w w w . r b o . o r g . b r
Case
Report
Pelvic
pseudotumor
following
total
hip
arthroplasty
–
case
report
夽,夽夽
Nelson
Franco
Filho
a,b,
Alexandre
de
Paiva
Luciano
a,b,∗,
Bruno
Vierno
baDepartmentofMedicine,UniversidadedeTaubaté(UNITAU),Taubaté,SP,Brazil
bOrthopedicsandTraumatologyService,UniversityHospitalofTaubaté,Taubaté,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received18September2013 Accepted7October2013
Availableonline18September2014
Keywords:
Plasmacellgranuloma Hiparthroplasty Pelvicneoplasms
a
b
s
t
r
a
c
t
Looseningisawell-knowncomplicationoftotalhiparthroplasty.Theaccumulationof detri-tusresultingfrommechanicalwearformsinflammatorycellsthathavethefunctionof phagocytizingthisdebris.Overthelongterm,thesecellsmaygiverisetoalocal granulo-matousreaction.Here,wepresentareportonacaseofpelvicpseudotumorsubsequent tototalhiparthroplasty,whichisconsideredrareintheliterature.Thepatientwasa 48-year-oldblackmanwhostartedtobefollowedupmedicallyeightmonthsearlierbecause ofuncharacteristicabdominalpains,dysuriaandpollakiuria.Hehadundergonelefttotal hiparthroplasty17 yearspreviously.Throughclinicalinvestigation andcomplementary examinations,anextra-articulargranulomatousmasswasdiagnosed,constitutingapelvic pseudotumor.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.Allrightsreserved.
Pseudotumor
de
pelve
pós-artroplastia
total
do
quadril
–
relato
de
caso
Palavras-chave:
Granulomadecélulasplasmáticas Artroplastiadequadril
Neoplasiaspélvicas
r
e
s
u
m
o
Asoltura éumacomplicac¸ãobemconhecidanasartroplastiastotaisdoquadril.O acú-mulodedetritosresultantedodesgastemecânicoformacélulasinflamatóriasquetêma func¸ãodefagocitaressesdetritosepodem,emlongoprazo,gerarumareac¸ãogranulomatosa
local. A seguir, apresentamos um relato de caso de pseudotumor de pélvis
pós-artroplastiatotaldoquadril,consideradoraronaliteraturaconsultada.Trata-sedepaciente
夽
Pleasecitethisarticleas:FrancoFilhoN,dePaivaLucianoA,ViernoB.Pseudotumordepelvepós-artroplastiatotaldoquadril–relato decaso.RevBrasOrtop.2014;49(5):543–9.
夽夽
WorkdevelopedintheDisciplineofOrthopedicsandTraumatology,DepartmentofMedicine,UniversidadedeTaubaté,andinthe OrthopedicsandTraumatologyService,UniversityHospitalofTaubaté,Taubaté,SP,Brazil.
∗ Correspondingauthor.
E-mail:alexandrepaiva76@ig.com.br(A.dePaivaLuciano).
http://dx.doi.org/10.1016/j.rboe.2013.10.001
544
rev bras ortop.2014;49(5):543–549de48anos,masculino,negro,queiniciouseguimentomédicopordoresabdominais incar-acterísticas,disúriaepolaciúriahaviaoitomeses.Apresentavaartroplastiatotaldoquadril esquerdohavia17anos.Apósinvestigac¸ãoclínicaepormeiodeexamescomplementares, diagnosticou-seumamassagranulomatosaextra-articular,pseudotumordepélvis.
©2014SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Todososdireitosreservados.
Introduction
Looseningisawell-knowncomplicationoftotalhip
arthro-plasty.Theaccumulationofdetritusfrom mechanicalwear
formsinflammatorycellsthathavethefunctionof phagocy-tizingthisdetritus.However,overthelongterm,formationof thesecellsmayresultinagranulomatousreaction.Thishas theeffectofcreatinganabnormaladditionaljointmassand mayleadtoatypicaljointorabdominalsymptoms.
Inthefollowing,wereportacaseoflooseningofan unce-mentedprosthesisinwhichanextra-articulargranulomatous masscomprisingapelvicpseudotumordeveloped.Inthe lit-erature,thisconditionisconsideredtoberare.
Description
of
the
clinical
condition
The patient was a 48-year-old black man who started to
undergomedicalfollow-upbecauseofabdominalpain irra-diatinguncharacteristicallytothelefthip,alongwithdysuria andpollakiuria,whichhehadhadforeightmonths.Hehad undergonetotalhiparthroplasty17yearsearlier.
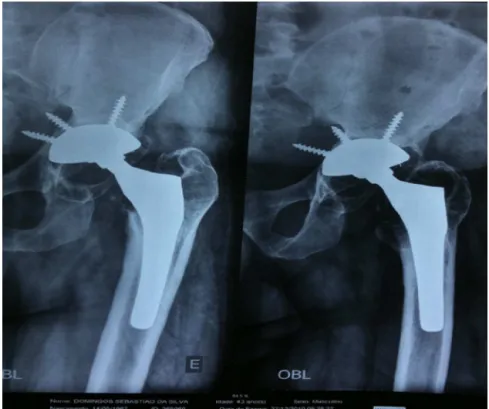
Fig.1–Radiographsofthelefthipinanteroposteriorandobliqueviews(December27,2010)showingtotalarthroplasty performed17yearsearlier.
At a consultationwith an urologist, no irregularities or alterationswerefoundthroughdigitalrectalexamination.The patientunderwentaprostatebiopsy,whichdidnotshowany neoplasticalterations.
Intheorthopedicphysicalexaminationonadmission,the patientpresentedthefollowing:
• Inspection:nogaitabnormalities;presenceofasurgicalscar
intheposterolateralregionofthelefthip;
• Bonepalpation:nopainintheleftorrighthip;
• Rangeofmotionofthelefthip:flexionof90◦,extensionof 20◦,abductionof25◦,adductionof15◦,internalrotationof 20◦andexternalrotationof15◦;
• Sensitivitypresentandnoalterationstothelowerlimbs;
• MusclestrengthofgradeVinbothlowerlimbs;
• Peripheralpulsepresentandfullinthelowerlimbs;
• Aftertheorthopedicclinicalexamination,aninvestigation
usingimagingexaminationswasconducted(Figs.1–3).
Withtheaidoftheimagingexaminations,surgical treat-mentwasthenproposed,withinterventionbytwospecialists
Fig.2–Echographicimagesoftheurinarytractandprostateshowingmassofcysticappearanceclosetothebladder.
546
rev bras ortop.2014;49(5):543–549Tensor fasciae latae
Gluteus maximus muscle
Gluteus medius muscle Vastus lateralis muscle
C
A
B
Fig.4–Detailofthesurgicalprocedureforrevisionoftotalhiparthroplastyandresectionofthetumoralmass.
performdecompressionandresectionofthemass;andfrom the joint reconstruction group to perform revision of the left-side total hip arthroplasty. These surgical procedures werecarriedoutinFebruary2011(Figs.4and5).
Afterthesurgicalresectiondescribedabove,thediagnosis
wasconfirmedbymeansofanatomopathological
examina-tion,whichshowedthepresenceofgranulomatoustissuewith absenceofneoplasticorinfectiouscells.
Eightmonthsaftertheoperation,controlradiographsof therevisionoftheleft-sidetotalhiparthroplastyin anteropos-teriorandlateralviewsandcontrolechographsoftheurinary tractandprostatewereproduced.Thesewerewithinnormal patternsanddemonstratedthattherehadnotbeenany recur-renceofthecyst(Figs.6and7).
Discussion
Clinical and radiographic signs of induced osteolysis are
frequently seen in relation to hip prostheses, and these
complicationsarewell-knownamonghipsurgeons.However,
a less commoncomplication may accompanysuchevents:
presenceofamassofsymptomaticsofttissue.Inourcase, thepatientpresentedinitialsymptomsrelatingtourological alterations,withoutsignsorsymptomsinthehipjoint.
Detritusresultingfromlooseningorwearisusually
phago-cytized bymacrophagesand inflammatorycells.In certain
situations,anaggressivegranulomatousreactionmayoccur, with the characteristics ofa foreign body. Thisreaction is characterized clinically by formation of progressive cysts
that generate symptomatic masses in the pelvis.1,2
San-tavirta et al.3 suggested that this granulomatosis would
involve decouplingofthenormalsequence of
“monocytes-macrophages-clearance”,mediatedbyforeignmaterialsand
tissue detritus, which is normally followed by fibroblasts. SchmalzriedandCallaghan4reportedthatthisaggressivelysis couldoccuratanypointalongthespaceofthehipjoint.A defectinthejointcapsuleorabonedefectmayresultin her-niationorinpropagationofthisspacetotheextra-articular
ESQ
ESQ
ESQ
ESQ
Fig.6–Postoperativecontrolradiographsinanteroposteriorandlateralviews,producedeightmonthsafterrevisionofthe left-sidetotalhiparthroplasty.
548
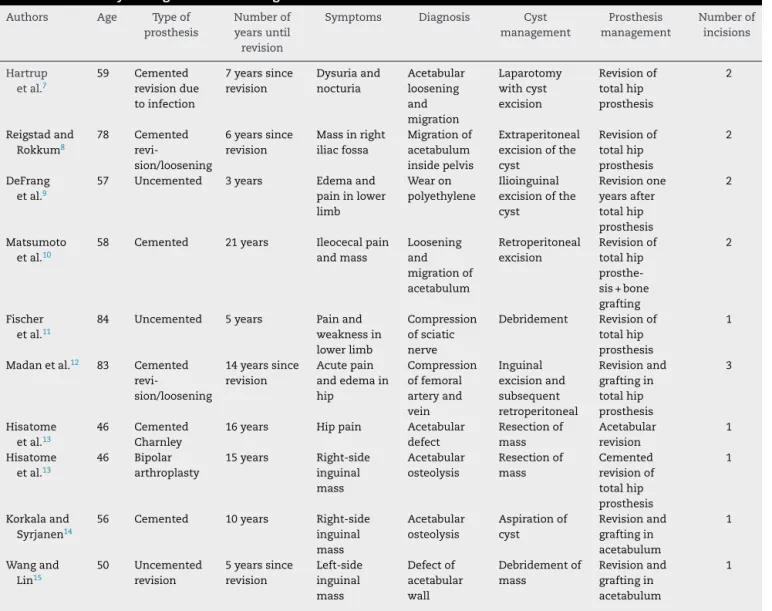
rev bras ortop.2014;49(5):543–549Table1–Summaryofdiagnosesandmanagementofsimilarcases.
Authors Age Typeof prosthesis
Numberof yearsuntil revision
Symptoms Diagnosis Cyst management Prosthesis management Numberof incisions Hartrup etal.7
59 Cemented
revisiondue toinfection
7yearssince revision Dysuriaand nocturia Acetabular loosening and migration Laparotomy withcyst excision Revisionof totalhip prosthesis 2 Reigstadand Rokkum8 78 Cemented revi-sion/loosening
6yearssince revision
Massinright iliacfossa
Migrationof acetabulum insidepelvis
Extraperitoneal excisionofthe cyst Revisionof totalhip prosthesis 2 DeFrang etal.9
57 Uncemented 3years Edemaand
paininlower limb
Wearon polyethylene
Ilioinguinal excisionofthe cyst Revisionone yearsafter totalhip prosthesis 2 Matsumoto etal.10
58 Cemented 21years Ileocecalpain
andmass Loosening and migrationof acetabulum Retroperitoneal excision Revisionof totalhip prosthe-sis+bone grafting
2
Fischer etal.11
84 Uncemented 5years Painand
weaknessin lowerlimb
Compression ofsciatic nerve
Debridement Revisionof
totalhip prosthesis
1
Madanetal.12 83 Cemented
revi-sion/loosening
14yearssince revision
Acutepain andedemain hip Compression offemoral arteryand vein Inguinal excisionand subsequent retroperitoneal Revisionand graftingin totalhip prosthesis 3 Hisatome etal.13
46 Cemented
Charnley
16years Hippain Acetabular
defect Resectionof mass Acetabular revision 1 Hisatome etal.13
46 Bipolar
arthroplasty
15years Right-side
inguinal mass Acetabular osteolysis Resectionof mass Cemented revisionof totalhip prosthesis 1 Korkalaand Syrjanen14
56 Cemented 10years Right-side
inguinal mass Acetabular osteolysis Aspirationof cyst Revisionand graftingin acetabulum 1 Wangand Lin15 50 Uncemented revision
5yearssince revision Left-side inguinal mass Defectof acetabular wall Debridementof mass Revisionand graftingin acetabulum 1
TranslatedandadaptedfromLeighW,O’GradyP,LawsonEM,HungNA,TheisJC,MathesonJ.Pelvicpseudotumor:anunusualpresentationof anextra-articulargranulomainawell-fixedtotalhiparthroplasty.JArthroplasty.2008;23(6):934–8.
region.5,6 Inourpatient,thismasswasconcentratedinthe extra-articularspace.Granulomatousmassesofthisnaturein
thepelvismaybesymptomaticorasymptomatic.Theymay
beidentifiedduringroutineinvestigationsforotherreasons ormaybecomeevidentduringthepreoperativeinvestigations forhiprevisionsurgery.7Inourpatient,revisionofthe pros-thesiswasindicatedonlyforremovalofthecyst.Thelesion
may causesymptoms, resulting from pressureon adjacent
structures,whichdidnotoccurinthispatient.Inthiscase,
thepelvicmasscausedabdominalpainswith
uncharacter-isticirradiationtothelefthip,accompaniedbydysuriaand pollakiuria.
Forthepurposesofmakingcomparisonswiththepresent case,Table1showsasummaryofdiagnosesandmanagement approachesusedinsimilarcases.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.ZicatB,EnghCA,GokcenE.Patternsofosteolysisaroundtotal hipcomponentsinsertedwithandwithoutcement.JBone JointSurgAm.1995;77(3):432–9.
2.JacobsJJ,ShanbhagA,GlantTT,BlackJ,GalanteJO.Wear debrisintotaljointreplacements.JAmAcadOrthopSurg. 1994;2(4):212–20.
3.SantavirtaS,KonttinenYT,BergrothV,EskolaA,TallrothK, LindholmTS.Aggressivegranulomatouslesionsassociated withhiparthroplasty:immunopathologicalstudies.JBone JointSurgAm.1990;72(2):252–8.
4.SchmalzriedTP,CallaghanJJ.Wearintotalhipandknee replacements.JBoneJointSurgAm.1999;81(1):115–36.
5.MakKH,WongTK,PoddarNC.Weardebrisfromtotalhip arthroplastypresentingasanintrapelvicmass.J Arthroplasty.2001;16(5):674–6.
6.MorrisonKM,ApelgrenKN,MahanyBD.Backpain,femoral veinthrombosis,andaniliopsoascyst:unusualpresentation ofaloosetotalhiparthroplasty.Orthopedics.1997;20(4):347–8.
8. ReigstadA,RøkkumM.Anintrapelvicgranulomainducedby acetabularcuploosening.ActaOrthopScand.
1992;63(4):465–6.
9. DeFrangRD,GuyerWD,PorterJM,DuweliusPJ.Synovialcyst formationcomplicatingtotalhiparthroplasty:acasereport. ClinOrthopRelatRes.1996;(325):163–7.
10.MatsumotoK,HukudaS,NishiokaJ,FujitaT.Iliopsoasbursal distensioncausedbyacetabularlooseningaftertotalhip arthroplasty:ararecomplicationoftotalhiparthroplasty. ClinOrthopRelatRes.1992;(279):144–8.
11.FischerSR,ChristDJ,RoehrBA.Sciaticneuropathysecondary tototalhiparthroplastyweardebris.JArthroplasty.
1999;14(6):771–4.
12.MadanS,JowettRL,GoodwinMI.Recurrentintrapelviccyst complicatingmetal-on-metalcementedtotalhip
arthroplasty.ArchOrthopTraumaSurg.2000;120(9):508–10.
13.HisatomeT,YasunagaY,IkutaY,TakahashiK.Hidden intrapelvicgranulomatouslesionsassociatedwithtotalhip arthroplasty:areportoftwocases.JBoneJointSurgAm. 2003;85A(4):708–10.
14.KorkalaO,SyrjänenKJ.Intrapelviccystformationafterhip arthroplastywithacarbonfibre-reinforcedpolyethylene socket.ArchOrthopTraumaSurg.1998;118(1/2):113–5.