w w w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Review
article
Platelet-rich
plasma
for
osteoarthritis
treatment
Eduardo
Knop
∗,
Luiz
Eduardo
de
Paula,
Ricardo
Fuller
RheumatologyService,HospitaldasClínicas,SchoolofMedicine,UniversidadedeSãoPaulo(USP),SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received3January2014 Accepted11January2015 Availableonline5August2015
Keywords:
Platelet-richplasma Cartilage
Osteoarthritis
a
b
s
t
r
a
c
t
Weconductedacomprehensiveandsystematicsearchoftheliteratureontheuseof platelet-richplasma(PRP)inthetreatmentofosteoarthritis,usingtheMedline,Lilacs,Cochraneand SciELOdatabases,fromMay2012toOctober2013.
Atotalof23studieswereselected,withninebeingcontrolledtrialsand,ofthese,seven randomized,whichincluded725patients.Inthisseries,thegroupreceivingPRPshowed improvementinpainandjointfunctioncomparedtoplaceboandhyaluronicacid.The responselasteduptotwoyearsandwasbetterinmildercases.
HoweveritwasfoundthatthereisnostandardizationinthePRPproductionmethod, neitherinthenumber,timing,andvolumeofapplications.Furthermore,thepopulations studiedwerenotclearlydescribedinmanystudies.Thus,theseresultsshouldbeanalyzed withcaution,andfurtherstudieswithmorestandardizedmethodswouldbenecessaryfor amoreconsistentconclusionaboutthePRProleinosteoarthritis.
©2015ElsevierEditoraLtda.Allrightsreserved.
Plasma
rico
em
plaquetas
no
tratamento
da
osteoartrite
Palavras-chave:
Plasmaricoemplaquetas Cartilagem
Osteoartrite
r
e
s
u
m
o
Fez-seumapesquisaabrangenteesistemáticadaliteratura sobreousodeplasmarico emplaquetas(PRP)notratamentodaosteoartritenasbasesdedadosdoMedline,Lilacs, CochraneeSciELO,demaiode2012aoutubrode2013.
Foramselecionados23estudos,entreelesnoveensaioscontroladose,desses,sete ran-domizados,osquaisincluíram725pacientes.Nessacasuística,ogrupoquerecebeuPRP apresentoumelhorianadorenafunc¸ãoarticularquandocomparadoaoquerecebeuplacebo eácidohialurônico.Arespostadurouatédoisanosefoimelhornoscasosmaisleves.
Entretanto,verificou-sequenãoháumapadronizac¸ãonométododeobtenc¸ãodoPRP,bem comononúmero,intervaloevolumedeaplicac¸ões.Alémdisso,aspopulac¸õesestudadas
∗ Correspondingauthor.
E-mail:eduardoknop@hotmail.com(E.Knop). http://dx.doi.org/10.1016/j.rbre.2015.07.002
rev bras reumatol.2016;56(2):152–164
153
tambémnãoforamclaramentedescritasemmuitosestudos.Dessemodo,essesresultados devemseranalisadoscomcautelaeseriamnecessáriosnovosestudoscommétodosmais padronizadosparaumaconclusãomaisconsistentesobreopapeldoPRPnaosteoartrite.
©2015ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Although osteoarthritis (OA) is one of the most prevalent musculoskeletaldiseasesintheworld,its treatmentisstill relativelylimited.1TheOsteoarthritisResearchSociety
Inter-nationalnotesthatthereislittleevidencethatthecurrently useddrugshaveeffectiveactionagainsttheprogressionofthe disease.2
ArelativelynewstrategyforthetreatmentofOAistheuse ofcellelementsandbiomediatorsoftissueresponse.Inthis context,theplatelet-richplasma(PRP)hasbeenconfiguredas aperspectiveforimprovingclinicalandstructuraloutcomes bydeliveringahighconcentrationofgrowthfactorsthat medi-atecartilagehealingandremodeling.Itspotentialhasbeen showninvitroandinvivostudies,howeveritsrealefficacyin OAisnotwellestablished.3
Thus,thisstudyhasthepurposetopresentsometechnical aspectsforobtainingPRP,possiblemechanismsofactionand areviewofitsuseinkneeosteoarthritis.
Methods
We conducted a comprehensive and systematic litera-ture search using MEDLINE, LILACS, Cochrane and SciELO databases,fromMay2012toOctober2013.Thekeywordsused were “platelet-rich plasma,” “platelet-rich growth factor”, “osteoarthritis”,“hip”, “knee”,“ankle”, “human”and “carti-lage”.Thestudiesfoundintheinitialsearchwerereviewed andadditionalreferenceswerealsoevaluatedandincluded whererelevant.Thesearchwaslimitedtostudiesperformed inhumans. The selected articles were read in full bytwo reviewersforanalysisoftheirmethodsandtheirlimitations. Disagreementswerediscussedforaconsensus,withthe medi-ationofathirdauthor.
Thequalityofthestudiesanalyzedwasinitiallyclassified accordingtorandomization.Thenweproceededtothe eval-uationofthefollowingitems: typeofcontrolgroup(active controller–hyaluronicacid–orplacebo),double-blind evalua-tion(withdescriptionofSHAMprocedure),numberoftreated patients,definitionofradiographicand levelofpaininthe inclusioncriteria,definitionofexclusioncriteria,description ofblindingandrandomizationprocess,intentiontotreat anal-ysis,assessmenttools(whetherincludingOMERACTcriteria ornot),descriptionoftheprocesstoobtainPRP,platelet con-centration, volume injected, guided-injection performance, numberofinjectionsinthetreatedandcontrolgroups,and reportofadverseevents.
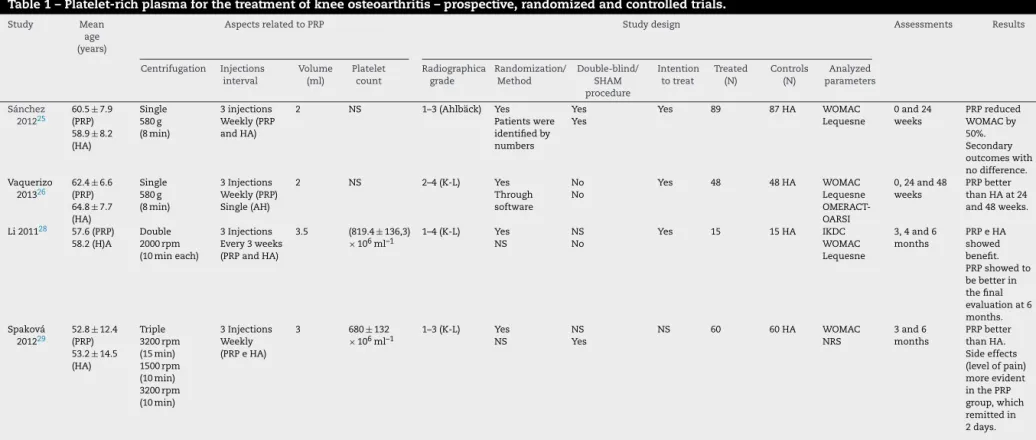
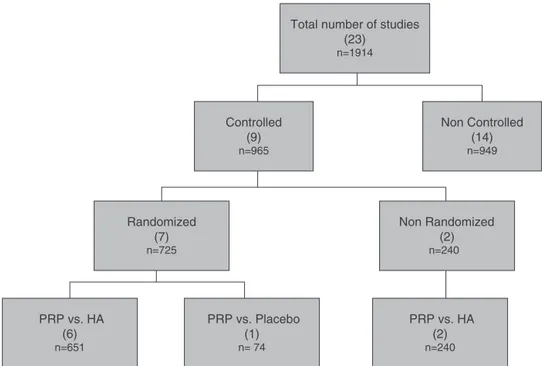
Atotalof23studies(Fig.1andTables1and2)wereselected, withninebeingcontrolledtrials,andofthese,seven random-ized,whichincluded725patients.Inthisreviewsomeresults
ofother13 non-controlledstudies,andalsoaretrospective cohortwerealsolisted.
Mechanism
of
action
of
PRP
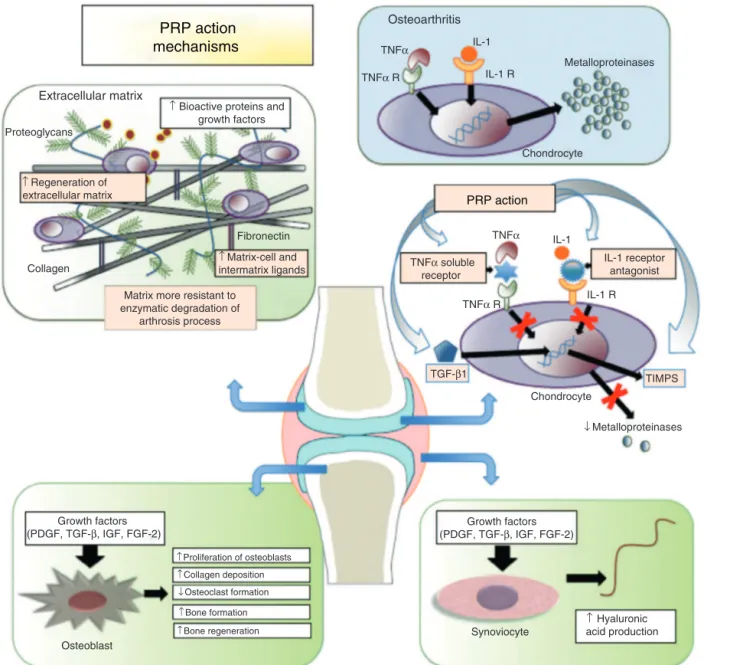
When PRP is injected into the injured site, platelets are activated by endogenous thrombin and/or intra-articular collagen.4Onceactivated,thereissecretionofgrowthfactors
by degranulation of the ␣-granules.5 Among secreted
sub-stances we canfind: platelet-derived growth factor (PDGF), interleukin-1receptorantagonist(IL-1RA),solublereceptorof tumornecrosisfactor␣(TNF-RI),transforminggrowthfactor
(TGF-),plateletfactor4(PF4),vascularendothelialgrowth fac-tor(VEGF),epidermalgrowthfactor(EGF),insulin-likegrowth factor(IGF),osteocalcin(Oc),osteonectin(On),fibrinogen, vit-ronectin,fibronectinandthrombospondin-1(TSP-1).6
Many ofthesemediators actasanti-catabolic and anti-inflammatoryagents.TheantagonistofIL-1receptorinhibits activationofNFBgene,cytokineinvolvedinapoptosis and inflammationprocess.4,7 Moreover, thesolublereceptorsof
the tumor necrosis factor bind to TNF-␣, preventing its interactionwithcellularreceptorsanditspro-inflammatory signaling. TGF-1 also acts as a factor inhibiting cartilage degradation,regulatingandenhancinggeneexpressionof tis-sueinhibitorsofmetalloproteinases(TIMP-1).8Otherfactors
suchasIGF-1,PDGFandTGF-1favorthestabilizationof car-tilagebycontrollingthemetabolicfunctionsofchondrocytes andsubchondralbone,maintainingthehomeostasisbetween thesynthesisanddegradationofproteoglycans,and stimulat-ingtheproliferationofchondrocytes.9,10Itwasalsofoundthat
plateletgrowthfactorsstimulatesynovialfibroblaststo syn-thesizehyaluronicacid.9Thesemechanismsareillustratedin
Fig.2.
Technical
aspects
for
obtainment
of
platelet-rich
plasma
PRPisobtainedbycentrifugingtheautologousvenousblood, causing a high concentration of platelets in a small vol-umeofplasma.11Thereisnostandardizationregardingthe
speed,durationandnumberofcentrifugationsneeded, nei-therwhichlayerexactlyisremovedfromtheprecipitateafter thisprocess.3
r
e
v
b
r
a
s
r
e
u
m
a
t
o
l
.
2
0
1
6;
5
6(2)
:152–164
PRP actio
n
mechanisms
Osteoarthritis
TNFα R
TNFα R
TGF-β1
Growth factors (PDGF, TGF-β, IGF, FGF-2) Growth factors
(PDGF, TGF-β, IGF, FGF-2)
TNFα
IL-1 R
IL-1 R
TIMPS Metalloproteinases
Chondrocyte
Chondrocyte
Osteoblast
Synoviocyte
↓Metalloproteinases
↑Bioactive proteins and growth factors
↑Regeneration of extracellular matrix
TNFα soluble receptor
IL-1 receptor antagonist TNFα
↑Matrix-cell and intermatrix ligands
↑Hyaluronic acid production
↓Osteoclast formation
↑Bone regeneration
↑Bone formation
↑Collagen deposition
↑Proliferation of osteoblasts
Matrix more resistant to enzymatic degradation of
arthrosis process Collagen
Fibronectin Proteoglycans
Extracellular matrix
IL-1
IL-1
PRP action
r
e
v
b
r
a
s
r
e
u
m
a
t
o
l
.
2
0
1
6;
5
6(2)
:152–164
155
Table1–Platelet-richplasmaforthetreatmentofkneeosteoarthritis–prospective,randomizedandcontrolledtrials.
Study Mean age (years)
AspectsrelatedtoPRP Studydesign Assessments Results
Centrifugation Injections interval
Volume (ml)
Platelet count
Radiographica grade
Randomization/ Method
Double-blind/ SHAM procedure
Intention totreat
Treated (N)
Controls (N)
Analyzed parameters
Sánchez 201225
60.5±7.9 (PRP) 58.9±8.2 (HA)
Single 580g (8min)
3injections Weekly(PRP andHA)
2 NS 1–3(Ahlbäck) Yes
Patientswere identifiedby numbers
Yes Yes
Yes 89 87HA WOMAC
Lequesne
0and24 weeks
PRPreduced WOMACby 50%. Secondary outcomeswith nodifference. Vaquerizo
201326 62.4
±6.6 (PRP) 64.8±7.7 (HA)
Single 580g (8min)
3Injections Weekly(PRP) Single(AH)
2 NS 2–4(K-L) Yes
Through software
No No
Yes 48 48HA WOMAC
Lequesne OMERACT-OARSI
0,24and48 weeks
PRPbetter thanHAat24 and48weeks.
Li201128 57.6(PRP) 58.2(H)A
Double 2000rpm (10mineach)
3Injections Every3weeks (PRPandHA)
3.5 (819.4±136,3)
×106ml–1 1–4(K-L) NSYes NSNo Yes 15 15HA IKDCWOMAC Lequesne
3,4and6 months
PRPeHA showed benefit. PRPshowedto bebetterin thefinal evaluationat6 months. Spaková
201229 52.8
±12.4 (PRP) 53.2±14.5 (HA)
Triple 3200rpm (15min) 1500rpm (10min) 3200rpm (10min)
3Injections Weekly (PRPeHA)
3 680±132
r
e
v
b
r
a
s
r
e
u
m
a
t
o
l
.
2
0
1
6;
5
6(2)
:152–164
Table1–(Continued)
Study Mean age (years)
AspectsrelatedtoPRP Studydesign Assessments Results
Centrifugation Injections interval
Volume (ml)
Platelet count
Radiographica grade
Randomization/ Method
Double-blind/ SHAM procedure
Intention totreat
Treated (N)
Controls (N)
Analyzed parameters
Cerza
201230 66.5
±1.3 (PRP) 66.2±10.6 (HA)
Double NS
4Injections Weekly (PRPeHA)
5.5 NS 1–3(K-L) Yes
NS
No No
Yes 60 60HA WOMAC 4,12and24 weeks
PRPbetter thanHA, regardlessof gradeof osteoarthritis. Filardo,
201231 55(PRP) 58(HA)
Double 1480rpm (6min) 3400rpm (15min)
3Injections Weekly (PRPeHA)
5 NS 1–3(K-L) Yes
NS
Yes Yes
Yes 55 54HA IKDC
EQ-VAS Tegner KOOS
2,6and12 months
Nodifference betweenPRP andHA. Tendencyof superiorityof PRPinlower gradesof osteoarthritis Patel
201333 53.1
±11.6 (GroupA) 51.6±9.2 (GroupB) 53.7±8.2 (GroupC)
Single 1500rpm (15min)
GroupA: Single(PRP) GroupB:2 ijections,one every3weeks (PRP) GroupC: Single (placebo)
8 31,014
×106L–1 1–2(Ahlbäck) YesThrough software
Yes Yes
No 26
(GroupA) 25 (GroupB)
23saline WOMAC 6;12and24 weeks
PRPsuperiorto placebo Nodifference betweenone ortwo Injections
r
e
v
b
r
a
s
r
e
u
m
a
t
o
l
.
2
0
1
6;
5
6(2)
:152–164
157
Table2–Plateletrichplasmaforthetreatmentofhumanosteoarthritis–nonrandomized,non-controlled,cohorttrials.
Studies Typeofstudy Joint Centrifugation Treated (N)
Controls (N)
Injections(N) interval
Analyzed parameter
Assessment Results
Say27 Prospective
Controlled Non-randomized
Knee Single 45 45HA InjectionSingle KOOS
VAS
0,3and6months PRPsuperiortoHA. Bettercost-benefitof PRP
Kon32 Prospective
Controlled Non-randomized
Knee Double 50 50HAAP
50LWHA
3injections Biweekly
IKDC EQ-VAS
2and6months PRPshowedbenefit;
Betterresultsinyoung peopleandlowerdegree ofdegeneration
Sánchez34 Retrospective Knee Single 30 30HA 3injections
Weekly
WOMAC 8weeks PRPsuperiortoHA
Kon35 Prospective Knee Double 100 None 3injections
Every3weeks
IKDC EQ-VAS
2,6and12months PRPshowedbenefit; Betterresultsinyoung peopleandlowerdegree ofdegeneration
Filardo36 Prospective Knee Double 91 None 3injections
Every3weeks
IKDC EQ-VAS
2,6,12and24 months
PRPshowedbenefit; Decreaseinresponse after12months,but higherthantheinitial scores
Sampson37 Prospective Knee Single 14 None 3injections
Monthly
Brittberg-Peterson VAS
KOOS Thickness
2,5,11,18and52 weeks
PRPshowedbenefit; Noincreaseinthickness ofcartilage
Ana
Wang-Saegusa38
Prospective Knee Single 261 None 3injections
Biweekly
VAS SF-36 WOMAC Lequesne
6months PRPshowedbenefit
Napolitano39 Prospective Knee Single 27 None 3injections
Weekly
WOMAC NRS
7daysand6 months
PRPshowedbenefit
Sanchez40 Prospective Hip Single 40 None 3injections
Weekly
WOMAC VAS HHS
6–7weeksand6 months
PRPshowedbenefit
Jang41 Prospective Knee Double 65 None Injectionssingle WOMAC 1,3,69and12
months
PRPshowedbenefit
Battaglia42 Prospective
Pilotstudy
Hip Notspecified 20 None 3injections
Biweekly
HHS WOMAC
3,6and12months PRPshowedbenefit; Decreaseinresponse after3months,but higherthantheinitial scores.
r
e
v
b
r
a
s
r
e
u
m
a
t
o
l
.
2
0
1
6;
5
6(2)
:152–164
Table2–(Continued)
Studies Typeofstudy Joint Centrifugation Treated (N)
Controls (N)
Injections(N) interval
Analyzed parameter
Assessment Results
Halpern43 Prospective
PilotStudy
Knee Notspecified 17 None InjectionsSingle VAS
WOMAC MRIdeknee
1,3,6and12 months
PRPshowedbenefit Therewasnoreduction incartilagethicknessin MRI
Gobbi44 Prospective Knee Single 50 None 2injections
Monthly
KOOS, VAS Tegner IKDC Marxscores
0,6and12months PRPshowedbenefit; Therewasnodifference betweenpatientsthat werepreviously approachedand patientswithno previousintervention.
Hart45 Prospective Knee Double 55 None 6injections
Weekly.After maintenance with3quarterly injections
Lysholm Tegner IKDC Cincinnati KneeMRI
0and12months PRPshowedbenefit
Therewasnoreduction incartilagethicknessin MRI
Filardo46 Prospective Knee Double 72PRGF
72PRP
None 3injections
Each3weeks
IKDC EQ-VAS Tegnerscores
2,6and12months Similarbenefitbetween methods;
Doublecentrifugation showsmoresideeffects
Dhollander47 Prospective Knee Double 5 None InjectionsSingle VAS
KOOS TegnerScore MOCART
0,12and24 months
Procedureleadsto clinicalimprovement; Noresponseinthe analysisofcartilagein MRI
rev bras reumatol.2016;56(2):152–164
159
Total number of studies (23)
n=1914
Controlled (9)
n=965
Non Controlled (14)
n=949
Non Randomized (2)
n=240
Randomized (7)
n=725
PRP vs. Placebo (1)
n= 74
PRP vs. HA (2)
n=240
PRP vs. HA (6)
n=651
Fig.2–Platelet-richplasma(PRP)inthetreatmentofhumanosteoarthritis.PRP,platelet-richplasma;HA,hyaluronicacid;n, totalnumberofpatientsevaluatedinallstudies;inbrackets,numberofstudies.
contrasttothepathofthrombin,whichinducesanimmediate releaseofgrowthfactors.12Regardlessoftheactivatorused,it
isrecommendedthatthecomponentisappliedimmediately afterplateletactivation.13
Recentlysomeauthors14developedaclassificationofthe
differenttypesofPRP,accordingtotheplateletcount,the acti-vatorused,andthepresenceofwhitebloodcells.Thissystem wascalledPAW(Platelets,ActivationandWhiteBloodCells). Theclassification,however,iscomplexanditspractical sig-nificancehasnotbeenestablishedyet.
Ingeneral,therearetwobasictypesofplatelet-richplasma compounds:theplatelet-richplasma,obtainedbydouble cen-trifugationofbloodtogetherwithananticoagulant(citratein general);andplateletrichingrowthfactors(PRGF)obtained throughasinglecentrifugation,alsowithananticoagulant agent.However,thereisnostandardizationforitsobtainment, andeachstudyhasitsownmethod.
Clinical
applications
of
platelet-rich
plasma
PRPhasbeenutilized invarious clinicalsituationsinorder toregenerate tissues. Itiscurrently usedin thetreatment of soft tissue lesions, such as repair of chronic ulcers,15
tendinopathiesandfasciitis.16 Itsuse indental procedures,
suchasperiodontalregenerationindentalimplants,17 bone
regenerationingrafts18andfractures,isalsonoteworthy.19
TheactionofthePRPbegantobestudiedinosteoarthritis inordertoincreasetheanabolicactivityofchondrocytes.The platelet-rich plasma iscapable ofinducing proliferation of mesenchymalcells,asdemonstratedinvitrobyHuangetal.20
andKilianetal.21PRPcanregulatetheactionof
metallopro-teinases and activate mechanisms of matrix regenerators such as the synthesis of collagen and proteoglycans.22
Nakagawaetal.23demonstrated theinvitro efficacyofPRP
stimulatingchondrocyteproliferationandsynthesisof colla-gen.Mishraetal.24showedthattheplatelet-richplasmacan
leadtoproliferationoffibroblastsinvitro,aswellasstimulate theexpressionofgenesresponsibleforthechondrogenicand osteogenicdifferentiation.
PRPcontrolledtrialsversushyaluronicacidorplacebo
Sánchezetal.25in2012,inadouble-blind,randomizedtrial,
comparedthePRPandhyaluronicacidin176patientswith kneeOA.ThescoresusedfortheanalysiswereWOMAC (West-ernOntarioMcMastersUniversitiesOsteoarthritisIndex)and Lequesne.TreatmentwithPRP reducedby50%theWOMAC index(primaryoutcome)andshowedatrendofimprovement in secondary outcomes,howeverwith no statistical signif-icance. The limitations mentioned by the author were no comparisonbetweenthelevelofphysicalactivitybeforeand after treatment, the short follow-up, the lack ofa placebo groupandtheexclusionofcasesconsideredtobesevereon radiographicexamination.
Vaquerizoetal.26publishedin2013astudywithsimilar
designtothestudybySanchez,where96patientswere eval-uatedfor48weeks.ThePRP showedbetterresponsesinall parametersanalyzed,bothin24andin48weeks,including the percentageofrespondersofOMERACT-OARSI(Outcome Measures for Rheumatology Committee and Osteoarthritis ResearchSocietyInternationalStandingCommitteefor Clini-calTrialsResponseCriteriaInitiative).
Anotherstudypublishedin2013conductedbySayetal.,27
Thestudyshowedclinicalimprovementwithbothtreatments afterthreeandsixmonthsoftheprocedures,however,with abetterresponseinpatientstreatedwithPRP.Furthermore, thecostoftreatmentwaslowerinthegrouptreatedwithPRP. Thelimitationsmentionedbytheauthorwerenopatients ran-domizationandtheexclusiveuseofclinicalparametersinthe resultsanalysis.
Li et al.28 in2011, conducteda randomizedstudy
com-paring the use of PRP and HA in 30 patients with knee osteoarthritis.BothgroupsshowedimprovementinWOMAC andIKDCindicators(InternationalKneeDocumentation Com-mittee),maintainingsimilarefficacyuptothefourthmonthof follow-upandsuperiorityofPRPinthesixthmonth.Theshort follow-upperioddoesnotallowtheevaluationoftheduration oftheresponse,butpointstothetrendofamoresustained responseofplatelet-richplasma.
Spaková et al.29 in 2012, in a randomized study,
fol-lowed120patientsforsixmonthswithkneeosteoarthritis: 60 received PRP and 60 HA. The group receiving PRP pre-sentedbetterimprovementcomparedtoHAwhenassessed byWOMACandtheNRS(NumericalRatingScale).
Cerzaetal.30comparedPRPandHAin120patientswith
kneeosteoarthritisfollowedfor24weeks.Theassessmentby theWOMACshowedbetterresponseswithPRP,regardlessof thedegreeofjointdamage(assessedbytheKellgren-Lawrence classification),contrastingwithHAwhichwasineffectivein treatingosteoarthritisgradeIII.
In 2012, Filardo et al.31 also compared PRP with HA in
109patientswithosteoarthritis ofthe knee througha ran-domizeddouble-blindstudy.Thepatientswereevaluatedby IKDC,EQ-VAS(visualanalogscaleEuroQol),TegnerandKOOS scoresoveraperiodof12months.Bothgroupsshowed clin-icalimprovement,withnodifferencebetweenthem.When comparingthegroupsregardingthedegreeofosteoarthritis inthescaleofKellgren-Lawrence,onlyatrendtowardbetter responsefromPRPinmilderdegree(degrees≤II)wasfound.
Konetal.32in2011treatedthreegroupsof50patientswith
kneeosteoarthritiswhoreceivedPRP,highandlowmolecular weightHArespectively.Arandomdistributionofpatientswas notcarriedoutamongthethreegroups,sincethetreatment performedwasdependentonthecenterwheretheinjections wereperformed,witheachinstitutionbeingresponsiblefor theapplicationofasinglesubstance.Clinicalresponse mea-suredbytheIKDCandEQ-VASscoreswashigherinpatients thatreceivedPRPinjectionscomparedtoHA.Thelow molec-ular weight HA performed better than the high molecular weight;however, still lower than theresponse obtainedby PRP.
Patel et al.33 in 2013 selected 74 patients with knee
osteoarthritisanddividedthemrandomlyintothreegroups: thosethatreceivedasinglePRPinjection(n=26);thosewho received two PRP injections3-weeks apart (n=25) and the thirdgroup(n=23)whoreceivedasingleplaceboinjectionof normalsaline.ThegroupswereassessedbyWOMACscoreby anobserverblindedtotreatmentstatusfor24weeks.There wasasignificantimprovementinbothgroupsreceiving inter-vention,withatendencytodecreaseinthelastassessment at six months. Regarding the number of injections, there wasnoincreaseinresponsetotreatmentwithanadditional application.
Non-controlledstudiesandretrospectivecohort
Inaretrospectivecohortstudy,Sánchezetal.34evaluatedtwo
groupsof30patientswithknee OAwho weretreatedwith PRPandHAinfiltrations,respectively.Patientswereevaluated byWOMAC(paindomainastheprimaryoutcome), compar-ing baseline data with those obtained after five weeks of injections. There wasa betterresponseofpatients treated withPRPcomparedtoHA.Asthiswasaretrospectivestudy andbasedondatareviewedinthemedicalrecords,thelack of some information, such as mean disease duration and use ofanalgesics,mayhavejeopardizedtheanalysisofthe data.
Kon et al.35 conducted a prospective study in 2010 in
which100patientswithkneeosteoarthritisweretreatedwith PRP andevaluated atsixand twelvemonthsthroughIKDC and EQ-VAS scales. There was afavorable responsein the firstsixmonths,notsustainedaftertwelvemonths,despite remainingsignificantlyabovetheinitialscores.Anotherstudy bythesamegroup,withsimilarmethods,publishedin2010 byFilardoetal.36demonstratedapositiveresponseinthefirst
twelvemonths,whichwasnotsustaineduntiltheendofthe secondyearoffollow-up.
Sampsonetal.37in2010evaluatedtheuseofPRPinknee
OAin14patientsusingtheKOOSandBrittberg-PetersonVAS scores,andfollowedthemfor52weeks.Therewasa signifi-cantclinicalimprovementinpatientstreatedwithPRP.
Ana Wang-Saegusa et al.38 conducteda study with 216
patientswithkneeOAthatreceivedPRPinjection,assessedby VASscores,SF-36(ShortForm36HealthSurvey),WOMACand Lequesneforsixmonths.Allindexesshowedimprovementin clinicalparametersevaluated.
Napolitanoetal.39injectedPRPin27patientswith
degen-erativediseasesoftheknee, dividedintotwogroups:those withosteoarthritisandthosewithcartilagediseases(not spec-ified).UsingtheWOMACandNRSquestionnaires,therewas an early and sustained responsefor sixmonths follow up inbothgroups. Aslimitations,theauthor does notspecify theselectioncriteriaandthestudylacksstatisticalanalysis, whichpreventstheinterpretationofresults.
Sanchezet al.40 studiedtheeffectofPRPinjectionin40
patientswithunilateralhipOA.Theindicesusedfor evalu-ationwere WOMAC,VASandHHS(HarrisHipScore).There wasapositiveresponsetoPRPandthepatientswhodidnot respondhadmoresevereosteoarthritisonradiographic exam-ination.
In2012,Jangetal.41studiedtheeffectofasingleapplication
ofPRPin65patientswithkneeosteoarthritis.Thepatients showedafavorableresponseintheVASforpain,andIKDCup tosixmonthsaftertreatment,whichwasnotsustainedafter oneyearoftheinjection.
Inapilotstudy,Battagliaetal.42checkedtheeffectofPRP
in 20 patientswith hip OA,assessedby HHSand WOMAC for12months.Therewasasignificantimprovementbetween the first and thirdmonths, with aprogressive decrease in theresponsethereafter.Afteroneyear,theindicesremained abovebaseline.
Inanotherpilotstudy conductedbyHalpernetal.,43 the
rev bras reumatol.2016;56(2):152–164
161
andfunctionalindicesweresignificantlyreducedatsixand twelvemonthscomparedtobaseline.
UseofPRPinprevioussurgicalinterventions
Gobbi et al.44 in 2012 studied the PRP application on the
kneeof50individuals,subdividingthemalsoinpatientswho hadundergonesurgeryinthisjointandotherswithnoprior approaches.Surgicalproceduresconsideredinthisstudywere thearthroscopicdebridementandmicrofractures.The instru-mentsusedwereKOOS,VAS,Tegner,IKDCandMarx.Aclinical improvementwasobservedinthepatientsafterinjectionof PRP regardingpain,functionand return tousualactivities, regardlessofsurgeryperformed.
In2013,Hartet al.45 performeda sequenceofnine PRP
applicationsafterundergoingarthroscopyin50patientswith kneeOA.TheassessmenttoolswereLyshcolm,Tegner,IKDC and Cincinnati scores. There was an improvement of the indicesaftersixmonthsoftreatment,whichwasnot main-tainedafter12months.
PRPobtainedfromsingleversusdoublecentrifugation
Regardingthe techniqueforobtainingplatelet-richplasma, Filardoetal.46in2011conductedastudywith144patients
with knee osteoarthritis, comparing the acquisition of platelets concentratebysingle (plasmarich ingrowth fac-tors–PRGF)ordoublecentrifugation(PRP).Itwasfoundthat the benefitwassimilar inboth groupsusing the IKDC,EQ VASandTegnerscores.However,adverseevents(especially localarthritis)occurred moreofteninthe PRP obtainedby doublecentrifugation,duetohigherleukocyteconcentration producedbythismethod.
PRPefficacyevaluationthroughimagingmethods
Thereisnoconsistentevidenceregardingtheeffectiveness ofPRPmeasuredbyimagingmethods.Somenon-controlled seriespointtoapossiblestabilizationofcartilageloss.
Sampsonetal.37 in2010,inadditiontoclinicalresponse
assessment previously described, performed a joint ultra-sound to measure the articular cartilage thickness one year afterPRP injectionin14 patients studied. Theresults showedno benefitinincreasing thethicknessofthe artic-ularcartilage,whichdoesnotmeananegativeresult,since the method sensitivity is low for the detection of small changes.
Dhollander et al.47 in 2011 treated five patients with
chondrallesions ofthe patellawith cartilage debridement, followedbyplacementofacollagenmembraneandPRP.The patientswereevaluatedbymagneticresonanceimaging(MRI) before the procedure and after 12 and 24 months. Bene-fits were observed in clinical scores (VAS, KOOS subscale), exceptforthe Tegner score. However,there wasno differ-enceinMOCARTscore(MagneticResonanceObservationof CartilageTissueRepair),andonlystabilityofthelesionstook place.
Hartetal.45in2013evaluatedPRPresponsein50patients
withkneeOAbyMRIbeforeandoneyearaftertheinjection. Thedegreeofcartilage damagewasmeasured bymodified
Outerbridge Grading Scale. Cartilage thickness remained unchanged in94%ofcasesand aslightincrease(lessthan 1mm)wasrecordedinthreecases(6%).Therewasnocontrol group.
In a pilot study, Halpern et al.43 also evaluated, in a
non-controlledmanner,thearticularcartilageof17patients undergoing PRP injection, using knee MRI. There was no reduction in cartilage thickness during the year analyzed. Consideringthatthereisanannualfallof4%to6%inthe volumeofarticularcartilageinosteoarthritis,47 theauthors
concludethatPRPcanhaveachondroprotectiveaction.
Side
effects
Sideeffectsrelatedtoinjectionofplatelet-richplasmaare con-sidereduncommonand,whenpresent,usuallymanifestina mildandself-limitedform.
Local symptoms are the most common adverse events, rangingfrom painattheinjectionsitetosignsofarthritis. Filardo etal.46 in2011showedthatthe wayofobtainment
ofPRPinfluencesthedegreeofintra-articularinflammatory response,withthiseffectbeingattributedtothenumberof leukocytespresentintheinfiltrate.Allergicreactionsare pos-siblebut rareeffectssinceitisanautologousproduct.The mostfearedcomplicationistheintra-articularinfectionthat canbepreventedbyperformingtheasepticprocedure.
In the studies selected from this review, the most fre-quently reported adverse events were arthralgia in the injected joint,whose intensityvaried from mildto moder-ate,anditsresolutionoccurredindays,extendingtoweeks inthemostseverecases.Dhollanderetal.47reportedacase
ofhypertrophyoftheregeneratedcartilagetissuediagnosed byanarthroscopyperformedbecauseofthepatient’s symp-toms,andwasresolvedbylocaldebridement.Sánchezetal.40
reportedacaseofrashaftertheinjection,theresolutionof whichwasspontaneous,withnoneedforspecifictreatment. Filardoetal.31demonstratedthathigherpost-injectionpain
wasnotedinthosepatientsinjectedwithPRP comparedto HA.Systemicsymptomsandinfectionswerenotreportedin theanalyzedstudies.
Final
considerations
Inthisreviewsevenrandomizedcontrolledtrialswerefound, whichshowedagreatmethodologicaldiversity,bothindesign and in procedure for obtainment and injection of PRP. Of these,onlyone33usedtheplacebocomparison.Theother
con-trolgroupsreceivedintra-articularhyaluronicacid,although there is no consensusin the literature about its effective-ness in the treatment of osteoarthritis.48 Only one of the
controlledstudies25definedthedegreeofpaininthesample
adoptionofanappropriateSHAMprocedure.Therewere dif-ferencesorlackofdataintherangeandnumberofinjections, administeredvolumeandplateletconcentration.The assess-menttoolsalsovaried,andonlyonestudy26usedOMERACT.
There are numerous other differences among the studies, asshowninTable1.Thislargevariabilitywasalsorecently appointedinaninterestingreview,3withtheconclusionthat
morecontrolledstudiesaboutthesubjectarenecessary. Despitethemethodologicalheterogeneityandgapsinthe designs,Changetal.,49in2013,publishedameta-analysison
theuseofPRPinpatientswithkneeosteoarthritis.Thequality oftheworkwasmeasuredbyJadadscore,withtheselection of16papers.Theanalysiswasbasedonthechoiceofonly oneofthe scoresusedineach article,establishingthe fol-lowingpriority:IKDC,KOOSandWOMAC.Theresultsshowed higherefficacyanddurabilityoftreatmentwithPRP compari-sonwiththecontrolgroup.Theauthorexposesthelimitations ofthemeta-analysis,highlightingthelackofstandardization inmethodsforPRPobtainment,thedifferentscoresusedin thework,resultinginaheterogeneousdataanalysis;andthe inclusionofpatientswithKellgren-Lawrencescaleofzeroin somestudies.
InthesameyearasystematicreviewbyKhoshbinet al. waspublished.50 Theirassessmentwasbasedinscalesthat
consider randomization, blinding, results, measurements, inclusionandexclusioncriteria,descriptionoftreatmentand statistical analysis. In the end, six studies were selected. AbenefitofPRP wasobservedcomparedtocontrolgroups (hyaluronicacidandsaline)inWOMACscoreinfourstudies andIKDCinthreestudies,butnobenefitsinothercriteriasuch asvisualscaleofpainandpatientsatisfactionscores.Adverse eventsweremorefrequentinthegroupreceivingPRP.
Weconcludethat,basedonrandomizedcontrolled stud-ies,PRP seems to produce improvementin pain and joint functioninkneeosteoarthritis,bothcomparedtoplaceboand hyaluronicacid.Theresponsecanbesustainedforaperiodof uptotwoyears,andseemstobemoreevidentinmildercases ofOA.ThereisnoconsistentevidenceoftheactionofPRPon thecartilagemeasuredbyimaging.
AlthoughPRPseemstobeaneffectiveoption,cautionis requiredininterpretingtheresults.Inmoststudiesthesample issmall,theperiodofobservationshortandOAcharacteristics havenotbeenfullydescribed.Thecomparisonoftheresults iscomplicatedbythelackofstandardizationinthecollection andapplicationofPRPregimen.
Thus,morerandomized,prospectivestudieswith appro-priatedesignare needed toconfirmthe actual PRP role in osteoarthritis.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. GerwinN,HopsC,LuckeA.Intraarticulardrugdeliveryin osteoarthritis.AdvDrugDelivRev.2006;58:226–42.
2.ZhangW,MoskowitzRW,NukiG,AbramsonS,AltmanRD, ArdenN,etal.OARSIrecommendationsforthemanagement ofhipandkneeosteoarthritis,PartII:OARSIevidence-based, expertconsensusguidelines.OsteoarthrCartil.2008;16: 137–62.
3.PourchoAM,SmithJ,WisniewskiSJ,SellonJL.Intraarticular platelet-richplasmainjectioninthetreatmentofknee osteoarthritis:reviewandrecommendations.AmJPhysMed Rehabil.2014;93:S108–21.
4.HarrisonS,VavkenP,KevyS,JacobsonM,ZurakowskiD, MurrayMM.Plateletactivationbycollagenprovidessustained releaseofanaboliccytokines.AmJSportsMed.
2011;39(4):729–34.
5.AhmadZ,HowardD,BrooksRA,WardaleJ,HensonF,Getgood A,etal.Theroleofplatelet-richplasmainmusculoskeletal science.JRSocMedShortRep.2012;3:40.
6.LacciKM,DardikA.Platelet-richplasma:supportforitsusein woundhealing.YaleJBiolMed.2010;83:1–9.
7.vanBuulGM,KoevoetWLM,KopsN,BosPK,VerhaarJAN, WeinansH,etal.Platelet-richplasmareleasateinhibits inflammatoryprocessesinosteoarthriticchondrocytes.AmJ SportsMed.2011;39:2362–70.
8.MixKS,SpornMB,BrinckerhoffCE,EyreD,SchurmanDJ. Novelinhibitorsofmatrixmetalloproteinasegeneexpression aspotentialtherapiesforarthritis.ClinOrthopRelatRes. 2004;427:129–37.
9.AnituaE,SánchezM,NurdenAT,ZalduendoMM,delaFuente M,AzofraJ,etal.Platelet-releasedgrowthfactorsenhance thesecretionofhyaluronicacidandinducehepatocyte growthfactorproductionbysynovialfibroblastsfrom arthriticpatients.Rheumatology.2007;46:
1769–72.
10.SchmidtMB,ChenEH,LynchSE.Areviewoftheeffectsof insulin-likegrowthfactorandplatelet-derivedgrowthfactor oninvivocartilagehealingandrepair.OstearthrCartil. 2005;14:403–12.
11.VendraminFS,FrancoD,FrancoTR.Métododeobtenc¸ãodo geldeplasmaricoemplaquetasautólogo.RevBrasCirPlást. 2009;24(2):212–8.
12.Sánchez-IlárduyaMB,TroucheE,TejeroR,OriveG,Reviakine I,AnituaE.Time-dependentreleaseofgrowthfactorsfrom implantsurfacestreatedwithplasmarichingrowthfactors.J BiomedMaterResA.2013;101(5):
1478–88.
13.MarxRE.Platelet-richplasma(PRP):whatisPRPandwhatis notPRP?ImplantDent.2001;10(4):225–8.
14.DeLongJM,RussellRP,MazzoccaAD.Platelet-richplasma:the PAWclassificationsystem.Arthroscopy.2012;28(7):
998–1009.
15.SakataJ,SasakiS,HandaK,UchinoT,SasakiT,HigashitaR, etal.Aretrospective,longitudinalstudytoevaluatehealing lowerextremitywoundsinpatientswithdiabetesmellitus andischemiausingstandardprotocolsofcareand platelet-richplasmagelinaJapanesewoundcareprogram. OstomyWoundManag.2012;58(4):36–49.
16.RabagoD,BestTM,ZgierskaAE,ZeisigE,RyanM,CraneD.A systematicreviewoffourinjectiontherapiesforlateral epicondylosis:prolotherapy,polidocanol,wholebloodand platelet-richplasma.BrJSportsMed.2009;43(7):
471–81.
17.PlachokovaAS,NikolidakisD,MulderJ,JansenJA,Creugers NH.Effectofplatelet-richplasmaonboneregenerationin dentistry:asystematicreview.ClinOralImplantsRes. 2008;19(6):539–45.
rev bras reumatol.2016;56(2):152–164
163
19.QiuJ,ZhangC,GuoY,YuanT,XieZ.ClinicalstudyonPRPin improvingbonerepair.ZhongguoXiuFuChongJianWaiKe ZaZhi.2009;23(7):784–7.
20.HuangQ,WangYD,WuT,JiangS,HuYL,PeiGX.Preliminary separationofthegrowthfactorsinplatelet-richplasma: effectsontheproliferationofhumanmarrow-derived mesenchymalstemcells.ChinMedJ(Engl).2009;122(1): 83–7.
21.KilianO,FleschI,WenischS,TaborskiB,JorkA,SchnettlerR, etal.Effectsofplateletgrowthfactorsonhuman
mesenchymalstemcellsandhumanendothelialcellsinvitro. EurJMedRes.2004;9(7):337–44.
22.FrazerA,BunningRA,ThavarajahM,SeidJM,RussellRG. StudiesontypeIIcollagenandaggrecanproductionin humanarticularchondrocytesinvitroandeffectsof transforminggrowthfactor-betaandinterleukin-1beta. OsteoarthrCartil.1994;2:235–45.
23.NakagawaK,SashoT,AraiM,KitaharaS,OginoS,WadaY. Effectsofautologousplatelet-richplasmaonthemetabolism ofhumanarticularchondrocytes.OsteoarthrCartil.
2007;15(2):134.
24.MishraA,TummalaP,KingA,LeeB,KrausM,TseV,etal. Bufferedplatelet-richplasmaenhancesmesenchymalstem cellproliferationandchondrogenicdifferentiation.Tissue EngPartCMethods.2009;15:431–5.
25.SánchezM,FizN,AzofraJ,UsabiagaJ,RecaldeEA,Gutierrez AG,etal.Arandomizedclinicaltrialevaluatingplasmarichin growthfactors(PRGF-endoret)versushyaluronicacidinthe short-termtreatmentofsymptomatickneeosteoarthritis. Arthroscopy.2012;28(8):1070–8.
26.VaquerizoV,PlasenciaMA,ArribasI,SeijasR,PadillaS,Orive G,etal.Comparisonofintra-articularinjectionsofplasma richingrowthfactors(PRGF-endoret)versusdurolane hyaluronicacidinthetreatmentofpatientswith
symptomaticosteoarthritis:arandomizedcontrolledtrial. Arthroscopy.2013;29(10):1635–43.
27.SayF,GürlerD,YenerK,BülbülM,Malkoc¸M.Platelet-rich plasmainjectionismoreeffectivethanhyaluronicacidinthe treatmentofkneeosteoarthritis.ActaChirOrthopTraumatol Cech.2013;80(4):278–83.
28.LiM,ChangqingZ,ZishengAI,TingY,YongF,WeitaoJIA. Therapeuticeffectivenessofintra-knee-articularinjectionof platelet-richplasmaonkneearticularcartilagedegeneration. ChinJReparReconstrSurg.2011;25(10):1192–6.
29.SpakováT,RosochaJ,LackoM,HarvanováD,GharaibehA. Treatmentofkneejointosteoarthritiswithautologous platelet-richplasmaincomparisonwithhyaluronicacid.Am JPhysMedRehabil.2012;91(5):411–7.
30.CerzaF,CarnS,CarcangiuA,VavoID,SchiavillaV,PecoraA, etal.Comparisonbetweenhyaluronicacidandplatelet-rich plasma,intra-articularinfiltrationinthetreatmentof gonarthrosis.AmJSportsMed.2012;40(12):
2822–7.
31.FilardoG,KonE,MartinoAD,MatteoBD,MerliML,Cenacchi A,etal.Platelet-richplasmavshyaluronicacidtotreatknee degenerativepathology:studydesignandpreliminaryresults ofarandomizedcontrolledtrial.MusculoskeletDisord. 2012;13:229.
32.KonE,MandelbaumB,BudaR,FilardoG,DelcoglianoM, TimonciniA,etal.Platelet-richplasmaintra-articular injectionversushyaluronicacidviscosupplementationas treatmentsforcartilagepathology:fromearlydegeneration toosteoarthritis.Arthroscopy.2011;27(11):
1490–501.
33.PatelS,DhillonMS,AggarwalS,MarwahaN,JainA. Treatmentwithplatelet-richplasmaismoreeffectivethan placeboforkneeosteoarthritis:aprospective,double-blind, randomizedtrial.AmJSportsMed.2013;41:356–64.
34.SánchezM,AnituaE,AzofraJ,AguirreJJ,AndiaI.
Intra-articularinjectionofanautologouspreparationrichin growthfactorsforthetreatmentofkneeOA:aretrospective cohortstudy.ClinExpRheumatol.2008;26(5):
910–3.
35.KonE,FilardoG,BudaE,TimonciniA,DiMartinoA,Cenacchi A,etal.Platelet-richplasma:intra-articularkneeinjections producedfavorableresultsondegenerativecartilagelesions. KneeSurgSportsTraumatolArthrosc.2010;18:
472–9.
36.FilardoG,KonE,BudaE,TimonciniA,DiMartinoA,Cenacchi A,etal.Platelet-richplasmaintra-articularkneeinjections forthetreatmentofdegenerativecartilagelesionsand osteoarthritis.KneeSurgSportsTraumatolArthrosc. 2010;19:528–35.
37.SampsonS,ReedM,SilversH,MengM,MandelbaumB. Injectionofplatelet-richplasmainpatientswithprimaryand secondarykneeosteoarthritis:apilotstudy.AmJPhysMed Rehabil.2010;89(12):961–9.
38.Wang-SaegusaA,CugatR,AresO,SeijasR,CuscóX,
Garcia-BalletbóM.Infiltrationofplasmarichingrowthfactors forosteoarthritisofthekneeshort-termeffectsonfunction andqualityoflife.ArchOrthopTraumaSurg.2011;131: 311–7.
39.NapolitanoM,MateraS,BossioM,CrescibeneA,CostabileE, AlmollaJ,etal.Autologousplateletgelfortissueregeneration indegenerativedisordersoftheknee.BloodTransfus. 2012;10:72–7.
40.SánchezM,GuadillaJ,FizN,AndiaI.Ultrasound-guided platelet-richplasmainjectionsforthetreatmentof osteoarthritisofthehip.Rheumatology.2012;51: 144–50.
41.JangSJ,KimJD,ChaSS.Platelet-richplasma(PRP)injections asaneffectivetreatmentforearlyosteoarthritis.EurJOrthop SurgTraumatol.2013;23:573–80.
42.BattagliaM,GuaraldiF,VanniniF,BuscioTR,GallettiS, GianniniS.Platelet-richplasmaintra-articular
ultrasound-guidedinjectionsasapossibletreatmentforhip osteoarthritis:apilotstudy.ClinExpRheumatol.
2011;29(4):754.
43.HalpernB,ChaudhuryS,RodeoSA,HayterC,BognerE,Potter HG,etal.ClinicalandMRIoutcomesafterplatelet-rich plasmatreatmentforkneeosteoarthritis.ClinJSportMed. 2013;23:238–9.
44.GobbiA,KarnatzikosG,MahajanV,MalchiraS.Platelet-rich plasmatreatmentinsymptomaticpatientswithknee osteoarthritis:preliminaryresultsingroupofactivepatients. SportsHealth.2012;4:162.
45.HartR,SafiA,KomzakM,JajtnerP,PuskeilerM,HartovaP. Platelet-richplasmainpatientswithtibiofemoralcartilage degeneration.ArchOrthopTraumaSurg.2013;133: 1295–301.
46.FilardoG,KonE,RuizMTP,VaccaroF,GuitaldiR,DiMartinoA, etal.Platelet-richplasmaintra-articularinjectionsfor cartilagedegenerationandosteoarthritis:single-versus double-spinningapproach.KneeSurgSportsTraumatol Arthrosc.2011;20:2082–91.
47.DhollanderAAM,DeNeveF,AlmqvistKF,VerdonkR, LambrechtS,ElewautD,etal.Autologousmatrix-induced chondrogenesiscombinedwithplatelet-richplasmagel: technicaldescriptionandafivepilotpatientsreport.Knee SurgSportsTraumatolArthrosc.2011;19:
536–42.
49.ChangK-V,HungC-Y,AliwargaF,WangT-G,HanD-S, ChenW-S.Comparativeeffectivenessofplatelet-richplasma injectionsfortreatingkneejointcartilagedegenerative pathology:asystematicreviewandmeta-analysis.ArchPhys MedRehabil.2014;95:562–75.
50.KhoshbinA,LerouxT,WassersteinD,MarksP,