SOCIEDADE BRASILEIRA DE ORTOPEDIA E TRAUMATOLOGIA
w w w . r b o . o r g . b r
Technical
note
Posterior
sacroiliac
osteotomy:
an
alternative
to
the
ilioinguinal
approach
for
pelvic
reconstruction
in
misalignment
lesions
夽
João
Antonio
Matheus
Guimarães
∗,
Vinícius
Magno
da
Rocha,
André
Luiz
Loyelo
Barcellos
InstitutoNacionaldeTraumatologiaeOrtopediaJamilHaddad,RiodeJaneiro,RJ,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received9December2016 Accepted26January2017 Availableonline24August2017
Keywords: Osteotomy Bonescrews Sacroiliacjoint Pelvicbones
a
b
s
t
r
a
c
t
Pelvicringfracturesoccurinassociationwithpotentiallyfatallesions,whosetreatmentis apriorityinthepolytraumasetting.Asconsequence,thedefinitiveorthopedicapproach maybepostponed,leadingpatientstochronicandpotentiallydisablingdeformities.The treatmentofthesedeformitiesisachallenge,requiringhighlycomplexandstagedsurgical reconstructions.Theilioinguinalapproachhasbeenwidelyusedinthesesurgeries,because itallowsthereleaseandmobilizationofthehemipelvisand,insomecases,anteriorfixation ofthesacroiliacjoint.However,inmostcases,stablepelvicringreconstructionrequiresthis approachtobecomplementedbytwoothersurgicalapproaches(posteriorlongitudinaland Pfannestiel).Thisrequirementcriticallyincreasesthesurgicaltimeandtheriskof com-plications,suchasneurovascularlesionsandsurgicalwoundinfection.Thecurrentstudy presentsaposteriorosteotomytechniqueforposteriorandanteriorreleaseofthesacroiliac joint,eliminatingtheneedforilioinguinalapproach.Thetechniqueisperformedby pos-teriorlongitudinalaccess;itallowsadequatemobilizationofthehemipelvisandreduction ofverticalandrotationaldeformities,beforethespinopelvicfixationandreductionofthe pubicsymphysis.
©2017SociedadeBrasileiradeOrtopediaeTraumatologia.PublishedbyElsevierEditora Ltda.ThisisanopenaccessarticleundertheCCBY-NC-NDlicense(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Osteotomia
sacroilíaca
posterior:
uma
opc¸ão
ao
acesso
ilioinguinal
na
reconstruc¸ão
pélvica
em
lesões
inveteradas
Palavras-chave: Osteotomia Parafusosósseos Articulac¸ãosacroilíaca Ossopélvico
r
e
s
u
m
o
Asfraturasdoanelpélvicoocorrememassociac¸ãocomlesõespotencialmentegraves,cujo tratamentoéprioritárionocenáriodeatendimentoaopolitraumatizado.Como consequên-cia,aabordagemortopédicadefinitivapodeserpostergada,fazendocomqueospacientesse apresentemcomdeformidadesinveteradasepotencialmenteincapacitantes.Otratamento dessasdeformidadeséumdesafio,requerreconstruc¸õescirúrgicasestagiadasealtamente
夽
StudyconductedatInstitutoNacionaldeTraumatologiaeOrtopediaJamilHaddad,RiodeJaneiro,RJ,Brazil.
∗ Correspondingauthor.
E-mail:jguimaraes@into.saude.gov.br(J.A.Guimarães). http://dx.doi.org/10.1016/j.rboe.2017.08.010
acessolongitudinalposteriorepermitemobilizac¸ãoadequadadahemipelveereduc¸ãode deformidadesverticaiserotacionaisantesdafixac¸ãoespinopélvicaereduc¸ãodasínfise púbica.
©2017SociedadeBrasileiradeOrtopediaeTraumatologia.PublicadoporElsevier EditoraLtda.Este ´eumartigoOpenAccesssobumalicenc¸aCCBY-NC-ND(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
Introduction
Pelvic ring injuries result from high energy trauma. Their associationwithcranioencephalictrauma,pulmonary contu-sions,and/orabdominalviscerallesionsincreasesthelength ofstayinintensivecareunits(ICU)forclinicalstabilization.1
Insomecountries,thedifficultytoaccessspecialized ortho-pediccentersforthetreatmentoftheselesionsfurtherdelays thedefinitiveapproach;it alsoincreasesthelengthof hos-pitalstayandthemorbidityresultingfromprolongeduseof externalfixators.1–3
Itisnotuncommonforthesesurvivorstoevolvewithpain, functionallimitationand,insomecases,neurologicaldeficits associatedwithinveteratedeformity,3whosetreatmentisstill
achallenge.Someofthedifficultiestobeovercomeinclude vicious consolidation, exuberant formation of bony callus, proximitytoabdominopelvicorgansandneurovascular struc-tures,andimplantpositioningincomplexfracturepatterns, withbonelossand/orinfectionresultingfromprolongeduse ofexternalfixators.1–4
Inmostcases,inveteratepelvicringlesionsaretreatedwith threesurgicalapproaches:(1)ilioinguinalapproach(first win-dow),toreleasetheanteriorportionofthesacroiliacjoint(SIJ); (2)longitudinalposteriorapproachtothesacrum,torelease theposteriorportionoftheSIJandposteriorlyfixatethepelvic ring;and (3) the Pfannenstielapproach, to reduceand fix-atethepubicsymphysis(PS).1,2 Thepresentstudypresents
atechniquethateliminatestheneedforthefirstilioinguinal window,reducingtheriskofneurovascularinjuryand infec-tion,aswellassurgicaltimeandoperativebloodloss.
Description
of
the
method
Inthereportedtechnique,theauthors describethecaseof a40-year-oldpatient,victimofa12-meterfall,whosuffered directtrauma tothe lower limbs.In addition tothe pelvic injury,thepatientwasadmittedtotheemergencyunitwith headandabdominaltrauma,pulmonarycontusionand mul-tipleribfracturesontheright,fracture-dislocationoftheright foot,andneurologicaldeficitoftherightL5nerveroot.After initialstabilizationofthepelvis(withexternalfixator)andof
the fracture-dislocationofthe foot andexploratory laparo-tomy, the patient stayed in the ICU for eight weeks until clinicalstabilization.Theexternalfixatorwasthenremoved intheICU,onthesixthweekafterthetrauma.
Twoyearsaftertheaccident,thepatientwasre-assessed. Shecomplainedoflowbackpain,painintherightinguinal region,anddifficultyinwalkingandsittingforlongperiods. Newimagingtestsrevealeddeformityinlateralrotationand highrighthemipelvis(Fig.1A–D),whichledtoshorteningof theipsilaterallowerlimb.Surgicaltreatmentwasindicatedfor reconstructionofthepelvicring.
Surgicaltechnique
Firststage
Weperformedaposteriorlongitudinalapproachtothesacrum withthepatientinventraldecubituspositioning,under gen-eral anesthesia, followed by dissectionof the musculature toallowwidevisualization oftherightSIJ.TheL5,S1, and iliac instrumentation were performedbilaterally, aimingto achieve spinopelvicfixationafterosteotomyandcorrection ofthedeformity.TheossificationobservedontheSIJ,sacral wing, and transverse process ofL5 was carefullyremoved, allowingthereleaseoftheL5root,whichwastrappedbetween thesacralwingandthetransverseprocessbytheraisedright hemipelvis.CarefulosteotomiesweremadeintheSIJfromits cephalictocaudalends;thinosteotomeswereusedfromthe posteriorsacralaspecttowardtheinsideofthejoint,creating aprogressivelywidergrooveinthejointspace(Fig.2A–C).At thisstage,asaprotectivemeasureforthevesselsandpelvic organs,weensuredthattheosteotomesdidnotsurpassthe anteriorportionofthejoint.Thethinbonylayerremainingin theanteriorportionofthejointwasthenremovedwith Ker-risonpunches(Fig.2D).Beforewoundclosure,afragmentof theiliaccrestbonewasresectedforuseinthenextstageof surgery.
Secondstage
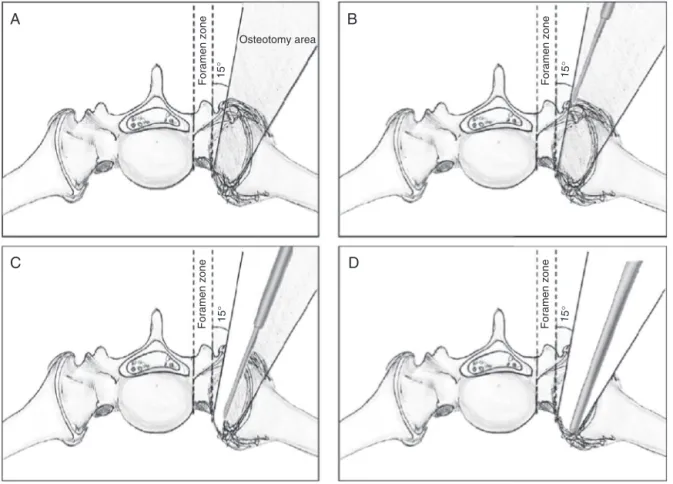
Fig.1–Three-dimensionalcomputedtomographyreconstructiontwoyearsafterthetrauma.(A)Anteriorview;(B)posterior
view;(C)leftwingview;(D)rightwingview.
A
Osteotomy area
Foramen zone
Foramen zone Foramen zone
Foramen zone
15
°
15
°
15° 15°
C
D
B
Fig.2–Posteriorsacroiliacosteotomy.(A)Demonstrationoftheareaofsafetyandangleofattackoftheosteotomeforthe
sequentialbonecuts;(BandC)sequentialboneresection,withgroovecreationandmaintenanceofthethinanteriorcortical
layer;(D)completionofosteotomyusingaKerrisonpunch.
previousstepwasinterposed,inordertoachievejointfusion. Asecondplatewaspositionedtofixatethegraftandprovide additionalrigiditytotheassembly.Thewoundwasclosedin planes,withgoodcoverageoftheimplants.
Thirdstage
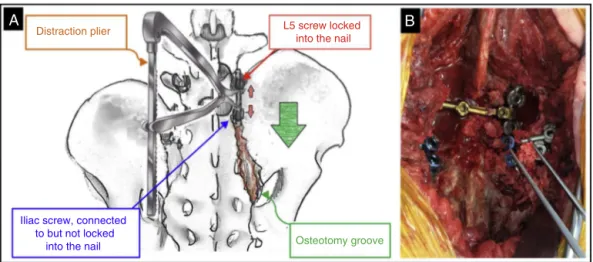
Patient was repositioned in the ventral decubitus and the accessmadeinthefirststagewasreopened.Thedeformity wasreducedwithpliersthatalloweddistractionoftheheads oftheL5andiliacscrews(Fig.3A).Spinopelvicfixationwas performedbylockingthenailstothescrewsandjoiningthem
throughatransverseconnector.Aspongygraftfromtheiliac crestwasthenplacedintheosteotomybedandtheSIJ(Fig.3B). Finally,thewoundwasclosedinlayers,withthesubcutaneous installationofHemovac®drain.
Iliac screw, connected to but not locked
into the nail Osteotomy groove
Fig.3–Posteriorreductionofdeformity.(A)Drawingofthetechniqueand(B)graftingoftheosteotomygroove.
Fig.4–Radiographsofthefirstpostoperativeyear.(A)Inletviewand(B)outletview.
Finalremarks
When addressed in the emergency room, most unstable pelvic fractures are treated with external fixators, even if temporarily.Lindhaletal.3reportedaseriesof110casesof
unstable fracturestreated withexternalfixation; in85% of cases,theresultswereunsatisfactory.Intheirstudy,themain complicationwasviciousconsolidationwithresidual defor-mity(58%).
Althoughthesedeformitiesare associatedwithreduced quality of life, the present authors agree with Mears and Velyvis4 that not all patients would benefit from surgical
reconstruction.Giventhe complexityoftheselesions, clin-icalandradiological aspectsshould betaken intoaccount, as well as the experience of the surgical team and the availabilityofadequateimplantsforthetreatmentofthese patients. Both hemipelvic vertical deviation greater than 10mm and rotation greater than 10 degrees are associ-ated with chronic pain and functional limitation; these parametersareusedtoindicatereconstructioninpatients pre-sentingwithpain,progressiveneurologicaldeficit,and/orgait difficulty.2,5
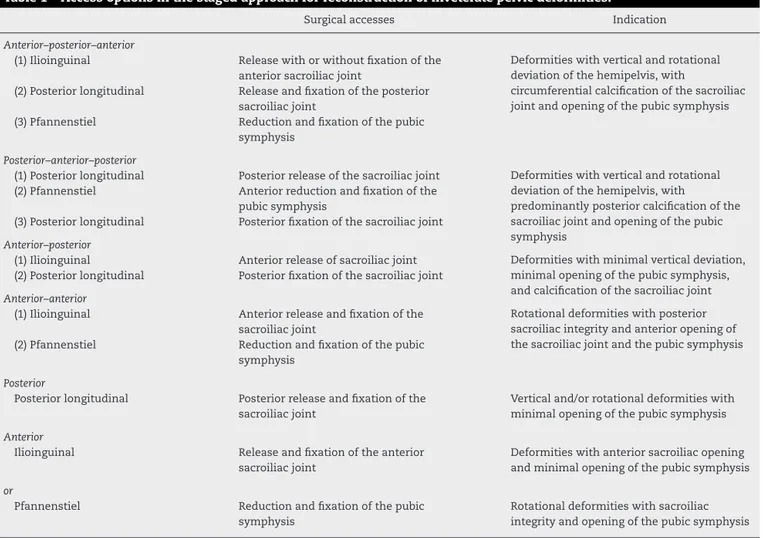
Usually,surgicalreconstructionrequiresastagedapproach to recreatethe initial lesion,allowing its mobilization and correction ofthe deformity. For each stageoftreatment, a differentsurgicalapproachisused(Table1).
Injuries withmultidirectional instabilityusually present withascendingandrotatinghemipelvis,circumferential cal-cificationoftheSIJ,andsofttissueretraction,andfrequently requiretriple-stagedapproach.2Inthisapproach,the
ilioin-guinalaccessisusedforanteriorreleaseoftheSIJ,andhas beenconsideredacornerstoneofthetreatment.2,4Thisaccess
increasesoperativetime,bloodloss,andtheriskof hetero-topicossification;italsoputstheL5nerverootandinguinal neurovascularbundleatriskandhasalreadybeenlinkedto abductormuscleweakness,incisionalhernias,and postopera-tiveinfections.6
Table1–Accessoptionsinthestagedapproachforreconstructionofinveteratepelvicdeformities.
Surgicalaccesses Indication
Anterior–posterior–anterior
(1)Ilioinguinal Releasewithorwithoutfixationofthe anteriorsacroiliacjoint
Deformitieswithverticalandrotational deviationofthehemipelvis,with
circumferentialcalcificationofthesacroiliac jointandopeningofthepubicsymphysis (2)Posteriorlongitudinal Releaseandfixationoftheposterior
sacroiliacjoint
(3)Pfannenstiel Reductionandfixationofthepubic symphysis
Posterior–anterior–posterior
(1)Posteriorlongitudinal Posteriorreleaseofthesacroiliacjoint Deformitieswithverticalandrotational deviationofthehemipelvis,with
predominantlyposteriorcalcificationofthe sacroiliacjointandopeningofthepubic symphysis
(2)Pfannenstiel Anteriorreductionandfixationofthe pubicsymphysis
(3)Posteriorlongitudinal Posteriorfixationofthesacroiliacjoint
Anterior–posterior
(1)Ilioinguinal Anteriorreleaseofsacroiliacjoint Deformitieswithminimalverticaldeviation, minimalopeningofthepubicsymphysis, andcalcificationofthesacroiliacjoint (2)Posteriorlongitudinal Posteriorfixationofthesacroiliacjoint
Anterior–anterior
(1)Ilioinguinal Anteriorreleaseandfixationofthe sacroiliacjoint
Rotationaldeformitieswithposterior sacroiliacintegrityandanterioropeningof thesacroiliacjointandthepubicsymphysis (2)Pfannenstiel Reductionandfixationofthepubic
symphysis
Posterior
Posteriorlongitudinal Posteriorreleaseandfixationofthe sacroiliacjoint
Verticaland/orrotationaldeformitieswith minimalopeningofthepubicsymphysis
Anterior
Ilioinguinal Releaseandfixationoftheanterior sacroiliacjoint
Deformitieswithanteriorsacroiliacopening andminimalopeningofthepubicsymphysis
or
Pfannenstiel Reductionandfixationofthepubic symphysis
Rotationaldeformitieswithsacroiliac integrityandopeningofthepubicsymphysis
reductionofthehemipelvisthroughtheilioinguinalapproach becomesinfeasible.
Another aspect that deserves attention is the insuffi-cientstabilityoftheanteriorsacroiliacosteosynthesis,which makes posterior complementation necessary, especially in deviatedandagedlesions.7Moreover,skeletaltractionoruse
ofSchanz screwsasajoystickmay benecessary toreduce theiliumandtopositiontheanteriorsacroiliacplates.When therelease ismade througha posteriorapproach, the dis-traction maneuversbetween L5 and the iliac screws allow adequatereduction,notrequiringadditionaldevicesthat fur-therincreasemorbidityanddurationofthesurgery.8
Inthepresent patient,thePfannenstielaccesswasused inthesecond stageofsurgerytoreduceand fixatethePS, providing greater stability to the pelvic ring. Biomechani-cal studies that evaluate the importance of this stage in pelvicreconstructionarestillnecessary.Theneedtofusion theSIJisanothercontroversialpointinthepresented tech-nique.Theauthorsusedgraftsintheosteotomyarea,because some areas of the groove made remained with no bone contactevenafterthedeformitywasreduced.The contralat-eralSIJisalsofused,because the authorsbelieve thatthis allowsreductionofthebiomechanicalstressonthe screws inserted in the ilium and thus the risk of loosening or breaking.
Thistechniqueisapromisingoption,butitisequally tech-nicallydemanding.Themainlimitationisstilltheneedfor integrationbetweentheorthopedictraumasurgeryandthe spinesurgeryteams.Trainingneworthopedistsinadvanced coursesofpelvictraumaisaninvestmentthatmustbe con-sideredinlightofthegrowingnumberoftraumapatientsand thecreationofspecializedcenters.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.KanakarisNK,AngoulesAG,NikolaouVS,KontakisG,
GiannoudisPV.Treatmentandoutcomesofpelvicmalunions
andnonunions:asystematicreview.ClinOrthopRelRes.
2009;467(8):2112–24.
2.OranskyM,TortoraM.Nonunionsandmalunionsafterpelvic
fractures:whytheyoccurandwhatcanbedone?Injury.
2007;38(4):489–96.
3.LindahlJ,HirvensaloE,BostmanO,SantavirtaS.Failureof
reductionwithanexternalfixatorinthemanagementof
injuriesofthepelvicringLong-termevaluationof110patients.