SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Original
article
Subchondroplasty
for
treating
bone
marrow
lesions
in
the
knee
–
initial
experience
夽
Marcelo
Batista
Bonadio
a,∗,
Pedro
Nogueira
Giglio
a,
Camilo
Partezani
Helito
a,
José
Ricardo
Pécora
b,
Gilberto
Luis
Camanho
b,
Marco
Kawamura
Demange
baUniversidadedeSãoPaulo,InstitutodeOrtopediaeTraumatologia,GrupodeJoelho,SãoPaulo,SP,Brazil
bUniversidadedeSãoPaulo,FaculdadedeMedicina,DepartamentodeOrtopediaeTraumatologia,SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received22June2016 Accepted18July2016 Availableonline28April2017
Keywords: Bonecements
Bonesubstitutes/administration& dosage
Bonemarrow/injuries Edema
a
b
s
t
r
a
c
t
Objective:Toevaluatetheuseofsubchondroplastyinthetreatmentofbonemarrowlesions inaninitialseriesoffivecases.
Methods:Thestudyincludedpatientsagedbetween40and75yearsold,withpaininthe kneeforatleastsixmonths,associatedwithhigh-signalMRIlesiononT2sequences,on thetibiaorfemur.PatientswereassessedusingthevisualanalogpainscaleandtheKOOS score,oneweekbeforesurgeryandone,three,six,12,and24weeksaftertheprocedure. Subchondroplastywasperformedwithatechniquedevelopedforfillingtheareaofthebone marrowlesionwithacalciumphosphatebonesubstitute.
Results:Thefillingwasperformedonthemedialfemoralcondyleinfourpatientsandmedial tibialplateauinonecase.Theassessment bytheKOOSscorepresenteda preoperative averageof38.44pointsand62.7,58.08,57.92,63.34,and71.26pointswithone,three,six,12, and24weeksaftersurgery,respectively.IntheevaluationbytheVAS,theaveragewas7.8 pointspreoperativelyand2.8,3,2.8,1.8,and0.6pointsoverthesameperiods.Allpatients wereabletoambulatewithoutadditionalsupport,onthefirstdayaftertheprocedure.One patienthadaminimalgraftdislocationtothesofttissue,withlocalpain,whichresolved completelyafteraweek.
Conclusion: The subchondroplasty technique provided significant improvements in the parametersofpainandfunctionalcapacityintheshort-termassessment.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
夽
StudyconductedattheUniversidadedeSãoPaulo,FaculdadedeMedicina,HospitaldasClínicas,InstitutodeOrtopediae Trauma-tologia,GrupodeJoelho,SãoPaulo,Brazil.
∗ Correspondingauthor.
E-mail:bonadio@usp.br(M.B.Bonadio). http://dx.doi.org/10.1016/j.rboe.2017.04.003
Cimentosparaossos Substitutos
ósseos/administrac¸ão& dosagem
Medulaóssea/lesões Edema
ósseasemsérieinicialdecincocasos.
Métodos: Oestudoincluiupacientesentre40e75anos,comdoremjoelhocompelomenos seismesesdedurac¸ão,associadaàressonânciamagnéticacomlesãohipercaptanteem ponderac¸ãodeT2natíbiaounofêmur.Ospacientesforamavaliadossegundoaescala visualanalógicadedor(EVA)epeloKneeInjuryandOsteoarthritisOutcomeScore(KOOS),uma semanaantesdacirurgiaeuma,três,seis,12e24semanasapós.Asubcondroplastiafoi feitacomtécnicadesenvolvidaparaopreenchimento,guiadoporradioscopia,daáreade lesãoósseamedular,comousodesubstitutoósseoempastaàbasedefosfatodecálcio. Resultados: Opreenchimentofoifeitocomsucessoemtodososcasos,quatronocôndilo femoralmedialeum noplanaltotibialmedial.Aavaliac¸ãopelo KOOSapresentouuma médiapré-operatóriade38,44pontose62,7,58,08,57,92,63,34e71,26pontoscomuma, três,seis,12e24semanasapósacirurgia,respectivamente.Naavaliac¸ãopelaEVA,amédia foide 7,8pontosnopré-operatórioe2,8,3, 2,8,1,8e0,6pontosnosmesmosperíodos. Todosospacientesconseguiramdeambular,semapoioadicional,jánoprimeirodiaapós oprocedimento.Umpacienteapresentoumínimoextravasamentodeenxertoparapartes moles,causoudorlocalqueseresolveucompletamenteapósumasemana.
Conclusão: Atécnicadesubcondroplastiadesenvolvidaproporcionoumelhorias significa-tivasnosparâmetrosdedorecapacidadefuncionalnaavaliac¸ãodecurtoprazo.
©2016SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Osteoarthritis of the knee is currently accepted as a dis-ease that affects the entire joint. It is interpreted as a multifactorial process involving cartilage, bone, menis-cus, ligaments, synovial tissue, and musculature; it is difficult to define how much each of these factors con-tributes to each case. Changes in subchondral bone are currentlyrecognizedasanimportantfactorinthisarthritic process.1,2
Bone marrow lesions (BMLs) characterizedby increased signal on T2-weighted sequences with fat suppression on magneticresonance imaging (MRI),known as bone edema lesions, indicate a mechanically and histologically altered subchondralbone. Suchlesions have been related topain, joint surface deformation, and accelerated osteoarthritis progression.3–6 Histological evaluations of these lesions demonstratethatthesearenotedemaareasperse,butrather asetofnonspecificchangesinvolvingfibrosis,medullaryfat necrosis,microfracturesofthetrabecularbone,andpoor min-eralization,confirmingthehypothesis ofareasofexcessive boneremodelingwithouttheabilitytoformbonewithnormal characteristics.7,8
Studies on natural history of arthritis demonstrate an acceleratedprogressionto totalknee arthroplasty (TKA) in patientswithBML,9whoareuptoninetimesmorelikelyto undergoTKAinthreeyears.10Thereisthereforeaninterestin therapiesdirectedtowardthesubchondralbonethataimon preservingthejoint.
Theuseofsodiumalendronateandstrontiumranelatehas beeninvestigatedasanoption,buttheresultsregardingthe controlofdiseaseprogressionaredivergent.11–14
Subchondroplastyconsistsoftheapplicationofasynthetic bonesubstitutebasedoncalciumphosphateintheBMLforthe treatmentoflesionsinwhichconservativetreatmentfailed. Thegoalistoimprovethestructuralqualityoftheaffected subchondralboneandpromotelocalboneremodeling,aiming topreventbonecollapseandtheprogressionofarthritis.15,16
Previous reports in the literature have demonstrated the feasibility and applicability of the technique to reduce pain and improve function, with a small risk of complications.17 However, this is the first study to assess the reproducibilityofthe subchondroplastytechniquewith a differentsystem andbonesubstitute, outside theUnited States.
Thus, the authors present the evaluation of the initial resultsofthe treatmentofBMLwithsubchondroplasty,the applicabilityandviabilityofthesurgicaltechniqueinBrazil, andtheinitialfunctionalresults.
Material
and
methods
Thisstudy wasapprovedbythe InstitutionalReviewBoard underNo.859.206.
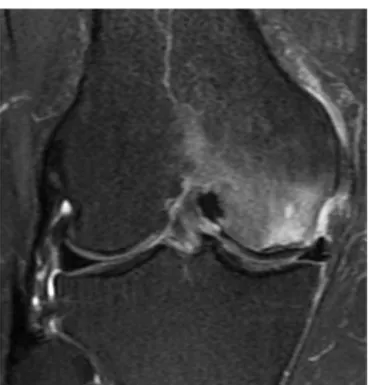
Fig.1–Bonemedullarylesioninmedialfemoralcondyle, withhypersignalonT2-weightedmagneticresonance image.
Theexclusioncriteriawere:autoimmunediseases,renal diseaserequiringdialysis,osteoarthritisradiographically clas-sified in the Kellgren–Lawrence system18 as greater than grade3,diversionofthemechanicalalignmentofthelower limbslargerthan8degrees,orradiographicalterationsofthe patellofemoral joint associated with symptoms ofanterior painintheknee.
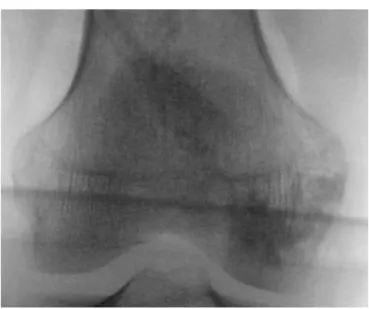
MRI images were analyzed using the iSite PACS server (Philips,Amsterdam,Netherlands).Lesionsweremappedand measured in the axial, coronal, and sagittal views toplan theinjectionsiteandthetrajectoryofthecannulausedfor theprocedure.Radiographsusinganteroposterior,profile,and Rosenbergviewsofthekneeandlowerlimbwereperformed toclassifythelesionaccordingtotheKellgren–Lawrence clas-sificationandtoassesslowerlimbalignment.
Patientswereassessedoneweekpriortotheprocedureand one,three,six,12,and24weeksafterit,usingtheKOOSand thevisualanalogscale(VAS)forpain.
Descriptionofthesurgicaltechnique
Aftermapping,patientsunderwentthesubchondroplasty pro-cedure, which was performed under spinal anesthesia, in anoperatingroom,afterconventionalpreppingtechniques. Patientswereplacedondorsalpositioningonaradiolucent table,withacushionundertheipsilateralhipforbetter con-troloftheexternalrotationofthelimb.Anothercushionwas alsopositionedunderthekneetobeoperated,aidinginthe lateralincidenceoffluoroscopyandavoidinganoverlapwith theimageofthecontralateralknee.Accordingtopreoperative planning,thecannulaentrypointwasdemarcatedwiththe aidoffluoroscopyinfrontandprofileviews.Thecannulawas
Fig.2–Imageofintraoperativeradioscopy,withcannula positioninginalesionmappedusingmagneticresonance imaging.
thenintroduced,withfluoroscopycontrol,towardthe previ-ouslydeterminedcenterofthelesion(Fig.2).Progressionwas performedmanuallyorwiththeuseofasurgicalmallet.
Thepastebonesubstitute(graft)wasthenprepareduntil it reachedliquid/pasty viscosity,and subsequently injected into theaffectedregion.Throughfluoroscopy,wewereable tovisualizethedistributionoftheproductinthebone mar-row,ensuringthattheapplicationfollowedthelesionmapping (Fig. 3). Graftys HBS® (Graftys, Aix en Provence, France) (ANVISA:80517190001)wasused.
The patients were hospitalized and discharged on the first postoperative day. After the procedure, patients were allowedtofullweightbearingastolerated,withfreerange ofmotion.Duringhospitalization,patientsreceivedanalgesia withdipyrone1gintravenouslyeverysixhourscombinedwith tramadol100mgintravenouslyeveryeighthours,ondemand iftheyindicatedpainhigherthan6onVAS.Afterhospital dis-charge,patientsreceivedanalgesiawithoraldipyrone4gdaily (1geverysixhours)forsevendays.
Statisticalanalysis
Thequantitativevalueswithnormaldistribution(parametric) wereanalyzedbyStudent’st-test;thosewithnonparametric distributionwereanalyzedusingtheMann–Whitneytest.
Results
Fig.3–Imageofintraoperativeradioscopy,with radiopacityafterfillingbysubchondroplasty,inaregion mappedusingmagneticresonanceimaging.
Fivepatients were prospectivelyevaluated, fourfemales andonemale,withamean of67.7 (±9.67)years;they pre-sented pain in one knee for at least six months, after a minimumofthreemonthsofconservativetreatmentwithout improvement.AllpatientshadaMRIscanwitha hypercap-tatinglesion inT2-weightedfat-suppression imagesinthe subchondralregionofthetibialplateauorfemoralcondyles.
Fillingwithbonesubstitutewasperformedinthemedial femoral condyle in four patients and in the medial tibial plateauinonecase.
Three patients were radiographically classified as Kellgren–Lawrence grade II and two grade patients as
gradeI. None of the patients presentedlesion or previous
surgeryintheevaluatedknee(Table1).
EvaluationusingtheKOOSshowedameantotalscorein thepreoperativeperiodof38.44pointsandof62.7(p<0.05), 58.08 (p<0.05), 57.92 (p<0.05), 63.34 (p<0.07), and 71.26 (p<0.05) points at one, three, six, 12, and 24 weeks after surgery,respectively.Inthe VASassessment,mean was7.8 pointspreoperativelyand2.8(p<0.05),3(p<0.05),2.8(p<0.05), 1.8 (p<0.05), and 0.6 (p<0.05) points in the same periods (Fig.4).
One of the patients had a minimal amount of graft extravasatedintothesofttissue,upontheintroductionofthe cannula;localpainwasobservedforoneweek,andresolved
Table1–Detailofthecasesthatunderwent
subchondroplasty:age,sex,laterality,lesiontopography, andKellgren–Lawrenceclassificationoftheradiograph.
Patient Age Sex Side Topographyof
thelesion
Kellgren-Lawrence
1 61 F R Femoralmedial I
2 69 M L Tibialmedial II
3 58 F L Femoralmedial II
4 85 F L Femoralmedial I
5 70 F R Femoralmedial II
5
4
3
2
1
0
Pre 1 Week 3 Week 6 Week 12 Week 24 Week
Fig.4–Meanvisualanalogscale(VAS)painpreoperatively (pre)andone,three,six,12,and24weeksafter
subchondroplasty.
completelyafterthisperiod.Theradiographicfollow-upalso demonstratedaprogressiveresorptionoftheproduct,which aftersixmonthsofsurgerywasstillpartiallyidentifiableon radiography.Nopatientrequiredadditionalproceduresduring follow-up.
Allpatientswereabletowalk,withoutadditionalsupport, onthefirstdayaftertheprocedure.
Discussion
Themainfindingofthepresentstudywasthatpatientswho underwentsubchondroplastyshowedasignificant improve-ment in functional capacity from the first week post procedure, which persistedin the subsequent six months. There was also asignificant and quick pain improvement, whichalsocontinuedduringthesixmonthsoffollow-up.
Osteoarthritisisadiseasecharacterizedbywearofhyaline cartilage; however,as thistissuedoes nothavenerve pain fibers, thecause ofthe pain isstillnot completelyclear.19 Nonetheless,painreceptorsarefoundinseveralother struc-tures affectedbythe pathological processofosteoarthritis, suchasjointcapsule,ligamentssurroundingtheknee,andthe peripheralportionofthemeniscus.Theperiosteumandbone marrowarealsorichlyinnervatedbynociceptivereceptors.4
Studies have shown that the presence ofBML insome patientswithosteoarthritisisassociatedwithpain, disease progression,jointdeformation,andrapidprogressionto treat-mentwitharthroplasty.3,5,10
Calciumphosphate-basedbonesubstitutehasbeenused primarily as a graft option in bone defects.20–22 For this function, biphasic calcium phosphate ceramics show good osteoinductiveandosteoconductiveresults.23,24Such proper-tiesmaycontributetothebalanceofthebonemineralization thatwaslostintheareasofBML,andmaymodifythecourseof thedisease.Unlikehydroxyapatite,whichpresentsaverylong reabsorptiontime,thedegradationofbiphasiccalcium phos-phateceramicsismoresimilartothatofautologousbone.25
anosteotomyinordertoreducetheoverloadoftheaffected compartment.
Thepresentstudydemonstratedasimpleandreproducible surgicaltechnique,whichsucceededinitsobjectiveof inject-ingcalcium-phosphate-basedbonesubstituteintoBMLareas. Theonlycomplication observedduring the study, extrava-sation of the bone substitute, did not lead to significant consequencesforthepatient.Asignificantreductionofpain, assessed by VAS, and KOOS improvement after subchon-droplastywerealsoevidenced.
Thesmallnumberofpatientsandtheabsenceofcontrol groupareimportantlimitationsofthepresentstudy,which reportsaninitialexperienceoverastillshort-termfollow-up period.Alargerstudy,withalong-termfollow-up,is under-way. Nevertheless, the present study is pioneering in the developmentand presentationofthesurgical techniqueof subchondroplastyintheBrazilianliterature.
Conclusion
Thedevelopedsubchondroplastytechniqueissafe,providing significantimprovementsinpainparametersandfunctional capacityintheshort-termevaluation.Subocondroplastymay bea newtreatment modality for early stageosteoarthritis whenanassociatedbonemarrowlesionispresent.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. MadryH,vanDijkCN,Mueller-GerblM.Thebasicscienceof thesubchondralbone.KneeSurgSportsTraumatolArthrosc. 2010;18(4):419–33.
2. OrthP,CucchiariniM,WagenpfeilS,MengerMD,MadryH. PTH[1-34]-inducedalterationsofthesubchondralbone provokeearlyosteoarthritis.OsteoarthritisCartilage. 2014;22(6):813–21.
3. FelsonDT,ChaissonCE,HillCL,TottermanSM,GaleME, SkinnerKM,etal.Theassociationofbonemarrowlesions withpaininkneeosteoarthritis.AnnIntMed.
2001;134(7):541–9.
4. SowersMF,HayesC,JamadarD,CapulD,LachanceL, JannauschM,etal.Magneticresonance-detected
subchondralbonemarrowandcartilagedefectcharacteristics associatedwithpainandX-ray-definedkneeosteoarthritis. OsteoarthritisCartilage.2003;11(6):387–93.
5. RoemerFW,GuermaziA,JavaidMK,LynchJA,NiuJ,ZhangY, etal.ChangeinMRI-detectedsubchondralbonemarrow lesionsisassociatedwithcartilageloss:theMOSTStudy.A longitudinalmulticentrestudyofkneeosteoarthritis.Ann RheumDis.2009;68(9):1461–5.
6. KrausVB,FengS,WangS,WhiteS,AinslieM,GraverandMP, etal.Subchondralbonetrabecularintegritypredictsand changesconcurrentlywithradiographicandmagnetic resonanceimaging-determinedkneeosteoarthritis progression.ArthritisRheum.2013;65(7):1812–21. 7. KazakiaGJ,KuoD,SchoolerJ,SiddiquiS,ShanbhagS,
BernsteinG,etal.Boneandcartilagedemonstratechanges localizedtobonemarrowedema-likelesionswithin
osteoarthriticknees.OsteoarthritisCartilage. 2013;21(1):94–101.
8.TaljanovicMS,GrahamAR,BenjaminJB,GmitroAF,Krupinski EA,SchwartzSA,etal.Bonemarrowedemapatternin advancedhiposteoarthritis:quantitativeassessmentwith magneticresonanceimagingandcorrelationwithclinical examination,radiographicfindings,andhistopathology. SkeletalRadiol.2008;37(5):423–31.
9.TanamasSK,WlukaAE,PelletierJP,PelletierJM,AbramF, BerryPA,etal.Bonemarrowlesionsinpeoplewithknee osteoarthritispredictprogressionofdiseaseandjoint replacement:alongitudinalstudy.Rheumatology. 2010;49(12):2413–9.
10.ScherC,CraigJ,NelsonF.Bonemarrowedemainthekneein osteoarthrosisandassociationwithtotalkneearthroplasty withinathree-yearfollow-up.SkeletalRadiol.
2008;37(7):609–17.
11.ShiraiT,KobayashiM,NishitaniK,SatakeT,KurokiH, NakagawaY,etal.Chondroprotectiveeffectofalendronatein arabbitmodelofosteoarthritis.JOrthopRes.
2011;29(10):1572–7.
12.ReginsterJY,BadurskiJ,BellamyN,BensenW,ChapurlatR, ChevalierX,etal.Efficacyandsafetyofstrontiumranelatein thetreatmentofkneeosteoarthritis:resultsofa
double-blind,randomisedplacebo-controlledtrial.AnRheum Dis.2013;72(2):179–86.
13.PelletierJP,RoubilleC,RaynauldJP,AbramF,DoraisM, DelormeP,etal.Disease-modifyingeffectofstrontium ranelateinasubsetofpatientsfromthePhaseIIIknee osteoarthritisstudySEKOIAusingquantitativeMRI:reduction inbonemarrowlesionsprotectsagainstcartilageloss.Ann RheumDis.2015;74(2):422–9.
14.HayamiT,PickarskiM,WesolowskiGA,McLaneJ,BoneA, DestefanoJ,etal.Theroleofsubchondralboneremodelingin osteoarthritis:reductionofcartilagedegenerationand preventionofosteophyteformationbyalendronateintherat anteriorcruciateligamenttransectionmodel.Arthritis Rheum.2004;50(4):1193–206.
15.SharkeyPF,CohenSB,LeinberryCF,ParviziJ.Subchondral bonemarrowlesionsassociatedwithkneeosteoarthritis.Am JOrthop.2012;41(9):413–7.
16.FarrJ,CohenSB.Expandingapplicationsofthe subchondroplastyprocedureforthetreatmentofbone marrowlesionsobservedonmagneticresonanceimaging. OperTechnSportMed.2013;21(2):138–43.
17.CohenSB,SharkeyPF.Subchondroplastyfortreatingbone marrowlesions.JKneeSurg.2016;29(7):555–63.
18.KellgrenJH,LawrenceJS.Radiologicalassessmentof osteo-arthrosis.AnnRheumDis.1957;16(4): 494–502.
19.Ulrich-VintherM,MaloneyMD,SchwarzEM,RosierR,O’Keefe RJ.Articularcartilagebiology.JAmAcadOrthopSurg. 2003;11(6):421–30.
20.EvaniewN,TanV,ParasuN,JurriaansE,FinlayK,DeheshiB, etal.Useofacalciumsulfate-calciumphosphatesynthetic bonegraftcompositeinthesurgicalmanagementofprimary bonetumors.Orthopedics.2013;36(2):e216–22.
21.KimJK,KimNK.Curettageandcalciumphosphatebone cementinjectionforthetreatmentofenchondromaofthe finger.HandSurg.2012;17(1):65–70.
22.WingeMI,ReikerasO,RokkumM.Calciumphosphatebone cement:apossiblealternativetoautologousbonegraft.A radiologicalandbiomechanicalcomparisoninrattibialbone. ArchOrthopTraumaSurg.2011;131(8):1035–41.
23.SurmenevRA,SurmenevaMA,IvanovaAA.Significanceof calciumphosphatecoatingsfortheenhancementofnew boneosteogenesis–areview.ActaBiomater.