Work developed in the Laboratory of Physiology, Hospital for Rehabilitation of Craniofacial Anomalies, Universidade de São Paulo – USP – São Paulo (SP), Brazil. (1) Graduate Program in Rehabilitation Sciences, Hospital for Rehabilitation of Craniofacial Anomalies, Universidade de São Paulo – USP – São Paulo (SP), Brazil. (2) Graduate Program (Master) in Rehabilitation Sciences, Hospital for Rehabilitation of Craniofacial Anomalies, Universidade de São Paulo – USP – São Paulo (SP), Brazil.
Conflicts of interest: No
Author´s contributions: APF: lead author, participation in the original study idea, data collection, data analysis and the writing of the article; CVDZ: participa-tion in statistical data analysis and the writing of the results; KFG: participation in the statistical analysis and the writing of the article; RPY: participation in data collection and the writing of the article; and IEK: research group leader, participation in the original study idea and the writing of the article.
Correspondence address: Ana Paula Fukushiro. R. Sílvio Marchione, 3/20, Vila Universitária, Bauru (SP), Brazil, CEP: 17012-900. E-mail: anapaulaf@usp.br Received: 4/25/2012; Accepted: 6/5/2013
Nasopharyngeal dimensions and respiratory symptoms
after pharyngeal flap surgery in children and adults
Dimensões nasofaríngeas e sintomas respiratórios após a cirurgia
de retalho faríngeo em crianças e adultos
Ana Paula Fukushiro1, Carmen Vivian Domingues Zwicker2, Katia Flores Genaro1, Renata Paciello Yamashita1,
Inge Elly Kiemle Trindade1
ABSTRACT
Purpose: To investigate the influence of age on nasopharyngeal di-mensions and respiratory symptoms in patients undergoing surgery to correct velopharyngeal insufficiency using the pharyngeal flap tech-nique. Methods: A sample comprising 103 individuals divided into three groups: children (6-12 years old), young adults (18-30 years old) and middle-aged adults (≥ 40 years old). This was a retrospective study that analyzed the values for the nasopharyngeal area (pressure-flow technique, reference value: 0.570 cm2) and the symptoms of oral respi-ration, snoring and respiratory difficulties during sleep. The values were obtained, on average, 12 months after surgery. The nasopharyngeal area was compared between the groups using analysis of variance, and res-piratory symptoms were compared using the chi-squared test (p<0.05). Results: The mean nasopharyngeal area values after surgery were 0.527±0.215 cm2, 0.599±0.213 cm2 and 0.488±0.276 cm2 for children, young adults and middle-aged adults, respectively, with no differences between groups. The proportions of oral respiration, snoring and brea-thing difficulty during sleep were, respectively, 66%, 69% and 9% in children; 51%, 49% and 7% in young adults; and 75%, 75% and 19% in middle-aged adults, with a higher frequency of snoring in middle-aged adults. Conclusion: Age did not affect nasopharyngeal dimensions in the presence of a pharyngeal flap, but it was an aggravating factor for respiratory symptoms, especially in older individuals.
Keywords: Cleft palate; Velopharyngeal insufficiency; Surgery, oral; Signs and symptoms, Respiratory; Rhinomanometry
RESUMO
Objetivo: Verificar a influência da idade sobre as dimensões nasofarín-geas e os sintomas respiratórios em pacientes submetidos à cirurgia para a correção da insuficiência velofaríngea pela técnica de retalho faríngeo. Métodos: Amostra formada por 103 indivíduos distribuídos em três grupos: crianças (6 a 12 anos), adultos jovens (18 a 30 anos) e adultos de meia-idade (≥40 anos). Trata-se de estudo retrospectivo que analisou os valores da área nasofaríngea (técnica fluxo-pressão, valor de referência 0,570 cm2) e os sintomas de respiração oral, ronco e dificuldade respira-tória durante sono, obtidos, em média, 12 meses após a cirurgia. A área nasofaríngea foi comparada entre os grupos por análise de variância e os sintomas respiratórios pelo teste Qui-quadrado (p<0,05). Resultados: Os valores médios da área nasofaríngea após a cirurgia foram 0,527±0,215 cm2, 0,599±0,213 cm2 e 0,488±0,276 cm2,respectivamente para crianças, adultos jovens e adultos de meia-idade, não havendo diferença entre os grupos. As proporções de respiração oral, ronco e dificuldade respiratória durante o sono foram, respectivamente, 66%, 69% e 9% nas crianças, 51%, 49% e 7% nos adultos jovens e 75%, 75% e 19% nos adultos de meia-idade, com maior frequência de ronco nos adultos de meia-idade. Conclusão: A idade não interferiu nas dimensões nasofaríngeas na presença de retalho faríngeo, mas foi um fator agravante de sintomas respiratórios, principalmente nos indivíduos mais velhos.
INTRODUCTION
Cleft lip/palate is a congenital deformity that can manifest in the lip, palate or both structures. Reconstructive surgery is re-quired to correct this abnormality. Cheiloplasty and palatoplasty are the first surgeries performed during the long and complex treatments which, in conjunction with other therapeutic appro-aches, are critical for patient rehabilitation(1).
A cleft palate is considered the most frequent cause of velopharyngeal insufficiency (VPI), a structural change in the velopharyngeal mechanism. The most common symptom of VPI is hypernasality, which is associated with nasal air emission and low intraoral air pressure(2-4).
It is generally agreed that palatoplasty should have the functional purpose of improving conditions for the velum to help the velopharyngeal mechanism. However, in many cases, even after primary corrective surgery, VPI symptoms persist, requiring a secondary procedure(5,6). Surgery using the
supe-riorly based pharyngeal flap technique is one of the methods most frequently employed to correct VPI. The technique con-sists of building a bridge of myomucosal tissue between the velum and the posterior pharyngeal wall, bounded by two side orifices that allow nasal breathing. The purpose of the flap is to create a mechanical obstruction to the airflow to eliminate hypernasality and nasal air emission, with increased intraoral pressure(7) during speech production.
Several studies have demonstrated the great success of pha-ryngeal flap surgery in reducing or eliminating VPI symptoms in speech, with success rates varying between 25% and 98% (8-10). However, the pharyngeal flap is also associated with upper
airway impairment, which may cause hyponasality, chronic nasal obstruction, snoring and obstructive sleep apnea, symp-toms that interfere with respiratory function and, consequently, quality of life(11-14).
It is also important to consider that a cleft lip/palate deter-mines nasal deformities that often reduce the dimensions of the nasal cavity(15) and increase nasal resistance to respiratory
airflow. It is therefore possible that in these cases, the placement of a flap in the velopharyngeal region may further aggravate impaired nasal patency(16).
Some studies have conducted surveys of clinical symptoms of respiratory obstruction, determining the area of the velopha-ryngeal orifice and using instrumental assessment to evaluate the effect of pharyngeal flap surgery on breathing in individuals with a cleft palate(14,17,18).
A preliminary sample showed that the pharyngeal flap had a variable effect on the nasal airway(18), and both positive
and negative changes were induced by the flap. The authors attributed this result to the presence of prior nasal obstruction, found in five of seven patients, and confirmed that the flap further decreased the nasal airway, which would explain the appearance of such breathing difficulties as snoring, chronic nasal obstruction and obstructive sleep apnea.
In studying sleep-disordered breathing in middle-aged adults who had undergone surgery to correct VPI using a pharyngeal flap, one study reported oral respiration, snoring and episodes of respiratory obstruction in 53% of cases, confirming that the pharyngeal flap can contribute to the worsening of respiratory disorders in this age group(19). In
young adults, the effect of the pharyngeal flap on the nasal and nasopharyngeal dimensions was investigated and corre-lated with respiratory complaints, showing the emergence or worsening of these complaints in 55% of cases in the short term and 36% in the long term. In an aerodynamic evaluation, a more pronounced decrease in nasopharyngeal dimensions was observed in patients who only reported respiratory com-plaints after surgery, highlighting the importance of moni-toring surgical results using objective measures(14). Another
study involving children analyzed respiratory symptoms and investigated the surgical complications of the pharyngeal flap, identifying oxygen desaturation in 8% of the sample and positive findings of obstructive sleep apnea in 3% six months after surgery(20).
In terms of VPI correction, surgery should be performed as soon as there is good nasal patency. However, the effects of the pharyngeal flap technique on respiration and the technique’s correlation with velopharyngeal orifice dimensions in different age groups is a subject that has been minimally explored to date. In addition, one must consider that respiratory changes related to nasopharyngeal obstruction during sleep increase with age(21).
Snoring during sleep, episodes of obstructive sleep apnea and other daytime symptoms manifest themselves most often after the age of 40 years(21-23).
The purpose of this study was therefore to determine the influence of age on nasopharyngeal dimensions and respiratory symptoms in patients who underwent surgery to correct velo-pharyngeal insufficiency using the velo-pharyngeal flap technique.
METHODS
This was a retrospective and cross-sectional study. It recei-ved approval from the Ethics Committee on Human Research of the Hospital for Rehabilitation of Craniofacial Anomalies of the Universidade de São Paulo (USP), protocol number 168/2009.
Initially, through convenience sampling and in accordance with the institution’s service order, the records of individuals with cleft palate and who had undergone surgery for VPI correction using the pharyngeal flap technique were selected. Cases in the sample that presented syndromes, neurological changes and residual fistula of the palate were excluded, as were cases that had undergone other surgical procedures after pharyngeal flap placement that could interfere with nasopha-ryngeal or nasal patency, such as secondary surgical revision and nasal surgery.
old (12 females and 20 males), 55 young adults between 18 and 30 years old (31 females and 24 males) and 16 middle--aged adults aged 40 years or over (8 females and 8 males). Information on these cases regarding the nasopharyngeal area and the presence of signs and symptoms of respiratory changes was collected on average 12 months after placement of the pharyngeal flap; this information was obtained from the institution’s medical records.
The nasopharyngeal dimensions were estimated by me-asuring the area of the velopharyngeal orifice during nasal breathing at rest via the pressure-flow technique, utilizing the PERCI-SARS computerized system Version 3.30 (Microtronics Corp®.). This technique relies on the principle that the area of an orifice can be estimated by simultaneously measuring the differential pressure between the two sides of the orifice and the airflow that passes through it(24). Thus, during several breathing
cycles, a catheter positioned in the oral cavity and another in one of the nostrils used a nasal shutter to measure the static air pressure, which was transmitted to pressure transducers. At the same time, a plastic tube connected to a heated pneumo-tachograph and linked to a pressure transducer was placed in the other nostril, the one with greater flow, to measure nasal airflow. The signals from the three transducers (nasal pressure, oral pressure and nasal airflow) were sent to the PERCI system for analysis with specificsoftware.
The mean reference value used was 0.570 cm2, as proposed
in a study conducted on normal adults(25). Areas smaller than
0.570 cm2 were therefore deemed to be probable
nasopharyn-geal obstructions.
The respiratory signs and symptoms survey was made con-ducted using questions on a survey sheet, which was applied routinely and filed in the medical record. The questions were based on the questionnaire proposed by Caouette-Laberge et al(11) and were considered information relating to daytime oral
respiration and/or oral respiration during sleep, snoring during sleep and difficulty breathing during sleep. Only reports of wor-sening preexisting symptoms or the onset of respiratory com-plaints that were not reported before surgery were considered. The significance of the differences between the three age groups was verified using analysis of variance with one criterion for the nasopharyngeal area and using the chi-squared test for respiratory symptoms. The results were considered significant if p<0.05.
RESULTS
In relation to the nasopharyngeal area, the comparison of values showed no difference among the three study groups (p>0.05). Considering the reference value of 0.570 cm2 for
the nasopharyngeal area, the group of children and the group of middle-aged adults had mean values lower than expected. One of the children had not undergone the rhinomanometric examination (Table 1).
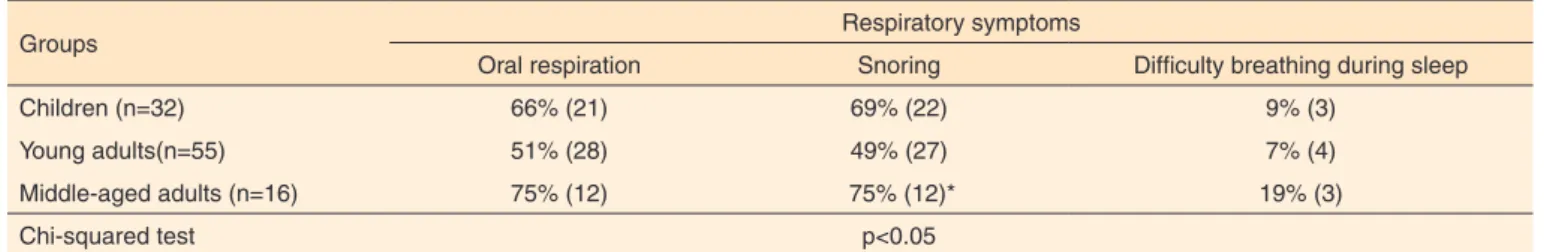
Regarding the survey of respiratory symptoms reported after surgery, there were reports of oral respiration, snoring and breathing difficulties during sleep in all groups. The comparison between the groups for each symptom indicated a difference with respect to snoring, which was reported more frequently by middle-aged adults (p<0.05) (Table 2).
DISCUSSION
The study of the effect of pharyngeal flap surgery on respi-ration is of fundamental importance in analyzing the surgical success of this procedure. Although many studies have reported surgical outcomes solely based on VPD symptoms, research on the occurrence of respiratory symptoms should always be valued. It is known that such symptoms as snoring and a mild sensation of nasal obstruction are often observed during the immediate postoperative period of pharyngeal flap surgery because of the reduced nasopharyngeal space caused by edema. However, when these symptoms persist for a long time and are compounded by other factors, such as oral respiration, episodes of obstructed breathing during sleep and daytime symptoms, such as excessive tiredness, headaches and drowsiness, the patient should be carefully evaluated.
The observation and investigation of respiratory signs and
Table 2. Relative and absolute frequency of respiratory symptoms after pharyngeal flap surgery
Groups Respiratory symptoms
Oral respiration Snoring Difficulty breathing during sleep
Children (n=32) 66% (21) 69% (22) 9% (3)
Young adults(n=55) 51% (28) 49% (27) 7% (4)
Middle-aged adults (n=16) 75% (12) 75% (12)* 19% (3)
Chi-squared test p<0.05
*Chi-squared test indicating greater frequency among middle-aged adults
Table 1. Mean and standard deviation of the nasopharyngeal area (cm2) after pharyngeal flap surgery
Groups Nasopharyngeal area
(cm2) p-value
Children (n=31) 0.527±0.215
p>0.05
Young adults (n=55) 0.599±0.213
Middle-aged adults (n=16) 0.488±0.276
symptoms should therefore be characterized as clinical prac-tice in services that use the pharyngeal flap, and the effects of pharyngeal flap surgery on breathing should be routinely evaluated in a subjective and instrumental manner(14,26). Based
on this assumption, this study aimed to verify the effect of age on nasopharyngeal dimensions and respiratory signs and symp-toms in patients with cleft lip/palate who underwent pharyngeal flap surgery. The study compared the results obtained across three different age groups because surgery may be indicated for different ages, from six years onwards.
Ideally, surgery should take place as early as possible to mi-nimize speech impediments. However, because of such factors as general health, dento-occlusal changes and the presence of compensatory articulations, surgery can take place later.
No difference was found when comparing the mean naso-pharyngeal area values among the three groups. It is noteworthy, however, that slightly lower values with a mean of 0.488 cm2
were observed in the group of middle-aged adults. Similarly, when comparing the values obtained with the reference value of 0.570 cm2, a noticeable reduction was observed in the same
group. The nasopharyngeal area of the young adults showed no evidence of obstruction.
A recent study performed a similar analysis of the rela-tionship between the nasopharyngeal area and respiratory symptoms in young adults (mean: 20 years old) who underwent the same surgical procedure. That study found a higher fre-quency of reported respiratory symptoms in patients with a nasopharyngeal area below 0.550 cm2. The authors concluded
that values below 0.550 cm2 may be related to a pharyngeal
flap obstruction and would call for a more careful evalua-tion(14). Because of the nature of the flap to act as a mechanical
obstruction preventing the escape of the expiratory air stream during speech, the reduction of the nasopharyngeal space is an expected result at any age. However, this reduction should not be excessive to the point of triggering respiratory symptoms that compromise quality of life.
In the analysis of the proportion of respiratory symptoms reported by the three age groups, differences were only found for snoring, which occurred in 75% of middle-aged adults, 69% of children and 49% of young adults. The fact that these symptoms occurred most frequently in the older population confirms the results of studies that have established consensus on the intensification of respiratory symptoms, especially sno-ring and obstructive sleep apnea, as age increases(21-23).
Snoring can be defined as a fricative noise originating in the soft tissues of the upper airways. It results from the vibration of the uvula and palate and occasionally the lateral pharyngeal wall, epiglottis and base of tongue during sleep. It is very com-mon in middle-aged men and in women after menopause(27).
The symptom is present in 90% to 95% of obstructive sleep apnea syndrome (OSA) cases.
One study found a prevalence of sleep-disordered brea-thing in middle-aged adults (≥40 years) who had undergone
pharyngeal flap surgery, including isolated or combined symptoms such as oral respiration, snoring and episodes of respiratory obstruction. In 53% of cases, there was also evidence of associated daytime symptoms, such as excessive sleepiness, headaches, constant fatigue, hypertension and obesity. The study authors concluded that the pharyngeal flap may contribute to the worsening of respiratory disorders in this age group(19).
In patients over 40 years with a pharyngeal flap, snoring is not only be associated with the presence of the flap but also with the effects of age, which indicates the importance of close monitoring of this population and of measures that prevent symptoms or stop them from worsening, such as correct posi-tioning during sleep, weight and neck circumference control and the adoption of healthy habits.
Although a difference could not be established between the three groups regarding oral respiration symptoms and breathing difficulties during sleep, there was a tendency for middle-aged adults to have more frequent symptoms, especially sleep breathing difficulties. The proportion of individuals re-porting difficulty breathing during sleep (19%) is considered high from a clinical point of view because given this severity of the symptom, it can be a strong indicator of obstructive sleep apnea. The gold standard test to confirm these findings is polysomnography.
According to the literature, the occurrence of respiratory changes after pharyngoplasty is extremely diverse, ranging from 4% to 92%(12-14). Such diversity may be related to the
methodology used, the age of the population studied and the criteria used to define the presence of respiratory changes, taking into account each patient’s individual tolerance of symptoms after surgery.
Another result observed in this study was the fact that children have a higher frequency of symptoms than young adults do. Some factors that may justify this fact could also be investigated, such as the presence of a higher incidence of upper airway infections(28) and hypertrophic tonsils and adenoids in
this age group(29), which can aggravate respiratory symptoms(30).
Furthermore, the presence in the children’s group of a caregiver or other person responsible for information about symptoms favors a detailed account of respiratory signs and symptoms during sleep, which is not available in the case of many young adults. In such cases, the occurrence of such symptoms may be underestimated because the sleep of young adults is rarely observed by others.
Indications for pharyngeal flap surgery should be evaluated as early as possible to eliminate or minimize speech symptoms and the concomitant psychosocial effects. Rigorous and sys-tematic lifelong monitoring of these cases should be part of the management of respiratory symptoms. Furthermore, other surgical treatments that are considered more physiological from an anatomical point of view and restorative procedures to correct velopharyngeal insufficiency can be used as efficient and preventative alternatives for this population.
CONCLUSION
Age at the time of pharyngeal flap surgery did not affect na-sopharyngeal dimensions, but it contributed to the occurrence of respiratory symptoms after surgery, especially in older subjects.
REFERENCES
1. Bertier CE, Trindade IEK, Silva Filho OG. Cirurgias primárias de lábio e palato. In: Trindade IEK, Silva Filho OG. Fissuras labiopalatinas: uma abordagem interdisciplinar. São Paulo: Santos; 2007. p. 73-85.
2. Genaro KF, Fukushiro AP, Suguimoto MLFCP. Avaliação e tratamento dos distúrbios da fala. In: Trindade IEK, Silva Filho OG. Fissuras labiopalatinas: uma abordagem interdisciplinar. São Paulo: Santos; 2007. p. 109-22.
3. Kummer AW. Velopharyngeal dysfunction (VPD) and resonance disorders. In: Kummer AW. Cleft palate and craniofacial anomalies: the effects on speech and resonance. San Diego: Singular; 2001. p. 145-76.
4. Peterson-Falzone SJ, Hardin-Jones MA, Karnell MP. Communication disorders associated with cleft palate. In: Peterson-Falzone SJ, Hardin-Jones MA, Karnell MP. Cleft palate speech. 3rd ed. Saint
Louis: Mosby; 2001. p.162-98.
5. Rocha DL. Tratamento cirúrgico da insuficiência velofaríngea. In: Trindade IEK, Silva Filho OG. Fissuras labiopalatinas: uma abordagem interdisciplinar. São Paulo: Santos; 2007. p.145-63. 6. Seagle MB, Mazaheri MK, Dixon-Wood VL, Williams WN.
Evaluation and treatment of velopharyngeal insufficiency: the University of Florida experience. Ann Plastic Surg. 2002May;48(5):464-70.
7. Berkowitz S. Variations in nasopharyngeal skeletal architecture. In: Berkowitz S. Cleft lip and palate: diagnosis and management. 2nd ed.
New York: Springer; 2005. p.621-42.
8. Morris HL, Bardach J, Jones D, Christiansen JL, Gray SD. Clinical results of pharyngeal flap surgery: the Iowa experience. Plast Reconstr Surg. 1995Apr;95(4):652-62.
9. Dailey SA, Karnell MP, Karnell LH, Canady JW. Comparison of resonance outcomes after pharyngeal flap and furlow double-opposing z-plasty for surgical management of velopharyngeal incompetence. Cleft Palate Craniofac J. 2006Jan;43(1):38-43. 10. Fukushiro AP, Trindade IEK. Nasometric and aerodynamic
outcome analysis of pharyngeal flap surgery for the management of
velopharyngeal insufficiency. J Craniofac Surg. 2011Sep;22(5):1647-51.
11. Caouette-Laberge L, Egerszegi EP, de Remont AM, Ottenseyer I. Long-term follow-up after division of a pharyngeal flap for severe nasal obstruction. Cleft Palate Craniofac J. 1992Jan;29(1):27-31. 12. Wells MD, Vu TA, Luce EA. Incidence and sequelae of nocturnal
respiratory obstruction following posterior pharyngeal flap operation. Ann Plast Surg. 1999Sep;43(3):252-7.
13. Liao YF, Chuang ML, Chen PKT, Chen NH, Yun C, Huang CS. Incidence and severity of obstructive sleep apnea following pharyngeal flap surgery in patients with cleft palate. Cleft Palate Craniofac J. 2002May;39(3):312-6.
14. Yamashita RP, Trindade IEK. Long-term effects of pharyngeal flaps on the upper airways of subjects with velopharyngeal insufficiency. Cleft Palate Craniofac J. 2008Jul;45(4):364-70.
15. Fukushiro AP, Trindade IEK. Nasal airway dimensions of adults with cleft lip and palate: differences among cleft types. Cleft Palate Craniofac J. 2005Jul;42(4): 396-402.
16. Warren DW, Trier WC, Bevin AG. Effect of restorative procedures on the nasopharyngeal airway in cleft palate. Cleft Palate J. 1974Oct;11:367-73.
17. Smith BE, Skef Z, Cohen M, Dorf DS. Aerodynamic assessment of the results of pharyngeal flap surgery: a preliminary investigation. Plast Reconstr Surg. 1985Sep;76(3):402-10.
18. Witssel DL, Drake AF, Warren DW. Preliminary data on the effect of pharyngeal flaps on the upper airway in children with velopharyngeal inadequacy. Laryngoscope. 1994Jan;104(1):12-5.
19. Trindade IEK, Fukushiro AP, Yamashita RP, Sampaio ACM, Trindade Junior AS. Prevalence of sleep-disordered breathing in middle-aged cleft adults with pharyngeal flaps. In: Proceedings of the 10th International Congress on Cleft Palate and Related Craniofacial Anomalies. September 4-8, 2005 Durban, South Africa International Confederation for Cleft Palate and Related Craniofacial Anomalies. 2005:171.
20. Cole P, Banerji S, Hollier L, Stal S. Two hundred twenty-two consecutive pharyngeal flaps: an analysis of postoperative complications. J Oral Maxillofac Surg. 2008Apr;66(4):745-8. 21. Mazzotti DR, Guindalini C, Sosa AL, Ferri CP, Tufik S. Prevalence
and correlates for sleep complaints in older adults in low and middle income countries: a 10/66 Dementia Research Group study. Sleep Med. 2012Jun;13(6):697-702.
22. Silva A, Andersen ML, De Mello MT, Bittencourt LR, Peruzzo D, Tufik S. Gender and age differences in polysomnography findings and sleep complaints of patients referred to a sleep laboratory. Braz J Med Biol Res. 2008Dec;41(12):1067-75.
23. Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010May;11(5):441-6.
24. Warren DW, Dubois AB. A pressure-flow technique for measuring velopharyngeal orifice area during continuous speech. Cleft Palate J. 1964Jan;1:52-71.
nasal e faríngea. I Congresso Científico da USP; 1997 Nov 28-29; Bauru. Livro de Resumos. Bauru: USP; 1997.
26. Zuiani TBB, Trindade IEK, Yamashita RP, Trindade Junior AS. The pharyngeal flap surgery in patients with velopharyngeal insufficiency: perceptual and nasometric speech assessment. Braz J Dysmorphol Speech Disord. 1998;2(1):31-42.
27. Mancini MC, Aloe F, Tavares S. Apnéia do sono em obesos. Arq Bras Endócrinol Metab. 2000Feb;44(1):81-90.
28. Pitrez PMC, Pitrez JLB. Infecções agudas das vias aéreas superiores - diagnóstico e tratamento ambulatorial. J Pediatr. 2003;79(Supl.1):77-86.
29. Bonuck KA, Chervin RD, Cole TJ, Emond A, Henderson J, Xu L et al. Prevalence and persistence of sleep disordered breathing symptoms in young children: a 6-year population-based cohort study. Sleep. 2011Jul;34(7):875-84.