r e v b r a s r e u m a t o l . 2016;56(1):75–78
w w w . r e u m a t o l o g i a . c o m . b r
REVISTA
BRASILEIRA
DE
REUMATOLOGIA
Case
report
Musculoskeletal
ultrasound
findings
in
paracoccidioidomycosis
José
Alexandre
Mendonc¸a
∗,
Faustino
Peron
Filho,
Nádia
Bossolan
Schincariol,
Cláudia
Valéria
Vierhout,
José
Roberto
Provenza
DepartmentofRheumatology,PontifíciaUniversidadeCatólicadeCampinas,Campinas,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received8November2013 Accepted21February2014 Availableonline28November2014
Keywords:
Parcoccidioidomycosis Ultrasound
Arthritis Tenosynovitis Synovitis
a
b
s
t
r
a
c
t
Paracoccidioidomycosis is a fungal infection endemicto South America. The infection isusuallyasymptomaticandmostlyaffectstheupper andlowerrespiratorytractswith clinical–radiologicaldissociation.Jointinvolvementisrarewithnospecificpatternor radio-logicalinjury.We reporta caseofparacoccidioidomycosisinwhichthepatient’s initial symptomswerehoarsenessandarthritis.Afteranultrasoundexamination,weperformed thedifferentialdiagnosisofothernoninfectiousarthropathiesandanalysisofthematerial collected,whichrevealedinfectionwiththefungusParacoccidioidesbrasiliensis.
©2014ElsevierEditoraLtda.Allrightsreserved.
Achados
ultrassonográficos
osteomusculares
na
paracoccidioidomicose
Palavras-chave: Paracoccidioidomicose Ultrassonografia Artrite
Tenossinovite Sinovite
r
e
s
u
m
o
Aparacoccidioidomicoseéumainfecc¸ãofúngicaendêmicanaAméricadoSul.Ainfecc¸ão geralmenteéassintomáticaeafetaprincipalmenteostratosrespiratóriossuperioreinferior, comdissociac¸ãoclínico-radiológica.Oenvolvimentoarticularéraro,semumpadrãoou lesãoradiológicaespecífica.Apresenta-seumrelatodecasodeparacoccidioidomicoseem queossintomasiniciaisdopacienteforamrouquidãoeartrite.Depoisdeumexamede ultrassonografia,foramfeitosodiagnósticodiferencialdeoutrasartropatiasnãoinfecciosas eaanálisedomaterialcoletado,querevelouinfecc¸ãopelofungoParacoccidioidesbrasiliensis. ©2014ElsevierEditoraLtda.Todososdireitosreservados.
∗ Correspondingauthor.
E-mail:mendocaja@ig.com.br(J.A.Mendonc¸a). http://dx.doi.org/10.1016/j.rbre.2014.02.022
76
r e v b r a s r e u m a t o l . 2016;56(1):75–78Introduction
Paracoccidioidomycosis is a fungal infection endemic to SouthAmericacausedbythethermodimorphicfungus Para-coccidioides sp.1 The fungus has a spatially heterogeneous
distribution, with areas of low and high endemicity, and thediseaseisacquiredbyairborneinhalationorvialesions inskinandmucosa.Theinfectionisusuallyasymptomatic and mostly affects the upper and lower respiratory tracts withclinic–radiologicaldissociation.Eventhough rare, sev-eralextrapulmonarymanifestationshavebeen reportedin the genitalia, gastrointestinal tract, intraspinal region, and centralnervoussystem,andtheassociationbetween paracoc-cidioidomycosisandcancerandHIVhasbeensuggested.Joint involvementisrarewithno specificpattern orradiological injury.2
Wereportacaseofparacoccidioidomycosisinwhichthe patient’sinitialsymptomswerehoarsenessand oligoarthri-tis. Anultrasound (US)was performed as an extension of thephysicalexaminationforpossibledifferential diagnosis ofother diseases that may produce similar joint changes. Articular manifestationsofparacoccidioidomycosis include carpaltunnelsyndrome,association withgoutyarthritisin theproximalphalanxofthehallux,andpyoarthritisevenin theabsenceofimmunosuppressionriskfactors.3,4
Osteoarticular involvement in paracoccidioidomycosis is variable, with 2.2–4% of bones and joints, and in the acute/subacute form of the disease it accounted for 20–26.4% of paracoccidioidomycosis cases.5,6 Skin
involve-mentpresentshistologicallyaspapillomatosis,with epider-malproliferationandformationofmicroabscesses.7
Interestingly, inthis clinical case we performed guided ultrasoundtocollect articularmaterial,whichresultedina moreaccurate diagnosis and detectionof previously unre-ported ecotextural changes and cutaneous manifestations suchasmicroabscesses.
Case
report
Thepatientwasa55-year-oldman,residentintheruralarea, stateofSãoPaulo,Brazilwithasix-monthhistoryofjointpain. Hepresentedwithasymmetricinflammatorypaininthe leftwristandinthefingers,mostlyinthe1strightdistal inter-phalangeal(DIP)and3rdproximalinterphalangeal(PIP)joints, associatedwithhoarseness,whichstartedatthesametimeas theothersymptoms.Inaddition,hereportedlosing3kgsince theonsetofsymptoms.Thepatientdeniedfeverorcontact withpeoplewithcontagiousdiseases.
On physicalexamination, hehad hoarseness,increased volumeandtemperatureonpalpation,inadditionto hyper-emiainthepalmandthenareminenceoftheleftwristand 1strightdistalinterphalangealjoint.
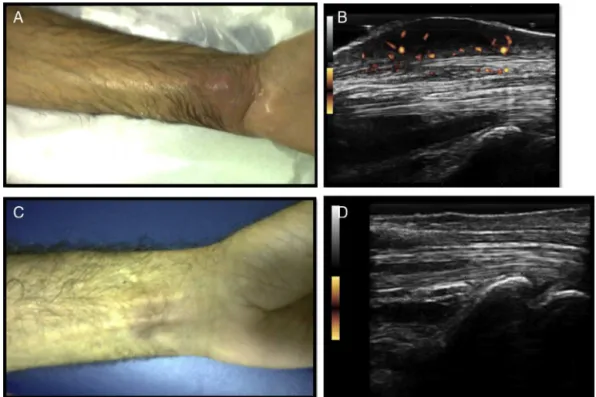
As aregular procedure in ourpractice, weperformed a musculoskeletal ultrasound (MSUS) asan extensionof the physicalexamination,whichshowedhypoechoic, heteroge-neous collection insubcutaneous planes, extendingto the flexortendonsoftheleftwristandfirstrightDIP, character-izingtenosynovitisandsynovitisindorsalrecessofthe1st rightDIPand3rdrightmetacarpophalangeal(MCP)joints,with importantinflammatoryactivity,shownbythe presenceof intensepowerDopplersignal(PD)(Figs.1and2).
WeperformedanUS-guidedpunctureofthecollectionand sentthematerialtothelaboratoryforbacillitests,fungaland bacterialcultures,and directmycological examination.The resultswerereturnedquickly,anddirectmycological exam-inationwaspositiveforParacoccidioidesbrasiliensis.Serologic testsforParacoccidioidesspp.werenotrealizedandbloodand wristsecretioncultureswerenegativeforMycobacteriumspp. andfungi.
On further investigation, laryngoscopy revealed glottic cleft,chestradiographthickreticularpatternaffectingboth lungs,chestcomputedtomography(CT)scanwithcavitations (Fig.3).ThepatientrefusedHIVtesting.
Fig.1–(A).LongitudinalUSimageofthepalmarrecessofthe1strightinterphalangeal(DIP)joint,showingsubcutaneous hypoechoiccollectioninvolvingtheflexordigitorumprofundustendonand(B)transversescanwithpositivePDsignal.US imageshowingdorsalrecesssynovitiswithpositivePDsignalof(C)1strightinterphalangeal(DIP)and(D)3rdright
r e v b r a s r e u m a t o l . 2016;56(1):75–78
77
Fig.2–(A)Palmaraspectoftheleftwristshowingafloatinglump.(B)USimageofthepalmarrecess,withsubcutaneous hypoechoiccollectioninvadingflexortendonsandpresenceofPDsignal.(C),Palmaraspectoftheleftwristaftertreatment. (D)USimageofthepalmarrecessoftheleftwrist,showingnochangesinflexortendonsaftertreatment.
Thepatient’streatmentcommencedwith sulfamethoxa-zole400mg/trimethoprim 80mg,two tablets three times a day.
Three months after treatment, US images showed the improvementofflexortendontenosynovitisintheleftwrist andsubcutaneouscollection,withoutPDsignal(Fig.2).
Kochbacillusandbacterialcultureresultswerenegative. Thepatientcurrentlyundergoesfollow-upinourinstitution.
Discussion
Paracoccidioidomycosis most commonly manifests as a chronicsystemicmycosisinadults,affectingthelungsand
Fig.3–ChesthighresolutionCTscan,sliceof
512×512pixels,ina55-year-oldman,Caucasian,resident
intheruralareaandjointpainshowingcavitationsinboth lungs,indicatedbythearrows.
upperrespiratory tract.8 Additionally, osteoarticular lesions
occurinallagegroups,butaremorefrequentinyoung sub-jects and,as inother clinicalpresentations ofthedisease, malesaremorefrequentlyaffected.Therearenoknownrisk factorsforthiskindofinvolvement,butlocalizedtraumasare believedtofacilitatetheestablishmentofthefungusinthe osteoarticularsystemduringfungemia.2
Many patientsaresickcarriersbecause ofanimbalance betweentheproductionofTh1andTh2lymphocytes,witha predominanceofthelatter,andcytokinessuchasIL-4,IL-5, IL-10,andIL-18thatpromotegranulomadisruption.9–12
Thereversedhalosignwithpneumonitisand reorganiza-tioninthechestCTscanishighlysuggestiveoflunginfection by paracoccidioidomycosis, even though other fungal and granulomatous infections may have similar symptoms.13
Directmycologicalexaminationisthesimplest,least expen-sive laboratory diagnosis, but negative results should be followedbyfungalcultureandmorespecifictestssuchasPCR andELISA.14
The treatment is prescribed according to the economic conditions of patients and availability of medications in the primary care network. However, the duration and the choice of the drug to treatment are still unclear. Both itraconazol 200mg/day for 6–9 months inmild forms and 12–18 months in moderate forms, or sulfamethoxazole 800–1.200mg+trimethoprim 160–240mg every 12h for 12 months in mild forms and 18–24 months in moderate formsareindicated.15
78
r e v b r a s r e u m a t o l . 2016;56(1):75–78oflowerrespiratorytractsymptoms,whichcouldbedetected onlyincomplementaryexams.Analysisofthefluiddrained fromthe wristabscesshelpedcompletethe diagnosis.The jointchangesdetectedbyhigh-resolutionultrasoundshowed greatsynovialinvolvementand subcutaneousinvolvement. However,nobonedamage,themostfrequentosteoarticular manifestation,norulcerationsinskinormucosacausedby fungaldisseminationweredetected,probablyduetotheearly diagnosis.
Inconclusion,ultrasoundexamsshouldbepartofroutine medicalcareasanextensionofrheumatologicphysical exam-inationtohelpformulatemoreaccuratedifferentialdiagnoses inpatientswithmono-oroligoarthritis,mainlyininfectious arthropathiessuchas tuberculosis,leprosy,septicarthritis, spondyloarthropathies,andalsoparacoccidioidomycosis.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. Queiroz-TellesF,EscuissatoDL.Pulmonary
paracoccidioidomycosis.SeminRespirCritCareMed. 2011;32:764–74.
2. MendesRP.Boneandjointlesions.Paracoccidioidomycosis. 2nded.BocaRaton:CRCPress;1994.p.331–8.
3. Bonilla-AbadíaF,VélezJD,Zárate-CorreaLC,CarrascalE, GuarínN,Casta ˜neda-RamírezCR,etal.Overinfectionby Paracoccidioidesbrasiliensisingoutycrystalarthritis.CaseRep Med.2012:1–3.
4.SaccenteM,WoodsGL.Clinicalandlaboratoryupdateon blastomycosis.ClinMicrobiolRev.2010;23:367–81.
5.TradHS,TradCS,EliasJJr,MugliaVF.Radiologicalreviewof 173consecutivecasesofparacoccidioidomycosis.RadiolBras. 2006;39:175–9.
6.Bellissimo-RodriguesF,BollelaVR,DaFonsecaBA,Martinez R.Endemicparacoccidioidomycosis:relationshipbetween clinicalpresentationandpatients’demographicfeatures. MedMycol.2013;51:313–8.
7.CostaMAB,CarvalhoTN,AraújoJúniorCR,BorbaAOC,Veloso GA,TeixeiraKS.Extra-pulmonarymanifestationsof
paracoccidioidomycosis.RadiolBras.2005;38:45–52. 8.Sant’AnnaGD,MauriM,ArrarteJL,CamargoHJr.Laryngeal
manifestationsofparacoccidioidomycosis(SouthAmerican blastomycosis).ArchOtolaryngolHeadNeckSurg.
1999;125:1375–8.
9.FortesMR,MiotHA,KurokawaCS,MarquesME,MarquesSA. Immunologyofparacoccidioidomycosis.AnBrasDermatol. 2011;86:516–24.
10.BenardG.Anoverviewoftheimmunopathologyofhuman paracoccidioidomycosis.Mycopathologia.2008;165:209–21. 11.deBritoT,FrancoMF.Granulomatousinflammation.RevInst
MedTropSaoPaulo.1994;36:185–92.
12.CorvinoCL,MamoniRL,FagundesGZ,BlottaMH.Serum interleukin-18andsolubletumournecrosisfactorreceptor2 areassociatedwithdiseaseseverityinpatientswith paracoccidioidomycosis.ClinExpImmunol.2007;147:483–90. 13.MarchioriE,ZanettiG,HochheggerB,IrionKL,CarvalhoAC,
GodoyMC.Reversedhalosignoncomputedtomography: state-of-the-artreview.Lung.2012;190:389–94.
14.TelesFR,MartinsML.Laboratorialdiagnosisof
paracoccidioidomycosisandnewinsightsforthefutureof fungaldiagnosis.Talanta.2011;85:2254–64.