w w w . j c o l . o r g . b r
Journal
of
Coloproctology
Original
article
Results
of
videolaparoscopic
surgical
treatment
of
diverticular
disease
of
the
colon
Vinícius
Pires
Rodrigues
∗,
Fábio
Lopes
de
Queiroz,
Paulo
Rocha
Franc¸a
Neto,
Maria
Emília
Carvalho
e
Carvalho
Fundac¸ãoLucasMachado(FELUMA),FaculdadedeCiênciasMédicasdeMinasGerais,BeloHorizonte,MG,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received18May2016 Accepted22May2016 Availableonline14July2016
Keywords:
Diseasediverticular Colorectalcancer Videolaparoscopy
a
b
s
t
r
a
c
t
Introduction:Diverticulardiseaseofthecolon(DDC)isthefifthmostcommon gastroin-testinaldiseaseindevelopedWesterncountries,withmortalityratesof2.5per100,000 inhabitantsperyear.
Objective:Theobjectiveofthisstudyistocomparetheoccurrenceofcomplications, con-versionrate,useofstoma,deathsandtimeofhospitalizationamongpatientsundergoing rectosigmoidectomyforDDCandpatientsundergoingthesamesurgeryforotherreasons.
Method:This was an observational retrospective comparative study. This study was approvedbytheethicscommitteeoftheHospitalFelicioRocho–MinasGerais,Brazil– andthedatawereobtainedfromthesamehospitaldatabase.
Results:Thegroups wereclassifiedaccordingtoage,gender,presenceofcomorbidities, andASAclassification.Therewasnoevidenceindicatingasignificantdifferencebetween groups.Inthisanalysis,noperioperativecomplicationswereobservedandtherewasno needforastoma,andnodeathsorfistulasoccurred.
Conclusion:ElectivelaparoscopicsurgicaltreatmentofDDCintheanalyzedgroupshowed nodifferenceincomplications,durationofsurgeryandhospitalizationtimeversuscontrol group.Therefore,thelaparoscopicsurgicaltreatmentofdiverticulardiseasetranslatesinto anexcellenttoolforboththesurgeonandthepatient.
©2016SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.This isanopenaccessarticleundertheCCBY-NC-NDlicense(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
Resultados
do
tratamento
cirúrgico
videolaparoscópico
da
doenc¸a
diverticular
do
cólon
Palavras-chave:
Doenc¸adiverticular Câncercolorretal Videolaparoscopia
r
e
s
u
m
o
Introduc¸ão:ADoenc¸aDiverticulardoCólon(DDC)éaquintadoenc¸agastrointestinalmais fre-quentenospaísesdesenvolvidosdoocidentecomíndicesdemortalidadede2,5por100.000 habitantesporano.
∗ Correspondingauthor.
E-mail:viniciusprodrigues@gmail.com(V.P.Rodrigues). http://dx.doi.org/10.1016/j.jcol.2016.05.008
Objetivo: Oobjetivodesseestudoécompararaocorrênciadecomplicac¸ões,taxade con-versão,utilizac¸ãodeestoma,óbitoetempodeinternac¸ãoentrepacientessubmetidosa retossigmoidectomiaporDDCepacientessubmetidosaomesmoprocedimentocirúrgico poroutrascausas.
Método: Trata-sedeumestudocomparativo,retrospectivoobservacional.Esteestudofoi aprovadopelocomitêdeéticadoHospitalFelícioRocho-MinasGerais,Brasil-eosdados foramobtidosnobancodedadosdomesmohospital.
Resultados: Osgruposforamclassificadosemrelac¸ãoàidade,sexo,presenc¸aounãode comorbidades e classificac¸ãoASA. Observou-se quenão existemevidências indicando diferenc¸asignificativaentreosgrupos.Nãohouveramcomplicac¸õesper-operatórias, neces-sidadedeestoma,bemcomoóbitosoufístulasnestaanálise.
Conclusão: OtratamentocirúrgicoeletivovideolaparoscópicodaDDCnogrupoanalisado não apresentoudiferenc¸aquanto às complicac¸ões, o tempode cirurgia e otempo de internac¸ãoemrelac¸ãoaogrupocontrole.Portanto,otratamentocirúrgicolaparoscópico dadoenc¸adiverticulartraduz-seemexcelenteferramentatantoparaocirurgiãoquanto paraopaciente.
©2016SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
Introduction
Diverticulardiseaseofthecolon(DDC)isthefifthmost com-mongastrointestinaldiseaseindevelopedWesterncountries andcourseswithanestimatedmortalityrateof2.5per100,000 inhabitantsperyear.1,2
About10–25%ofpatientswithDDCwilldevelop diverticuli-tisanditsassociatedcomplications.3Thesigmoidisthemost
affectedsegmentandisinvolvedin90%ofcases.4
The American Society of Colorectal Surgeons (ASCRS) recommendsthattheelectivesurgicaltreatment ofDDC is basedontheevaluationofeachcase,takingintoaccountthe patient’sage,clinicalconditions,andtheseverityofhis/her diverticulitiscrisisandpersistentsymptomsafter conserva-tivetreatmentofanacuteepisode.5–8
With the development of videolaparoscopic techniques (VL)inthe1990s,thisaccesshasbeenusedforthetreatment ofcomplicatedDDC,orincaseswithrecurrentdiverticulitis attacks.Inastudyof1118patientsundergoinglaparoscopic colectomy,DDCwasthereasonfortheindicationin27%of cases.9
In amulticenter study conductedin Brazil in2007 and involving 4744 patients undergoing colorectal laparoscopic surgery,diverticulardiseasewasthecause ofsurgical indi-cationin40.0%ofpatients.10
Duringthesameperiod,Queirozetal.conductedastudy inthestateofMinasGerais;inatotalof503colorectalsurgery procedures by videolaparoscopic access, 31 cases were of patientswithDDC.11
Although laparoscopy is a method of treatment with proven benefits, for example, less blood loss, less post-operative pain, shorter recovery time and less days of hospitalization,besidesafasterreturntoprofessional activ-itieswhencomparedtoconventionalsurgery,manyauthors reportgreaterdifficultiesincarryingoutaleftcolectomyin patientswithDDCversuspatientswhounderwentthesame surgeryforotherreasons,suchasneoplasticdiseases.12–14
DespiteallthebenefitsalreadyknownwiththeuseofVL colectomycomparedtotheconventionalmethod,only5–10% oftheproceduresarecarriedoutbythatroute.Ofthissmall percentage,lessthanhalfarerelatedtothetreatmentofDDC, eventakingintoaccountthatthisconditionismoreprevalent thancolorectalcancer(CRC).
Thisgreatertechnicaldifficulty,reportedbysomeauthors, could be attributed to the formation of adhesions and local fibrosis, secondary to a chronic or recurrent inflam-matory process.Thereare fewstudies thathave examined whethertherateofcomplications,technicaldifficulties,and ofconversion observedin patientssubmitted toleft colec-tomy/rectosigmoidectomyishigherinpatientsoperatedfor DDCversuspatientsundergoingthesameprocedure,butfor othercauses,suchascolorectalcancer.
Objective
Theaimofthisstudyistocomparetheoccurrenceof compli-cations,conversionrate,useofastoma,deathsandhospital stayamongpatientsundergoingrectosigmoidectomyforDDC andpatientsundergoingthesamesurgeryforotherreasons.
Method
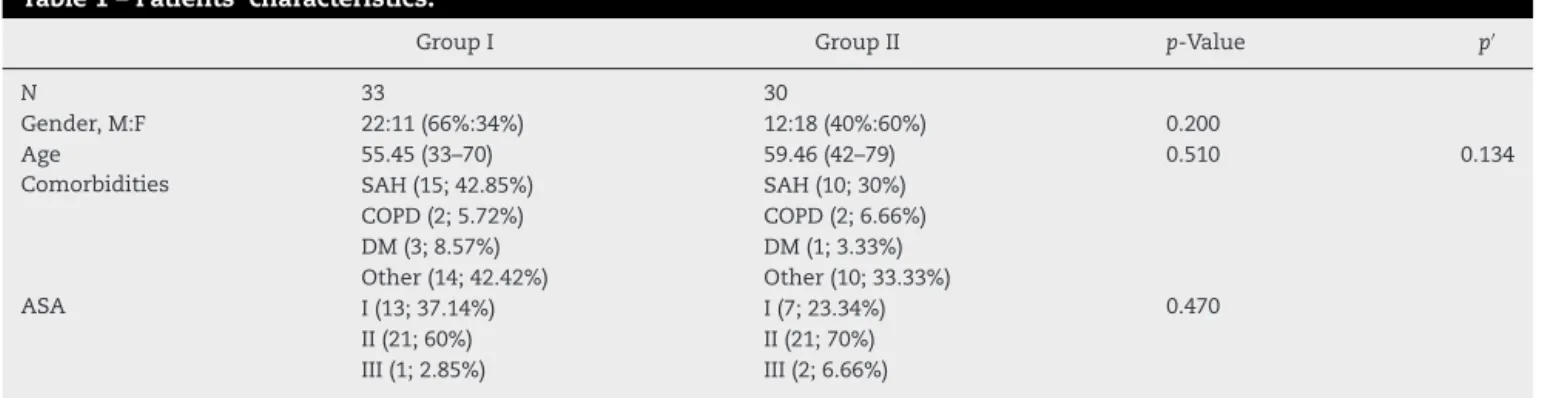
Table1–Patients’characteristics.
GroupI GroupII p-Value p′
N 33 30
Gender,M:F 22:11(66%:34%) 12:18(40%:60%) 0.200
Age 55.45(33–70) 59.46(42–79) 0.510 0.134
Comorbidities SAH(15;42.85%) SAH(10;30%)
COPD(2;5.72%) COPD(2;6.66%)
DM(3;8.57%) DM(1;3.33%)
Other(14;42.42%) Other(10;33.33%)
ASA I(13;37.14%) I(7;23.34%) 0.470
II(21;60%) II(21;70%)
III(1;2.85%) III(2;6.66%)
ASA,AmericanSocietyofAnesthesiology;SAH,systemicarterialhypertension;COPD,chronicobstructivepulmonardisease;DM,diabetes mellitus.
IVtumors, locally invasive, and synchronoustumors were
excluded.
Sixty-fivepatientsundergoingvideolaparoscopic
rectosig-moidectomy(VLRS)wereincluded,ofwhom35hadsigmoid
DDC(GroupI)and30hadsigmoidCRC,Tstage(is-3)N(0–1)M0
(GroupII).
IngroupI,twopatientswereexcludedbecausetheyhad
beenpreviouslytreatedwithtotalcolectomywithileorectal
anastomosisduetoadiffuseinvolvementofthecolonbythe
diverticulardiseasewithareasoffibrosis,hemorrhagicareas,
andmicroabscess.
IngroupII,threepatientshadtheirlaparoscopicprocedure
convertedtolaparotomyduetothedifficultyofexposureand
adhesionsandthuswereexcluded.
All patients underwent ananterograde bowel cleansing
with ingestion of90ml ofdisodium phosphate (oral
solu-tion)dividedinto2parts,withanintervalof6h.Parenteral
antibiotic prophylaxis with ceftriaxone 2g and
metronida-zole1.5gwasadministered30minbeforetheprocedure,and
antithromboticprophylaxiswithenoxaparin40mgwasalso
carriedout.
Theprocedurewasperformedwiththepatientsupineon
thetablewithsplitleggingsafterurinarycatheterizationand
anasogastricprobe(withremovalafterthesurgery).The
oper-ationsbeganbyanumbilicalpuncturewithaVeressneedle,
followedbypneumoperitoneum,placementof5portals(one
of12mm,twoof10mmandtwoof5mm):oneportalforthe
opticaldevice,twoportalstotherightandtwoothertotheleft
ofthepatient,andthepneumoperitoneumwasmaintainedat
apressureof15mmHg.
Trendelenburg position was used to obtain a proper
exposure, and the dissection was performed in a
medial-lateral direction, starting at the inferior mesenteric vein
(IMV),followedbythereleaseofthemesocolonofthebody
and tail ofthe pancreas. Next, ligatureand section ofthe
Table2–Statisticalanalysisofcontinuousvariables.
Normalitytest (p-value)
Comparison betweenGroupsI
andII(p-value)
Hospitalstay 0.047 0.583
Surgerytime 0.035 0.229
inferiormesentericartery(IMA)werecarriedout,with
sub-sequentreleaseofthecolonfromtheparietocolicgutterand
systematicreleaseofthesplenicflexure.
InmalepatientswithDDC(GroupI),wheneveritwas
tech-nicallypossible,thesuperiorrectalarterywaspreserved,in
order toget betterresultsfrom thepointofviewofsexual
function,andalsotodecreasethechanceofananastomotic
dehiscence.
Thetwogroupswerecomparedwithrespecttoage,
gen-der,presenceofcomorbidities,and ASAclassification,with
no difference betweengroups (Table 1).Thevariables
ana-lyzedandcomparedbetweengroupsweresurgicaltime,the lengthofhospitalstay,theoccurrenceofperi-and postopera-tivecomplications,theconversionrate,theneedforastoma, anddeaths.
The data analysis was performed by statistical meth-odsusingtheKolmogorov–Smirnovtest,thenon-parametric Mann–Whitney test (a hypothesis testing tool), and the Fisher’sexacttestandthettestforindependentsamples.
To evaluatethe normalityofvariables “length of hospi-tal stay” and “surgicaltime,” the Kolmogorov–Smirnovtest wasconducted.Inthistest,p-valuesgreaterthan0.10 indi-catethenormalityofvariables.AscanbeseeninTable2,no normalityoccurredforthevariables“lengthofhospitalstay” and“surgerytime.”Forsuchsituations,thenon-parametric Mann–Whitneytestforhypothesistestingwascarriedout,in ordertoassessthepresenceofasignificantdifference(p<0.05) betweentheelapsedtimeinbothgroups.
To evaluate the existence of a significant difference (p<0.05)betweenthehospitalizationtimes,at-testfor inde-pendentsampleswasconducted.
Results
Thegroupswereclassifiedaccordingtoage,gender,presence ofcomorbiditiesandASAclassification(Table1).
Table3–Chronology.
GroupI GroupII
N 35 30
Table4–Statisticalanalysisofpostoperatorycomplications.
GroupI GroupII p-Value
Postoperatory complications
Urinaryretention(2;5.72%) Paralyticileum(1;3.33%) 0.558
Thelengthofhospitalstayrangedfrom2to12days:4.5
daysingroupIand5.2daysingroupII(Table3).Thereisno
evi-denceindicatingasignificantdifferencebetweenthegroups (Table2).
Surgicaltimerangedfrom2h30minto5h10mininthe DDCgroup(mean,3h52m)andfrom2h00minto6h00min intheCRCgroup(mean,4h07min).Theresultsindicatethat thereisnoevidenceofadifferenceinsurgerytimebetween groups(Table2).
Conversiontoopensurgeryoccurredinthreeof63(4.63%) operatedpatientsandallcasesoccurredingroupII.Although theconversionratewashigheringroupII,thesamplesize didnotallowanassessmentoftheriskinvolved,anditwas notpossibletocalculatetheodds ratiooreventoevaluate theexistenceofassociationbytheuseoftheFisher’sexact test.Thus,alargersampleisrequiredinordertoallowan assessmentofthepresenceofarelationship.
Inthisanalysis,nointraoperativecomplicationsoccurred, andtherewasnoneedforastoma;ontheother hand,no deathsorfistulasoccurred.
Finally,tostudytheoccurrenceofpostoperative complica-tionsbetweengroups,theFisher’sexacttestwasperformed (Table4).Thep-valuewas0.558,indicatingthatthereisalso noevidenceindicatinganassociationbetweenthevariables inquestion.
Discussion
Studieshave shownthat theexperience gatheredwiththe useofvideolaparoscopicaccessintheelectivesurgical treat-mentofDDCcausedthistechniquetobecomethepreferred procedurefortreatingsuchacondition.15
Thesampleassessedin ourstudy showedhomogeneity amongtheevaluatedgroupsandsimilarityamongthe eval-uatedindividuals,inthesettingofbettercontrolcriteria.
It was observed that there were no differences in the occurrence of deaths and in stoma rates among groups, althoughsomestudiesdisagreewiththisfinding,statingthat the practice of colectomy for DDC increases both morbid-ity and mortality. The most recent studies agree withour findings,16–19 consideringthattheyhadshown that
intesti-nalbypassincreasesmorbidity(surgicalsiteinfection,DVT, AKI,sepsis,etc.),reoperationrateandmortalityrateofthose patientsundergoingcolectomywithoutanincreasedriskof fistula.
Althoughfewstudieshaveevaluatedthelengthofhospital stayanddurationofthesurgicalprocedurefortheVLRS pro-cedure,theirresultsinvolveastatisticallysignificantincrease ofbothvariableswhenrelatedtothetreatmentofcanceror inflammatorydisease.20However,ouranalysisshoweda
sim-ilaritybetweenthe lengthofhospitalstay and duration of surgerybetweentheanalyzedgroups.
In the past, some studies have shown a higher rate of peri-andpostoperativecomplicationsinVLRS.However,more recentstudiesdonotshowdifferentratesofperi-and postop-erativecomplications.Inthisanalysis,nopatientdeveloped stenosisoranastomoticdehiscence;furthermore,therewas noneedforstomataorsurgicalreinterventions.Schwandner etal.evaluatedtheseoutcomesandshowedthatlaparoscopic colectomyforthetreatmentofdiverticulardiseasedoesnot implyincreasedmorbidity,whencomparedtoother proce-duresrequiringthesametreatment;theseauthorspointedas acausalfactoroftheoccurrenceofanastomoticdehiscence theimpliedtension,whenthemobilizationofthesplenic flex-ureisnotcarriedout.21–23Asinotherstudies,theprevalenceof
minorcomplications,forinstance,paralyticileusandurinary retention,waslow.24
Special circumstances relating to the complexity of the procedureandthepresenceofsevereinflammation accom-panied byadhesions,collections andfistulaswere reported inseveralstudies,ascausesofconversiontoDDCinpatients treatedwithVLRS.25–27 Theoverallconversionratefor
colo-rectal surgery was estimatedat 15.38% ina meta-analysis publishedin2001.25Theelectivecolectomytoprevent
recur-renceorprogressionofthediseasepresentsconversionrates between 2% and 19.7%.28 However, our study showed no
conversions, whichmay berelatedtotheexperienceofthe surgicalteam,theknowledgeofanatomy,andthepathology ofpatients.
IntheUSA,recentlyVanArendonketal.performeda retro-spectiveanalysisinvolvingnearly20%ofthehospitalsinthat country,withanassessmentofthecostsofelectivesurgeryfor thetreatmentofdiverticulardisease,comparingthemwith the costsofotherdiseases thatalsorequiredcolectomy. In this study,50.5% ofpatients had DDCand 43.48% suffered CRC. Afteranalyzing the data, the authors concluded that the elective surgical treatment ofDDC has a high rate of complicationsand ahigh costversussurgicaltreatmentof CRC.20
However,VanArendonketal.conductedananalysis involv-ing the surgical modalities of laparotomy and VL, which compared patientswithvarious comorbidities, withhigher andlowerscoresASA,andwithdifferentdiseasesites.Soon theauthorsobtaineddiscrepantresultspointingtobetterand tendentiousindicesforthegroupwithCRC.
Weunderstandthatthisisaretrospectivestudyconducted inasingleinstitutionandwhichexaminedasmallsampleof individuals.However,thetestsusedforstatisticalanalysisare specifictosmallsamplesandtranslatereliability.
Conclusion
differenceincomplications,duration ofsurgeryand length ofhospitalstaywhencomparedtothetreatmentof colorec-talcancerbythesameapproach.Intheanalyzedgroup,the resultsofrectosigmoidectomyinpatientswithDDCwere sim-ilartothoseofthesameprocedureperformedinpatientswith CRC.
Weacknowledgethatthetreatmentofdiverticulardisease isfraughtwithvariablesthatallowustocarefullyevaluatethe individualneedsofeachpatient;sowhenindicatingsurgery asthebesttherapeuticoption,weshouldnotfearor under-estimatethe videolaparoscopicprocedure, sincewhenwell indicated,ittranslatesintoanexcellenttoolforboththe sur-geonandthepatient.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. ParksTG.Naturalhistoryofdiverticulardiseaseofthecolon. ClinGastrointestinal.1975;4:53–69.
2. SandlerRS,EverhartJE,DonowitzM,AdamsE,CroninK, GoodmanC,etal.Theburdenofselecteddigestivediseases intheUnitedStates.Gastroenterology.2002;122:
1500–11.
3. ChapmanJ,DaviesM,WolffB,DozoisE,TessierD,Harrington J,etal.Complicateddiverticulitis:isittimetorethinkthe rules.AnnSurg.2005;242:576–83.
4. Young-FadokTM,RobertsPL,SpencerMP,WolffBG.Colonic diverticulardisease.CurrProbSurg.2000;37:
459–514.
5. StandardTaskforceAmericanSocietyofColonandRectal Surgeons(ASCRS).Practiceparametersforthetreatmentof sigmoiddiverticulitis.http://ascrs.affiniscape.com/ displaycommon.cfm?an=1&subarticlenbr=124. 6. StollmanNH,RaskinJB.Diagnosisandmanagementof
diverticulardiseaseofthecoloninadults.AdHocPractice ParametersCommitteeoftheAmericanCollegeof Gastroenterology.AmJGastroenterol.1999;94:3110–21. 7. SSATguideline:surgicaltreatmentofdiverticulitis.
http://www.ssat.com/cgi-bin/divert.cgi.
8. AmericanSocietyofColonandRectalSurgeons(ASCRS). WebcastcomToniaYoung-FadokdaMayoMedicalSchool. “CoreSubjects–DiverticularDisease”.www.vioworks.com. 9. KockerlingKF,ScheiderC,ReymondMA,ScheidbachH,
ScheuerleinH,KonradtJ,etal.Laparoscopicresectionof sigmoiddiverticulitis.Resultsofamulticenterstudy. LaparoscopicColorectalSurgeryStudyGroup.SurgEndosc. 1999;13:567–71.
10.CamposFG,ValariniR.Evolutionoflaparoscopiccolorectal surgeryinBrazil:resultsof4744patientsfromthenational registry.SurgLaparoscEndoscPercutanTech.2009.
11.QueirozFL,CôrtesMGW,RochaNetoP,AlvesAC,FreitasAHA, LacerdaFilhoA,etal.Resultadosdoregistrodecirurgias colorretaisvideolaparoscópicasrealizadasnoEstadode MinasGerais-Brasilde1996a2009.RevBrasColoproct. 2010;30:61–7.
12.JonesOM,StevensonAR,ClarkD,StitzRW,LumleyJW. Laparoscopicresectionfordiverticulardisease–follow-upof 500consecutivepacients.AnnSurg.2008;248:1092–7. 13.ConstantinidesVA,TekkisPP,AthanasiouT,AzizO,
PurkayasthaS,RemziFH,etal.Primaryresectionwith anastomosisvs.Hartmann’sprocedureinnonelectivesurgery foracutecolonicdiverticulitis:asystematicreview.DisColon Rectum.2006;49:966–81.
14.RotholtzNA,MonteroM,LaporteM,BunM,LencianasS, MezzadriN.Patientswithlessthanthreeepisodesof diverticulitismaybenefitfromeletivelaparoscopic sigmoidectomy.WordJSurg.2009;33:2444–7. 15.ScheidbachH,SchneiderC,RoseJ,KonradtJ,GrossE,
BärlehnerE,etal.Laparoscopicapproachtotreatmentof sigmoiddiverticulitis:changesinthespectrumofindications andresultsofaprospective,multicenterstudyon1545 patients.DisColonRectum.2004;47:1883–8.
16.WiseKB,MercheaA,CimaRR,ColibaseanuDT,ThomsenKM, HabermannEB.Proximalintestinaldiversionisassociated withincreasedmorbidityinpatientsundergoingelective colectomyfordiverticulardisease:anACS-NSQIPStudy.J GastrointestSurg.2015;19:535–42.
17.PlatellC,BarwoodN,MakinG.Clinicalutilityofa de-functioningloopileostomy.ANZJSurg.2005;75:147–51. 18.LuglioG,PendlimariR,HolubarSD,CimaRR,NelsonH.Loop
ileostomyreversalaftercolonandrectalsurgery:asingle institutional5-yearexperiencein944patients.ArchSurg. 2011;146:1191–6.
19.ThalheimerA,BueterM,KortuemM,ThiedeA,MeyerD. Morbidityoftemporaryloopileostomyinpatientswith colorectalcancer.DisColonRectum.2006;49:1011–7. 20.VanArendonkKJ,TymitzKM,GearhartSL,StemM,LidorAO.
Outcomesandcostsofelectivesurgeryfordiverticular disease:acomparisonwithotherdiseasesrequiring colectomy.JAMASurg.2013;148:316–21.
21.StevensonARL,StitzR,LumleyJ,FieldingG.Laparoscopically assistedanteriorresectionfordiverticulardisease:follow-up of100consecutivepatients.AnnSurg.1998;227:335–42. 22.SchwandnerO,FarkeS,BruchHP.Laparoscopiccolectomyfor
diverticulitisisnotassociatedwithincreasedmorbiditywhen comparedwithnon-diverticulardisease.IntJColorectalDis. 2005;20:165–72.
23.SchwandnerO,FarkeS,FisherF,EckmannC,SchiedeckTHK, BruchHP.Laparoscopiccolectomyforrecurrentand
complicateddiverticulitis:aprospectivestudyof396patients. LangenbecksArchSurg.2004;389:97–103.
24.VargasHD,RamirezRT,HoffmanGC,HubbardGW,GouldRJ, WohlgemuthSD.Definingtheroleoflaparoscopic-assisted sigmoidcolectomyfordiverticulitis.DisColonRectum. 2000;43:1726–31.
25.GervazP,PikarskyA,UtechM,SecicM,EfronJ,BelinB,etal. Convertedlaparoscopiccolorectalsurgery.SurgEndosc. 2001;15:827–32.
26.LeMoineMC,FabreJM,VacherC,NavarroF,PicotMC, DomegueJ.Factorsandconsequencesofconversionin laparoscopicsigmoidectomyfordiverticulardisease.BrJ Surg.2003;90:232–6.
27.SchwandnerO,SchiedeckTHK,BruchHP.Theroleof conversioninlaparoscopiccolorectalsurgery:dopredictive factorsexist?SurgEndosc.1999;13:151–6.