
Keywords: Family; Rehabilitation; Hearing loss; Hearing aids; Lan-guage development
RESUMO
Objetivo: Discutir a adesão das famílias na fase inicial de intervenção quanto ao uso do Aparelho de Amplificação Sonora (AASI), a participa-ção no processo, e sua relaparticipa-ção com desempenho auditivo e de linguagem das crianças com deficiência auditiva. Métodos: Estudo realizado com pais e/ou responsáveis de 16 crianças deficientes auditivas em processo de ADAPTI (Adaptação de AASI e Terapia Inicial) no ano de 2009 e que estavam regularmente inscritas no Serviço de Saúde Auditiva Centro Audição na Criança – CeAC. Os pais foram divididos em três grupos: Pré-determinado - PD (famílias participantes da terapia fonoaudiológica e do Grupo de Adesão Familiar – GrAF, do primeiro ao último dia de atendimento estabelecido); Fluxo contínuo - FC (famílias que iniciavam a participação no GrAF a partir do momento em que chegavam ao servi-ço de saúde para a adaptação de AASI, sem início estabelecido) e Con-trole - C (famílias que participaram somente da terapia fonoaudiológica, mas não do GrAF). Resultados: Foi constatada a efetividade da adesão dos pais ao tratamento dos filhos, sendo registrado o comparecimento em mais de 66% dos atendimentos propostos (terapia fonoaudiológica e/ou GrAF). Na análise estatística dos agrupamentos de crianças, foi possível a formação de três diferentes grupos no que se refere ao uso do datalog (horas/dia), envolvimento familiar e grau de perda auditiva. Conclusão: O uso sistemático de AASI foi a única variável com forte relação com habilidades auditivas e de linguagem. O grau de perda auditiva e a idade de início de amplificação não explicaram o desenvolvimento das crianças do estudo.
INTRODUCTION
Early diagnosis of hearing impairment in children and early intervention are crucial for auditory and language development, with important implications for the social inclusion and the communicative performance.
Many authors report that for a better prognosis, diagnosis and intervention should occur before six months of life, thus ensuring the best use of the hearing potential of the child. Moreover, the effective use of hearing aid or cochlear im-plant, the family expectations, the degree of involvement with treatment and aspects related to socioeconomic and cultural conditions all affect this outcome(1-7).
The speech and language therapy aimed at the acquisition of oral language has been one of the main clinical proposals for children with hearing impairment. It implies considering the peculiarities in the constitution of social, emotional, psycholo-gical and cognitive development besides reordering interaction situations, thus favoring the mode of communication of these patients(4,8-10).
However, for this ideal to be achieved, it is necessary that parents of children with hearing loss understand what they aim at the Hearing Health Service in order to make their choices with clarity and insight, comprehend the potential of their children and set their expectations during this process.
The contact of the family with the speech and language pathologist and audiologist in the process of adaptation of individual hearing aids (HA) also serves as clarification of treatment goals and clinical and educational options available in the community. Within the hearing health, it is essential to also clarify the function of the use of amplification for auditory and oral language development.
The intervention involves several professionals with the ability to carefully absorb and meet the demand of patients who need special attention. Thus, it is important that the health professional is able to perceive the changes that may occur within the family, the anguish on the problem and possible denials so one can contribute to the process of reorganization of the family on the diagnosis, monitoring the development of the child(11).
The Child Hearing Center (Centro Audição na Criança
- CeAC) of the Division of Education and Rehabilitation of Communication Disorders (Divisão de Educação e Reabilitação dos Distúrbios da Comunicação - DERDIC ) and
part of the structure of the Pontifícia Universidade Católica de São Paulo (PUC-SP), is a service of high complexity accredi-ted by the Brazilian Public Health System (Sistema Único de Saúde – SUS), which provides care to children with suspected or diagnosed hearing loss under 3 years of age. The following services are offered: diagnosis, selection and fitting of hearing aids, speech and language therapy, monitoring and guidance to families. The CeAC also offers therapy for part of the demand that is created by its own diagnostic service. The other part is
referred to municipal services or other service locations near the residences of families. This implies the need to perform procedures for systematic evaluation of hearing, language and family involvement in order to ensure the quality of care for all children, inside and outside of the center, which is responsible for tracking the cases.
When the diagnosis is completed and the hearing impair-ment is confirmed, the hearing aid fitting process is carried out in parallel to the selection of hearing aids, involving the initial stages of the therapeutic process, with the purposes of adap-tation, and speech and language therapy with an emphasis on family participation besides the reception and initial guidance to parents. This step process is named ADAPTI.
As part of the initial therapeutic process, the Group of Family Involvement (GrAF) occurs weekly. The goal of the GrAF is to provide different modes of action with all the parents of children. The GrAF includes beginner parents to discuss the auditory potential of the child, the possible intervention me-thods and the referral to appropriate programs of intervention. This period lasts four months on average, depending on the availability of family and counter-reference process to centers closer to home.
Given the importance of the family in all stages of interven-tion for the child to achieve the best prognosis, GrAF aims to contribute to approximate parents to the hearing rehabilitation of their children in order to develop a set of actions that invol-ve different modalities in the initial phase of treatment. Such actions are part of the therapeutic process. This step of the process is accomplished by focusing on parents or guardians.
Historically, it has been observed that some families qui-ckly engage in the process, achieve consistent use of hearing aids and position themselves in relation to treatment. Other families seem content to be receiving the service, but do not know what to expect from the device use and often, though regularly attending therapies, children do not use the device at home.
Given this situation, the present study aimed to examine alternatives that can ensure adherence to the use of hearing aids and greater family involvement in the initial stages of the intervention.
In fact, the proposed actions are necessary under the inter-vention in Hearing Health Services that ensure adherence to treatment, both in regard to family involvement - willingness to participate - as the systematic and consistent use of hearing aids. Moreover, relations between auditory and language per-formance and monitoring of family involvement can contribute to a better understanding of the therapeutic process and, con-sequently, better results in Hearing Health.
METHODS
This consisted on a qualitative descriptive study with parents (or guardians) and speech language pathologists and audiologists of 16 children with hearing impairment who had initiated treatment at ADAPTI (hearing aid fitting and initial therapy) and who were regularly enrolled at CeAC. All participants signed a consent form, obeying ethical prin-ciples. This study was approved by the Ethics Committee of Pontifícia Universidade Católica de São Paulo (PUC) under protocol number 292/2008 .
Study participants were divided into three types of moda-lities according to the participation on the Family Adhesion Group (GrAF) and type of fit:
- Pre-determined (PD): composed of six families of children enrolled in ADAPTI. These families attended both speech and language therapy and GrAF in the first semester of 2009 – from the first to the last established day of attendance – with twelve meetings scheduled. In this group there were no entries of family members after the beginning of service or outputs before the time established and agreed upon all participants.
- Continuous flow (CF): composed of six families who par-ticipated in the GrAF in the second half of 2009, from the moment they arrived at CeAC and started the ADAPTI. The immediate participation in GrAF was allowed underway. Fifteen meetings were scheduled.
- Control (C): composed of four families of ADAPTI who participated in speech and language therapy, but not GrAF. All 16 planned sessions were carried out and included care and guidance to parents.
The inclusion of subjects was conducted according to the following criteria: members of families with children with hearing loss who regularly followed their speech and language therapy performed at CeAC; the child should be using hearing aids for a maximum of six months, with the appointments scheduled at ADAPTI; availability of parent or guardian to attend the activities proposed by the established schedules and agreement on participation in the study.
With the aim of evaluating family involvement in the the-rapeutic process of the hearing impaired child, the following instruments were used:
- Interview Guide(12): questions that lead parents to identify the attitudes of the child’s communication, the participation of these parents in the intervention program, the guidance received to deal with the child and expectations regarding the development of the hearing impaired child;
- Family Involvement Rating(1): rating scale consisting of five items : 1 - limited participation; 2 - participation below average; 3 – median participation; 4 - good participation; 5 - ideal participation. The families were classified by the-rapists who had extensive contact with the parents and the child;
- MUSS(13): scale in the form of a questionnaire that aims to assist in evaluating oral language/speech production skills of children in situations of daily life;
- IT MAIS(14): it aims to evaluate auditory behaviors of children in situations of daily life, reflecting on changes in vocalization, integrated to the use of the electronic device, attention to the various environmental sounds and assigning meaning to sounds;
- Activities of cultural awareness(12): activities used as the triggering at GrAF, aiming to let the parents more comfor-table to talk about their own individual issues and bring issues relating to their children. The activities themselves were not evaluated and described after GrAF because their only goal was to trigger conversations and discussions on issues related to hearing and language skills of the children attended;
- Evaluation of the effective use of hearing aids: note of average daily hours of use.
From the data obtained in the different procedures and instruments used in this study, the analysis was conducted considering the following:
1. Characterization of family according to the PD, FC and C groups in terms of gender, age and education level; evaluation of attendance of families in the sessions (therapy and GrAF); description of the audiological characteristics of children studied with respect to the following aspects: age of onset of hearing aid selection (months); degree of hearing loss; electronic device and therapeutic purposes after the end of the group. The frequency of daily use of hearing aids was determined at the time of periodic monitoring through the Datalog registry in children in which the device was available. 2. Establishment of groups of children according to IT MAIS, MUSS, Datalog hours/day, Family Involvement and Degree of Hearing Loss, through the preparation of tables with descriptive statistics of these variables according to groups. Tables with frequencies and percentages of the categories of those who participated in the GrAF were also created. The condition set was that the groups were internally ho-mogeneous and heterogeneous among themselves according to the variables IT MAIS and MUSS. The technique used was the average of the distances. The distance between the subjects was measured by Euclidean distance by applying the technique of cluster analysis(15).
Ages of children at the time of analysis were rounded up to 15 days or less for the previous month and 15 days or more for the following month (e.g., 12 months and 13 days = 12 months or 12 months and 17 days = 13 months).
RESULTS
In the pre-determined (PD) group, eight family members of six children participated in GrAF, being 5 mothers (63%), two fathers (25%) and 1 grandmother (12%); and in group Continuous Flow (CF) nine family members participated in GrAF, being six mothers (67%) and three fathers (33%); and on the Control group (C) the GrAF was not carried out (only the therapeutic sessions were). The age of onset of hearing aid use by children seen in ADAPTI ranged from 24 days to 47 months.
The frequency of attendance of parents in ADAPTI was evaluated in order to observe the adherence to the treatment of children. In this study, parents’ compliance to treatment (GrAF and therapy) was analyzed. Nine of the 16 (56.25%) participants attended 66.6% or more of the GrAF sessions and five of 12 (41.66%) participants attended 72.7% or more of the therapy sessions performed. All families were instructed to re-main at the service for two hours to attend both the therapeutic sessions and the GrAF. The dendrogram obtained from the cluster analysis, suggesting the existence of three homogeneous groups according to IT MAIS and MUSS simultaneously is shown in Figure 1.
This type of analysis groups subjects most likely to exhibit similar performances on the analyzed variables. From this analysis, families were organized into three groups:
Group 1: Families FC5, FC6, FC3, C2 and PD2, whose children tended to have lower values of IT MAIS and MUSS. In addition, similarities were found for the attendance higher
than 50% in the therapeutic care and differences of hearing loss in children.
Group 2: Families PD6, C4, FC4, PD1, PD5, whose children composed an intermediate group with regard to the values of IT MAIS and MUSS and had a mean (500 to 2 kHz) hearing loss greater than 80 dBHL.
Group 3: Families C3, PD4, FC2, FC1, whose children ten-ded to have higher values of IT MAIS and MUSS. Furthermore, these children resembled regarding the average (500 to 2 kHz) hearing loss, which was between 55 and 90 dB HL.
The means and medians of the two variables were lower in group 1 than in the other groups. The highest mean and me-dian were shown in group 3. Thus, it can be said that children in group 1 tended to have the lowest values of IT MAIS and MUSS and those in group 3, the highest values. In this aspect, group 2 was an intermediate group. This result can be visuali-zed in the scatterplot of IT MAIS and MUSS, with each point corresponding to one child according to the groups (Figure 2).
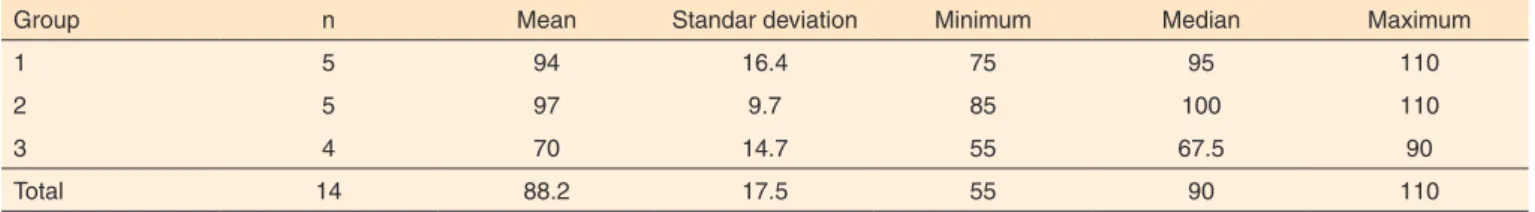
The values of descriptive statistics for Degree of Hearing Loss, Family Involvement and Datalog (hours/day) are pre-sented in Tables 1, 2 and 3 respectively. The individual and mean values of these variables for each group are shown in Figures 3, 4 and 5.
It is observed in Table 1 and Figure 3 that individuals in the group 3 had, on average, a smaller degree of hearing loss than those of groups 1 and 2.
The degree of hearing loss was not a variable that justified the formation of clusters.
Children from families PD2, PD5, C2 presented hearing losses of 110 dBHL (mean 500 to 2 kHz) being represented respectively in groups 1 and 2. Those with the same degree of hearing loss were allocated to different groups regarding responses in IT MAIS and MUSS due to expectations and possibilities of hearing and language presented by each.
The child of family PD2 was unable to undergo surgery of the IC since he had inner ear malformation and ossified cochleas bilaterally. The children of the families C2 and PD5 were being
Note: Group 1 (Families: FC5: Vit - FC6: Vi - FC3: Ir - C2: Br; PD2: Ma); Group 2 (Families - PD6: He; C4: St; FC4: Lu; PD1: Ga; PD5: Ma); Group 3 (Families - C3:
Fr - PD4: Ra - FC2: Ro - FC1: Ed)
Figure 1. Dendrogram from cluster analysis with the variables IT MAIS
and MUSS
evaluated for cochlear implant surgery. Thus, even with similar hearing loss, each child, due to whether or not they received a cochlear implant, could also differ in the questionnaires.
The child of family PD4, from group 3, had hearing loss of 55 dB HL (mean 500 to 2 kHz), which shows that the smaller the degree of the hearing loss, the better the responses of scores found in IT MAIS and MUSS. Probably due to the degree of hearing loss and therapy attendance over 70% (72.7%) there was a good assessment of family involvement (score 4) and also in relation to the use of hearing aids for six hours per day. The hearing aid fitting initiated when the child was 10 months.
Family involvement (Table 2 and Figure 4) was similar in the three groups. Two extremes were found in the evaluations of the degree of family involvement performed by speech
Table 1. Descriptive statistics for hearing loss degree according to group
Group n Mean Standar deviation Minimum Median Maximum
1 5 94 16.4 75 95 110
2 5 97 9.7 85 100 110
3 4 70 14.7 55 67.5 90
Total 14 88.2 17.5 55 90 110
Table 2. Descriptive statistics for family involvement according to group
Group n Mean Standar deviation Minimum Median Maximum
1 5 3.0 1.0 2 3 4
2 5 3.4 0.9 3 3 5
3 4 3.5 0.6 3 3.5 4
Total 14 3.3 0.8 2 3 5
Table 3. Descriptive statistics for Datalog hours/day according to group
Group n Mean Standar deviation Minimum Median Maximum
1 3 3.0 1.0 2 3 4
2 3 3.7 0.6 3 4 4
3 4 5.8 2.6 2 6.5 8
Total 10 4.3 2.1 2 4 8
Figure 5. Individual and mean values of Datalog hours/day according
to group
Figure 3. Individual and mean values of the degree of hearing loss
according to group
Figure 4. Individual and mean values of family involvement according
therapists who met the children in ADAPTI (Figure 4). The FC3 family presented a score 2 on the scale of family involvement, possibly by having attended few therapeutic sessions (54.5%), suggesting little involvement of the family in the hearing rehabilitation process of the child.
In contrast, despite the family FC6 score 2, they attended all scheduled visits (100%), both in therapeutic interventions and in Graf. Therefore, the rationale for the evaluation from the therapist would not be attending the service, as in the previous case. So probably this note reflects the fact that the child has started late in hearing aid fitting.
Children from families FC3 and FC6 received diagnosis and speech and language therapy after two years of age, with 35 and 34 months respectively.
The other end shown in Figure 4 refers to the family PD5, which was received a score of five on the family involvement scale. This score is justified because as soon as the child had her hearing aids fitted (at two months), she simultaneously began ADAPTI and evaluation process for cochlear implant surgery. Parents attended 72.7% of scheduled therapeutic sessions, being involved in all the treatment proposed by the Hearing Health Service.
It is observed that individuals in group 3 tended to use the device for more hours than those in the other groups (Table 3 and Figure 5).
The scarce daily use of hearing aids (two hours) by the child of family FC6, even attending all therapies and GrAF, can be related to the fact that the Brazilian Sign Language (LIBRAS) was the choice of the family from the beginning. In this case, considering low audibility of speech sounds, the use of the device cannot be perceived as a factor that contributes to the communication, considering that LIBRAS became the main communication mode of the child.
Children of families FC2 and C3 from Group 3 use the hearing aid eight and two hours per day, respectively.
The group that demonstrated greater involvement was the one of children who, in most cases, had an average hearing
loss of 55dBHL (PD4), 65 dBHL (C3) and 70dBHL (FC1), representing 75 % (Figure 4). In this group, there was a child with average hearing loss of 90 dBHL (FC2), but with the longest use of hearing aids (eight hours/day). It is noteworthy that this was one of the oldest children in the group, with 80% attendance in therapeutic care, whose family, although with a score 3 in family involvement, was present in GrAF, worried about future issues of the child regarding hearing, language and education. Good answers in the questionnaires occurred becau-se it is an older child (she started the hearing aid fitting at 37 months) and, therefore, quickly acquired the skills questioned at the instruments IT MAIS and MUSS, with high percentage in scores in both instruments.
Another exception in this group is that the child from C3 presented only two hours of use of hearing aids monitored in Datalog. According to the mother, the child was not wearing hearing aids as before (more often) because the twin brother was very ill, burdening the family and leading the mother to put the device less often in the child. In this case, although it is considered a mother who is actively participant, the use of hearing aids does not seem to be appreciated by the family.
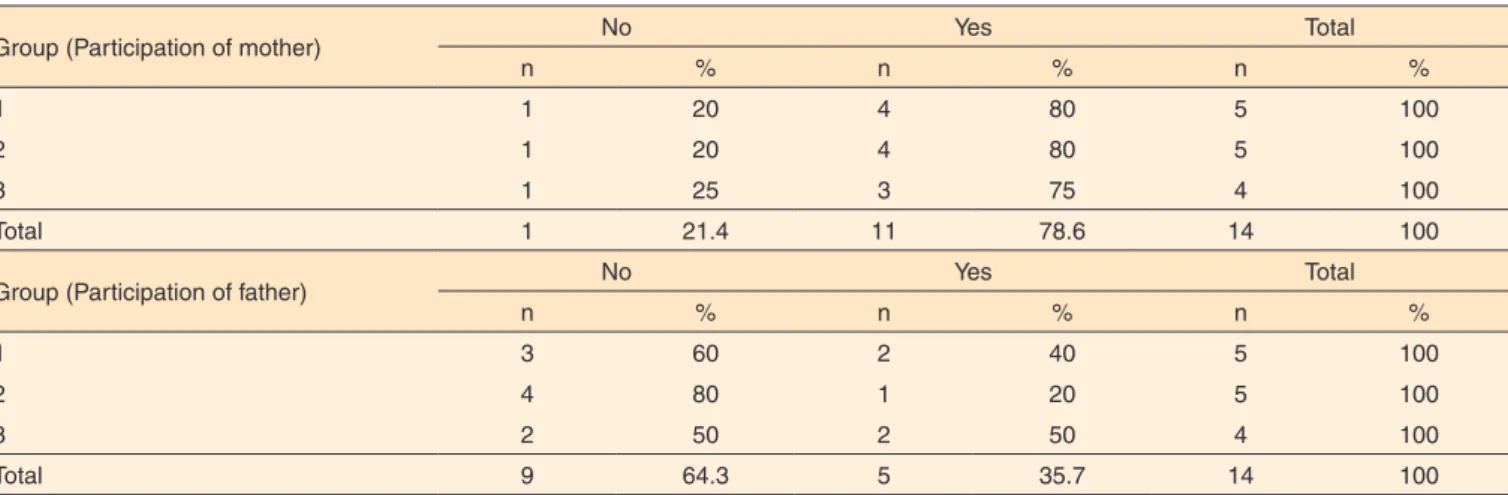
It was observed that most mothers of the three groups par-ticipated in the GrAF. The percentage of parents who did not participate is greater than or equal to 50% in the three groups, with the lowest percentage of participation observed in group 2. There was no difference as to whether or not parents have participated in the GrAF PD or FC given the similarity in frequencies (Table 4).
DISCUSSION
As observed in the present study, the increased participation of mothers in ADAPTI indicates that they spend most of their time with their children and are responsible for following them in appointments and therapy sessions. Because of the fact they exercise professional activities, fathers are less present at these commitments. It is for the speech language pathologist and
Table 4. Frequencies and percentages of “participated in GrAF” (mother) by group/Frequencies and percentages of “participated in GrAF” (father)
by group
Group (Participation of mother) No Yes Total
n % n % n %
1 1 20 4 80 5 100
2 1 20 4 80 5 100
3 1 25 3 75 4 100
Total 1 21.4 11 78.6 14 100
Group (Participation of father) No Yes Total
n % n % n %
1 3 60 2 40 5 100
2 4 80 1 20 5 100
3 2 50 2 50 4 100
audiologist to recognize the importance of fathers in children’s lives and aim to increasingly insert them in the process of auditory (re)habilitation(16-18).
The intervention soon after diagnosis of hearing impaired children is of utmost importance for development of auditory skills, speech and language to occur. Therefore, the use of hearing aids and/or other devices such as cochlear implants is essential(11,18-21).
The fact that the answers are not yet consistent at early sta-ges of hearing aid fitting - depending on the degree of hearing loss - decreases the motivation of parents to insist on the use of the devices. As the answers appear, child and family miss the hearing aids(4).
In this study, adherence to the use of the electronic device was not related to statistical significance to any specific factor given the small number of subjects in the sample. However, there was a trend for better answers on the scale of assessment of family involvement, use of hearing aids and frequency of attendance in therapies of children who had early diagnosis and intervention process. Treatment adherence is a multifactorial process that is comprised of a partnership. It regards to fre-quency, constancy and perseverance in the pursuit of health(22). The involvement of some families in the group and parti-cipation on the proposed activities suggest that this may be a strategy with repercussions on the accession to the process of auditory rehabilitation. In fact, to engage, embrace, and build partnerships and linkages with the family during the speech and language therapy are essential to achieve a favorable outcome and satisfactory results regarding the use of hearing aids by children(5,23).
The diversity in the characteristics of the families in this study on the groups organized according to auditory and langua-ge skills suglangua-gests that special attention is needed at the initial processes of intervention, with procedures of hosting families so that the partnership between the professional and the family can be established in order to promote a more consistent use of hearing aids in everyday situations(23). The more the child has access to information transmitted through the social contacts established, the better the development of oral language will be. Therefore, if the use of hearing aids is not effective and consistent, the child loses auditory information, which leads to communication difficulties(24-27).
The professionals involved need to guide and advise pa-rents by providing clear information on diagnosis, hearing aid use, its benefits and limitations, handling, maintenance and care for the safe use of the device as well as on the progress that the child can achieve with the device and the intervention program. Accordingly, ensuring the adaptation and the daily use of hearing aids allows children to have experiences with their hearing at practically every hour of the day.
The speech language pathologist and audiologist should gui-de parents or guardians on the controls of the gui-device, ear molds, battery and care in relation to handling and maintenance(27,28). It
is important to fit the hearing aids in children as early as possible and also to follow up in a specialized service(11,19). However, our experience with the groups suggests that family comprehen-sion on the importance of hearing rehabilitation depends on motivation strategies and adjustment of expectations, besides the information on the importance of the electronic device.
Importantly, many times a positive attitude to the processes of scheduled appointments may be confused with what the scale of family involvement seeks to determine. Hence the discrepancy found in different families evaluated in this study.
CONCLUSION
The systematic use of hearing aids was the only variable with a strong relationship to auditory and language skills. Degree of hearing loss, age of onset of amplification and therapeutic process with or without participation in the Group of Adhesion did not explain the development of children stu-died. Low adherence to the systematic use of hearing aids by parents who participated in GrAF suggests that specific and short-term goals must be included in the goals to be achieved by the groups.
Manifestations of family involvement mirrored in the willingness to participate not always ensured systematic and consistent use of hearing aids. In this sense, hearing health intervention actions that ensure adherence to treatment are necessary so that result measures may reflect the investment in residual hearing. This suggests that, even in families apparently committed to intervention, it is essential to verify the number of hours of hearing aid use per day through objective measures such as the Datalog.
In the case of profound hearing loss, the sooner the tests to referral to cochlear implant surgery are carried out, the more accurate the positioning of professionals about the prognosis for oral language and hence adaptations to the expectations of the family.
Further studies that involve monitoring results of auditory and language development and characteristics of adhesion to the intervention program in the Hearing Health Services are necessary.
REFERENCES
1. Moeller MP. Early Intervention and language development in children who are deaf and hard of hearing. Pediatrics. 2000;106(3):43-7.
2. Yoshinaga-Itano C. From screening to early identification and intervention: discovering predictors to successful outcomes for children with significant hearing loss. J. Deaf Stud. Deaf Educ (Oxford). 2003;8(1):11-30.
4. Novaes BCAC, Mendes BCA. Terapia fonoaudiológica da criança surda. In: Fernades FDM, Mendes BCA, Navas ALPGP. (Orgs). Tratado de Fonoaudiologia. 2a.ed. São Paulo: Roca; 2009. p. 202-9. 5. Sininger YS, Grimes A, Christensen E. Auditory development
in early amplified children: factors influencing auditory-based communication outcomes in children with hearing loss. Ear Hear. 2010;31(2):166-85.
6. Muñoz K, Roberts M, Mullings D, Harward R. Parent hearing aid experiences. Volta Review. 2012;112(1):63-76.
7. Hoffman J, Beauchaine K. Babies with hearing loss: steps for effective intervention. ASHA Leader. 2007;12(2):8-23.
8. Figueiredo RSL, Novaes, BCAC. Rumo às primeiras palavras: o enquadre na terapia fonoaudiológica do bebê com deficiência auditiva. Rev CEFAC. 2012;5(1):50-8.
9. Nery DM, Novaes BC. Identificação de estratégias no processo terapêutico de uma criança deficiente auditiva. Distúrb Comum. 2001;13(1):49-67.
10. Scappaticci ALSS. A importância do sistema familiar no desenvolvimento da criança: um enfoque para a Pediatria. In: Carvalho ES, Carvalho WB. Terapêutica e prática pediátrica. 2a ed. São Paulo: Atheneu; 2001. p. 73-7.
11. Halpin KS, Smith KY, Widen JE, Chertoff ME. Effects of universal newborn hearing screening on an early intervention program for children with hearing loss, birth to 3 yr of age. J Am Acad Audiol. 2010;21(1):169-75.
12. Novaes BCAC. Hearing impaired children in São Paulo, Brazil: knowledge and attitudes of mothers regarding hearing impairment and early intervention programs, and the implications for habilitation. Columbia: Columbia University; 1986.
13. Robbins AM, Osberger MJ. Meaningful use of speech scales. Indianápolis: University of Indiana School of Medicine; 1990. 14. Zimmerman-Philips S, Osberger MJ, Robbins AM. Infant-Toddler:
meaningful auditory integration scale (IT-MAIS). Sylmar, Advanced Bionics Corporation; 1997.
15. Johnson RA, Wichern DM. Applied Multivariate Statistical Analysis. 3rd ed. New Jersey: Prentice-Hall; 1992.
16. Boscolo CC, Momensohn-Santos TM. A deficiência auditiva e a família: sentimentos e expectativas de um grupo de pais de crianças com deficiência da audição. Distúrb Comum. 2005;17(1):69-75.
17. Caldas FF, Lemos AB, Tschiedel RS. O envolvimento do pai no processo de (re) habilitação auditiva de seu filho deficiente auditivo. Comum Ciênc Saúde. 2009;20(1):17-28.
18. Erenberg A, Lemons J, Sia C, Trunkel D, Ziring P. Newborn and infant hearing loss: detection and intervention, American Academy of Pediatrics. Task Force on Newborn and Infant Hearing, 1998 – 1999. Pediatrics. 1999;103(2):527-30.
19. Harisson M, Rouch J, Wallace J. Trends in age of identification and intervention in infants with hearing loss. Ear Hear. 2003;24(1):89-95. 20. Gatto CI, Tochetto TM. Deficiência auditiva infantil: implicações e
soluções. Rev CEFAC. 2007;9(1):110-5.
21. Prendergast S, Lartz MN, Fiedler BC. Ages of diagnosis, amplification, and early intervention of infants and young children with hearing loss: findings from parent interviews. Am Ann Deaf. 2002;147(1):24-30.
22. Silveira LMC, Ribeiro VMB. Grupo de adesão ao tratamento: espaço de “ensinagem” para profissionais de saúde e pacientes. Interface. 2005;9(16):91-104.
23. Moeller MP, Hoover B, Peterson B, Stelmachowicz P. Consistency of hearing aid use in infants with early-identified hearing loss. Am J Audiol. 2009;18(1):14-23.
24. Serbetcioglu MB. Critical learning period for speech acquisition and screening techniques in early detection of hearing impairment. Turk J Pediatr. 2001;43(2):128-32.
25. Moeller MP. Optimizing early word learning in infants with hearing loss. Audiology Today. 2010;18(1):19-27.
26. Fagan MK, Pisoni DB. Hearing experiences and receptive vocabulary development in deaf children with cochlear implants. J Deaf Stud Deaf Educ. 2010;15(2):149-61.
27. Brazorotto JS. A terapia fonoaudiológica da criança surda. In: Bevilacqua MC, Moret ALM. Deficiência Auditiva: Conversando com familiares e profissionais de saúde. São José dos Campos: Pulso; 2005. p. 203-23.