w w w . r b h h . o r g
Revista
Brasileira
de
Hematologia
e
Hemoterapia
Brazilian
Journal
of
Hematology
and
Hemotherapy
Original
article
Patient
posture
for
blood
collection
by
venipuncture:
recall
for
standardization
after
28
years
Gabriel
Lima-Oliveira
∗,
Gian
Cesare
Guidi,
Gian
Luca
Salvagno,
Elisa
Danese,
Martina
Montagnana,
Giuseppe
Lippi
UniversityofVerona,Verona,Italy
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received29October2016 Accepted23January2017 Availableonline22February2017
Keywords:
Pre-analyticalvariability Posture
Plasmavolumechange Hematology
Completebloodcellcount
a
b
s
t
r
a
c
t
Background:Althoughdataabouttheeffectofpostureonroutinehematologicaltestingwere published28yearsago,thispre-analyticalissuehasnotbeenstandardizedsofar.Thisstudy wasplannedtoevaluatewhetherpostural changesinfluencetheresultsofhematology testing.
Methods:Acompletebloodcountwasperformedin19healthyvolunteersafter25mininthe supineposition,20mininasittingpositionand20minstationarystandinginanupright position.
Results:Thechangefromsupinetosittingpositioncausedclinicallysignificantincreases inthehemoglobin,hematocritandredblood cellcount.Furthermore,thechangefrom supinetostandingcausedclinicallysignificantincreasesinthehemoglobin,hematocrit, redbloodcell,leukocyte,neutrophil,lymphocyte,basophilandplateletcounts,andmean plateletvolume,andthatfromsittingtostandingcausedclinicallysignificantincreasesin hemoglobin,hematocrit,andredbloodcell,leukocyte,neutrophilandlymphocytecounts.
Conclusion: Theresultsofthisinvestigationprovidefurthersupporttothenotionthateffort should bemade toachieve widespreadstandardization inthe practiceof phlebotomy, includingpatientposture.
©2017Associac¸ ˜aoBrasileiradeHematologia,HemoterapiaeTerapiaCelular.Published byElsevierEditoraLtda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
The complete blood count (CBC) is one of the tests most frequentlyrequestedinthe clinicalpractice,becauseitisa
∗ Correspondingauthorat:SectionofClinicalBiochemistry,DepartmentofNeurosciences,BiomedicineandMovementSciences,
Univer-sityofVerona,Verona,Italy.
E-mailaddress:dr.g.lima.oliveira@gmail.com(G.Lima-Oliveira).
multi-taskinganalysisthatprovidesvaluableinformationon abroadrangeofclinicalconditions(i.e.,anemia,hemostasis, inflammation,malignancies).1ThesamplesforCBCarehence routinelyrequestedinvirtuallyallhealthcareenvironments, includingemergencydepartments,andclinicalandsurgical
http://dx.doi.org/10.1016/j.bjhh.2017.01.004
128
revbrashematolhemoter.2 0 1 7;39(2):127–132wards.2Moreover,bothhematocritandhemoglobinareuseful forscreeningblooddonors.
In general, drawing of ethylenediaminetetraacetic acid (EDTA)-anticoagulatedspecimensbyvenipuncture(i.e.,those usedforCBCtesting)canbeperformedwithpatientsin dif-ferentposturesincludinglyinginbed,afterwalkingthrough ambulatoryservicesandsittingjustbeforethetest(i.e.,less than3min) orsitting foralong time(i.e.,afterperforming intravenousinfusiontherapyindaycarefacilities).
TheClinicalandLaboratoryStandardsInstitute(CLSI) H03-A6 document, renamed the GP 41-A6 standard, currently recommendsthatbloodspecimensshouldbecollectedwith the patient comfortably seated in an appropriate chair or lyingdown,butdoesnotprovidespecificationsaboutsupine orstanding positionsandtime ofpermanenceinacertain position.3 Since the posture may influence the concentra-tionofseveralblood constituentsduetodecreased plasma volumeoccurringonchangingfrom lyingtostanding,4 itis conventionallyassumedthatremainingsupineforalongtime maybeassociatedwithconsistenthemodilution.Ontheother hand,thestandingposturemaybeacauseofblood concen-trationduetotheeffectofgravitationalforceandhydrostatic pressure, which cause ultrafiltration of plasma and small moleculesintheinterstitialspace.5
Itisacommonexperiencethatcliniciansnotonlycomplain aboutunexpectedvariationsinhemoglobinlevels,especially whentheseapproximatethetransfusionthreshold,6butalso frequentlyappraisevirtuallyunexplainablechangesin addi-tionalparametersoftheCBC,suchasplateletsortheleukocyte countanddifferential.Itisnowclearlyacknowledgedthatthe vastmajorityoflaboratoryerrorsoccurinthepre-analytical phaseand are primarilyattributabletoalackof standard-izedprotocolsduringvenousbloodsampling.7,8Theinfluence ofpostureontheCBCwasinvestigatednearly30yearsago byLeppanenandGrasbeck,9whomanuallymeasuredwhite blood cell (WBC) differential counts in 22 healthy women after2hfasting.9 Theseauthors recommendedthatvenous bloodsamplingshouldbestandardizedtoareferenceposition, eithersitting or supine.However,this experimentaldesign –entailing2hoffasting10andmanualanalysis11–isbarely reproducibleaccordingtothecurrentpracticeandtechnology. Therefore,thisstudywasplannedtoevaluatewhether postu-ralchangesinfluencetheresultsoftheCBC,withspecialfocus onplatelets,leukocytecountanddifferential.
Methods
Thestudypopulationconsistedof19healthysubjects(mean age44±11years;sevenmaleand12female)recruitedfrom thelaboratorystaffoftheUniversityHospitalofVerona(Italy). Venousbloodwascollectedafterovernightfasting(12h)bythe standardtechniqueandwithoutvenous stasis.12,13 Inbrief, three5.9mgofK2EDTAbloodtubes(Venosafe,TerumoEurope N.V.,Leuven,Belgium)werecollectedfromeachvolunteeron thesameday. Thefirsttube wasdrawnafter25mininthe supineposition,thesecondafter20mininthesittingposition andthelastafter20mininthestandingposition.Blood col-lectionswereseriallyperformedintheorderlistedabove,and theintervalswereonlythosespentineachposture.TheCBC
wasperformedwiththeAdvia2120hematologicalanalyzer (Siemens Healthcare Diagnostics, Deerfield, IL). The delta plasmavolumechange(PVC) wascalculatedwiththe ref-erenceformulaofDillandCostillasfollows:PV(%)=100× ((Hemoglobinpre/Hemoglobinpost)×(100−Hematocritpost)/ (100−Hematocritpre)−1), using hematocrit values as per-centages and hemoglobin values in g/dL.14 Results are expressed as medians and interquartile range (IQR). The significance of differences was evaluated with Wilcoxon’s signedranktest,usingAnalyse-it(Analyse-itSoftwareLtd., Leeds, UK). The percentage variation calculated from the different postural positions was also compared with the desirablequalityspecificationsforbiasderivedfrom biologi-calvariations15asprovidedbyRicosetal.Briefly,thisisbest achieved for measurands under strict homeostatic control in order topreserve their concentrations inthe body fluid ofinterest,but it canalsobeappliedtoother measurands thatareinasteadystateinbiologicalfluids.Inthiscase,it is expectedthat the ‘noise’produced bythe measurement procedure willnotsignificantlyalterthesignalprovidedby theconcentrationofthemeasurand.16Eachpatientprovided writtenconsentbeforebeingenrolledinthestudy,whichwas performedinaccordwiththeethicalstandardsestablished bytheinstitutioninwhichtheexperimentswereperformed andtheHelsinkiDeclarationof1975.
Results
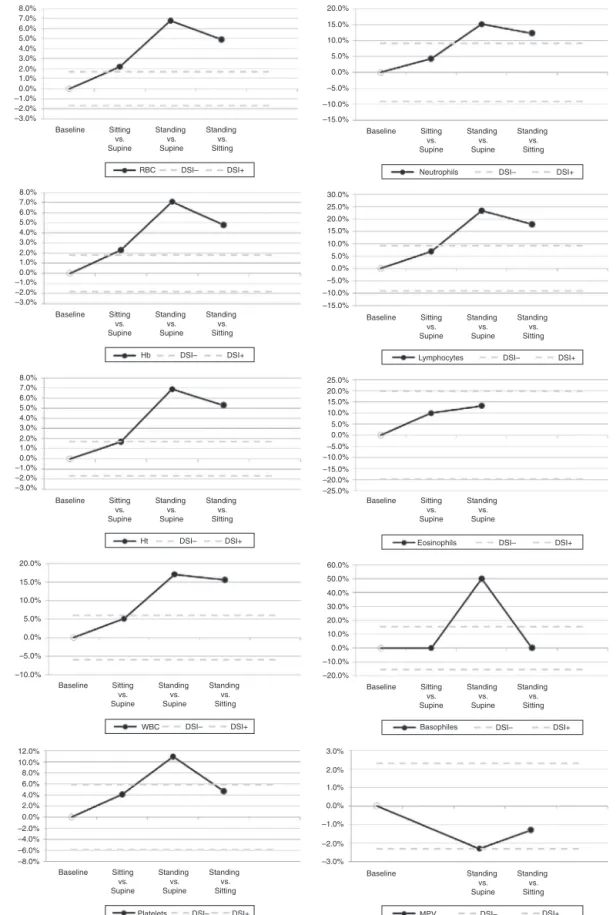
TheresultsofthisstudyareshowninTable1andFigure1. According tothe formulaofDill andCostill,thePVCwas −3.4%fromsupinetositting,−14.1%fromsupineto stand-ingand−9.3%fromsittingtostanding.Statisticallysignificant variationsfromsupinetosittingwerefoundfortheredblood cell(RBC),WBC,neutrophil,lymphocyte,eosinophil,basophil andplateletcounts,hemoglobinandhematocrit.Whenthese variations were compared to the quality specifications for bias derived from biological variations, meaningful differ-enceswereonlyobservedfortheRBCcount,hemoglobinand hematocrit.Statisticallysignificantvariationsfromsupineto standingwererecordedfortheRBC,WBC,neutrophil, lympho-cyte, eosinophil, basophil, andplatelet counts,hemoglobin andhematocritandmeancorpuscularvolume(MPV).When thesevariationswerecomparedagainstthequality specifica-tions,meaningfuldifferenceswerefoundfortheRBCcount, hemoglobin, hematocrit,andWBC,neutrophil, lymphocyte, basophil,andplateletcountsandMPV.Furthermore, statisti-cally significantvariationsfromsittingtostandingposition were observed forthe RBC count, hemoglobin, hematocrit, WBC,neutrophil,lymphocyte,basophil, andplateletcounts andMPV.Whenthesevariationswerecomparedtothequality specifications,meaningfulbiaswasfoundfortheRBC,WBC, neutrophilandlymphocytecounts,hemoglobinand hemat-ocrit.
Discussion
rev
bras
hema
tol
hemoter.
2
0
1
7;
3
9(2)
:127–132
129
bias
Value p-Value vs.supine
Bias(%) vs.supine
Value p-Value vs.supine
Bias(%)vs. supine
p-Value vs.sitting
Bias(%)vs. sitting
PVC(%variation) – – −3.4(−1.5to−4.3) <0.001 – −14.1(−9.1to−15.7) <0.001 −9.3(−11.1to−6.6) <0.001 –
RBCcount(×1012/L) ±1.7% 4.7(4.4–5.2) 4.8(4.5–5.3) <0.001 2.2(1.8–2.8) 5.0(4.7–5.4) <0.001 6.8(5.1–9.0) <0.001 4.9(2.8–5.9)
Hemoglobin(g/L) ±1.8% 131(127–145) 134(129–150) <0.001 2.3(1.9–2.9) 141(134–154) <0.001 7.1(5.3–8.9) <0.001 4.8(3.9–6.0)
Hematocrit(%) ±1.7% 0.41(0.40–0.44) 0.42(0.41–0.44) 0.009 1.7(1.3–2.5) 0.44(0.43–0.47) <0.001 6.9(5.0–8.9) <0.001 5.3(3.3–6.3)
MCV(fL) ±1.3% 89(87–92) 90(87–92) 0.057 – 90(87–92) 0.420 – 0.670 –
MCH(pg) ±1.3% 29.2(27.7–30.0) 29.5(28.0–30.3) 0.145 – 29.2(28.1–30.2) 0.147 – 0.170 –
RDW(%) ±1.7% 13.4(12.9–13.9) 13.4(12.9–13.8) 0.424 – 13.4(12.9–14.1) 0.176 – 0.178 –
WBCcount(×109/L) ±6.0% 5.4(4.6–6.7) 5.7(4.9–6.1) <0.001 5.1(3.2–8.1) 6.2(5.3–6.7) <0.001 17.1(14.2–24.2) <0.001 15.6(8.2–18.8)
Neutrophils(×109/L) ±9.2% 3.2(2.4–3.5) 3.3(2.5–3.7) <0.001 4.3(2.9–8.0) 3.7(3.0–4.1) <0.001 15.2(12.6–25.9) <0.001 12.3(7.7–16.8)
Lymphocytes(×109/L) ±9.2% 1.7(1.2–2.0) 1.8(1.2–2.1) <0.001 6.9(4.5–7.8) 1.9(1.5–2.5) <0.001 23.4(14.1–34.9) <0.001 17.9(9.3–23.9)
Monocytes(×109/L) ±13.2% 0.28(0.23–0.32) 0.28(0.22–0.32) 0.325 – 0.28(0.24–0.32) 0.117 – 0.054 –
Eosinophils(×109/L) ±19.8% 0.07(0.06–0.11) 0.08(0.06–0.13) 0.008 10.0(0.0–17.1) 0.09(0.06–0.13) 0.009 13.3(0.0–34.3) 0.284 –
Basophils(×109/L) ±15.4% 0.02(0.01–0.03) 0.02(0.02–0.03) 0.008 0.0(0.0–50.0) 0.03(0.02–0.04) <0.001 50.0(12.5–66.7) 0.012 0.0(0.0–50.0)
LUC(×109/L) Not
available
0.13(0.12–0.14) 0.13(0.10–0.14) 0.145 – 0.13(0.11–0.16) 0.259 – 0.054 –
Platelets(×109/L) ±5.9% 194(181–233) 200(190–243) <0.001 4.1(2.1–6.3) 210(198–248) <0.001 10.9(4.6–14.8) 0.002 4.7(0.0–8.8)
MPV(fL) ±2.3% 8.9(8.5–9.3) 8.9(8.3–9.3) 0.122 – 8.8(8.1–9.1) 0.018 −2.3(−4.5to−0.5) 0.041 −1.3(−3.3to0.5)
Resultsareexpressedasmediansandinterquartilerange,significantdifferencesareinbold.
130
revbrashematolhemoter.2 0 1 7;39(2):127–132 8.0% 20.0% 15.0% 10.0% 5.0% 0.0% –5.0% –10.0% –15.0% 30.0% 25.0% 20.0% 15.0% 10.0% 5.0% –10.0% 0.0% –5.0% –15.0% 25.0% 20.0% 15.0% 10.0% 5.0% 0.0% –15.0% –5.0% –10.0% –20.0% –25.0% 7.0% 6.0% 5.0% 4.0% 3.0% 2.0% 1.0% 0.0% –1.0% –2.0% –3.0% 8.0% 7.0% 6.0% 5.0% 4.0% 3.0% 2.0% 1.0% 0.0% –1.0% –2.0% –3.0% 8.0% 7.0% 6.0% 5.0% 4.0% 3.0% 2.0% 1.0% 0.0% –1.0% –2.0% –3.0% 20.0% 12.0% 3.0% 2.0% 1.0% 0.0% –1.0% –2.0% –3.0% 10.0% 8.0% 6.0% 4.0% 2.0% 0.0% –2.0% –4.0% –6.0% –8.0% 60.0% 50.0% 40.0% 30.0% 20.0% 10.0% 0.0% –10.0% –20.0% 15.0% 10.0% 5.0% 0.0% –5.0% –10.0%Baseline Sitting Baseline
vs. Supine Sitting vs. Supine Standing vs. Supine Standing vs. Supine Baseline Sitting vs. Supine Standing vs. Supine RBC Hb Ht WBC Platelets Neutrophils Lymphocytes Eosinophils Basophiles MPV DSI– DSI– DSI– DSI– DSI– DSI– DSI– DSI– DSI+ DSI+ DSI+ DSI– DSI– DSI+ DSI+ DSI+ DSI+ DSI+ DSI+ DSI+ Standing vs. Sitting Baseline Sitting vs. Supine Standing vs. Supine Standing vs. Sitting Baseline Sitting vs. Supine Standing vs. Supine Standing vs. Sitting Baseline Sitting vs. Supine Standing vs. Supine Standing vs. Sitting Baseline Sitting vs. Supine Standing vs. Supine Standing vs. Sitting Standing vs. Sitting Baseline Sitting vs. Supine Standing vs. Supine Standing vs. Sitting Baseline Sitting vs. Supine Standing vs. Supine Standing vs. Sitting Baseline Standing vs. Supine Standing vs. Sitting
Figure1–Interferogramsrelatedtopatientpostureduringbloodcollectionbyvenipuncture.Patientposture(x-axis)is
plottedagainstbiasvalues(y-axis).Solidline–bias.Dashedlines–acceptablecriteriabasedondesirablespecificationfor
MPVthat were significantlybiasedwhen patients changed positionfromstandingtothesupineposition(Table1).MPV is an important parameter in the differential diagnosis of patientswiththrombocytopenia,17 andforrisk assessment ofcardiovasculardisorders.18Aclinicallysignificantbiaswas alsoobservedforleukocytes.Interestingly,increasesinthe WBC,neutrophil, lymphocyte,andbasophilcountswereon average2-to5-foldlargerthanexpectedaccordingtothe cal-culatedPVC(Table1).Thisevidencesuggeststhatanactive releaseofleukocytesmayoccurfromdynamicreservoirs,such asthespleen,whenthepatientchangesfromthesupine posi-tiontostanding.19
TheCBChas asubstantial diagnostic valueinthe daily clinicalpractice.Whencarefullyinterpretedaccordingtothe clinical history of signs and symptoms, this analysis pro-videsusefulinformationinthediagnosisandmanagementof patientswithanumberofhematologicaldisorders.TheCBC isalsohelpfulforlongitudinalmonitoringofRBCs,platelets andleukocytesinresponsetodrugand/orsurgicaltreatment. However,aftertheintroductionofautomatedbloodcount ana-lyzers, a complete panel of blood cell indices can now be generatedwith amuchhigher degree ofanalytical quality andaccuracy,20andthusmucheffortisrequiredto standard-izeextra-analyticalissues(i.e.,patientpostureduringblood collectionbyvenipuncture).21–23
The influence of patient posture on blood components hasbeeninvestigatedpreviouslywithspecialfocusonlarger moleculessuch asalbumin, serum enzymes,bilirubin and lipoproteins.4,6,24–28 Mayer et al. first studiedthe influence ofpostureon hematocritand demonstrated that achange ofposition fromrecumbenttositting wassufficientto sig-nificantlyincreasethehematocrit,withstandingproducing anevengreaterincrease.24Mawetal.alsoinvestigatedthe underlyingmechanisms of this modification by measuring body fluid rearrangement during postural variations, and concludedthatintravascularfluidlossduringstandingwas mainlyduetofiltrationofplasmaintotheinterstitium.29More recently,Inagakietal.demonstratedthattheredistributionof waterbetweenthe intra-and extra-vascularspaces follow-ingposturalchangesduringhemodialysiswasanimportant sourceofchangesinblood components,thusunderpinning theimportanceofposturaleffectsforevaluatingblood param-etersduringhemodialysis.30
Thefindings ofthis study have somepotentially useful clinicalimplications.First,theevidencethatseveral param-etersoftheCBCaresignificantlyaffectedbydifferentpostural positionsraisesthecrucialissuethatpatientpostureshould beaccuratelystandardizedduringblooddrawing,especially whendefiningreferencerangesformanylaboratorytestsand assessing longitudinalvariations of the same subject over time.Asecondimportantaspectisthatphysiciansshouldnot discountthefactthatvirtuallyinexplicablevariationsofRBC, plateletsandleukocytesmaybecausedbythecollectionof venousbloodindifferentposturesratherthanbydisease(e.g., acutebleeding,plateletconsumptionasinthecaseof dissem-inatedintravascularcoagulation),oranalyticalerrors.Thisis particularlycrucialforparameterssuchastheWBCand lym-phocytecounts,whichincreasedbyapproximately20%from supinetostandingposition(Table1andFigure1).Finally,we alsoraisetheissuethatguidelinesforvenipuncturesuchas
thoseoftheCLSI3shouldincludeaclearindicationthat stan-dardizingpatientpostureisnecessarytoproducesoliddata andenablereliablecomparisonsovertime.
Conclusions
Inconclusion,theresultsofthisinvestigationprovidefurther supporttothenotionthateffortshouldbemadetoachieve awidespreadstandardizationofthepracticeofphlebotomy. Clearindicationsshouldbegiventhatpatientpostureduring venousbloodsamplingmustbestandardizedtoareference position,eithersittingorsupine.Irrespectiveofthechosen criterion,arecommendationshouldbegiventhataminimum period (i.e., 15 or 20min) ofresting in the reference posi-tion should beobservedbefore collectingvenousblood for CBC.
Authorship
GLO, GLS, GCG and GL conceivedand designed the study, analyzed the data, performed the statistical analysis and draftedthemanuscript;EDandMMreviewedtheliterature, acquired data, interpretedthe resultsand criticallyrevised themanuscript.Alltheauthorsreadandapprovedthefinal versionofthemanuscript.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.LippiG,SalvagnoGL,SoleroGP,FranchiniM,GuidiGC. Stabilityofbloodcellcounts,hematologicparametersand reticulocytesindexesontheAdviaA120hematologic analyzer.JLabClinMed.2005;146(6):333–40.
2.DavesM,ZaglerEM,CeminR,GnechF,JoosA,PlatzgummerS, etal.Samplestabilityforcompletebloodcellcountusingthe SysmexXNhaematologicalanalyser.BloodTransfus. 2015;13(4):576–82.
3.ClinicalLaboratoryStandardsInstitute.Proceduresforthe collectionofdiagnosticbloodspecimensbyvenipuncture. CLSIH3-A6document.6thed.Wayne,PA:ClinicalLaboratory StandardsInstitute;2007.
4.ThompsonWO,ThompsonPK,DaileyME.Theeffectof postureuponthecompositionandvolumeofthebloodin man.JClinInvestig.1928;5(4):573–604.
5.FawcettJK,WynnV.Effectsofpostureonplasmavolumeand somebloodconstituents.JClinPathol.1960;13:304–10. 6.DixonM,PatersonCR.Postureandthecompositionof
plasma.ClinChem.1978;24(5):824–6.
7.Lima-OliveiraG,LippiG,SalvagnoGL,PichethG,GuidiGC. Laboratorydiagnosticsandqualityofbloodcollection.JMed Biochem.2015;34(3):288–94.
132
revbrashematolhemoter.2 0 1 7;39(2):127–1329. LeppanenEA,GrasbeckR.Experimentalbasisofstandardized specimencollection:effectofpostureonbloodpicture.EurJ Haematol.1988;40(3):222–6.
10.LippiG,Lima-OliveiraG,SalvagnoGL,MontagnanaM,Gelati M,PichethG,etal.Influenceofalightmealonroutine haematologicaltests.BloodTransfus.2010;8(2):94–9. 11.InternationalCouncilforStandardizationinHaematology
WGBriggsC,CulpN,DavisB,d’OnofrioG,ZiniG,MachinSJ. ICSHguidelinesfortheevaluationofbloodcellanalysers includingthoseusedfordifferentialleucocyteand reticulocytecounting.IntJLabHematol.2014;36(6):613–27. 12.GuidiGC,SimundicAM,SalvagnoGL,AquinoJL,
Lima-OliveiraG.Toavoidfastingtime,moreriskthan benefits.ClinChemLabMed.2015;53(10):e261–4.
13.Lima-OliveiraG,LippiG,SalvagnoGL,MontagnanaM,Picheth G,GuidiGC.Theeffectivereductionoftourniquetapplication timeafterminormodificationoftheCLSIH03-A6blood collectionprocedure.BiochemMed(Zagreb).
2013;23(3):308–15.
14.DillDB,CostillDL.Calculationofpercentagechangesin volumesofblood,plasma,andredcellsindehydration.JAppl Physiol.1974;37(2):247–8.
15.WestgardJ.Biologicalvariationdatabasespecifications;2010. Availablefrom:http://www.westgard.com/biodatabase1.htm [cited04.10.16].
16.CeriottiF,Fernandez-CalleP,KleeGG,NordinG,SandbergS, StreichertT,etal.Criteriaforassigninglaboratory
measurandstomodelsforanalyticalperformance
specificationsdefinedinthe1stEFLMStrategicConference. ClinChemLabMed.2017;55(2):189–94.
17.ChandraH,ChandraS,RawatA,VermaSK.Roleofmean plateletvolumeasdiscriminatingguideforbonemarrow diseaseinpatientswiththrombocytopenia.IntJLabHematol. 2010;32(5):498–505.
18.LippiG,MattiuzziC,ComelliI,CervellinG.Meanplatelet volumeinpatientswithischemicheartdisease: meta-analysisofdiagnosticstudies.BloodCoagul Fibrinolysis.2013;24(2):216–9.
19.SummersC,RankinSM,CondliffeAM,SinghN,PetersAM, ChilversER.Neutrophilkineticsinhealthanddisease.Trends Immunol.2010;31(8):318–24.
20.ButtarelloM,PlebaniM.Automatedbloodcellcounts:stateof theart.AmJClinPathol.2008;130(1):104–16.
21.LippiG,SalvagnoGL,Lima-OliveiraG,BroccoG,DaneseE, GuidiGC.Posturalchangeduringvenousbloodcollectionisa majorsourceofbiasinclinicalchemistrytesting.ClinChim Acta.2015;440:164–8.
22.LippiG,SalvagnoGL,Lima-OliveiraG,DaneseE,FavaloroEJ, GuidiGC.Influenceofpostureonroutinehemostasistesting. BloodCoagulFibrinolysis.2015;26(6):716–9.
23.LippiG,SalvagnoGL,Lima-OliveiraG,MontagnanaM,Danese E,GuidiGC.CirculatingcardiactroponinTisnotinfluenced byposturalchangesduringvenousbloodcollection.IntJ Cardiol.2014;177(3):1076–7.
24.MayerGA.Diurnal,posturalandpostprandialvariationsof hematocrit.CanMedAssocJ.1965;93(19):1006–8.
25.StatlandBE,BokelundH,WinkelP.Factorscontributingto intra-individualvariationofserumconstituents:4.Effectsof postureandtourniquetapplicationonvariationofserum constituentsinhealthysubjects.ClinChem.
1974;20(12):1513–9.
26.RenoeBW,McDonaldJM,LadensonJH.Influenceofposture onfreecalciumandrelatedvariables.ClinChem.
1979;25(10):1766–9.
27.FeldingP,TrydingN,HyltoftPetersenP,HorderM.Effectsof postureonconcentrationsofbloodconstituentsinhealthy adults:practicalapplicationofbloodspecimencollection proceduresrecommendedbytheScandinavianCommittee onReferenceValues.ScandJClinLabInvestig.1980;40(7): 615–21.
28.MillerM,BachorikPS,CloeyTA.Normalvariationofplasma lipoproteins:posturaleffectsonplasmaconcentrationsof lipids,lipoproteins,andapolipoproteins.ClinChem. 1992;38(4):569–74.
29.MawGJ,MackenzieIL,TaylorNA.Redistributionofbodyfluids duringposturalmanipulations.ActaPhysiolScand.
1995;155(2):157–63.
30.InagakiH,KurodaM,WatanabeS,HamazakiT.Changesin majorbloodcomponentsafteradoptingthesupineposition duringhaemodialysis.NephrolDialTransplant.