w w w . j c o l . o r g . b r
Journal
of
Coloproctology
Original
Article
Number
of
lymph
nodes
dissected
in
colorectal
cancer
and
probability
of
positive
nodes,
angiolymphatic/perineural
invasion,
and
intracellular
mucin
in
a
referral
service
Murilo
Zomer
Frasson
∗,
Kaiser
S.
Kock,
Letícia
F.
Monteiro,
Jonas
V.
Romagna
UniversidadedoSuldeSantaCatarina,Tubarão,SC,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received19August2014
Accepted19June2016
Availableonline18July2016
Keywords:
Colorectalneoplasms
Lymphnodes
Lymphnodeexcision
a
b
s
t
r
a
c
t
Amongthemalignancies,colorectalcancerranksfourthinincidenceinBrazil.Themain
prognosticmeasureisrelatedtotheamountofaffectedlymphnodes.Thus,manystudies
trytocorrelatethenumberofextractedlymphnodes,withtheprobabilityofobtaining
positivenodes.
Studyobjectives:Determinewhetherdissection≥12lymphnodesincreasesprobabilityof
findingneoplasticinvolvementinrelationtoresectionoffewer.Assessthepresenceof
angiolymphaticinvasion;perineuralandintracelluarmucinandcorrelateitwithtumor
differentiationandTNMclassification.Correlatetheaverageofpositivenodeswith
angi-olymphaticandperineuralinvolvement.
Methods:PathologicalreportsofpatientsoperatedforCRCfrom1997to2013wereanalyzed.
Aprobability(p)lessthan0.05wasconsideredtoindicatestatisticalsignificance.
Results:Medianoflymphnodessenttoanalysiswas12nodes.Averagenumberoflymph
nodesaffectedwashigherwhena number ≥12 lymphnodes weredissected(p=0.001)
(Kruskal–Wallis).Therewaspositiveassociationbetweenaverageofaffectedlymphnodes
andpresence ofangiolymphatic(p<0.0001)or perineuralinvasion(p=0.024).
Angiolym-phaticandintracellular mucinarelesspresentinwell-differentiatedadenocarcinomas.
PerineuralandangiolymphaticweremorepresentinT4stages.
Conclusions:Dissection≥12lymphnodesincreaseschancesoffindingpositivenodes.There
isrelationbetweenangiolymphaticinvasion;perineuralandintracellularmucinandtype
oftumordifferentiation,aswellasTNMclassification.Averagenumberoflymphnodes
affectedwashigherinpresenceofperineuralorangiolymphaticinvasion.
©2016SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.This
isanopenaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/
licenses/by-nc-nd/4.0/).
∗ Correspondingauthor.
E-mail:murilozf@hotmail.com(M.Z.Frasson).
http://dx.doi.org/10.1016/j.jcol.2016.06.004
2237-9363/©2016SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.ThisisanopenaccessarticleundertheCC
Número
de
Linfonodos
Dissecados
no
Câncer
Colorretal
e
Probabilidade
de
Nodos
Positivos,
Invasão
Angiolinfática,
Perineural
e
Mucina
Intracelular
em
Servic¸o
de
Referência
Palavras-chave:
Neoplasiascolorretais
Linfonodos
Excisãodelinfonodo
r
e
s
u
m
o
Dentreasneoplasiasmalignas,ocâncercolorretalocupaoquartolugaremincidênciano
Brasil.Umadasprincipaismedidasdeprognósticoestárelacionadaàquantidadede
linfon-odosacometidos.Sendoassim,muitostrabalhosestudammeiosdecorrelacionaronúmero
delinfonodosdissecados,comaprobabilidadedeseobteremlinfonodospositivos.
Objetivosdoestudo: Determinarseadissecc¸ão≥12linfonodosaumentaaprobabilidadede
seencontraracometimentoneoplásiconosmesmosemrelac¸ãoàmenorressecc¸ão.Avaliar
apresenc¸adeinvasãoangiolinfática;perineuralemucinaintracelularecorrelacioná-lacom
diferenciac¸ãotumoraleclassificac¸ãoTNM.Correlacionaramédiadenodospositivoscom
acometimentoangiolinfáticoeperineural.
Métodos: Foramanalisadoslaudosanatomopatológicosdepacientesoperadosporcâncer
colorretal(CCR)de1997a2013.Aprobabilidade(p)menorque0,05foiconsideradapara
indicarsignificânciaestatística.
Resultados: Amédiadelinfonodoscomprometidosfoimaiorquandoumnúmero≥12
lin-fonodosforamdissecados(p=0,001)(Kruskal-Wallis).Houveassociac¸ãopositivaentrea
médiadelinfonodosafetadoseapresenc¸adeinvasãoangiolinfática(p<0,0001)ou
perineu-ral(p=0,024).Ainvasãoangiolinfáticaeamucinaintracelularestavammenospresentesem
adenocarcinomasbemdiferenciados.Invasãoperineuraleangiolinfáticaestiverammais
presentesnosestádiosT4.
Conclusões: Adissecc¸ão≥12linfonodosaumentaaschancesdeseencontrarnodo
posi-tivo.Existerelac¸ãoentreinvasãoangiolinfática;perineuralemucinaintracelulareotipode
diferenciac¸ãotumoral,bemcomoaclassificac¸ãoTNM.Amédiadelinfonodos
comprometi-dosfoimaiornapresenc¸adeinvasãoperineuralouangiolinfática.
©2016SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda.Este
´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/
licenses/by-nc-nd/4.0/).
Introduction
Colorectal cancer(CRC)is the fourthmostfrequent
malig-nancyinBrazil.Itisestimatedthatin2014,32,600newCRC
caseswerediagnosedinthiscountry.Ofthese,15,070were
maleand17,530werefemalesubjects,corresponding toan
estimatedriskof15.44and17.24casesper100,000population
formenandwomen,respectively.1 Intheworld,CRCisthe
thirdmostprevalentcancer;andinWesterncountries,isthe
secondleadingcauseofcancer-relateddeaths.2
DuetothehighprevalenceofCRC,agreatemphasisisgiven
tothepublicationofstudiestoevaluatethecharacteristicsof
thisdisease,aswellasthedeterminantfactorsofitscourse.
In1932,Dukesproposedthatthedepthoftumorinvasionin
thecolonicwall,lymphnodeinvolvement,andthepresence
ofmetastaseswouldbedeterminingfactorsfortumorstaging
and,todate,theseareconsideredthemostimportantfindings
fordiseaseprognosis.3
Inrecentyears,therelationshipbetweenthenumber of
resected lymphnodes and those compromisedbyCRC, i.e.
thelymphnoderatio (LNR),hasbeen subjecttoevaluation
inseveralstudies.ResearchevaluatingLNRinpatientswith
primarytumorsofthestomach,bladder,breast,andpancreas
revealedtheexistenceofarelationshipbetweenthe
propor-tionofpositivelymphnodes,disease-freesurvival,andoverall
survival.4–8
Theminimumnumberoflymphnodesthatmustbe
diss-ectedhasbeenthesubjectofsomestudies,andsomeofthem
suggested12astheminimumnumberoflymphnodestobe
dissected.9,10Thisisalsothenumberthathasbeenaccepted
bytheAmericanJointCommitteeonCancerandtheWorld
CongressofGastroenterologyinordertostratifythepatients
as free of metastatic disease. In addition to these
organi-zations, in2007the Association ofColoproctologyofGreat
BritainandIrelandalsostartedrecommendinganaverageof
12lymphnodes.11
LymphnodedissectioninCRCcasesmanagedtoestablish
itselfasanimportantmethodforprognosticevaluation.Thus,
ithasbecomecriticalthatmorestudiesbepublishedinorder
toevaluatethismethod,sothatonecandeterminemore
pre-ciselyitstruepotentialinrelationtowhatitcanrepresentin
termsofknowledgeandprognosiswithrespecttoCRC.
Theobjectivesofthisstudyaresetforthbelow.
Primaryobjective
(1) To determine if the dissection of ≥12 lymph nodes
increasestheprobabilityoffindingneoplasticinvolvement
in thesestructures, comparedwith a lessernumber of
resectedlymphnodes.
Secondaryobjectives
(2) Toevaluatethepresenceofangiolymphaticandperineural
invasionandintracellularmucinandtocorrelatethe
(3) Tocorrelatetheaverageofpositivenodeswith
angiolym-phaticandperineuralinvolvement.
Methods
Allpathologyreportsofsurgicalspecimensofpatients
under-goingelectiveornon-electivesurgeryforCRCfrom January
1997toDecember2013,operatedintheHospitalNossa
Sen-horadaConceic¸ão,inthecityofTubarao–SC,wereanalyzed
inacase-series,cross-sectional,retrospectivestudy.Thedata
wereselectedwiththeuseofacollectioninstrument
devel-opedbytheauthors,whichincludedthefollowingvariables:
dateofthepathologyreport,patient’sgenre,year,patient’
s age, tumor location,size of the surgical specimen, TNM
classification,Astler–Collerclassification,typeofsurgery
per-formed,numberofdissectedlymphnodes,numberofaffected
lymphnodes,tumordifferentiation,presenceofintracellular
mucin,angiolymphaticinvasion,andperineuralinvasion.
Allpathologyreportsofsurgicalspecimensdiagnosedwith
colorectal adenocarcinoma, classified as belonging to any
TNMclassificationstage,wereincludedinthisstudy.Patients
whometthefollowingcriteriawereexcluded:
1. CRCdiagnosisassociatedwithinflammatoryboweldisease
(Crohn’sdiseaseorulcerativecolitis).
2. Neoplasmswithahistopathologicdiagnosisnot
compati-blewithadenocarcinoma.
3. Patientsundergoingneoadjuvanttherapy.
All patients were operated on by laparotomy or
laparoscopy, and the surgical treatment chosen followed
the conventional pattern of resection, including
lym-phadenectomyand,inthecaseofrectaltumors,mesorectal
resection.
ThestudywasapprovedbytheResearchEthicsCommittee
(CEP) ofthe Universidade doSulde Santa Catarina
(proto-colnumber13.004.4.01.III).Thestudyfollowedtheregulations
ofResolution466of2012.Thankstotheabsenceofadirect
contactwithpatientsinthestudy,thefreeandinformed
con-sentterm(FICT)wasnotnecessary.Consentoftheinstitutions
involvedfortheuseofthedatawasobtained.
Datawerecatalogedintheformofanelectronic
spread-sheet(MicrosoftExcel)andtransferredforstatisticalanalysis
toEpiInfo/SPSSversion18software.Qualitativevariableswere
describedbyabsoluteandrelativefrequencies,and
quantita-tivevariablesweredescribedasamean,medianandstandard
deviation.Statisticalanalyseswereperformedusingthe
chi-squaredtest,Student’st-test,Kruskal–WallistestandFisher
testwithMonteCarlocorrection,asneeded.Thelevelof
sig-nificancewassetat5%.
Results
Intotal,thestudyinvolved290patientswhounderwent
sur-gicaltreatmentforCRCresectionbetween1997and2013.The
meanagewas61.9(SD=13.4)yearsandthemedianagewas63
years.Malesubjectswereslightlymoreaffectedversusfemale
subjects.Ofallpatients,149(51.4%)weremen.Themeanage
ofthepatientsatthetimeofsurgerywas62.8yearsformen
and61.0yearsforwomen.T3isthemostprevalenttumor
stag-ingamongpatients(229cases,i.e.73%ofthetotal).Ofthe290
patients, 151(52.10%) had≥12 lymphnodesdissected.The
medianofthenumberoflymphnodessentfor
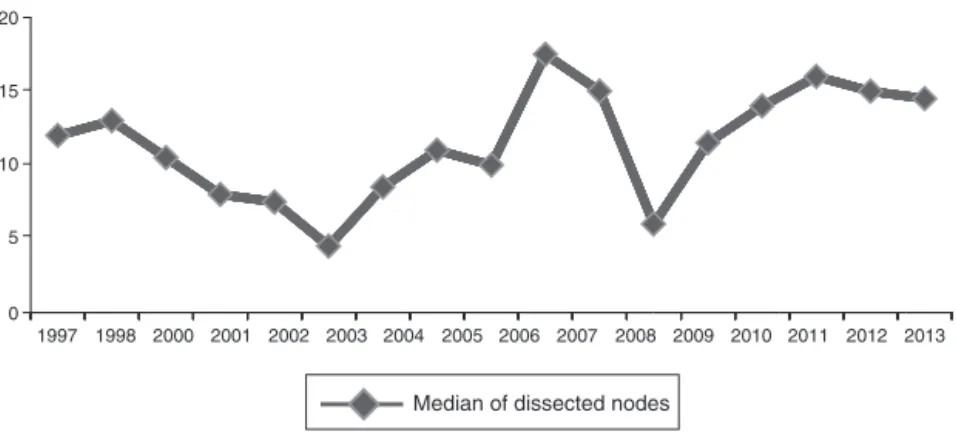
histopatholog-icalanalysiswas12(range:1–53).Fig.1illustratesthemedian
forlymphnodesdissectedoverthestudiedyears.
Ofall the patientsstudied, only17had metastasis (M1)
by TNM classification at the time of surgery,
represent-ing 5.9%. The most common tumor differentiation was a
well-differentiatedadenocarcinomafor212patients(73.1%).
Table1liststheinformationrelatedtothefollowingvariables:
gender,anatomicalsite,tumorinvasion(T),affectedregional
lymphnodes(N),distantmetastasis(M)andtumor
differen-tiation.Table2liststheproportionofpositivelymphnodes,
accordingtothenumberofanalyzedganglia.
Thestudyshowedthatwhen≥12lymphnodesare
dissec-ted,theprobabilityoffindingapositivenodeishigherversus
asmallernumberofnodesresected(p=0.001)(Table3).
Theprobabilityofanangiolymphaticinvasionwaslowerin
thewell-differentiatedtypethaninmoderatelydifferentiated
andundifferentiatedtypes(p=0.0005).Thewell-differentiated
typewasthatthatpresentedleastintracellularmucinin
rela-tiontomoderatelydifferentiatedandundifferentiatedtypes
(p=0.001)(Fisher’sexacttestwithMonteCarlocorrection).
Perineuralinvasionwassignificantlymorepresentincases
of moderately differentiated adenocarcinoma versus other
subtypes (p<0.01) (Fisher test). This same poor prognosis
1997
Median of dissected nodes
Median of dissected nodes
2003 2002 2001
2000 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 1998
20
15
10
5
0
Table1–Generalcharacteristicsofthestudysample.
Variable Total <12resectednodes ≥12resectednodes p-Value
n % n % n %
Gender
Male 149 51.4 69 46.31 80 53.69 0.570
Female 141 48.6 70 49.65 71 50.35
Anatomiclocation
Colon,unspecified 108 37.2 54 50.00 54 50.00 0.475
Rectosigmoid 82 28.3 39 47.56 43 52.44
Rightcolon 33 11.4 11 33.33 22 66.67
Colonandrectum 21 7.2 12 57.14 9 42.86
Sigmoid 16 5.5 9 56.25 7 43.75
Rectum 11 3.8 7 63.64 4 36.36
Leftcolon 9 3.1 5 55.56 4 44.44
Largeintestineandanus 5 1.7 1 20.00 4 80.00
Transversecolon 4 1.4 1 25.00 3 75.00
Leftcolonandsigmoid 1 0.3 0 0.00 1 100.00
Tumorinvasion(T)
T0 0 0 0.020
T1 6 2.1 4 66.67 2 33.33
T2 26 9 19 73.08 7 26.92
T3 229 79 106 46.29 123 53.71
T4 29 10 10 34.48 19 65.52
Affectedregionallymphnodes(N)
N0 154 53.1 82 53.25 72 46.75 <0.001
N1 67 23.1 41 61.19 26 38.81
N2 68 23.4 15 22.06 53 77.94
N3 1 0.3 1 100.00 0 0.00
Distantmetastasis(M)
MX 273 94.1 135 49.45 138 50.55 0.038
M0 0 0 0 0
M1 17 5.9 4 23.53 13 76.47
Tumordifferentiation
Welldifferentiated 212 73.1 101 47.64 111 52.36 0.184
Moderatelydifferentiated 42 14.5 21 50.00 21 50.00
Undifferentiated 13 4.5 3 23.08 10 76.92
Othera 23 7.9 14 60.87 9 39.13
a Rankedamongwell-tomoderatelyundifferentiated(n=22)andadenomucinous(n=1).
Table2–Proportionofpositivelymphnodesaccordingtothenumberofgangliaanalyzed.
Numberofnodes examined
Numberof patients
Patientswith +nodes
%+nodes Meanof+nodes Standard
deviation
0–4 36 14 38.9 0.78 1.10
5–9 71 29 40.8 1.21 1.98
10–14 75 33 44 2.20 3.53
15–19 53 29 54.7 4.28 5.11
20–24 30 15 50 2.23 4.16
25–29 15 10 66.7 7.20 8.89
≥30 10 5 50 8.50 11.68
Table3–Meanofpositivenodesinconnectionwiththedissectionof12ormorelymphnodes.
Lymphnodes Patients Compromised
lymphnodes
Mean Variance Standard
deviation
<12 139 179 1.2878a 4.8731 2.2075
≥12 151 587 3.8874a 35.7139 5.9761
Table4–Comparisonbetweenthemeannumberof compromisedlymphnodesandthepresenceof perineuralorangiolymphaticinvasion.
Meanof compromised
nodes
Number Standard
deviation
Perineuralinvasion present
5.28a 18 7.25
Perineuralinvasion absent
2.59a 247 4.63
Angiolymphatic invasionpresent
4.19b 112 5.99
Angiolymphatic invasionabsent
1.74b 153 3.54
a p=0.024.
b p<0.0001.
factorwasalsomoreprevalent inT4(24%)comparedtoT3
(5.6%),T2(0%)andT1(0%)staging(p=0.013).Perineural
inva-sion was also more present when there was atleast one
affected regional lymphnode (N1) (10.9%)or four or more
affectedlymphnodes(N2)(10.8%)versuslymphnodeswith
noinvolvement(N0)(2.9%)(p=0.028).
Angiolymphaticinvasionwas significantlymorepresent
whenthetumorwasatT4stage(72%)versusalesserdegree
ofinvasion(p=0.01). Regarding thepresenceor absence of
metastasis, the angiolymphatic invasion was more
preva-lent in cases with distant metastasis (40.2%) (chi-squared
test=0.006246).Positivelymphnodeinvolvementalsoshowed
ahigherprevalenceofangiolymphaticinvasionthan inthe
absenceofaffectedlymphnodes(N0,29.4%),(N1,53.1%),(N2,
58.5%)(p=0.0001).
Thepresenceofintracellularmucinhadasignificant
cor-relationonlyontumordifferentiation,beingmorepresentin
undifferentiatedadenocarcinoma(30.8%)(p=0.005).
Inthecomparisonbetweenthemeannumberofaffected
lymphnodeswithperineuralorangiolymphaticinvasion,it
wasobservedanincreaseinthemeanofpositivenodeswhen
thesefactorsarepresent(Table4).
Themostcommonlyperformedsurgeriesinthestudyand
thepercentageofcompromisedgangliabytypeofsurgeryare
listedinTable5.
Discussion
AccordingtotheCentersforDiseaseControlandPrevention
(CDC), the majority ofpatients diagnosed withCRC in the
UnitedStatesbelongtothemalegender,withapercentage
of51.8%(70,099patients)inapopulationof135,260patients
diagnosedintheyear2011(themostrecentyearavailable).12
SimilartotheUSdata,thisstudyalsofoundagreater
preva-lenceofmen,with51.4%.Bycomparison,theBraziliandata
citeanestimated32,600newcasesofCRCdiagnosedin2014.1
Thisstudyshowedthatthemeanageatthetimeoftumor
resectionisapproximately 61years.Whenoneaddstothis
thefactthat,inoursample,mostofthepatientswereseen
in advancedstages, both inthe TNMclassification, witha
prevalenceofT3andintheAstler–Collerclassification,with
B2class,onecanverifythatthediagnosticofCRCisnottimely
obtained.Thus,itshouldbenotedtheimportanceofan
ade-quateCRCscreening,especiallysincethistumorhasaslow
evolution, allowingconsiderable time forits detection and
treatment.
OtherstudieshavealsopresentedT3andN0stagesasthe
mostprevalent,13–15asisthecaseinthestudybyOliveiraetal.
of74patientswithcolorectalcancer;inthisstudy,62.1%of
patientshadaT3classificationand59.5%wereinN0stage.
Forthesakeofcomparison,Jacomoetal.studied90patients
withrectalcancer,excludingpatientswithcolonictumor,with
similarfindingsforT3(55.5%)andN0(67.7%)stages.
Basedoncollecteddata,onecantraceacurvethatshows
thelymphnodedissectionovertheyears–avaluabledatato
verifytheperformanceofthehealthserviceintheareasince
lymphnodecollectionhasbeenusedasameasuring
instru-mentofmedicalcarequality.16 Thus,itispossibletoreport
that inthelast four yearsthe medianforextractedlymph
nodesremainedabovetheminimumnumberindicated.This
monitoringbecomesimportantwhenweconsiderthatLanza
etal.concludedthattheevaluationofafewregionallymph
nodescanresultinanunderstagingofN0tumors.17
Themedianofresectedlymphnodeswas12,whichagrees
withthenumberproposedbyvariousagenciesandstudies.9,11
However,consideringtheresultsinTable3, itappearsthat
only 52.07%ofpatients underwent resection of>12 lymph
nodes.Thus,theuseofthemedianasthesoleformof
assess-ment is not fully indicated, since a large part (47.93%) of
Table5–Percentageofnumberofaxillarynodesaccordingtothetypeofsurgery.
Typeofresection Numberof
patients
Patientswith node+
% Meanof
ganglia+
Standard deviation
Rectosigmoidectomy 190 88 46.3 2.77 4.98
Totalcolectomy 20 6 30 0.85 2.25
Hemicolectomy,unspecified 20 13 65 4.4 7.01
Amputationofrectum 17 8 47.1 2.76 4.01
Colectomy,unspecified 14 7 50 2.36 3.43
Hemicolectomy 10 3 30 0.7 1.16
Leftsigmoidectomy 7 4 57.1 1.43 1.62
Righthemicolectomy 6 3 50 3.5 4.72
Transversectomy 3 1 33.3 2.67 4.62
patientshadlessthan12oftheirlymphnodesresected.Thus,
besidesthemedian,weshouldalsoassessthepercentageof
patientsundergoingresectionof12ormorelymphnodes.
Wecouldnotsettherealreasonforthenumericaldecline
oflymphnode dissectionsin2002and2008, shownin
fig-ure. However,onepossibleexplanationisthe fact thatthe
vastmajorityofsurgeriesperformedinthisstudyconsisted
ofrectosigmoidectomy procedures.Onestudywhich
exam-ined388patientswithCRCshowedagreatertendencyforthe
resectionoffewerlymphnodesinthedistalregionsofthe
colon,comparedtowhatoccursmoreproximalregions.18
Butitbecomescleartheimportanceofsuchmonitoringfor
theresectionoflymphnodes.Baxteretal.,ina
population-basedstudy,foundthatin2001themajorityofpatientswith
CRCwerestillreceivinganinadequatelymphnode
evalua-tionintheUnitedStates,whereonly37%ofthepatientswere
having≥12lymphnodesresected.9
Stillwithregardtothenumberofdissectedlymphnodes,
this study demonstratedthat whenone gets≥12 nodes,it
becomesmorelikely thefinding of anode affected bythe
tumor.However,Yoshimatsuetal.reportthat≥9lymphnodes
wouldbetheminimumnumbertobeobtainedinthecaseof
colorectaltumorswithaBclassificationintheDuke’ssystem
–thestagemostcommonlyfoundsothatonecouldassess
the negativity oflymph node involvement.10 On the other
hand,Kimetal.,bydividingthelymphnoderesectioninto0–4,
5–9,and10–14groups,foundasignificantlyhigher
probabil-ityoffindingpositivenodesfromanumberof10–14resected
nodes19–averysimilarresulttothatobtainedinthepresent
study.Thus,aresectionof12lymphnodesissuggested,
tak-inginto accountthatathreetimeslargermeannumber of
positivelymphnodeswasobtainedwhen≥12lymphnodes
wereresected.Thisfindingunderlinestheimportanceofan
accuratelymphnoderesection,byallowingagreaternumber
ofdetectionsofnodalinvolvement,whichwouldagreewith
previousstudiesandwithwhathasbeenproposedbythemain
guidelines.9–11
CRCmayexhibitsomefeaturesthat areassociatedwith
a poor prognosis, such as perineural invasion,
angiolym-phaticinvasionandthepresenceofintracellularmucin,20–22
althoughsomeauthorsalsocommentontheneedformore
studieson the prognosticvalueofsuchelements.23 Inour
sample, it was found that in the well-differentiated
sub-typetherewasadecrease inangiolymphaticinvasion.This
factrevealsaninverseassociationbetweenthesevariables,
suggestingthataneoplasiawithahigherdegreeof
differenti-ationislesslikelytoprogresswithinvolvementofbloodand
lymphvessels.Intracellularmucinwasalsolessprevalentin
suchsubtype,whichcouldbeenvisagedwhenonetakesinto
accounttheexpectationofalessaggressivebehaviorwitha
well-differentiatedtumor.
Thefinding ofacorrelationofintracellularmucinsolely
withtumordifferentiationmaysuggestthatthis
characteris-ticisnotrelatedtothelevel ofinvasiveness,butonlywith
thedifferentiationoftheneoplasticcells.However,thisstill
remainsapoorprognosticindicator,duetotheassociation
withpoorlydifferentiatedadenocarcinoma.
We also observed that the mean number of
compro-misedlymph nodes was significantly higher incases with
perineuralorangiolymphaticinvasion;however, duringour
databasesurvey,nostudiesevaluatingtheseassociationswere
found.
The sitespecifically most affected byCRC was the
rec-tosigmoid,despitethelargenumberofpatientswhosereports
did not indicate the tumorsite, which affected the
analy-sisofthisvariable.However,bycheckingthemostcommon
typeofsurgery,itwasobservedthatrectossigmoidectomywas
themostcommonprocedure,indicatingthatthiswasindeed
the preferredsite ofthe neoplasm.Saad-Hossne etal.also
demonstratedthatsigmoidandrectumwerethemost
com-monsites.24
Conclusion
Thisstudyagreeswithothersimilarstudies;wecould
demon-stratethatthedissectionof≥12lymphnodesincreasesthe
chancesoffindingapositivenodecomparedtothedissection
offewernodes.Itwasalsoobservedarelationshipbetween
angiolymphaticinvasion,perineuralinvasionand
intracellu-lar mucin and the type oftumor differentiation and TNM
classification.Inaddition,anotherfindingwasthatthemean
numberofcompromisedlymphnodesissignificantlyhigher
whenaperineuralorangiolymphaticinvasionispresent.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.MinistériodaSaúdeInstitutoNacionaldeCâncer.Estimativa 2014:incidênciadecâncernoBrasil.RiodeJaneiro:INCA; 2014.
2.CentersforDiseaseControlandPrevention(CDC).Vitalsigns: colorectalcancerscreening,incidence,andmortality–United States,2002–2010.MMWRMorbMortalWklyRep.
2011;60:884–9.
3.DukesCE.Theclassificationofcanceroftherectum.JPathol Bacteriol.1932;35:323–32.
4.CelenO,YildirimE,BerberogluU.Prognosticimpactof positivelymphnoderatioingastriccarcinoma.JSurgOncol. 2007;96:95–101.
5.PersianiR,RauseiS,BiondiA,BocciaS,CananziF,D’UgoD. Ratioofmetastaticlymphnodes:Impactonstagingand survivalofgastriccancer.EurJSurgOncol.2007;34:519–24.
6.HerrHW,BochnerBH,DalbagniG,DonatSM,ReuterVE, BajorinDF.Impactofthenumberofthelymphnodes retrievedonoutcomeinpatientswithmuscleinvasive bladdercancer.JUrol.2002;167:1295–8.
7.SchiffmanSC,MCMastersKM,ScogginsCR,MartinRC, ChagparAB.Lymphnoderatio:aproposedrefinementof currentaxillarystaginginbreastcancerpatients.JAmColl Surg.2011;213:45–52.
8.BhattiI,PeacockO,AwanAK,SemeraroD,LarvinM,HallRI. Lymphnoderatioversusnumberofaffectedlymphnodesas predictorsofsurvivalforresectedpancreatic
adenocarcinoma.WorldJSurg.2010;34:768–75.
10.YoshimatsuK,IshibashiK,UmeharaA,YokomizoH,Yoshida K,FujimotoT,etal.Howmanylymphnodesshouldbe examinedinDukes’Bcolorectalcancer?Determinationon thebasisofcumulativesurvivalrate.Hepatogastroenterology. 2005:1703–6.
11.AssociationofColoproctologyofGreatBritainandIreland. Guidelinesforthemanagementofcolorectalcancer.London: AssociationofColoproctologyofGreatBritainandIreland; 2007.p.53–65.
12.U.S.CancerStatisticsWorkingGroup.UnitedStatescancer
statistics:1999–2011incidenceandmortalityweb-based
report.Atlanta,GA:DepartmentofHealthandHuman
Services,CentersforDiseaseControlandPrevention,and
NationalCancerInstitute;2014.Availableat:
http://www.cdc.gov/cancer/colorectal/statistics/index.htm
[accessedin15.06.15].
13.OliveiraRG,FariaFF,LimaJuniorACB,RodriguesFG,Andrade MMdA,GomesDMBM.Cirurgianocâncercolorretal– abordagemcirúrgicade74pacientesdoSUSportadoresde câncercolorretalemprogramadepós-graduac¸ãolatosensu emcoloproctologia.RevBrasColo-Proctol.2011;31:44–57.
14.JacomoAL,MartinezCAR,SerraMMP,AkamatsuFE,Pereira JA,FigueiredoMA.Prognosticimpactoflymphnode metastaticratioon5-yearsurvivalofpatientswithrectal cancernotsubmittedtopreoperativechemoradiation.J Coloproctol.2011;31:311–24.
15.GreenJ,WatsonJ,RocheM,BeralV,PatnickJ.Stage,gradeand morphologyoftumorsofthecolonandrectumrecordedin theOxfordCancerRegistry,1995–2003.BrJCancer. 2007;96:140–2.
16.FieldK,PlatellC,RiegerN,SkinnerI,WattchowD,JonesI, etal.Lymphnodeyieldfollowingcolorectalcancersurgery. ANZJSurg.2011;81:266–71.
17.LanzaG,GafàR,DecarliN.Pathologicalfactorsinvolvedin lymphnodestatusdeterminationincolorectalcarcinoma: analysisof166caseswithlong-termfollow-up.Pathologica. 2001;93:631–9.
18.PappasAV,LangoudianakisEE,DallianoudisIG, KotzadimitriouKT,KoronakisNE,ChrysikosID,etal. Differencesincolorectalcancerpatternsbetweenrightand leftsidedcolorectalcancerlesions.JBUON.2010;15:509–13.
19.KimJ,HuynhR,AbrahamI,KimE,KumarRR.Numberof lymphnodesexaminedanitsimpactoncolorectalcancer staging.AmSurg.2006;72:902–5.
20.DurantePA,BrombergHS,BarretoE,CapellanoG,deGodoy CA.Importânciadainvasãoneuralelinfáticanoprognóstico doadenocarcinomacolorretal.RevistadaAssociac¸ãoMédica Brasileira.2004;50:21–6.
21.doEspíritoSantoGGF,deAguilar-NascimentoJE,KishimaMO, TakiuchiA.Correlac¸ãodefatoresanatomopatológicoscoma sobrevidadepacientesoperadosporadenocarcinoma colorretal.RevistadoColégioBrasileirodeCirurgiões. 2008;35:182–7.
22.MulcahyHE,TonerM,PatchettSE,DalyL,O’DonoghueDP. IdentifyingstageBcolorectalcancerpatientsathighriskof tumorrecurrenceanddeath.DisColonRectum.
1997;40:326–31.
23.ComptonCC,Fenoglio-PreiserCM,Petti-grewN,FieldingLP. AmericanJointCommitteeonCancerPrognosticFactors ConsensusConference:ColorectalWorkingGroup.Cancer. 2000;88:1739–57.