w w w . j c o l . o r g . b r
Journal
of
Coloproctology
Original
Article
Rectal
cancer
survival
in
a
Brazilian
Cancer
Reference
Unit
Romualdo
da
Silva
Corrêa
a,b,c,∗,
Francisco
Edílson
Leite
Pinto
Junior
a,b,c,
Lucas
Vinícius
Silva
dos
Santos
c,
Mariana
Carlos
de
Góis
c,
Rumenick
Pereira
da
Silva
d,
Hylarina
Montenegro
Diniz
Silva
e aLigaNorteRiograndenseContraoCâncer,Natal,RN,BrazilbUniversidadeFederaldoRioGrandedoNorte(UFRN),Natal,RN,Brazil
cUniversidadePotiguar(UnP),Natal,RN,Brazil
dUniversidadeFederaldeMinasGerais(UFMG),DepartamentodeEstatística,BeloHorizonte,MG,Brazil
eUniversidadeFederaldoRioGrandedoNorte(UFRN),MaternidadeEscolaJanuárioCicco,Natal,RN,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received4April2016 Accepted25April2016 Availableonline30June2016
Keywords: Colorectalcancer Surgery
Survival
a
b
s
t
r
a
c
t
Colorectalcancerisoneofthemostcommonmaligntumorsinmenandwomenalloverthe world.Inspiteofpreventionadvancesinthelastfewyears,worldwideincidenceremains significant,aboutonemillionperyear.
Objectives: Evaluaterectalcancersurvivalinpatientsdiagnosedandsurgicallytreatedatthe CancerReferenceUnitatRioGrandedoNorteState,Brazil.
Methods:Observationalretrospectivestudycomposedby135patientsassistedfrom2007 to 2014 at Doctor Luiz Antonio Hospital, Natal, Brazil. Data were collected from the patientrecordsrevisionandsurvivalrateswerecalculatedandanalyzedbynon-parametric Kaplan–MeierandWilcoxontests,respectively.Allpatientsweresubmittedtosurgical treat-ment,chemotherapyand/orradiotherapy.
Results:Overallsurvivalwas62%insevenyears,whiledisease-freesurvivalinone,three andfiveyearswas91.7%,75.5%and72.1%,respectively.
Conclusion: Overallsurvivalanddisease-freesurvivalremainedenhanceduntiltheendof thestudy,suggestingthatthetreatmentprotocolsusedintheinstitutionhaveshowntobe effective.
©2016SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.This isanopenaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/
licenses/by-nc-nd/4.0/).
∗ Correspondingauthor.
E-mail:romualdocorrea@uol.com.br(R.S.Corrêa).
http://dx.doi.org/10.1016/j.jcol.2016.04.015
Sobrevivência
de
câncer
colorretal
em
uma
Unidade
de
Referência
do
Câncer
Palavras-chave: Câncercolorretal Cirurgia Sobrevida
r
e
s
u
m
o
Ocâncercolorretaléumdostumoresmalignosmaiscomunsemhomensemulheresem todoomundo.Apesardasmelhoriasnaprevenc¸ãonosúltimosanos,aincidênciaglobal aindaéexpressiva,cercadeummilhãoporano.
Objetivos: Avaliarasobrevidadocâncerderetonospacientesdiagnosticadosetratados cirurgicamentenaUnidadedeReferênciadoCâncernoRioGrandedoNorte,Brasil. Métodos:Estudoobservacionalretrospectivocompostopor135pacientes,compreendidono períodode2007a2014noHospitalDr.LuizAntônio,Natal,Brasil.Osdadosforamcoletados atravésdarevisãodeprontuárioseassobrevidasforamcalculadasecomparadasutilizando, respectivamente,osmétodosnão-paramétricosdeKaplan-MeieretestedeWilcoxon.Todos ospacientesforamsubmetidosatratamentocirúrgico,quimioterápicoeradioterápico. Resultados: Asobrevidaglobalfoide62%emseteanos,sendoasobrevidalivrededoenc¸a emum,trêsecincoanosde91,7%,75,5%e72,1%,respectivamente.
Conclusão:Assobrevidasglobalelivredadoenc¸asãoelevadasatéoencerramentodoestudo, oquedemonstraqueosprotocolosdetratamentoutilizadosnainstituic¸ãotêmsemostrado eficazes.
©2016SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/
licenses/by-nc-nd/4.0/).
Introduction
Colorectalcancer(CRC)isoneofthemostcommon malign tumorsinmenandwomenallovertheworld.Inspiteof pre-ventionadvancesinthelastfewyears,worldwideincidence remainssignificant(aboutonemillionperyear).CRCcauses morethan500,000deathsperyearandisthethirdmost com-moncauseofcancer-relateddeaths.
BrazilianNationalCancerInstituteestimatesfortheyear of2016inBrazil16,660newlydiagnosedcasesofCRCinmen and17,620inwomen.1
Inaregionalperspective,excludingnon-melanoma skin tumors,CRC isthe fourthmostfrequentinmenin Brazil-ianNortheast (5.34/100,000).For women, isthe third most frequentinthesameregion(8.77/100,000).2
Manyriskfactorscouldcontributetothedevelopmentof CRC,asage,diet,geneticfactors,predisposingmedical con-ditionsandtobacco.Peoplewithmorethan40yearsagehave higherriskofCRCdevelopment,withapeakat65yearsagein UnitedStates.Occidentaldietisalsoariskfactorforcolon car-cinomaduetothehighintakeofanimalfat,exposingcolonic mucosatohighlevelsofcarcinogeniccompounds.The occi-dentallowfiber dietalsopromotesalowintestinaltransit, whichincreasestheexpositiontimetocoloniccarcinogenic.3 Considering genetic factors, susceptibility to CRC includes well-definedhereditarysyndromes,asLynchSyndromeoften calledhereditarynonpolyposiscolorectalcancer(HNPCC)and Familial Adenomatous Polyposis (FAP). Therefore, it is rec-ommended that family history of CRC patients should be consultedandconsideredinariskevaluation.4
Avarietyofsurgicalapproaches,consideringlocationand extension ofthe disease, are used to treatthe rectal can-cerprimarylesions.Thesemethodsincludelocalprocedures,
aspolypectomy,transanalexcisionandtransanalendoscopic microsurgery,andmoreinvasiveproceduresinvolving trans-abdominal resection (for example, low anterior resection, proctectomy with total mesorectal excision and coloanal anastomosisorabdominoperianalresection).4
Therapy forstage II (T3-4disease, without lymph node involvement) or for stage III(positive lymph node without distant metastasis)rectal cancer often includemultimodal treatment with an association of neoadjuvant/adjuvant chemotherapyduetothehighriskoflocoregionalrecurrence. Thisrisk isassociatedwiththe rectumproximitytopelvic structuresandorgans,theabsenceofserousaroundthe rec-tum and the technical difficulties in having wide surgical resectionmargins.4
Survivalisanessentialpartinthestudyofpatients sub-mittedtocolorectalcancertreatment.Statisticalanalysisas survival analysisrefers tothe study ofdatarelated to the timeoftheeventofinterest.Inotherwordsreferstothetime betweenoneinitialeventwhenonepatientorobjectstartsone specificstageandafinalevent,whenthisstageischanged. Thistimeisnamedlifetimeorfailuretimeandcouldbesince deathasaconsequenceofdiseaseoratimeuntilonerelapse event.5
About50–60%ofCRCpatientswilldevelopmetastasisand 80–90%ofthemwilldevelopresectablemetastaticliver dis-ease.Metastaticdiseasefrequentlydevelopsinametachronic wayafterlocoregionalcolorectalcancertreatmentandliveris themostcommonorganinvolved.4
compromisedlymphnodesrepresentsasignificantprocedure inanatomopathologicalanalysisofoperatoryspecimensfrom patientssubmittedtocolorectalcancertreatment.6
CRChasagoodprognosticwhendiseaseisdiagnosedat ini-tialstages.5-yearoverallisabout55%indevelopedcountries and40%indevelopingcountries.Asoccurstoincidence, mor-tality rates due to CRC are lower in women than in men worldwide,exceptintheCaribbean.2
Therefore,theaimofthisstudyistoevaluatesurvivalof patientswithrectumcancerdiagnosedandsurgicallytreated atCancerReferenceUnitofRioGrandedoNorteStatefrom 2007to2014.
Methods
An observational retrospective study composed by 135 patientswasdevelopedatDoctorLuizAntonioHospital, Can-cer Reference Unit of Rio Grande do Norte State, Brazil, from2007to2014.ThestudywasapprovedbytheResearch EthicsCommittee(REC)fromLigaNorteriograndenseContra oCâncer(Protocol044/044/2009).
All patients more than 18 years old with rectal adeno-carcinomadiagnosedbyhistopathologyandradicalsurgical treatment with chemotherapy and/or radiotherapy were includedinthestudy.Patientswithothersformsofcancer wereexcludedfrom thisstudy.During theresearch,eleven patientswere excluded duethe absenceofinformationon theirrecords about neoadjuvanttreatment, adjuvant treat-mentandstaging.
Datawerecollectedfromtherecordsrevisionconsidering thefollowinformation:age,sex,origin,diagnosis,dateof diag-nosis(dateofbiopsy),TNMstage,neoadjuvanttreatment,type ofsurgicaltreatment,adjuvanttreatment,recurrence,death, dateofdeathandcauseofdeath.
All patients were submitted to surgical treatment, chemotherapyand/orradiotherapyproceededbymembersof themedicalstafffromDoctorLuizAntonioHospital.Cancer stagingwasperformedaccordingtoTNMsystemfrom Amer-icanJointCommitteeofCancers(AJCC).
Overallsurvivalwasconsideredstartingfromthedateof diagnosis,whiledisease-freesurvivalstartingfromthedate ofsurgery.Kaplan–MeierandWilcoxonnon-parametrictests were usedtoestimateand compare survivals,respectively. EvidenceresultsfromWilcoxontestwereevaluated consider-ingsignificancelevelof5%.ForstatisticalanalysisRsoftware wasused(3.2.2version).8,9
Results
From2007to2014wereconsultedrecordsfrom124patients. Themeanofagewas67.1years(±15.87),with50.3%menand 49.7%women.Consideringneoadjuvanttreatment,3.2%were submittedtochemotherapy,3.2%toradiotherapy,37.2% per-formedbothofthemand56.4%noneofthem.
Considering surgical procedures, 63.7% were submit-ted to abdominal retossigmoidectomy, 21.7% to rectal abdominoperianealamputation,6.4%tolocalresectionand 8.06%palliativeprocedures.Consideringadjuvanttreatment, 41.12%performedchemotherapy,7.25%radiotherapy,19.35%
1.00
0.75
0.50
0.25
0.00
0.0 2.5 5.0
Time (years)
Ov
er
all sur
viv
al
7.5
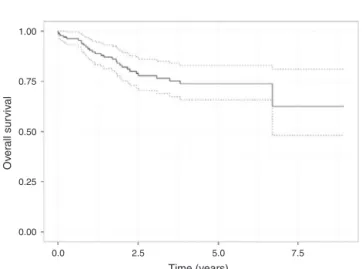
Fig.1–Overallsurvival(solidline)and95%confidence intervals(dashedline)estimatedbyKaplan–Meierforrectal cancerdata.
performed chemotherapy associated to radiotherapy and 32.25%didnotperformanyofthem.
Cancerrecurrenceoccurredin25.19%ofcases.Datafrom patientdeathrevealsthat34.67%died:74.41%duetocancer, 11.62%duetocancercomplicationsand13.95%duetoothers causes.
Overallsurvival(Fig.1)ofpatientsintreatmentagainst rec-talcancerwas62%insevenyears,whiledisease-freesurvival (Fig.2)inone,threeandfiveyearswas91.7%,75.5%and72.1%, respectively.
Concerningagegroups,weobservedanincreased disease-freesurvivalinpatientswithage below50years andfrom 70 onwardscomparedtopatientsbetween50 and70 years ofage; however,no statisticaldifference wasevidenced (p -value=0.441).Nevertheless,overallsurvivalincreasesasage rises, as demonstrated when comparing patients with age below50yearsversuspatientswithagefrom70onwards(p -value=0.008)(Fig.3).
Regarding cancer staging,from 125 patients 18.4%were classifiedasstageI,29.6%asstageII,39.2%asstageIIIand
1.00
0.75
0.50
0.25
Disease-free sur
viv
al
0.00
0.0 2.5 5.0
Time (years)
7.5
1.00
0.75
0.50
Wilcoxon test: p-value=0.026
Under 50 years vs 70 years over (p-value=0.008) 50-70 years vs 70 years over p-value=0.244)
Under 50 years 50-70 years 70 years over Under 50 years vs 50-70 years over (p-value=0.077) 0.25
Ov
er
all sur
viv
al
0.00
0.0
Age group:
2.5 5.0 7.5
Time (years)
Fig.3–OverallsurvivalestimatedbyKaplan–Meierfor rectalcancerdatacomparingagegroups.
12.8%asstageIV.Significantdifferencewasfoundbetween overall survivals related to cancer staging. However, only patientsfromstageIandIIdifferinasignificantway consid-ering disease-free survival (Fig. 4). On the other hand, for patientsclassifiedasstageIVitwasobservedashorter over-allsurvival,whichisstatisticallydifferentfromothersstages overallsurvival(Fig.5).
In contrast, data relative to sex, surgical procedures, neoadjuvanttreatment,adjuvant treatmentandrecurrence treatmentnotshowedanystatisticaldifferenceinoverall sur-vivalanddisease-freesurvival.
Discussion
Distributionbysexandmeanageofpatientsdiagnosedwith rectumcancerfoundinourstudycorrespondstothesame
1.00
0.75
0.50
0.25
0.00
0.0 2.5
Wilcoxon test: p-value<0.001 I vs II (p-value=0.043) I vs III (p-value=0.182)
I vs IV (p-value=0.102) II vs III (p-value=0.662) II vs IV (p-value<0.639) III vs IV (p-value<0.216)
5.0 7.5
Time (years)
Cancer staging
Ov
er
all sur
viv
al
I II III IV
Fig.4–Disease-freesurvivalestimatedbyKaplan–Meierfor rectalcancerdatacomparingcancerstaging.
1.00
0.75
0.50
0.25
0.00
0.0 2.5
Wilcoxon test: p-value<0.001 I vs II (p-value=0.171) I vs III (p-value=0.123)
I vs IV (p-value=0.007) II vs III (p-value=0.981) II vs IV (p-value<0.001) III vs IV (p-value<0.010)
5.0 7.5
Time (years)
Cancer staging
Ov
er
all sur
viv
al
I II III IV
Fig.5–OverallsurvivalestimatedbyKaplan–Meierfor rectalcancerdatacomparingcancerstaging.
featuresfoundintheliterature,aswellasthepredominance ofretossigmoidectomyassurgicaltreatment.
A study conducted byPinhoet al.10 revealed a discreet prevalence in male gender, with a mean age of 61 years old, and abdominal retossigmoidectomy asthe most com-monsurgicalprocedureperformedcorrespondingto45.3%of allsurgicaltreatments.Furthermore,itshowedthatfrom89 patientsinfollow-up,33presenteddiseaserelapse,similarto oursresults.
After a detailed analysis of data, it was observed that elderly was the age group most affected by rectal cancer, regardlessofgender,andabdominalretossigmoidectomythe mostcommonprocedure.Fromall patientsincludedinour study,onethirddiedduecancerorcancercomplications.
AccordingtodataanalysisfromSurveillanceEpidemiology andEndResults(SEER),survivalinfiveyearsincreasedfrom 56.5%inpatientsdiagnosedinthebeginningof1980sto63.2% inpatientsdiagnosedinthebeginningof1990sandrecentlyto 64.9%.Thissurvivalincreaseisduemainlytoearlydiagnosis and treatment.Itisknownthatpatientprognosisishighly dependentonthestaging:infiveyearstheoverallsurvivalis up than90%topatientsclassified asDukesA,but only5% whentheyareclassifiedasDukesD.Unfortunately,only10% ofpatientswiththisneoplastic diseasearediagnosedearly andmostofthempresentadvanceddisease.11,12
Overallsurvivalofpatientssubmittedtorectalcancer treat-mentwas62%insevenyears,whiledisease-freesurvivalin one,threeandfiveyearswas91.7%,75.5%and72.1%, respec-tively. Mussnich et al.13 evaluated overall and clinical and pathologicalfactorsrelatedtorectaladenocarcinomaad ver-ifiedthatoverallinfiveyearswas51%and64patients(57%) presentedrecurrence.
withinamonthafterdiagnosisandforbothtypesofcancer advancedage,cancerstageatthemomentofdiagnosisand emergencypresentationwereassociatedwithearlydeath. Dif-ferently,ourresultshadnotshowedanynegativeinfluenceof advancedageinoverallsurvivalofthesepatients.
AccordingtoPhippsetal.,15comparingwithpatientsthat remainedaliveattheendofthefollow-uporinfiveyearsafter diagnosis,patientsthatdiedwithinfiveyearsafterdiagnosis weremorelikelytobemale(58%vs.51%)andtobesmokers (64%vs.59%).Furthermore,mortalityduetodistalcolon can-cerandrectalcancerwassignificantlylowerthanmortality duetoproximalcoloncancer.Althoughthelackofevaluation ofcoloncancerinthepresentstudy,itwasfoundasignificant mortalityinrectalcancerpatientsasmentioned byPhipps etal.15However,oursdatadidnotrevealeddifferencein mor-talitybetweengenders.
Considering all surgical procedures, our study did not showed any significant difference in overall survival and disease-free survival between them. Differently, according toNational ComprehensiveCancerNetwork(NCCN),recent retrospectives comparisons between patients submitted to abdominoperianalresection and patientssubmitted tolow anteriorresectionforcancertreatmentrevealedthatformer onespresentedworstlocalcontrolandoverallsurvival.
Conclusion
Afteradetailedanalysisofdata,itwasobservedasignificant percentageofpatientsfreefromrectalcanceronceoverall sur-vivalanddisease-freesurvivalremainedenhanceduntilthe endofthestudy,suggestingthatthetreatmentprotocolsused intheinstitutionhaveshowntobeeffective.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. ParkinDM,BrayF,FerlayJ,PisaniP.Globalcancerstatistics
2002.CACancerJClin.2005;55:74–108.
2. InstitutoNacionaldeCâncerJoséAlencarGomesdaSilva.
Coordenac¸ãodePrevenc¸ãoeVigilânciaEstimativa2016:
IncidênciadeCâncernoBrasil/InstitutoNacionaldeCâncer
JoséAlencarGomesdaSilva,Coordenac¸ãodePrevenc¸ãoe
Vigilância.RiodeJaneiro:INCA;2016.
3.CarterK,KotlyarovE.PETandPET/CTimagingfortheearliest
detectionandtreatmentofcolorectalcarcinoma.BrazArch
BiolTechnol.2005;48:169–74.
4.NationalComprehensiveCancerNetwork.NCCNClinical PracticeGuidelinesinOncology:RectalCancer,V.4.2013;2013.
www.nccn.org[accessed07.09.15].
5.TeixeiraMTB,FaersteinE,LatorreMR.Técnicasdeanálise
desobrevida.CadSaúdePúblicaRiodeJaneiro.2002;18:
579–94.
6.NagtegaalID,MarijnenCA,KranenbargEK,vandeVeldeCJ,
vanKriekenJH.Circumferentialmargininvolvementisstill
animportantpredictoroflocalrecurrenceinrectal
carcinoma:notonemillimeterbuttwomillimetersisthe
limit.AmJSurgPathol.2002;26:350–7.
7.DukesCE.Thespreadofcanceroftherectum(subsectionina
paperbyGordonWatsonC&DukesCE).BrJSurg.
1930;17:643–8.
8.ShimakuraSE,CarvalhoMS,AndreozziVL,Codec¸oCT,
BarbosaMTS.Análisedesobrevida:Teoriaeaplicac¸õesem
saúde.RiodeJaneiro:EditoraFiocruz;2005.
9.RCoreTeam.Alanguageandenvironmentforstatistical computing.Viena,Áustria:RFoundationforStatistical Computing;2014[accessedat:http://www.R-project.org].
10.PinhoMSL,FerreiraLC,JuniorHK.TratamentoCirúrgicodo
CâncerColorretal:Resultadosalongoprazoeanáliseda
Qualidade.RevBrasColoproctol.2006;26:422–8.
11.RiesLAG,MelbertD,KrapchoM,StinchcombDG,HowladerN, HornerMJ,etal.,editors.SEERCancerStatisticsReview, 1975–2005.NationalCancerInstitute;2008.Availablefrom:
http://seer.cancer.gov/csr/19752005/resultsmerged/topic
survival.pdf[accessed06.08.08].
12.AHCPR(AgencyforHealthCarePolicyandResearch).
Colorectalcancerscreening.Technicalreview1.Rockville,
MD:AgencyforHealthCarePolicyandResearch;1998.AHCPR
PublicationNo.98-0033.
13.MussnichHG,MoreiraLF,GusP,PimentelM,SimonT,
SantosMB.FatoresPrognósticoseSobrevidano
AdenocarcinomaPrimáriodeReto.RevBrasColoproctol.
2008;28:62–71.
14.DowningA,AravaniA,MacleodU,OliverS,FinanPJ,Thomas
JD,etal.EarlymortalityfromcolorectalcancerinEngland:a
retrospectiveobservationalstudyofthefactorsassociated
withdeathinthefirstyearafterdiagnosis.BrJCancer.
2013;108:681–5.
15.PhippsAI,LindorNM,JenkinsMA,BaronJA,WinAK,
GallingerS,etal.Colonandrectalcancersurvivalbytumor
locationandmicrosatelliteinstability:theColonCancer