w w w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Original
article
The
correlation
between
antiphospholipid
syndrome
and
cryoglobulinemia:
case
series
of
4
patients
and
review
of
the
literature
Shiber
Shachaf
a,b,∗,
Molad
Yair
a,baRheumatologyUnit,RabinMedicalCenter,PetachTikva,Israel
bSacklerFacultyofMedicine,TelAvivUniversity,TelAviv,Israel
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received1March2014
Accepted14September2014
Availableonline7January2015
Keywords:
Cryoglobulinemia
Antiphospholipidsyndrome
Vasculitis
a
b
s
t
r
a
c
t
Background:Cryoglobulinemiaisanimmune-complex-mediatedsmallvesselvasculitisthat
classicallyinvolvestheskin,kidneysandperipheralnerves.Antiphospholipidsyndrome
(APS)isanautoimmunehypercoagulabledisorderwhichcausesbloodvesselthrombosis.It
canpresentasamulti-organmicrothromboticdisorderwhichiscalledcatastrophicAPS.
Objective:Inthiscaseseriesweaimtodescribethediagnosticandmanagementchallenges
thatarisewhenthesetwoseveredisorderssimultaneouslypresentinthesamepatient.
Methods:Wedescribefourpatientswhowereadmittedtoourhospitalduetomulti-organ
lifethreateningdamagemediatedbycryoglobulinemicvasculitiswithconcurrentAPS.
Results:Clinicalmanifestations includedleg ulcers,livedo reticularis,renal failure,and
peripheralneuropathy.Suggestedetiologiesforthecombinedsyndromeswerehepatitis
C,systemiclupuserythematosusandmyeloproliferativediseaserectalmaltoma. Allof
ourpatientsweretreatedwithanticoagulation,high-dosecorticosteroids,rituximab,
intra-venousgammaglobulinsandplasmaexchange.
Conclusion:Therareassociationofsevereor catastrophicAPS withcryoglobulinemiain
patientsshouldbeconsideredbyphysicianswhotreatpatientswithmulti-organischemia
ornecrosis.
©2014ElsevierEditoraLtda.Allrightsreserved.
DOIoforiginalarticle:http://dx.doi.org/10.1016/j.rbr.2014.09.005.
∗ Correspondingauthor.
E-mail:sofereret@gmail.com(S.Shachaf).
http://dx.doi.org/10.1016/j.rbre.2014.09.007
Correlac¸ão
entre
a
síndrome
antifosfolipídica
e
a
crioglobulinemia:
série
de
quatro
casos
e
revisão
da
literatura
Palavras-chave:
Crioglobulinemia
Síndromeantifosfolipídica
Vasculite
r
e
s
u
m
o
Introduc¸ão: Acrioglobulinemiaéumavasculitedepequenosvasosmediadapor
imuno-complexosquenormalmenteenvolvemapele,osrinseosnervosperiféricos.Asíndrome
antifosfolipídica(SAF) éumtranstornodahipercoagulabilidadeautoimunequeprovoca
trombosedosvasossanguíneos.Podesemanifestarcomoumdistúrbiomicrotrombótico
queafetamúltiplosórgãos,denominadoSAFcatastrófica.
Objetivo: Estasériedecasosobjetivadescreverosdesafiosdediagnósticoetratamentoque
surgemquandoessesdoisgravestranstornosestãopresentessimultaneamentenomesmo
paciente.
Métodos: Foramdescritosquatropacientesinternadosemnossohospitalemdecorrência
dedanosgravesamúltiplosórgãosmediadospelavasculitecrioglobulinêmicacomSAF
concomitante.
Resultados:Asmanifestac¸õesclínicasincluíramúlcerasdeperna,livedoreticular,
insuficiên-ciarenaleneuropatiaperiférica.Asetiologiassugeridasparaacombinac¸ãodesíndromes
foramahepatiteC,olúpuseritematososistêmicoeadoenc¸amieloproliferativaretal
asso-ciadaalinfomadezonamarginaltipocélulasB.Todosospacientesforamtratadoscom
anticoagulantes,altasdosesdecorticosteroides,rituximabe,gamaglobulinasintravenosas
etrocadeplasma.
Conclusão: Araraassociac¸ãoentreaSAFgraveoucatastróficaeacrioglobulinemiadeveser
consideradapormédicosqueatendempacientescomisquemiaounecrosedemúltiplos
órgãos.
©2014ElsevierEditoraLtda.Todososdireitosreservados.
Introduction
Cryoglobulins (CG) are immune complexes comprised of
immunoglobulins(IGs),eitherpoly-ormonoclonal,thatbinds
other IGs that are deposited in small blood vessels and
glomeruli upon exposureto coldtemperatures. The
preva-lence of clinically significant cryoglobulinemia has been
estimatedatapproximately1in100,000.1–4 Thepresenceof
theCG-containingimmunecomplexesoftenresultsinsmall
tomediumvesselvasculitis.5–7 TheBrouetclassificationof
cryoglobulinemiaisbasedon the compositionofthe CGs:8
Type I – isolated monoclonal IGs; Type II – Mixed CGs –
immunecomplexes formed bymonoclonal IGs,this isthe
mostcommontypeandassociatedwithHCVandHIV;Type
III–MixedCGs–immunecomplexesformedbypolyclonal
IGs.
Although most of the patients with cryoglobulinemia
remainasymptomatic,the disease may involve mainlythe
skin, kidneys and peripheral nervous system. Type I
cryo-globulinemiamanifestationsareusuallyduetohyperviscosity
and/or thrombosis,including Raynaud’sphenomenon,
dig-italischemia and gangrene,livedo reticularis,purpura and
neurologic symptoms. In contrast, type II and III
cryo-globulinemia causes arthralgia, fatigue, myalgia, palpable
purpura, peripheral neuropathy as well as
membranopro-liferativeglomerulonephritis.9–11Antiphospholipidsyndrome
(APS) is an autoimmune hypercoagulable disorder
charac-terized by arterial and/or venous thrombosis, pregnancy
morbidityincludingrecurrentfetallossandeclampsiainthe
presenceofelevatedlevels ofanti-cardiolipin(ACL)(≥40U)
and/or2glycoproteinIIgGand/orIgMantibody(>99th
per-centile)and/orlupusanticoagulant(LAC).
Antiphospholipidantibodies (aPL). According tothe
lab-oratory revised criteria the anti-cardiolipin (ACL) IgG, IgM
antibodyand/oranti-2glycoproteinI(2GPI)IgG,IgM
(accord-ing toour laboratory kit, above >20U) and/or positive test
forlupusanticoagulant(LAC)testedpositiveon2
consecu-tive occasions at least 12 weeksapart.12–15 An association
between cryoglobulinemia and APS has been previously
reported(Table1).16–20Inthisstudy,wedescribefourpatients
whopresentedwithmanifestationsofbothcryoglobulinemic
vasculitis21andAPS.
Case
presentation
Case1
A 51-year-oldfemale waspresentedwithdiabetes mellitus
type2andhypertension.In1997shesufferedfrom sudden
lossofvisioninrighteye.In2001shedevelopedlivedo
reticu-larisofbothlowerextremities.Laboratorytestsrevealedurine
sticktestproteinlevelof500mg/dL,CRPlevelwas54.85mg/dL
(uppernormalrange–0.5mg/dL),andpositiveaPLserology
(2teststaken12weeksapart–valuesarelistedinTable2).
Also, positive ANA titer (1:160), positive
cryofibrino-gen IgG and IgM kappa, and IgM cryoglobulins type 1
(215mg/L, reference range 0–60mg/L) were revealed.
Kid-neybiopsydemonstratedevidenceofmembranoproliferative
glomerulonephritis.Thepatientwastreatedwith1g
Table1–Laboratorycharacteristicsofourpatientscaseseries.
Patient num.
Age Sex Etiology ACL antibodya,b
Anti-2GPI antibodya,b
LACa,c ANA Anti-DsDNA
RF Cryoglobulins mono-clonal/polyclonal/ mixed
1 51 F Idiopathic +
IgM=153U, 109U IgG=98U, 115U
+
IgM=100U, 73U IgG=81U, 49U
- + - NS IgMkappamonoclonal
2 66 M Multiple
myeloma
− +
IgG=78U, 122U
− + − − IgGkappamonoclonal
3 40 M HCV
andSLE +
IgM=132U, 49U
+ IgM=67U, 50U
+ + + − Mixed
4 65 F MALT
lymphoma + IgG=91U, 73U
+ IgG=56U, 62U
+ + − + Mixed
ACL,anticardiolipin;anti2GPI,anti-2glycoproteinI;LAC,lupusanticoagulant;ANA,antinuclearantibody;antiDsDNA,antidoublestrand DNA;RF,rheumaticfactor;HCV,hepatitisCvirus
a 2valuesfor2teststaken12weeksapart.
b ACLandanti-2GPIIgG,IgMantibodyassayedbyELISAaccordingtomanufacturer’sguidelines.
c LupusanticoagulanttestedwithRVVT,Positivevaluesabove1.5ratio.
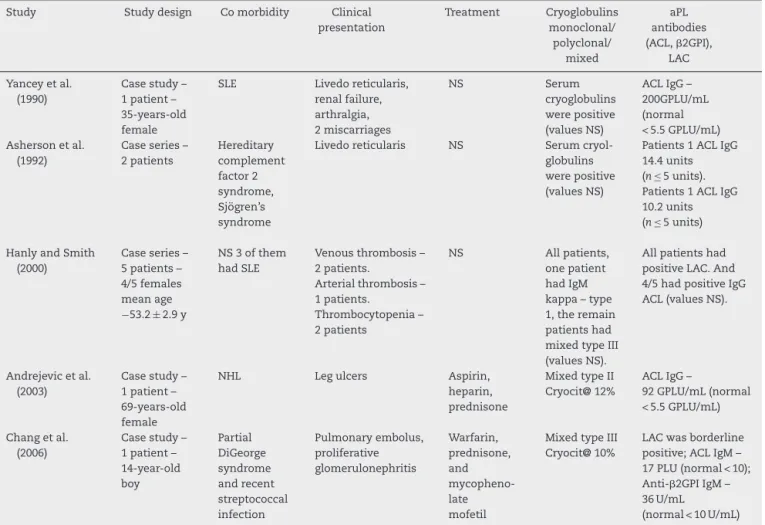
Table2–Summaryofcasestudiesandseriesofclinicalandlaboratorycharacteristicinpatientwithantiphospholipid syndromeandcryoglobulinemia.
Study Studydesign Comorbidity Clinical presentation Treatment Cryoglobulins monoclonal/ polyclonal/ mixed aPL antibodies (ACL,2GPI), LAC
Yanceyetal. (1990)
Casestudy– 1patient– 35-years-old female
SLE Livedoreticularis, renalfailure, arthralgia, 2miscarriages NS Serum cryoglobulins werepositive (valuesNS)
ACLIgG– 200GPLU/mL (normal <5.5GPLU/mL) Ashersonetal.
(1992)
Caseseries– 2patients Hereditary complement factor2 syndrome, Sjögren’s syndrome
Livedoreticularis NS Serum cryol-globulins werepositive (valuesNS)
Patients1ACLIgG 14.4units (n ≤ 5units). Patients1ACLIgG 10.2units (n ≤ 5units)
HanlyandSmith (2000)
Caseseries– 5patients– 4/5females meanage −53.2± 2.9y
NS3ofthem hadSLE
Venousthrombosis– 2patients.
Arterialthrombosis– 1patients.
Thrombocytopenia– 2patients
NS Allpatients, onepatient hadIgM kappa–type 1,theremain patientshad mixedtypeIII (valuesNS).
Allpatientshad positiveLAC.And 4/5hadpositiveIgG ACL(valuesNS).
Andrejevicetal. (2003)
Casestudy– 1patient– 69-years-old female
NHL Legulcers Aspirin, heparin, prednisone
MixedtypeII Cryocit@12%
ACLIgG–
92GPLU/mL(normal <5.5GPLU/mL)
Changetal. (2006)
Casestudy– 1patient– 14-year-old boy Partial DiGeorge syndrome andrecent streptococcal infection Pulmonaryembolus, proliferative glomerulonephritis Warfarin, prednisone, and mycopheno-late mofetil
MixedtypeIII Cryocit@10%
LACwasborderline positive;ACLIgM– 17PLU(normal<10); Anti-2GPIIgM– 36U/mL
(normal<10U/mL)
to60mgprednisone.3yearslater,thepatientwasadmitted
tothehospitalwithpurpura,ulcersinherlowerextremities
andsplinterhemorrhagesofthenails.
Sheshowedevidenceofnephroticsyndromewithurine
proteinof5g/24handacuterenalfailure(serumcreatinine
levelwas2.8mg/dL).Skinbiopsydemonstratedathrombotic
eventwithoutevidenceofvasculitis.Urinewaspositivefor
Bence-Jones protein. CGsand Cryofibrinogen were positive
(315mg/L,referencerange0–60mg/L,and3g/L;uppernormal
range–0.5g/L,respectively).HepatitisBandCwereboth
neg-ative.Bonemarrowbiopsyshowednoevidenceofmyeloma
orotherlymphoproliferativedisease.
Thepatientwastreatedwith60mgprednisoneand
war-farin (dose adjusted according to INR goal of 2–3) with
improvementofcutaneousfindingsandpartialnormalization
ofcreatininelevel(1.7mg/dL).Urineproteinwas2.3g/24h.
Twoyearslatershepresentedwithdyspnea,hemoptysis,
anemia, lower extremitiespurpura and elevated creatinine
level. Chest CT revealed diffuse alveolar hemorrhage. The
treatmentwithwarfarinwasthen discontinued.Creatinine
level was4.62mg/dLwith urine proteinof7.125g/24h and
RBCcastswereobservedonmicroscopicexaminationofurine.
CryofibrinogenIgGkappawas positive(2g/L, uppernormal
range 0.5g/L). CGs were negative(32mg/L, reference range
0–60mg/L)andaPLwerepositive.Treatmentwasinitiatedwith
dialysis,hydrocortisone(100mg×3d),2coursesofrituximab
(1g) infusionsandplasmapheresis.Thepatientdied inthe
intensivecareunit2weeksafterbeingadmittedtothehospital
duetosepsis.
Case2
A66-year-oldmalewithdiabetesmellitustype2.In2003he
presentedwithlowerextremityulcers(mainlyintoes).Hewas
treatedwithprednisone(60mg×1d)withtaperingdownfor
3monthsandIViloprost(prostacyclinPGI2analog).Serology
for Hepatitis B was positive (HBs and HBe were positive)
and anti-viraltreatment withLamivudine(nucleoside
ana-logreversetranscriptaseinhibitor)wasinitiated(300mg×1d).
Underthistreatmentthepatient’sulcersimproved.
Three years later he presented with ischemic ulcers in
a number of toes and purpura in both lower extremities.
Skinbiopsyrevealedfreshbleedingindermiswith
mononu-clearinfiltratearound blood vessels. Oneblood vesselwas
surrounded by polymorphonuclear infiltrate and in some
vessels thrombi were evident. Monoclonal CGs IgG light
chain kappa type 1 was found (152mg/L, reference range
0–60mg/L).C3andC4levelswerenormal.Bonemarrowbiopsy
revealed 7–8%plasma cells positiveforIgG kappa. Mostof
theplasmacellswere monoclonalforIgA.Thepatientwas
treatedfortype 1cryoglobulinemiawith monoclonal
gam-mopathywithplasmaphersis andIVcyclophosphamidefor
6months.
Sixyearsafterthe initialpresentationhedevelopedleft
hemiparesis.Laboratorytestswerepositivetwice,12weeks
apart,foraPLserology(Table2)andANAtiterwas1:160.The
patientwasdiagnosedwithAPSandtreatedwithwarfarin.
Oneyearlater,hepresentedwithright3rdfinger
necro-sisandpalpablepurpuraonleftlowerlimb.Hewastreated
with a sympathetic block, hydrocortisone (100mg×3d),
plasmapheresis,IViloprostandwarfarin.Bonemarrowbiopsy
demonstratedpositivityforCD138withplasmacellssecreting
lambdaandkappalightchains.
In 2011 a bone marrow biopsy showed 15% plasma
cells positive for IgG kappa light chain secretion
(multi-ple myeloma-clonal plasma cells >10% on bone marrow
biopsy). The patient was positive for CGs (343mg/L,
refer-encerange0–60mg/L).Therefore,thepatientwasdiagnosed
withmultiplemyelomaandbegantreatmentwithmelphalan,
prednisoneandbortezomib.
Case3
A40-year-oldmaleknowntobeahepatitisC(HCV)carrierwas
diagnosedwithsystemiclupuserythematosus(SLE)in1999.
The disease presentation included malarrash, leucopenia,
thrombocytopenia, photosensitivity, arthritis and alopecia.
Laboratory:analysisshowedthatANAanddsDNAwere
pos-itive(ANAof1:160,dsDNAof25%,normalrange0–20%).The
patientwastreatedwithhydroxychloroquineandprednisone
(invaryingdosages).Fiveyearslaterhepresentedwithright
footgangrenewhichnecessitatedbelowkneeamputationand
CVA withright hemiparesis. CT scan revealed left parietal
infarct. In laboratory testing, there was positivity for aPL
(2 teststaken12 weeksapart–valuesare listedinTable2)
and mixedcryoglobulinemia (type 2) – 511mg/L(reference
range 0–60mg/L). He was treated with warfarin,
hydroxy-chloroquine(200mg×2d)andprednisone(60mg)withthree
monthstaperingdown.
Case4
A65-year-oldfemalewhohadbeensufferingfrom
intermit-tent purpura fornearly 30 years and inthe last few years
begancomplainingofnumbnessofthelowerlimb.EMG
stud-iesrevealedsevereaxonopathy.CTofthespineshowedonly
spondylolisthesisinL5-S1.Laboratorywaspositiveformixed
cryoglobulinemia – CGs level of 215mg/L (reference range
0–60mg/L)andANAtiterof1:160.C3andC4levelswerevery
lowand serology’sforhepatitisCand Bwere negative.aPL
serologywaspositive(2teststaken12weeksapart–Table2).
ThepatientunderwentanabdominalCTwhichrevealedan
inflamedterminalileum.
Colonoscopic examination showed macroscopic
appear-ance of proctitis and the biopsy was compatible with
mucosa-associatedlymphoidtissue(MALT)lymphoma.
Treat-mentwithrituximab,cyclophosphamideandprednisonewas
initiated. Aweek later,the patient wasre-admitted to the
hospitalduetolivedoreticularis,purpura,lowerextremities
ulcers andconfusion.HeadCTshowed noinfracts.
Labora-torytestsrevealedmicroangiopathicanemia(schistocyteson
bloodsmear)andthrombocytopeniaof70K/L(normalrange
150,000–450,000K/L).
Treatment with hydrocortisone (100mg×3d) and
anti-coagulation with IV heparin was initiated. Under this
treatment,theconfusionimprovedpartially,butthelegulcers
progressedtoanaerobicinfectionandthensepsis,eventually
Discussion
Inthecaseseriespresentedherewedescribefourpatients
withcryoglobulinemic vasculitis present concurrently with
clinicalfeaturesofAPS.Allourpatientssufferedfrom
recalci-trantlegulcersandskinnecrosis,resultinginamputationsin
2outofthe4patients.
Inacase-seriesof200consecutivepatientswithAPS(either
primary APS or APS secondary to SLE), skin ulcers and/or
necrosiswasreportedinonly2%ofthepatients,22whereas
itoccursin10%ofpatientswithcryoglobulinemia.23 Inour
series,allfourpatientssufferedfromskinulcersandnecrosis,
mostprobablysecondarytothesynergisticeffectof
cryoglob-ulinandthrombosis-mediatedcutaneousischemiaasresult
ofsmallandmedium-sizedbloodvesselocclusion.
Ourcase-seriesisinaccordancewiththreecase-seriesof
patientswithbothcryoglobulinemiaandAPS.16–18This
sug-geststhattheconcurrentpresentationofoverlappingclinical
featuresduetocryoglobulinemiaandAPSshouldbeassessed
inpatientswithsevereischemiccutaneouslesions.The
eti-ologyofcryoglobulinemiaandAPSintheHanlyandSmith16
andYanceyetal.17serieswasmostlyduetoSLE.Inourcase
series,twopatients(2,4)suffered fromlymphoproliferative
disease,onepatientwasdiagnosedwithprimaryAPSandone
hadHCVandSLE.
Likepatients2and4inourserieswho had
lymphopro-liferativedisease,Andrejevicetal.,18describedpatientswith
non-Hodgkinslymphoma,monoclonalcryoglobulinemiaand
ACLantibodieswithvasculitis.Theyconcludedthatpatients
with lymphoid malignancies and ACL antibodies in their
cryoprecipitatemaybeatriskfordevelopingclinical
mani-festationsofAPS.
Chang et al.19 also described a patient with DiGeorge
syndromewhodevelopedmixedcryoglobulinemia,APSand
systemicvasculitisafterastreptococcalinfection.
Ashersonet al.,20 described twosibling with hereditary
complementfactor2deficiencies.Theybothpresentedwith
cutaneousvasculitis,cryoglobulinemiaand ACL antibodies.
Afterremovalofthecryoprecipitatefromtheserumsample
ofthe two patients the serum antibodies ofACL fell. This
implicatestheincorporationofACLantibodieswithin
cryo-precipitates.
Theformationof2glycoproteinIandanti-2glycoprotein
Iantibodyimmune-complexeshasbeendocumented.24
However,Bardin et al.25 described 55 patientswith APS
whowerepositiveforbothcryoglobulinemiaandIgM
phos-phatidylethanolamineantibodies(aPE).DeterminationofIgM
aPElevelswasmadebeforeandafterremovalof
cryoprecip-itatefrom the serum. Ofthe 55 patients, 52 (95%)showed
nosignificant difference ofIgMaPElevels beforeand after
cryoprecipitation.Theyconcluded thatinmost cases
cryo-precipitationdoesnotinterferewithIgMaPElevel.Thus,IgM
aPEdoes notappeartobeinvolvedintheformationofthe
cryoprecipitate.
Our study isnot without limitations;it includesonly a
smallnumberofpatients,withdifferenttypesof
cryoglobu-lins,differentisotypesofantiphospholipidantibodies,aswell
asdifferentco-morbidities.Inspiteofthisheterogeneity,all
fourpatientshadhardtotreatischemiccutaneousulcersand
thisisthemostimportantmanifestationrelatedtothe
pre-sentationofthetwosyndromespresentedtogether.
WerecommendrulingoutthepresenceofAPSinpatients
withcryoglobulinemicvasculitisrecalcitranttothestandard
therapyandviceversa.
Conflicts
of
interests
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.BonnetF,PineauJJ,TaupinJL,FeylerA,BonarekM,deWitteS,
etal.Prevalenceofcryoglobulinemiaandserologicalmarkers
ofautoimmunityinhumanimmunodeficiencyvirusinfected
individuals:acrosssectionalstudyof97patients.J
Rheumatol.2003;30:2005.
2.García-CarrascoM,Ramos-CasalsM,CerveraR,TrejoO,
YagüeJ,SisóA,etal.Cryoglobulinemiainsystemiclupus
erythematosus:prevalenceandclinicalcharacteristicsina
seriesof122patients.SeminArthritisRheum.2001;30:366.
3.Ramos-CasalsM,CerveraR,YagüeJ,García-CarrascoM,Trejo
O,JiménezS,etal.CryoglobulinemiainprimarySjögren’s
syndrome:prevalenceandclinicalcharacteristicsinaseries
of115patients.SeminArthritisRheum.1998;28:200.
4.CicardiM,CesanaB,DelNinnoE,PappalardoE,SiliniE,
AgostoniA,etal.Prevalenceandriskfactorsforthepresence
ofserumcryoglobulinsinpatientswithchronichepatitisC.J
ViralHepat.2000;7:138.
5.JennetteJC,FalkRJ,AndrassyK,BaconPA,ChurgJ,GrossWL,
etal.Nomenclatureofsystemicvasculitidesproposalofand
internationalconsensusconference.ArthritisRheum.
1994;37:187.
6.DispenzieriA,GorevicPD.Cryoglobulinemia.HematolOncol
ClinNorthAm.1999;13:1315.
7.LamprechtP,GauseA,GrossWL.Cryoglobulinemicvasculitis.
ArthritisRheum.1999;42:2507.
8.BrouetJC,ClauvelJP,DanonF,KleinM,SeligmannM.Biologic
andclinicalsignificanceofcryoglobulins.Areportof86cases.
AmJMed.1974;57:775.
9.MontiG,GalliM,InvernizziF,PioltelliP,SaccardoF,
MonteverdeA,etal.Cryoglobulinaemias:amulti-centre
studyoftheearlyclinicalandlaboratorymanifestationsof
primaryandsecondarydisease.GISC.ItalianGroupforthe
StudyofCryoglobulinaemias.QJM.1995;88:115.
10.MontagninoG.Reappraisaloftheclinicalexpressionofmixed
cryoglobulinemia.SpringerSeminImmunopathol.1988;10:1.
11.TrejoO,Ramos-CasalsM,García-CarrascoM,YagüeJ,Jiménez
S,delaRedG,etal.Cryoglobulinemia:studyofetiologic
factorsandclinicalandimmunologicfeaturesin443patients
fromasinglecenter.Medicine(Baltimore).2001;80:252.
12.MiyakisS,LockshineMD,AtsumiT,BranchDC,BreyRL,
CerveraR,etal.Internationalconsensusstatementonan
updateoftheclassificationcriteriafordefinite
antiphospholipidsyndrome(APS).JThrombHaemost.
2006;4:295–306.
13.NairS,KhamashtaMA,HughesGRV.SyndromeXandHughes
syndrome.Lupus.2002;11:332–9.
14.Ruiz-IrastorzaG,CrowtherM,BranchW,KhamashtaMA.
Antiphospholipidsyndrome.Lancet.2010;376:1498–509.
15.MiyakisS,LockshinMD,AtsumiT,BranchDW,BreyRL,
CerveraR,etal.Internationalconsensusstatementonan
updateoftheclassificationcriteriafordefinite
antiphospholipidsyndrome(APS).JThrombHaemost.
16.HanlyJG,SmithSA.Autoimmuneantiphospholipid
antibodiesandcryoglobulinemia.Lupus.2000;9:264–70.
17.YanceyWB,EdwardsNL,WilliamsRC.Cryoglobulinsina
patientwithSLE,livedoreticularis,andelevatedlevelof
anticardiolipinantibodies.AmJMed.1990;88:699.
18.AndrejevicS,Bonaci-NikolicB,BukilicaM,MilivojevicG,
BasanovicJ,NikolicMM.Purpuraandlegulcersinapatient
withcryoglobulinaemia,non-Hodgkin’slymphoma,and
antiphospholipidsyndrome.ClinExpDermatol.
2003;28:151–3.
19.ChangAD,TachdjianR,GallagherK,McCurdyDK,LassmanC,
StiehmER,etal.TypeIIImixedcryoglobulinemiaand
antiphospholipidsyndromeinapatientwithpartial
DiGeorge’ssyndrome.ClinDevImmunol.2006;13:261–4.
20.AshersonRA,D’CruzD,HughesGR.Cryoglobulins,
anticardiolipinantibodiesandlivedoreticularis.JRheumatol.
1992;19:826.
21.KamaliS,Artim-EsenB,ErerB,OzdenerL,GulA,OcalL,etal.
Re-evaluationof129patientswithsystemicnecrotizing
vasculitidesbyusingclassificationalgorithmaccordingto
consensusmethodology.ClinRheumatol.2012;31:325–8.
22.FrancèsC,NiangS,LaffitteE,PelletierFL,CostedoatN,Piette
JC.Dermatologicmanifestationsoftheantiphospholipid
syndrome:twohundredconsecutivecases.ArthritisRheum.
2005;52:1785–93.
23.MontiG,GalliM,InvernizziF,PioltelliP,SaccardoF,
MonteverdeA,etal.Cryoglobulinaemias:amulticentrestudy
oftheearlyclinicalandlaboratorymanifestationsofprimary
andsecondarydisease.GISC.ItalianGroupfortheStudyof
Cryoglobulinaemias.QJM.1995;88:115–26.
24.GeorgeJ,GilburdB,LangevitzP,LevyY,NezlinR,HaratsD,
etal.Beta2glycoproteinIcontainingimmunecomplexesin
lupuspatients:associationwiththrombocytopeniaand
lipoprotein(a)levels.Lupus.1999;8:116–20.
25.BardinN,PommierG,SanmarcoM.Cancryoglobulins
interferewiththemeasurementofIgM
antiphosphatidylethanolamineantibodiesbyElisa?Thromb