SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Update
Article
Traumatic
anterior
instability
of
the
shoulder
夽
João
Roberto
Polydoro
Rosa
∗,
Caio
Santos
Checchia,
Alberto
Naoki
Miyazaki
FaculdadedeCiênciasMédicasdaSantaCasadeSãoPaulo(FCM-SCSP),DepartamentodeOrtopediaeTraumatologia,SãoPaulo,SP, Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received27August2016 Accepted1September2016 Availableonline22September2017
Keywords:
Jointinstability Orthopedicprocedures Recurrence
Shoulderdislocation Shoulderjoint
a
b
s
t
r
a
c
t
Theshoulderisthemostunstablejointinthehumanbody.Traumaticanteriorinstability oftheshoulderisacommoncondition,which,especiallyinyoungpatients,isassociated withhighrecurrencerates.Theeffectivenessofnon-surgicaltreatmentswhencompared tosurgicalonesisstillcontroversial.Thepurposeofthisstudywastoreviewtheliterature forcurrentconceptsandupdatesregardingthetreatmentofthiscondition.
©2017PublishedbyElsevierEditoraLtda.onbehalfofSociedadeBrasileiradeOrtopedia eTraumatologia.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Instabilidade
anterior
traumática
do
ombro
Palavras-chave:
Instabilidadearticular Procedimentosortopédicos Recidiva
Luxac¸ãodoombro Articulac¸ãodoombro
r
e
s
u
m
o
Aarticulac¸ãodoombroéamaisinstáveldocorpohumano.Suainstabilidadeanteriorde causatraumáticaéumacondic¸ãocomumecomaltataxaderecidivaempacientesjovens.A eficáciadotratamentoconservadorcomparadocomotratamentocirúrgico,emsuas diver-sasabordagens,aindaédebatida.Opropósitodesteestudofoirevisaraliteratura,rever conceitoseúltimasatualizac¸õessobreotratamentodessaafecc¸ão.
©2017PublicadoporElsevierEditoraLtda.emnomedeSociedadeBrasileirade OrtopediaeTraumatologia.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND (http://creativecommons.org/licenses/by-nc-nd/4.0/).
夽
PaperdevelopedattheFaculdadedeCiênciasMédicasdaSantaCasadeSãoPaulo(FCM-SCSP),DepartamentodeOrtopediae Trau-matologia,SãoPaulo,SP,Brazil.
∗ Correspondingauthor.
E-mail:jopoly01@yahoo.com.br(J.R.Rosa). http://dx.doi.org/10.1016/j.rboe.2017.09.003
Thefirstepisodeofshoulderdislocation(primarydislocation) hasanincidenceof1.7%inthegeneralpopulation.Amongthe differenttypesofthisjointinstability,theanteriordislocation duetotraumaisthemostcommontype,corresponding to morethan90%ofthecases.1–3 Onthistopic,Hoveliusetal.
developedthreestudies ofgreatrelevance. Inthe first,257 patientswere followedforaprospective10 yearsafter pri-maryshoulderdislocation,andfounda49%recurrencerate. Thesecondstudy,whichfollowedthefirst(butthistimewith a25-yearfollow-up),hadtwoimportantresults:(1)72%ofthe patientswithless than22yearsatthetimeoftheprimary dislocationprogressedwithrecurrence,whereasthisratewas only27%inthoseolderthan30years;(2)almosthalfofthe casesofprimarydislocationoccurredbetween15and29years. Inthethirdstudy,from2008,Hoveliusetal.wereawarded aprizeforresearchonthedevelopmentofarthrosisinthe samepopulationofthesecondstudy.Ofthegroupthat pro-gressedwithinstability,29%developedmildarthrosis,9%had moderatearthrosis,and17%hadseverearthrosis.Incontrast, 18%ofthepatients,whohadonlyoneepisodeofdislocation, developedmoderatetoseverearthrosis.Detailedevaluationof thesubgroupsallowedtheidentificationofthreeriskfactors forthedevelopmentofarthrosis:under25yearsofageatthe timeoftheprimarydislocation,alcoholismandhigh-energy sports.Itisimportanttonotethatevenpatientswhohadonly oneepisode ofdislocationalsopresent risksof developing arthrosis.4–6Duetotheanatomicalpeculiaritiesandthe
con-troversiesaboutthetreatmentofprimarydislocation,besides thehighrecurrencerateinyoungpatients,wewilladdressthe mostimportantaspectsthatwillhelpusunderstandandtreat thiscondition.
Primarydislocationnon-surgicaltreatment
Inthecaseofacuteanterior primarydislocation,the most preferablyusedtreatmentisthereductionofthejointandits immobilization,followedbyavariableperiodofrehabilitation torestoretherangeofmotionandmusclestrengtharoundthe shoulder.7
Themostfrequentcomplication,areasonforsubsequent instability,istheavulsionoftheanteroinferiorportionofthe glenoidlabrum,andthe lowermarginoftheglenoid fossa, knownasBankartlesion.8,9Ifitheals,whichcanoccurinup
to50–80%ofthetime,therecurrencebecomes,intheory,less frequent.10Itisthereforedebatedwhetherthedurationand
positionoftheshoulderimmobilizationarefactorscapableof influencinglabrumhealing.
Ameta-analysisbyPatersonet al.,which includednine studies withlevelsI and IIevidence, showedno benefitin immobilizationformorethanoneweek.However,itshowed alowertendencyofrecurrencewithimmobilizationinlateral andmajorrotationifthepatient’s agewasover30years.11
In1999,Itoi etal. proposedthatthis initiallateralrotation immobilizationwould promote, byligamentotaxis,a better reductionoftheBankartlesionand,therefore,higherhealing rates.12
betweentwogroupsof20patientseach.Theresultsshoweda significantreductionintherateofrecurrenceinthose immo-bilized inlateral rotation forthreeweeks, whencompared withthoseinmedialrotation,especiallyinpatientsunder30 years.In2007,thesameauthorsconductedasimilarresearch, but this time ina largerpopulation (159patients) and the resultscorroborated thefindings ofthe firstsurvey.14 More
recently,in2010,Taskoparanetal.alsofoundfavorableresults forlateralimmobilization(inthisstudy,itwasmaintainedat tendegreesforthreeweeks,andwasremovedonlyfor per-sonalhygiene).15
Incontrast,in2009Finestoneetal.didnotfinddifferences inrecurrencerateswhenimmobilizing51patientsduringfour weeks(27oftheminlateralrotationof15to20degreesand 24inmedialrotation).Liavaagetal.publishedastudywith 188patientsin2011–95patientsimmobilizedinmedial rota-tion and 93 in 15-degreelateral rotation forthree weeks– anddidnotfinddifferencesbetweenthetwogroups.16–18The
systematicreview(whichalsoincludedtheselattertwo stud-ies)developedbyPatricketal.10didnotshowadecreasein
recurrencewithlateralrotationimmobilization.However,in a newstudy in2015, Itoi et al.19 show that the best
posi-tion for injury reduction would be in 30-degree abduction with60-degreelateralrotation,andthatabove30-degree lat-eralrotationwealreadyfindreductionoftheanteriorlesion, butnotoftheinferiorone.Itmaybefinallyarguedthatthe 10–20degreesofrotationusedintheotherstudieswere insuf-ficient forinjury reduction.Another hypothesis isthat the jointhematomawouldpreventthecoaptationofthelabrum lesiontoitsbed,andthatthejointdrainagecouldfacilitateits coaptation.10,19,20
Finally,wecanseethattheexistingpublicationstodate donotsupport, withsufficientscientificevidence,the best periodand thebest positionforimmobilization;new stud-iesarenecessarytodeterminethebestwayfornon-surgical managementofthiscondition.
Primarydislocationsurgicaltreatment
Theindicationofsurgicaltreatmentintraumaticprimary dis-locationiscontroversial.
Several authors havedemonstrated favorableresultsfor surgical stabilization afterprevious traumatic primary dis-location in young and activepatients, inorder to avoidor decreaserecurrencerates.21–27BetweenAugust2000and
Octo-ber 2008,14 shoulders were treated, of14 patients, bythe ShoulderandElbowGroupofSantaCasadeSãoPaulo. Satis-factoryresults(with100%excellentresults)wereobtainedin allcases,accordingtotheRoweevaluationcriterion.28
How-ever, this strategy unnecessarily exposessome patients to surgical risk, because notall ofthem would progresswith recurrences. On the other hand, we must remember that a recurrence can lead to anincrease in osteocartilaginous lesionsandlesionsoftheshoulderstabilizingligaments.6,23,29
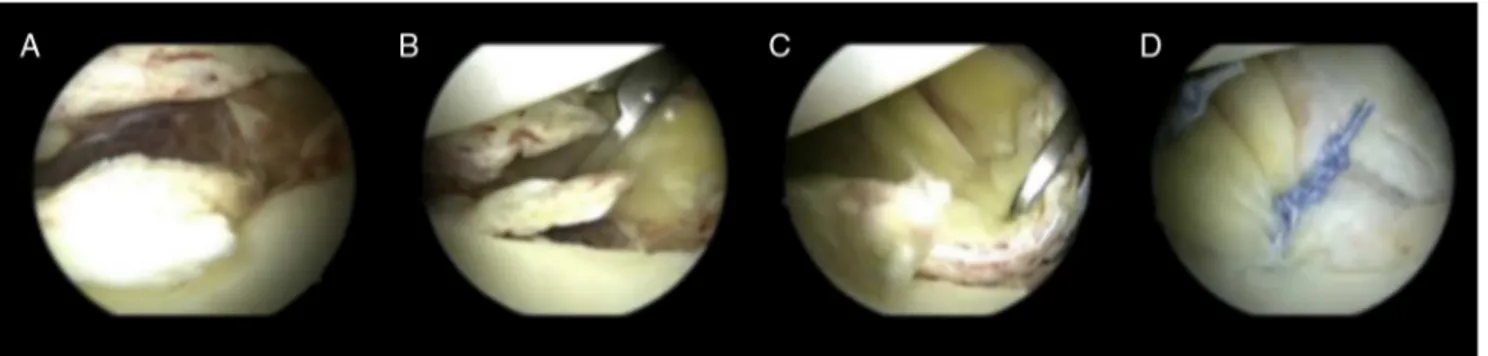
Fig.1–Leftshoulder,jointviewthroughtheposteriorportal.(A)Bankartlesion;(BandC)preparationforlesionrepair;(D) Bankartlesionarthroscopicrepair.
Table1–SystematicreviewcomparingopenrepairandarthroscopicrepairofBankartlesionsregardingthenumberof recurrences.
Authors Publicationdate Quorom Lowernumberof
recurrences
Freedmanetal.44 July2004 15 Openrepair
Mohtadietal.40 June2005 13 Openrepair
Hobbyetal.34 September2007 14 Discordant
Lentersetal.45 February2007 16 Discordant
Ngetal.41 June2007 16 Discordant
Pulavartietal.46 October2009 16 Nodifferences
Petreraetal.42 March2010 17 Nodifferences
betterinformed and want tobase their decisionson solid evidence.Weshouldalwaysconsiderthepatient’sage, domi-nance,sportmodality,andtypeofworkactivity.Climbersand surfers,forexample,areatriskofdeath(fallingordrowning) iftheydislocateashoulderduringtheiractivities.Professional athletesmayalsohavetheirsurgicalprocedureadvancedor postponedbasedontheircompetitionschedules.29,30
Habermeyer31 introducedthe SeverityShoulder
Instabil-ity Score (SSIS). It uses some risk factors as criteria for recurrence.Itsgoalistofacilitatethedecisionbetween non-surgical and surgical treatment. Among the criteria, there are:patient’s age, sports modality practiced,typeoflesion found in the glenoid cavity (Bankart lesion associated or notwithglenoidfractureand/orSLAPinjury),mechanismof trauma,presenceofotherassociatedlesions(rotatorcuffand HillSachslesions),presenceofgeneralizedligament hyper-laxity, type ofdislocation reduction (whether spontaneous orassisted), andthe degreeofpatientreliabilitytocomply witharehabilitationprotocol.Whenapplyingthisscoreina groupof80patients, Habermeyer31 obtained2.9%of
recur-renceinpatientstreatedsurgicallyand10.9%inthosetreated non-surgically.31
Openversusarthroscopicrepairofalabrumlesion
Recurrentdislocations occur between 25% and 100% ofall casessubmittedtoconservativetreatment.5,9,21,22,32,33
How-ever, surgical treatment reduces the risk of recurrence by 6–22%.21,22,33–35Althoughtheaimofsurgicaltreatmentisto
repairtheinjuredstructurestorestorethephysiological sta-bilityoftheglenohumeraljoint,thereisstilldoubtastothe bestmethodofrepair.36
Thereismuchdiscussionofthemethodsofapproach(open orarthroscopic)forthefixationoftheBankartlesion.37–43The
argumentsinfavorofopenrepairarethatitallowsthe sur-geontoperformamoreanatomicallabrum repair,and the positioning of anchors ina safer direction. Thosein favor of arthroscopy (Fig. 1), intheir turn,argue that there is a reductionofcomplicationswhencomparedtoopensurgery, suchasahigherinfectionrate,greater bleeding, subscapu-lardehiscenceandarthrofibrosis,withequivalentandfaster repair.38,40–42Chalmersetal.,36in2015,publisheda
system-aticreviewofeightmeta-analyzescomparingtheresultsof thesetwotherapeuticmethods.Init,themeta-analyzeswere scored(from0to18points)accordingtoatoolcalledQuorom (QualityofReportingofMeta-Analyzes)(thehigherthescore, thebetterthelevelofevidence).Twometa-analysespublished before2007,withaQuoromscoreof15and13,showedfewer recurrencesafterrepair.Thethreemeta-analysesconducted in2007,withscoresof14,16and16,werediscordant.Thelast three,publishedafter2008(scoresof12,16and17),didnot finddifferencesinrecurrencerateswhencomparingthetwo methods.Notethatamongthesethereisthemeta-analysis withthebestlevelofevidence(17points)36(Table1).34,40–46
Mohtadietal.40performedaprospectiveandrandomized
didnotfinddifferencesinrecurrenceratesbetweenthetwo techniquesbutobtainedshortersurgicaltimeandbetterrange ofmotionwiththearthroscopicapproach.Inthegroup sub-mitted to open repair, two of the 29 patients experienced recurrences.Intheothergroup(32arthroscopies),therewas onlyonerecurrence.37
Bankartlesionopenrepairversusopenboneblock procedure
Helfet47wastheonewhodescribedtheprocedurepopularized
byBristow,whichconsistsoftransferringthetipofthe cora-coidprocesstotheanteriorborderoftheglenoidthroughthe fibersofthesubscapularismuscle;inthismuscle,the trans-feris fixedtothe joint capsulewithout theuse ofscrews. Latarjet48 and Patte et al.49 modified the techniquein two
ways:(1)thepositioningofthecoracoidgraft,whichputin toa“lying”position(withitslargestaxisinaverticalposition; paralleltothearticularsurfaceoftheglenoid)and(2)its fixa-tionthroughtwocompressionscrews.48–50Nowadays,thisis
themostcommonlyusedtechnique.49
Although this procedure has been criticized,51,52 good
resultshavebeenfoundinseveralstudies.Stabilityisbelieved to be achieved by a triple mechanism of humeral head restraint:thatofthe“brace”,inwhich thecoracobrachialis andshortheadofthebicepstendonsandthelowerportion ofthesubscapularisrestraintheanteroinferiorjointcapsule; thatofthe boneblock procedure,in whichthe transferred choroidalprocessfunctionsasanextensionoftheglenoid cav-ity;andthatofligamentreinforcement,sincethestumpofthe coracoacromialligamentissuturedtothejointcapsule.49
Hovelius et al.,53 in 2012, described the results of 97
consecutivecasesofpatientsundergoingLatarjetprocedure comparedto88casesofopenrepairoftheBankartlesion;the latterwasperformedwithanchorsorthroughtransglenoidal orifices.Witha17-year postoperativefollow-up,recurrence occurredin14%ofthe patients(13of97cases) undergoing Latarjetprocedure,withasatisfactionindexabove95%.Onthe otherhand,ofthe88casesundergoingBankartlesionrepair, 25progressedwithrecurrence(28%), with80%satisfaction. Amongthefindingsofthisstudy,thebestscoreswereDash (Disabilitiesofthearm,shoulderandhand),Wosi(Western OntarioShoulderInstabilityIndex)andSSV(subjective shoul-dervalue)scores.Finally,theycametotwoconclusions:(1)the Latarjetprocedureleadstobettersubjectiveresultsand pro-videsgreaterstabilitytotheshoulder;(2)theliprepairthrough transglenoidalorifices wassuperiortothat performedwith anchors.53
ArthroscopicrepairofBankartlesionversusopenbone blockprocedure
Althoughbeingrathervariable,therateofrecurrenceofthe arthroscopicrepairoftheBankartlesionisstillconsideredan effectiveprocedurewithgoodreproducibility,especiallywhen thepatientiswellselected.
Thus,BalgandBoileau54developedtheInstability
Sever-ity Index Score (ISIS) in 2006as a means for determining whichpatientsshouldbenefitfromanarthroscopicanchorage
the researchers identified six risk factors that when com-binedinascoringsystemresultinunacceptablehighrates ofBankartarthroscopicrepairfailure.Patientswithascore abovesixhad70%ofrecurrence,whereasinpatientswitha scoreequaltoorlowerthansixfellto10%.54Accordingtothe
ISIS,patientswithascoreabovesixshouldundergothe Latar-jetprocedureandwithsixorlesstheBankart’sarthroscopic repair.
In2013,Rouleauetal.,55 inamulticenterstudywith114
consecutivecases,validatedISIS.TheresultsshowedthatISIS ishighly reproducible,thatis,easy toapply;quality oflife questionnairesdidnotcorrelatewithISIS,alsoshowingthat patientswithISIS greaterthan sixhadahighernumberof recurrencesbeforesurgery;andthatinthemedicalcenters whereitwasapplied,itwasanindicatorofwhichpatients would require more complex surgeries, such as Hill-Sachs lesionfilling(remplissage)oraLatarjetprocedure.55
It was observed that ISIS was used by authors, but it has been adapted. Some authors, such as Boileau, have described that somepatients with ISISgreater than three, andglenoidcavitybonedefectswerecandidatesfor Bankart-Britow-Latarjetarthroscopicsurgery.56Thomazeauetal.used
ascoreoflessthanorequaltofourtoindicatearthroscopic surgery.57
Like Boileauetal.,56 thereisacurrent trendtowardthe
indicationofboneblocks(Latarjet,Eden-HybinetteorBristow surgeries)whenthereisglenoiderosion.58,59 Defectsgreater
than20%oftheanteroposteriorjointdiameterareconsidered the limit forseveral authors.58–60 However, boththis value
and the erosion measurementtechnique are still topicsof debate.61Forsome,58–60thepracticeofcompetitivesportsisan
independentriskfactorforrecurrenceand,therefore,isalso anindependentindicatorforboneblocks.
Despiteprovidingfewerrecurrences,“boneblocks”arenot freeofcomplications. Paladinietal.62 showedalossofthe
isometriccontractionforceofthesubscapularisaftertheir L-shapedtenotomyand,therefore,theyrecommendthat the glenoidapproach(whichisnecessarilyperformedthroughthe subscapular)bemadelongitudinally(by separationoftheir fibers). Subscapular muscle deficiency explains the lossof activemedialrotationaftersurgery.
Other possible complicationsare loss oflateral rotation thatleadstoglenohumeralarthrosisandthoserelatedtograft positioning, which should be done as closeas possible to the glenoidjointsurface(less than10mmofmedialization andbelowthe“equatorline”).Ifitsfixationistoomedialor toohigh,forexample,theremaybetherapeuticfailure(with maintenanceofinstability). AcaseseriesbyHoveliusetal. showedpoorpositioningin42%oftimes(32%oftimesabove the“equatorline”and6%toomedial).53Overhanginggrafts,
intheirturn,cancausearthrosisregardlessofotherfactors.63
Bipolar
defects
to bipolar defects is not clear when the defect is in the glenoidcavityandhumeralheadsimultaneously(Hill-Sachs lesion).65
Greisetal.65demonstratedthatthegreatertheboneloss
oftheglenoidcavity,thegreaterthecontactpressureofthe humeralhead against the glenoid cavity. For example,the labral lesion reducesthe contact area by7% and 15% and increasesthecontactpressureby8%and20%.Alossof30%of theglenoidcavityincreasesthepressureintheanteroinferior regionby300%and400%,andconsiderablyincreasestherisk ofrecurrence.
BurkhartandDeBeer66 identifiedtheriskofarthroscopy
failurewhen, duringthe procedure, it isobservedthat the appearanceoftheglenoidcavityhastheshapeofan“inverted pear”.Onthehumeralside,Hill-Sachslesions,inwhich engag-ingat90degreesofabductionandlateralrotationtakesplace, areconsideredasriskylesionsonlyfortheperformanceof Bankartlesionrepair.
Yamamoto et al.,67 in 2007 demonstrated the contact
area ofthe humeralhead and the glenoid cavityfrom the pointofglenohumeraldislocation,anddefinedthiszoneof contact as glenoid track. This intact region ensures bone stability.
Theintraoperative test forengaging performed prior to thearthroscopicrepairoftheBankartlesionisoverestimated becauseligamentinsufficiencyallowsforagreater transloca-tionofthehumeralhead.68ThetestafterBankartlesionrepair,
definedbyKurokawaastrue“engaging”,leadstotheriskof damagetotherepairperformed.Kurokawaetal.69evaluated
100shoulders,in94casestherewereHill-Sachslesions,only sevencases(7.4%)weredefinedastrueengaging.Parkeetal.70
evaluated983shoulders,found70 casesoftrue “engaging” (7.1%)ofthecases.BeforeBankartlesionrepair,anincidence ofengagingbetween34%and46%ofthecasesisdescribed.
Forthisevaluation,withouttheriskofcausingoverloadto Bankart’sinjuryrepair,weusetheglenoidtrack.Through a tomographicstudyweevaluatedifthemedialmarginofthe Hill-Sachslesionisincontactwiththeglenoidtrack;then,the lesioniscalledontrack;however,iftheHill-Sachslesionis moremedialthantheglenoidtrack,itiscalledofftrack,in whichtheriskofengagingisgreater.68
Thisevaluationleadstofourcategories:thefirstincludes patientswith glenoidalcavity defects<25%, and with Hill-Sachs on track lesion; the second, patients with glenoid cavitydefects<25%andHill-Sachsoff-tracklesion,thethird ofpatientswithdefects≥25%and withHill-Sachsontrack lesion,andthefourth,patientswithdefects≥25%and Hill-Sachsoff-tracklesions.68
Therefore,basedonthereportabove,thesuggestionisto treatpatients ofthefirst categorywith arthroscopic repair oftheBankartlesion;thesecond,withcomplementationof thetreatmentwiththeremplissagetechnique;thethird,with Latarjet procedure, and the fourth with Latarjet procedure associatedornotwiththeHill-Sachslesionfilling (remplis-sage)orbonegraftofthehumeralhead68(Table2).
Hill-Sachslesiontreatment
In1940,HillandSachswerethefirsttodescribethe postero-lateralfractureofthehumeralheadbyimpactionagainstthe
Table2–Categoriesofanteriorinstabilityand recommendedtreatment.
Groups Glenoidfossa defect
Hill-Sachs lesion
Recommended treatment
1 <25% Ontrack Arthroscopicrepairof Bankartlesion 2 <25% Offtrack Arthroscopicrepairof
Bankartlesion+remplissage
3 ≥25% Ontrack Latarjetprocedure
4 ≥25% Offtrack Latarjetprocedurewithor
withouthumeralhead procedure(remplissageor graft)
glenoid,whichoccurssecondarytotheanteriordislocation oftheshoulder.71Itsincidenceintheprimarydislocationis
47–80%and,intherelapsingdislocation,ofupto93%. Sev-eral treatments havebeen used72; currently,the technique
oflesionfillingwiththeinfraspinatustendon(remplissage) has become the most popular treatment.73 In 2014, Buza
et al.74 described a systematic review with the inclusion
of167patientsundergoingtheremplissagetechnique,with a mean follow-up of 26.8 months, in which there was a small lateral rotation deficit (57.2◦ to 54.6◦), and 5.4% of
recurrences.
AretrospectiveevaluationbyBoileauetal.showedthathe usedremplissagein47of459patients(10.2%)inhisseries.The meanlateralrotationdeficitwas8degrees.Ofthe41patients whopracticedsports,37returnedtopractice(90%),with28at thesamesportslevel(includingpitchers).Therecurrencerate wasonly2%.75
Gracitelli et al. published a retrospective analysis of ten shoulders simultaneously undergoing remplissage and Bankartlesionrepair(bothbyarthroscopy).Theindicationwas forlesionswithlessthan25%impactionofthehumeralhead, and withengaging duringthearthroscopic evaluation.The resultswereimprovedRowescoresfrom22.5to80.5,andUCLA from18.0to31.1withtwocasesofrecurrence,onedislocation andonesubluxation.76
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.RomeoAA,CohenBS,CarreiraDS.Traumaticanterior shoulderinstability.OrthopClinNorthAm.
2001;32(3):399–409.
2.MaffulliN,LongoUG,GougouliasN,LoppiniM,DenaroV. Long-termhealthoutcomesofyouthsportsinjuries.BrJ SportsMed.2010;44(1):21–5.
3.GossTP.Anteriorglenohumeralinstability.Orthopedics. 1988;11(1):87–95.
SurgAm.1996;78(11):1677–84.
5. HoveliusL,OlofssonA,SandströmB,AugustiniBG,KrantzL, FredinH,etal.Nonoperativetreatmentofprimaryanterior shoulderdislocationinpatientsfortyyearsofageand younger.aprospectivetwenty-five-yearfollow-up.JBone JointSurgAm.2008;90(5):945–52.
6. HoveliusL,SaeboeM.NeerAward2008:arthropathyafter primaryanteriorshoulderdislocation–223shoulders prospectivelyfollowedupfortwenty-fiveyears.JShoulder ElbowSurg.2009;18(3):339–47.
7. JakobsenBW,JohannsenHV,SuderP,SøjbjergJO.Primary repairversusconservativetreatmentoffirst-timetraumatic anteriordislocationoftheshoulder:arandomizedstudywith 10-yearfollow-up.Arthroscopy.2007;23(2):118–23.
8. RoweCR,PatelD,SouthmaydWW.TheBankartprocedure:a long-termend-resultstudy.JBoneJointSurgAm.
1978;60(1):1–16.
9. TaylorDC,ArcieroRA.Pathologicchangesassociatedwith shoulderdislocations.Arthroscopicandphysical examinationfindingsinfirst-time,traumaticanterior dislocations.AmJSportsMed.1997;25(3):306–11.
10.VavkenP,SadoghiP,QuiddeJ,LucasR,DelaneyR,MuellerAM, etal.Immobilizationininternalorexternalrotationdoesnot changerecurrenceratesaftertraumaticanteriorshoulder dislocation.JShoulderElbowSurg.2014;23(1):13–9. 11.PatersonWH,ThrockmortonTW,KoesterM,AzarFM,Kuhn
JE.Positionanddurationofimmobilizationafterprimary anteriorshoulderdislocation:asystematicreviewand meta-analysisoftheliterature.JBoneJointSurgAm. 2010;92(18):2924–33.
12.ItoiE,HatakeyamaY,UrayamaM,PradhanRL,KidoT,SatoK. Positionofimmobilizationafterdislocationoftheshoulder.A cadavericstudy.JBoneJointSurgAm.1999;81(3):385–90. 13.ItoiE,HatakeyamaY,KidoT,SatoT,MinagawaH,
WakabayashiI,etal.Anewmethodofimmobilizationafter traumaticanteriordislocationoftheshoulder:apreliminary study.JShoulderElbowSurg.2003;12(5):413–5.
14.ItoiE,HatakeyamaY,SatoT,KidoT,ItoiE,HatakeyamaY, etal.Immobilizationinexternalrotationaftershoulder dislocationreducestheriskofrecurrence.Arandomized controlledtrial.JBoneJointSurgAm.2007;89(10):2124–31. 15.Tas¸koparanH,Kılınc¸o ˘gluV,TunayS,Bilgic¸S,Yurttas¸Y,
KömürcüM.Immobilizationoftheshoulderinexternal rotationforpreventionofrecurrenceinacuteanterior dislocation.ActaOrthopTraumatolTurc.2010;44(4):278–84. 16.FinestoneA,MilgromC,Radeva-PetrovaDR,RathE,Barchilon
V,BeythS,etal.Bracinginexternalrotationfortraumatic anteriordislocationoftheshoulder.JBoneJointSurgBr. 2009;91(7):918–21.
17.LiavaagS,BroxJI,PrippAH,EngerM,SoldalLA,Svenningsen S.Immobilizationinexternalrotationafterprimaryshoulder dislocationdidnotreducetheriskofrecurrence:a
randomizedcontrolledtrial.JBoneJointSurgAm. 2011;93(10):897–904.
18.JadadAR,MooreRA,CarrollD,JenkinsonC,ReynoldsDJ, GavaghanDJ,etal.Assessingthequalityofreportsof randomizedclinicaltrials:isblindingnecessary?ControlClin Trials.1996;17(1):1–12.
19.ItoiE,KitamuraT,HitachiS,HattaT,YamamotoN,SanoH. ArmabductionprovidesabetterreductionoftheBankart lesionduringimmobilizationinexternalrotationafteran initialshoulderdislocation.AmJSportsMed.
2015;43(7):1731–6.
20.SeyboldD,SchliemannB,HeyerCM,MuhrG,GekleC.Which labrallesioncanbebestreducedwithexternalrotationofthe shoulderafterafirst-timetraumaticanteriorshoulder dislocation?ArchOrthopTraumaSurg.2009;129(3):299–304.
Bankartrepairversusnonoperativetreatmentforacute, initialanteriorshoulderdislocations.AmJSportsMed. 1994;22(5):589–94.
22.BottoniCR,WilckensJH,DeBerardinoTM,D’AlleyrandJC, RooneyRC,HarpstriteJK,etal.Aprospective,randomized evaluationofarthroscopicstabilizationversusnonoperative treatmentinpatientswithacute,traumatic,first-time shoulderdislocations.AmJSportsMed.2002;30(4):576–80. 23.DeBerardinoTM,ArcieroRA,TaylorDC,UhorchakJM.
Prospectiveevaluationofarthroscopicstabilizationofacute, initialanteriorshoulderdislocationsinyoungathletes. Two-tofive-yearfollow-up.AmJSportsMed.2001;29(5):586–92. 24.KirkleyA,WerstineR,RatjekA,GriffinS.Prospective
randomizedclinicaltrialcomparingtheeffectivenessof immediatearthroscopicstabilizationversusimmobilization andrehabilitationinfirsttraumaticanteriordislocationsof theshoulder:long-termevaluation.Arthroscopy.
2005;21(1):55–63.
25.LawBK,YungPS,HoEP,ChangJJ,ChanKM.Thesurgical outcomeofimmediatearthroscopicBankartrepairforfirst timeanteriorshoulderdislocationinyoungactivepatients. KneeSurgSportsTraumatolArthrosc.2008;16(2):188–93. 26.OwensBD,DeBerardinoTM,NelsonBJ,ThurmanJ,Cameron
KL,TaylorDC,etal.Long-termfollow-upofacutearthroscopic Bankartrepairforinitialanteriorshoulderdislocationsin youngathletes.AmJSportsMed.2009;37(4):669–73. 27.RobinsonCM,JenkinsPJ,WhiteTO,KerA,WillE.Primary
arthroscopicstabilizationforafirst-timeanteriordislocation oftheshoulder.Arandomized,double-blindtrial.JBoneJoint SurgAm.2008;90(4):708–21.
28.MiyazakiAN,FregonezeM,SantosPD,daSilvaLA,doVal SellaG,BotelhoV,etal.Assessmentoftheresultsfrom arthroscopicsurgicaltreatmentfortraumaticanterior shoulderdislocation:firstepisode.RevBrasOrtop. 2015;47(2):222–7.
29.BishopJA,CrallTS,KocherMS.Operativeversusnonoperative treatmentafterprimarytraumaticanteriorglenohumeral dislocation:expected-valuedecisionanalysis.JShoulder ElbowSurg.2011;20(7):1087–94.
30.BrophyRH,MarxRG.Thetreatmentoftraumaticanterior instabilityoftheshoulder:nonoperativeandsurgical treatment.Arthroscopy.2009;25(3):298–304.
31.HabermeyerP.Theseverityshoulderinstabilityscore(SSIS):a guidefortherapyoptionforfirsttraumaticshoulder
dislocation.Edinburgh:11◦
CongressoMundialICSES;2010. Dissertac¸ão.
32.MaransHJ,AngelKR,SchemitschEH,WedgeJH.Thefateof traumaticanteriordislocationoftheshoulderinchildren.J BoneJointSurgAm.1992;74(8):1242–4.
33.RobinsonCM,HowesJ,MurdochH,WillE,GrahamC. Functionaloutcomeandriskofrecurrentinstabilityafter primarytraumaticanteriorshoulderdislocationinyoung patients.JBoneJointSurgAm.2006;88(11):2326–36. 34.HobbyJ,GriffinD,DunbarM,BoileauP.Isarthroscopic
surgeryforstabilisationofchronicshoulderinstabilityas effectiveasopensurgery?Asystematicreviewand meta-analysisof62studiesincluding3044arthroscopic operations.JBoneJointSurgBr.2007;89(9):1188–96. 35.MagnussonL,EjerhedL,Rostgård-ChristensenL,SernertN,
ErikssonR,KarlssonJ,etal.Aprospective,randomized, clinicalandradiographicstudyafterarthroscopicBankart reconstructionusing2differenttypesofabsorbabletacks. Arthroscopy.2006;22(2):143–51.
36.ChalmersPN,MascarenhasR,LerouxT,SayeghET,VermaNN, ColeBJ,etal.Doarthroscopicandopenstabilization
reviewofoverlappingmeta-analyses.Arthroscopy. 2015;31(2):355–63.
37.BottoniCR,SmithEL,BerkowitzMJ,TowleRB,MooreJH. Arthroscopicversusopenshoulderstabilizationforrecurrent anteriorinstability:aprospectiverandomizedclinicaltrial. AmJSportsMed.2006;34(11):1730–7.
38.HarrisJD,GuptaAK,MallNA,AbramsGD,McCormickFM, ColeBJ,etal.Long-termoutcomesafterBankartshoulder stabilization.Arthroscopy.2013;29(5):920–33.
39.KimSH,HaKI,KimSH.Bankartrepairintraumaticanterior shoulderinstability:openversusarthroscopictechnique. Arthroscopy.2002;18(7):755–63.
40.MohtadiNG,BitarIJ,SasyniukTM,HollinsheadRM,Harper WP.Arthroscopicversusopenrepairfortraumaticanterior shoulderinstability:ameta-analysis.Arthroscopy. 2005;21(6):652–8.
41.NgC,BialocerkowskiA,HinmanR.Effectivenessof arthroscopicversusopensurgicalstabilisationforthe managementoftraumaticanteriorglenohumeralinstability. IntJEvidBasedHealthc.2007;5(2):182–207.
42.PetreraM,PatellaV,PatellaS,TheodoropoulosJ.A meta-analysisofopenversusarthroscopicBankartrepair usingsutureanchors.KneeSurgSportsTraumatolArthrosc. 2010;18(12):1742–7.
43.WangC,GhalamborN,ZarinsB,WarnerJJ.Arthroscopic versusopenBankartrepair:analysisofpatientsubjective outcomeandcost.Arthroscopy.2005;21(10):1219–22. 44.FreedmanKB,SmithAP,RomeoAA,ColeBJ,BachBR.Open
Bankartrepairversusarthroscopicrepairwithtransglenoid suturesorbioabsorbabletacksforrecurrentanterior instabilityoftheshoulder:ameta-analysis.AmJSportsMed. 2004;32(6):1520–7.
45.LentersTR,FrantaAK,WolfFM,LeopoldSS,MatsenFAIII. Arthroscopiccomparedwithopenrepairsforrecurrent anteriorshoulderinstability.JBoneJointSurgAm. 2007;89(2):244–54.
46.PulavartiRS,SymesTH,RanganA.Surgicalinterventionsfor anteriorshoulderinstabilityinadults.CochraneDatabase SystRev.2009;7(4),
http://dx.doi.org/10.1002/14651858.CD005077.pub2.CD005077. 47.HelfetAJ.Coracoidtransplantationforrecurringdislocation
oftheshoulder.JBoneJointSurgBr.1958;40-B(2): 198–202.
48.LatarjetM.Treatmentofrecurrentdislocationofthe shoulder.LyonChir.1954;49(8):994–7.
49.PatteD,BernageauJ,RodineauJ,GardesJC.Unstablepainful shoulders(author’stransl).RevChirOrthopReparatrice ApparMot.1980;66(3):157–65.
50.WalchG.Chronicanteriorglenohumeralinstability.JBone JointSurgBr.1996;78(4):670–7.
51.YoungDC,RockwoodCAJr.ComplicationsofafailedBristow procedureandtheirmanagement.JBoneJointSurgAm. 1991;73(7):969–81.
52.BoileauP,MercierN,OldJ.Arthroscopic
Bankart-Bristow-Latarjet.(2B3)Procedure:howtodoitand trickstomakeiteasierandsafe.OrthopClinNorthAm. 2010;41(3):381–92.
53.HoveliusL,SandströmB,OlofssonA,SvenssonO,RahmeH. Theeffectofcapsularrepair,boneblockhealing,andposition ontheresultsoftheBristow-Latarjetprocedure(studyIII): long-termfollow-upin319shoulders.JShoulderElbowSurg. 2012;21(5):647–60.
54.BalgF,BoileauP.Theinstabilityseverityindexscore.Asimple pre-operativescoretoselectpatientsforarthroscopicoropen shoulderstabilisation.JBoneJointSurgBr.2007;89(11): 1470–7.
55.RouleauDM,Hébert-DaviesJ,DjahangiriA,GodboutV,Pelet S,BalgF.Validationoftheinstabilityshoulderindexscoreina
multicenterreliabilitystudyin114consecutivecases.AmJ SportsMed.2013;41(2):278–82.
56.BoileauP,MercierN,RoussanneY,ThéluCÉ,OldJ. ArthroscopicBankart-Bristow-Latarjetprocedure:the developmentandearlyresultsofasafeandreproducible technique.Arthroscopy.2010;26(11):1434–50.
57.ThomazeauH,CourageO,BarthJ,PélégriC,CharoussetC, LespagnolF,etal.FrenchArthroscopySociety.Canwe improvetheindicationforBankartarthroscopicrepair?A preliminaryclinicalstudyusingtheISISscore.Orthop TraumatolSurgRes.2010;968Suppl:S77–83.
58.YamamotoN,ItoiE,AbeH,KikuchiK,SekiN,MinagawaH, etal.Effectofananteriorglenoiddefectonanteriorshoulder stability:acadavericstudy.AmJSportsMed.
2009;37(5):949–54.
59.SouthgateDF,BokorDJ,LongoUG,WallaceAL,BullAM.The effectofhumeralavulsionoftheglenohumeralligaments andhumeralrepairsiteonjointlaxity:abiomechanical study.Arthroscopy.2013;29(6):990–7.
60.BessiereC,TrojaniC,PélégriC,CarlesM,BoileauP.Coracoid boneblockversusarthroscopicBankartrepair:acomparative pairedstudywith5-yearfollow-up.OrthopTraumatolSurg Res.2013;99(2):123–30.
61.LongoUG,LoppiniM,RizzelloG,CiuffredaM,MaffulliN, DenaroV.Latarjet,BristowandEden-Hybinetteprocedures foranteriorshoulderdislocation:systematicreviewand quantitativesynthesisoftheliterature.Arthroscopy. 2014;30(9):1184–211.
62.PaladiniP,MerollaG,DeSantisE,CampiF,PorcelliniG. Long-termsubscapularisstrengthassessmentafter
Bristow-Latarjetprocedure:isometricstudy.JShoulderElbow Surg.2012;21(1):42–7.
63.TorgJS,BalduiniFC,BonciC,LehmanRC,GreggJR,Esterhai JL,etal.AmodifiedBristow-Helfet-Mayprocedurefor recurrentdislocationandsubluxationoftheshoulder.Report oftwohundredandtwelvecases.JBoneJointSurgAm. 1987;69(6):904–13.
64.GerberC,NyffelerRW.Classificationofglenohumeraljoint instability.ClinOrthopRelatRes.2002;(400):65–76. 65.GreisPE,ScuderiMG,MohrA,BachusKN,BurksRT.
Glenohumeralarticularcontactareasandpressuresfollowing labralandosseousinjurytotheanteroinferiorquadrantof theglenoid.JShoulderElbowSurg.2002;11(5):442–51. 66.BurkhartSS,DeBeerJF.Traumaticglenohumeralbonedefects
andtheirrelationshiptofailureofarthroscopicBankart repairs:significanceoftheinverted-pearglenoidandthe humeralengagingHill-Sachslesion.Arthroscopy. 2000;16(7):677–94.
67.YamamotoN,ItoiE,AbeH,MinagawaH,SekiN,ShimadaY, etal.Contactbetweentheglenoidandthehumeralheadin abduction,externalrotation,andhorizontalextension:anew conceptofglenoidtrack.JShoulderElbowSurg.
2007;16(5):649–56.
68.DiGiacomoG,ItoiE,BurkhartSS.Evolvingconceptofbipolar bonelossandtheHill-Sachslesion:from
engaging/non-engaginglesiontoon-track/off-tracklesion. Arthroscopy.2014;30(1):90–8.
69.KurokawaD,YamamotoN,NagamotoH,OmoriY,TanakaM, SanoH,etal.TheprevalenceofalargeHill-Sachslesionthat needstobetreated.JShoulderElbowSurg.2013;22(9):1285–9. 70.ParkeCS,YooJH,ChoNS,RheeYG.Arthroscopicremplissage
forhumeraldefectinanteriorshoulderinstability:isit needed?39thannualmeetingofJapanShoulderSociety, Tokyo,October5–6.2012.
71.HillHA,SachsMD.Thegrooveddefectofthehumeralhead. Radiology.1940;35:690–700.
2012;20(4):242–52.
73.BiglianiLU,FlatowEL,PollockRG.Fracturesoftheproximal humerus.In:RockwoodCA,GreenDP,BucholzRW,editors. Fracturesinadults.4thed.Philadelphia:Lippincott-Raven; 1996.p.1055–107.
74.BuzaJA3rd,IyengarJJ,AnakwenzeOA,AhmadCS,Levine WN.ArthroscopicHill-Sachsremplissage:asystematic review.JBoneJointSurgAm.2014;96(7):549–55.
factorsforrecurrenceofshoulderinstabilityafter arthroscopicBankartrepair.JBoneJointSurgAm. 2006;88(8):1755–63.