www.rpped.com.br
REVISTA
PAULISTA
DE
PEDIATRIA
EDITORIAL
In
time:
averting
the
legacy
of
kidney
disease
---
focus
on
childhood
Em
tempo:
evitando
as
consequências
da
doenc
¸a
renal
---
foco
na
infância
Julie
R.
Ingelfinger
a,∗,
Kamyar
Kalantar-Zadeh
b,
Franz
Schaefer
c,
on
behalf
of
the
World
Kidney
Day
Steering
Committee
♦aMassachusettsGeneralHospital,Boston,USA
bUniversityofCalifornia,Irvine,USA
cHeidelbergUniversityHospital,Heildelberg,Alemanha
Received5November2015
‘‘Forineveryadulttheredwellsthechildthatwas,and ineverychildthereliestheadultthatwillbe.’’
---JohnConnolly,TheBookofLostThings
Introduction
and
overview
The11thWorldKidneyDaywillbecelebratedonMarch10, 2016,aroundtheglobe.Thisannualevent,sponsoredjointly by the International Society of Nephrology (ISN) and the InternationalFederationof KidneyFoundations(IFKF), has becomeahighlysuccessfulefforttoinformthegeneral pub-licandpolicymakersabouttheimportanceandramifications ofkidneydisease.In2016,WorldKidneyDaywillbe dedi-catedtokidneydiseaseinchildhoodandtheantecedentsof adultkidneydisease,whichcanbegininearliestchildhood. Children who endure acute kidney injury (AKI) from a wide variety of conditions may have long-term sequelae thatcan leadtochronic kidney disease(CKD)many years later.1---4 Further,CKD inchildhood,muchofit congenital,
∗Correspondingauthor.
E-mail:myriam@worldkidneyday.org(J.R.Ingelfinger). ♦ PhilipKamTaoLi,GuillermoGarcia-Garcia,WilliamG.Couser,
TimurErk,JulieR.Ingelfinger,KamyarKalantar-Zadeh,Charles Ker-nahan, CharlotteOsafo, Miguel C. Riella, Luca Segantini,Elena Zakharova.
andcomplications from themany non-renal diseases that can affect the kidneys secondarily, not only lead to sub-stantialmorbidity andmortalityduringchildhoodbutalso resultinmedicalissuesbeyondchildhood.Indeed,childhood deathsfromalonglistofcommunicablediseasesare inextri-cablylinkedtokidney involvement.Forexample,children whosuccumbtocholeraandotherdiarrhealinfectionsoften die,notfromtheinfection,butbecauseofAKIinducedby volumedepletionandshock.Inaddition,asubstantialbody ofdataindicatesthathypertension,proteinuriaandCKDin adulthood have childhoodantecedents ---from asearly as in utero and perinatallife (see Table 1 for definitions of childhood).WorldKidneyDay2016aimstoheightengeneral awarenessthatmuchadultrenaldiseaseisactuallyinitiated inchildhood.Understandinghighriskdiagnosesandevents thatoccurinchildhoodhavethe potentialtoidentifyand intervenepreemptively in those peopleat higherrisk for CKDduringtheirlifetimes.
Worldwideepidemiologic dataonthespectrumof both CKD and AKI in children are currently limited, though increasinginscope.Theprevalence ofCKDinchildhoodis rare---andhasbeenvariouslyreportedat15---74.7per mil-lionchildren.3SuchvariationislikelybecausedataonCKD
areinfluencedbyregionalandculturalfactors,aswellasby themethodologyusedtogeneratethem.TheWorldHealth Organization(WHO)hasrecentlyaddedkidneyandurologic disease to mortality information tracked worldwide, and
http://dx.doi.org/10.1016/j.rppede.2015.12.001
Table1 Definitionsofstagesofearlylife.
Perinatalperiod 22completedweeksofgestationto Day7ofpostnatallife
Neonatalperiod BirthtoDay28ofpostnatallife Infancy Birthto1yearofage
Childhood 1yearofageto10yearsofage Adolescence 10yearsofageto19yearsofage
Notes:ThedatainthistableareasdefinedbytheWorldHealth
Organization.
Thereisvariationworldwideinhowthesestagesofearlylife aredefined.Somewoulddefine‘‘youngpeople’’asthoseage 24orless.IntheUnitedStates,childhoodisasawholedefined asgoingtoage21.
shouldbea valuablesource of suchdataover time--- yet WHOdoesnotposttheinformationbyagegroup.5Databases
suchastheNorthAmericanPediatricRenalTrialsand Col-laborativeStudies (NAPRTCS)6 theU.S. RenalDataSystem
(USRDS)7 andthe EDTAregistry8include dataonpediatric
end-stagerenaldisease,andsomeonCKD.Projectssuchas theItalKid9andChronicKidneyDiseaseinChildren(CKiD)10
studies,theGlobalBurdenofDiseaseStudy2013,aswellas registriesthat nowexistinmanycountriesprovide impor-tantinformation,andmoreisrequired.11
AKImayleadtoCKD,accordingtoselectedadult popula-tionstudies.12TheincidenceofAKIamongchildrenadmitted
toanintensivecareunitvarieswidely---from8%to89%.1The
outcome depends on the available resources. The results fromprojectssuchastheAWAREstudy,afive-nationstudyof AKIinchildrenareawaited.13Singlecenterstudies,aswell
asmeta-analysesindicatethatbothAKIandCKDinchildren accountfor aminorityofCKDworldwide.2,3However,itis
increasinglyevidentthatkidneydiseaseinadulthoodoften springsfromachildhoodlegacy.
Spectrum
of
pediatric
kidney
diseases
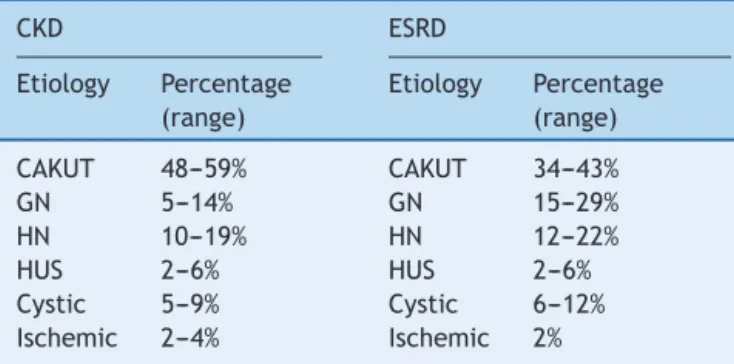
The conditionsthat account for CKD in childhood,witha predominance ofcongenitaland hereditarydisorders, dif-fersubstantially fromthosein adults.To date, mutations in more than 150 genes have been found to alter kidney developmentor specificglomerularor tubularfunctions.14
Mostof thesegeneticdisorders present during childhood, and many lead to progressive CKD. Congenital anomalies of the kidney and urinary tract (CAKUT) account for the largestcategoryofCKDinchildren(seeTable2)andinclude renalhypoplasia/dysplasiaandobstructiveuropathy. Impor-tant subgroups amongthe renal dysplasias are the cystic kidney diseases, which originate from genetic defects of the tubuloepithelial cells’ primary cilia. Many pediatric glomerulopathiesarecausedbygeneticoracquireddefects ofthepodocytes,theuniquecelltypeliningtheglomerular capillaries.Lesscommonbutimportantcausesofchildhood CKDareinheritedmetabolicdisorderssuchashyperoxaluria andcystinosis,andatypicalhemolyticuremicsyndrome,a thromboticmicroangiopathyrelatedtogenetic abnormali-tiesofcomplement,coagulationormetabolicpathways.
Invariousclassificationsitisnotclearhowtocategorize childrenwhohave sufferedAKIandapparentlyrecovered,
Table2 Etiologyofchronickidneydiseaseinchildren.2
CKD ESRD
Etiology Percentage (range)
Etiology Percentage (range)
CAKUT 48---59% CAKUT 34---43%
GN 5---14% GN 15---29%
HN 10---19% HN 12---22%
HUS 2---6% HUS 2---6%
Cystic 5---9% Cystic 6---12%
Ischemic 2---4% Ischemic 2%
CKD,chronickidneydisease;ESRD,childhoodonsetend-stage renaldisease; CAKUT,congenitalanomaliesofthekidneyand urinarytract;GN,glomerulonephritis;HN,hypertension;HUS, hemolyticuremicsyndrome.RarecausesincludecongenitalNS, metabolicdiseases,cystinosis.Miscellaneouscausesdependon howsuchentitiesareclassified.
ChronicKidneyDiseasedataarefromNorthAmericanPediatric RenalTrialsandCollaborativeStudies,theItalianRegistryand theBelgian Registry.Childhood onsetend-stage renal disease dataarefromANZDATA,ESPN/ERA-EDTA,UKRenalRegistryand theJapaneseRegistry.
or how and whether to include those children who have hadperinatalchallenges,likelyresultinginarelativelylow nephronnumber.
Among children with childhood-onset end-stage renal disease(ESRD)glomerulopathiesareslightlymoreand con-genitalanomalieslesscommon(Table2),duetothetypically more rapid nephron loss in glomerular disease. However, recent evidence suggests that many patients with milder forms of CAKUT may progress to ESRD during adulthood, peakinginthefourthdecadeoflife.15
Therearenationalandregionaldifferencesinthetypes and course of both AKI and CKD during childhood and beyond. Death from kidney disease is higher in develop-ing nations, and national and regional disparities in care and outcome must be addressed. Further, access to care is variable, depending on the region, the countryand its infrastructure.Byfocusingonkidney diseaseinchildhood, cost-effectivesolutionsmaybereached,astreatingdisease earlyandpreemptivelymaypreventlater,moreadvanced CKD. Expectations depend onthe availability of care and management. Treating children, even from infancy, who haveAKIandCKDthatrequiresrenalreplacementtherapy canbeeffectiveinmitigatingtheburdenofkidneydisease inadulthood.Doingsorequiresresourcesthatfocusonthe most expeditiousandcost-effective waystodeliveracute RRTinchildhood.
Congenital
kidney
disease
and
developmental
origins
of
health
and
disease,
renal
endowment
and
implications
arenotidentifieduntilmuchlater,whensymptomsdevelop. Whilegeneralizedscreeningforproteinuria,hematuriaand urinarytract infections arecarried out in some countries and regions, there is a lack of consensusas to its effec-tiveness.However,thereisgeneralagreementthatchildren withantenatalultrasoundstudiesthatindicatepossible gen-itourinaryanomalies,childrenwithafamilyhistoryofkidney disease, and children withsigns such as failure to thrive or a history of urinary tract infection, voiding dysfunc-tionor an abnormalappearingurine shouldbeexamined. Initial screening would include a focused physical exami-nation and a urine dipstick, formalurinalysis and a basic chemistrypanel,followedbyamorefocusedevaluationif indicated.
Depending on thediagnosis, definitive therapy may be indicated.However,theevidencethattherapywillslow pro-gressionof CKD inchildhoodremains limited. Angiotensin convertingenzyme inhibitors, angiotensin receptor block-ers, antioxidants and, possibly, dietary changes may be indicated, depending on the diagnosis. However, dietary changes need to permit adequate growth and develop-ment.TheESCAPEtrialprovidedevidencethatstrictblood pressurecontrolretardsprogressionofCKDinchildren irre-spectiveofthetypeofunderlyingkidneydisease.16
Someveryyoungchildrenmayrequirerenalreplacement therapyinearlyinfancy.Recentdatapooledfromregistries worldwide indicate good survival, even when dialysis is requiredfromneonatalage.2,17Kidneytransplantation,the
preferredrenalreplacementtherapy inchildren,is gener-allysuitableafter12monthsofage,withexcellentpatient andallograftsurvival,growthanddevelopment(Fig.1).
Evidenceisaccumulatingthatchildhood-onsetCKDleads toacceleratedcardiovascularmorbidityandshortenedlife expectancy.Ongoing largeprospectivestudies suchasthe (CardiovascularComorbidityinChildrenwithCKD(4C)Study areexpectedtoinformaboutthecausesandconsequences ofearlycardiovasculardiseaseinchildrenwithCKD.18
Inadditiontothosechildrenwithcongenitalkidney dis-ease,itisnowknownthatperinataleventsmayaffectfuture health in the absence of evident kidney disease in early life.19 Premature infants appearto beparticularly at risk
forkidneydiseaselongaftertheyareborn,basedbothon observational cohort studies, as well as on case reports. Increasinglyprematureinfantssurvive,includingmanyborn wellbeforenephrogenesisis complete.20 The limiteddata
availableindicatethatintheprocessofneonatalICUcare, suchbabiesreceivemanynephrotoxins,andthatthosedying priortodischargefromthenurseryhavefewerandlarger glomeruli.21 Additionally, thosesurvivinghaveevidenceof
renalimpairmentthatmaybesubtle.22Evenmore
concern-ing,abundantepidemiologicdataindicatethatpersonsborn attermbutwithrelativelylowbirthweightsmaybeathigh risk for hypertension,albuminuriaand CKDin laterlife.23
When direct measurementsarepursued,such persons, as adults,may have fewer nephrons, thus a low cardiorenal endowment.
InfocusingonchildrenforWorldKidneyDay,we would note that it is key to follow kidney function and blood pressure throughout life in those persons born early or small-for-dates.Bydoingso,andavoidingnephrotoxic med-icationsthroughoutlife,itmaybepossibletoavertCKDin manypeople.
Resources
and
therapeutics
for
children
---differences
from
therapeutics
in
adults
DisparitiesexistintheavailabilityofresourcestotreatAKI inchildrenandyoungpeople;consequently,toomany chil-dren and young adults in developing nations succumb if AKI occurs. To address the problem the ISN has initiated theSavingYoungLivesProject,whichaimsbothtoprevent AKIwithprompttreatmentof infectionand/or deliveryof appropriatefluidandelectrolytetherapy,andtotreatAKI whenitoccurs. This ongoing project inSubSaharanAfrica andSouthEastAsia,inwhichfourkidneyfoundations par-ticipate equally[IPNA (International PediatricNephrology Association),ISN(InternationalSocietyofNephrology),ISPD (InternationalSocietyforPeritonealDialysis),SKCF (Sustain-ableKidneyCareFoundation)],focusesonestablishingand maintainingcentersforthecareofAKI,includingthe provi-sionofacuteperitonealdialysis.ItlinkswiththeISN’s0by 25project,whichcallsonmemberstoensureby2025that nobodydiesfrompreventableandacutekidneyinjury.
Inviewofthepreponderanceofcongenitaland heredi-tarydisorders,therapeuticresourcesforchildrenwithCKD havehistoricallybeenlimitedtoafewimmunological condi-tions.Veryrecently,progressindrugdevelopmentinconcert withadvancesingeneticknowledgeanddiagnostic capabil-itieshasbeguntoovercomethelong-standing‘therapeutic nihilism’inpediatrickidneydisease.AtypicalHUS,long con-sidered ominous,with a high likelihood of progression to ESRDandpost-transplantationrecurrence,hasturnedinto a treatable condition --- withthe advent of a monoclonal antibody that specifically blocks C5 activation.24 Another
exampleis the useof vasopressin receptor antagonists to retardcystgrowthandpreservekidneyfunctionin polycys-tickidneydisease.25 Firstprovenefficaciousinadultswith
autosomaldominantpolycystickidneydisease,therapywith vaptansholdspromisealsofortherecessiveformofthe dis-ease,which presentsandoften progressestoESRDduring childhood.
However,patientbenefitfrompharmacologicalresearch breakthroughsisjeopardizedonaglobalscalebythe enor-mouscostofsomeofthenewtherapeuticagents.Thequest foraffordableinnovativetherapiesforrarediseaseswillbe akeyissueinpediatricnephrologyintheyearstocome.
Congenital Kidney Disease or Inherited Disorders
Acquired Kidney Disease
Contribution of nephron number
Contribution of life challenges
Late fetal Life Newborn Infant Toddler Child Adult Old age
Figure1 Thetypesandrisksofkidneydiseasechangeacrossthelifecycle.Thecontributionofnephronnumberincreasesover thelifecycle,inconcertwitheventsthatprovidedirectinsultsandchallengestokidneyhealth.
reliableinformationonthedemographicsandoutcomesof pediatricRRT,theInternationalPediatricNephrology Asso-ciation(IPNA)isabouttolaunchaglobalpopulation-based registry.Ifsuccessful,theIPNARRTregistrymightbecome arolemodelforglobaldatacollection.
Transition
from
pediatric
to
adult
care
Transitionofcareforadolescentswithkidney diseaseinto an adult setting is critical both for patients and their caregivers. Non-adherence is a too-frequent hallmark of transitionfrom pediatric toadult care for young patients with chronic disease states.26---28 Hence, considered steps
combinedwithsystematicallydefinedproceduressupported byvalidated pathways and credibleguidelines must bein placetoensuresuccessfuloutcomes.
In the process of change from pediatric toadult care ‘‘transition,’’ which should occur gradually, must be dis-tinguishedfrom‘‘transfer,’’ whichis often an abruptand mechanistic change in provider setting. Introducing the conceptoftransitionshouldbepreemptive,startingmonths toyearspriortothetargetedtime,aschildrenmove into adolescenceandadulthood.Theultimategoalistofostera strongrelationshipandindividualizedplaninthenew set-tingthatallowsthepatienttofeelcomfortableenoughto reportnon-adherenceandotherlapsesincare.
A transition plan must recognize that the emotional maturityofchildrenwithkidneydiseasemaydifferwidely. Assessmentofthecaregiverandthefamilystructureaswell ascultural,social,andfinancialfactorsatthetimeof tran-sitionarekey,includingarealisticassessmentofcaregiver burden.4 The appropriatetiming and format of transition
mayvarywidelyamongdifferentpatientsandindifferent settings;therefore,aflexibleprocesswithoutasetdateand evenwithoutadelineatedformatmaybepreferred.
Importantly,transitionmay needtobe slowed, paused or evenreversedtemporarily duringcrisessuchasdisease flares or progression, or if family or societal instability occurs.Arecentjointconsensusstatementbythe Interna-tionalSocietyofNephrology(ISN)andInternationalPediatric Nephrology Association (IPNA) proposed steps consistent withthepointsjustoutlined,aimingtoenhancethe transi-tionofcareinkidneydiseaseinclinicalpractice.29,30
Call
for
generating
further
information
and
action
Givenvulnerabilitiesofchildrenwithkidneydisease includ-ingimpactongrowthanddevelopmentandfuturelifeasan adult, and given the muchgreater proportion of children in developing nations facing resource constraints educat-ing everyone involved is imperative in order to realign communicationsandactions.31,32 Theseeffortsshould
fos-terregionalandinternationalcollaborationsandexchange of ideas between local kidney foundations, professional societies,othernot-for-profitorganizations,andstatesand governments, so as to help empower all stakeholders to improvethe health, well-beingandqualityof lifeof chil-drenwithkidneydiseasesandtoensuretheirlongevityinto adulthood.
Untilrecently,however,theWHOconsensusstatementon non-communicable diseases (NCD)included cardiovascular disease, cancer, diabetes andchronic respiratory disease, butnot kidneydisease.33,34 Fortunately,due, inpart,toa
globalcampaignledbytheISN,thePoliticalDeclarationon NCDs fromthe UnitedNations Summit in 2011mentioned kidneydiseaseunderItem19.35
mortality from NCD with a 10 year target population levelinitiativesfocusingonchangesinlifestyle(including tobaccousereduction,salt intakecontrol,dietaryenergy control,andalcoholintakereduction)andeffective inter-ventions(includingbloodpressure,cholesterolandglycemic control).
Heightened efforts are needed to realign and expand thesemultidisciplinary collaborationswith moreeffective focusonearlydetectionandmanagementofkidneydisease in children. Whereas the issues related tokidney disease maybeovershadowedbyotherNCDswithapparentlylarger public health implications such as diabetes, cancer, and cardiovascular diseases, our efforts should also increase educationandawarenessonsuchoverlappingconditionsas cardiorenalconnections,theglobalnatureoftheCKDand ESRDasmajorNCDs,andtheroleofkidneydiseaseasthe multiplier disease and confounder for other NCDs. White papers including consensusarticles and blueprint reviews byworldclassexpertscanservetoenhancethesegoals.36
Funding
Thestudyreceivednofunding.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.GoldsteinSL.Acutekidneyinjuryinchildrenanditspotential consequencesinadulthood.BloodPurif.2012;33:131---7. 2.Harambat J, Van Stralen KJ, Kim JJ, Tizard EJ.
Epidemiol-ogy of chronic kidney disease in children. Pediatr Nephrol. 2012;27:363---73.
3.WaradyBA,ChadhaV.Chronickidneydiseaseinchildren:the globalperspective.PediatrNephrol.2007;22:1999---2009. 4.FurthSL, ColeSR, Moxey-MimsM,KaskelF,MakR,Schwartz
G,etal.Designandmethodsofthechronickidneydiseasein children(CKiD)prospectivecohortstudy.ClinJAmSocNephrol. 2006;1:1006---15.
5.World Health Organization. Health statistics and informa-tion systems: estimates for 2000---2012; 2015. Available from:http://www.who.int/healthinfo/globalburdendisease/ estimates/en/index1.html[cited26.10.15].
6.NAPRTCS. NAPRTCS Annual Reports; 2015. Available from: https://web.emmes.com/study/ped/annlrept/annlrept.html [cited26.10.15].
7.Saran R, Li Y, Robinson B, Ayanian J, Balkrishnan R, Bragg-Gresham J, et al. US Renal Data System 2014 Annual Data Report:EpidemiologyofKidneyDiseaseintheUnitedStates. AmJKidneyDis.2015;65:A7.
8.ESPN/ERA-EDTA Registry. ESPN/ERA-EDTA Registry, European Registryfor Children on Renal Replacement Therapy; 2015. Available from: http://www.espn-reg.org/index.jsp [cited 26.10.15].
9.ArdissinoG,DaccòV,TestaS,BonaudoR,Claris-AppianiA,Taioli E,etal.Epidemiologyofchronicrenalfailureinchildren:data fromtheItalKidproject.Pediatrics.2003;111:e382---7. 10.WongCJ,Moxey-MimsM,Jerry-FlukerJ,WaradyBA,FurthSL.
CKiD(CKDinchildren)prospectivecohortstudy:a reviewof currentfindings.AmJKidneyDis.2012;60:1002---11.
11.Global Burden of Disease Study 2013 Collaborators. Global, regional,andnationalincidence,prevalence,andyearslived withdisabilityfor301acuteandchronicdiseasesandinjuriesin 188countries,1990---2013:asystematicanalysisfortheGlobal BurdenofDiseaseStudy2013.Lancet.2013;386:743---800. 12.CocaSG,SinganamalaS,ParikhCR.Chronickidneydiseaseafter
acute kidneyinjury: a systematic reviewand meta-analysis. KidneyInt.2012;81:442---8.
13.Basu RK, Kaddourah A, Terrell T, MottesT, Arnold P,Jacobs J,etal.AssessmentofWorldwide AcuteKidneyInjury,Renal AnginaandEpidemiologyincriticallyillchildren(AWARE):study protocolfor aprospectiveobservational study.BMC Nephrol. 2015;16:24.
14.EckardtKU,CoreshJ,DevuystO,JohnsonRJ,KöttgenA,Levey AS,etal.Evolvingimportanceofkidneydisease:from subspe-cialtytoglobalhealthburden.Lancet.2013;382:158---69. 15.WühlE,VanStralenKJ,VerrinaE,BjerreA, WannerC,Heaf
JG,etal. Timingand outcomeofrenalreplacementtherapy inpatients withcongenitalmalformations ofthekidney and urinarytract.ClinJAmSocNephrol.2013;8:67---74.
16.ESCAPE Trial GroupWühl E, Trivelli A, Picca S, Litwin M, Peco-Antic A, et al. Strict blood-pressure control and pro-gressionofrenalfailureinchildren.NEnglJMed.2009;361: 1639---50.
17.vanStralenKJ,Borzych-Du˙zalkaD,HatayaH,KennedySE,Jager KJ,VerrinaE,etal.Survivalandclinicaloutcomesofchildren startingrenalreplacementtherapyintheneonatalperiod. Kid-neyInt.2014:86.
18.QuerfeldU, AnaratA, BayazitAK, Bakkaloglu AS, BilginerY, CaliskanS,etal.TheCardiovascularComorbidityinChildren withChronicKidneyDisease(4C)study:objectives,design,and methodology.ClinJAmSocNephrol.2010;5:1642---8.
19.HoyWE,IngelfingerJR,HallanS,HughsonMD,MottSA,Bertram JF.Theearlydevelopmentofthekidneyandimplicationsfor futurehealth.JDevOrigHealthDis.2010;1:216---33.
20.FlynnJT,NgDK,ChanGJ,SamuelsJ,FurthS,WaradyB,etal. Theeffectofabnormalbirthhistoryonambulatoryblood pres-sureand diseaseprogression inchildrenwithchronic kidney disease.JPediatr.2014;165:154---62.
21.Rodríguez MM, Gómez AH, Abitbol CL, Chandar JJ, Duara S, Zilleruelo GE. Histomorphometric analysis of postnatal glomerulogenesis in extremely preterm infants. Pediatr Dev Pathol.2004;7:17---25.
22.AbitbolCL,BauerCR,MontanéB,ChandarJ,DuaraS, Zilleru-elo G. Long-term follow-up of extremely low birth weight infantswithneonatalrenalfailure.PediatrNephrol.2003;18: 887---93.
23.HodginJB,RasoulpourM,MarkowitzGS,D’AgatiVD.Verylow birth weight is a risk factor for secondary focal segmental glomerulosclerosis.ClinJAmSocNephrol.2009;4:71---6. 24.VerhaveJC,WetzelsJF,VandeKarNC.Novelaspectsof
atyp-icalhaemolyticuraemicsyndromeandtheroleofeculizumab. NephrolDialTransplant.2014;29Suppl.4:iv131---41.
25.TorresVE.Vasopressinreceptorantagonists,heartfailure,and polycystickidneydisease.AnnuRevMed.2015;66:195---210. 26.JarzembowskiT,JohnE,PanaroF,HeiliczerJ,KraftK,Bogetti
D,etal.Impactofnon-complianceonoutcomeafterpediatric kidneytransplantation:ananalysisinracialsubgroups.Pediatr Transplant.2004;8:367---71.
27.Watson AR. Non-complianceand transferfrom paediatricto adulttransplantunit.PediatrNephrol.2000;14:469---72. 28.Aujoulat I, Deccache A, Charles AS, Janssen M, Struyf C,
PélicandJ,etal.Non-adherenceinadolescenttransplant recip-ients:theroleofuncertaintyinhealthcareproviders.Pediatr Transplant.2011;15:148---56.
andtheInternationalPediatricNephrologyAssociation(IPNA). KidneyInt.2011;80:704---7.
30.WatsonAR,Harden P,FerrisM,KerrPG,MahanJ,RamzyMF. Transitionfrom pediatrictoadultrenalservices:aconsensus statementbytheInternationalSocietyofNephrology(ISN)and theInternationalPediatricNephrologyAssociation(IPNA). Pedi-atrNephrol.2011;26:1753---7.
31.GallieniM,AielloA,TucciB,SalaV,MandalSK,DonedaA,etal. The burdenofhypertension and kidneydisease inNortheast India:theInstituteforIndianMotherandChild noncommunica-blediseasesproject.SciWorldJ.2014:3208---69.
32.White A, Wong W, Sureshkumur P, Singh G. The burden of kidney disease in indigenous children of Australia and New
Zealand, epidemiology, antecedent factors and progression tochronic kidney disease. JPaediatrChild Health.2010;46: 504---9.
33.ZarocostasJ.Needtoincreasefocusonnon-communicable dis-easesinglobalhealth,saysWHO.BMJ.2010;341:c7065. 34.Gulland A. WHO agrees to set up body to act on
non-communicablediseases.BMJ.2013;346:f3483.
35.Feehally J. Chronic kidney disease: Health burden of kid-ney disease recognized by UN. Nat Rev Nephrol. 2011;8: 12---3.
ERRATUM
In the editorial Erratum of “In time: averting the legacy of kidney disease – focus on childhood” [Rev Paul Pediatr.
2016;34(1):5-10], in the Table 2, which reads:
Table 2 Etiology of chronic kidney disease in children.2
DRC DRET
Etiology Percentage (range)
Etiology Percentage (range)
CAKUT 48-59% CAKUT 34-43%
GN 5-14% GN 15-29%
HN 10-19% HN 12-22%
HUS 2-6% HUS 2-6%
Cystic 5-9% Cystic 6-12% Ischemic 2-4% Ischemic 2%
CKD, chronic kidney disease; ESRD, childhood onset end-stage renal disease; CAKUT, congenital anomalies of the kidney and urinary tract; GN, glomerulonephritis; HN, hypertension; HUS, hemolytic uremic syndrome. Rare causes include congenital NS, metabolic diseases, cystinosis. Miscellaneous causes depend on
how such entities are classiied.
Chronic Kidney Disease data are from North American Pediatric Renal Trials and Collaborative Studies, the Italian Registry and the Belgian Registry. Childhood onset end-stage renal disease data are from ANZDATA, ESPN/ERA-EDTA, UK Renal Registry and the Japanese Registry.
Table 2 Etiology of chronic kidney disease in children.2
DRC DRET
Etiology Percentage (range)
Etiology Percentage (range)
Etiology Percentage (range)
Etiology Percentage (range) CAKUT 48-59% CAKUT 34-43%
GN 5-14% GN 15-29%
HN 10-19% HN 12-22%
HUS 2-6% HUS 2-6%
Cystic 5-9% Cystic 6-12%
CKD, chronic kidney disease; ESRD, childhood onset end-stage re-nal disease; CAKUT, congenital anomalies of the kidney and urina-ry tract; GN, glomerulonephritis; HN, hereditaurina-ry nephropathy; HUS, hemolytic uremic syndrome. Rare causes include congenital NS, metabolic diseases, cystinosis. Miscellaneous causes depend
on how such entities are classiied.
Chronic Kidney Disease data are from North American Pediatric Renal Trials and Collaborative Studies, the Italian Registry and the Belgian Registry. Childhood onset end-stage renal disease data are from ANZDATA, ESPN/ERA-EDTA, UK Renal Registry and the Japanese Registry.