www.jped.com.br
REVIEW
ARTICLE
Education
in
children’s
sleep
hygiene:
which
approaches
are
effective?
A
systematic
review
夽
,
夽夽
Camila
S.E.
Halal
a,b,
Magda
L.
Nunes
b,∗aGrupoHospitalarConceic¸ão,PortoAlegre,RS,Brazil
bFaculdadedeMedicina,PontifíciaUniversidadeCatólicadoRioGrandedoSul(PUC-RS),PortoAlegre,RS,Brazil
Received7May2014;accepted14May2014 Availableonline25June2014
KEYWORDS
Sleephygiene; Sleepeducation; School-aged; Child
Abstract
Aim: Toanalyze the interventionsaimed atthe practiceofsleephygiene, aswell astheir
applicabilityandeffectivenessintheclinicalscenario,sothattheymaybeusedbypediatricians
andfamilyphysiciansforparentaladvice.
Sourceofdata: AsearchofthePubMeddatabasewasperformedusingthefollowing
descrip-tors:sleephygieneORsleepeducationANDchildrenorschool-aged.IntheLILACSandSciELO
databases,thedescriptorsinPortuguesewere:higieneEsono,educac¸ãoEsono,educac¸ãoE
sonoEcrianc¸as,ehigieneEsonoEinfância,withnolimitationsofthepublicationperiod.
Summaryofthefindings: Intotal,tenarticleswerereviewed,inwhichthemainobjectives
weretoanalyzetheeffectivenessofbehavioralapproachesandsleephygienetechniqueson
children’ssleepqualityandparents’qualityoflife.Thetechniquesusedwereoneormoreofthe
following:positiveroutines;controlledcomfortingandgradualextinctionorsleepremodeling;
aswellaswrittendiariestomonitorchildren’ssleeppatterns.Alloftheapproachesyielded
positiveresults.
Conclusions: Althoughbehavioralapproachestopediatricsleephygieneareeasytoapplyand
adhereto,therehavebeenveryfewstudiesevaluatingtheeffectivenessoftheavailable
tech-niques.Thisreviewdemonstratedthatthesemethodsareeffectiveinprovidingsleephygiene
forchildren,thusreflectingonparents’improvedqualityoflife.Itisofutmostimportancethat
pediatriciansandfamilyphysiciansareawareofsuchmethodsinordertoadequatelyadvise
patientsandtheirfamilies.
©2014SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Allrightsreserved.
夽 Pleasecitethisarticleas:HalalCS,NunesML.Educationinchildren’ssleephygiene:whichapproachesareeffective?Asystematic
review.JPediatr(RioJ).2014;90:449---56.
夽夽
StudyconductedatPontifíciaUniversidadeCatólicadoRioGrandedoSul,PortoAlegre,RS,Brazil.
∗Correspondingauthor.
E-mail:nunes@pucrs.br,camilahalal.neuro@hotmail.com(M.L.Nunes). http://dx.doi.org/10.1016/j.jped.2014.05.001
PALAVRAS-CHAVE
Higienedosono; Educac¸ãodosono; Infância;
Crianc¸a
Educac¸ãoemhigienedosononainfância:quaisabordagenssãoefetivas?Uma revisãosistemáticadaliteratura
Resumo
Objetivo: Avaliarasintervenc¸õesvisandopráticasdehigienedosonoemcrianc¸as,sua
aplicabil-idadeeefetividadenapráticaclínica,paraqueasmesmaspossamserutilizadasnaorientac¸ão
dospaispelospediatrasemédicosdefamília.
Fontedosdados: Foirealizadabusca nabasededadosdaPubmedutilizando osdescritores
sleephygieneORsleepeducationANDchildorschool-aged,enasbasesLilacseScielo,com
asseguintespalavras-chave:higieneEsono,educac¸ãoEsono,educac¸ãoEsonoEcrianc¸as,e
higieneEsonoEinfância,nãotendosidolimitadooperíododebusca.
Síntesedosdados: Foram revisados10 artigos cujosobjetivos eram analisar efetividade de
abordagenscomportamentaisedetécnicasdehigienedosonosobreaqualidadedosonodas
crianc¸asenaqualidadedevidadospais.Foramutilizadasumaoumaisdasseguintestécnicas:
rotinaspositivas,checagemmínimacomextinc¸ãosistemáticaeextinc¸ãogradativaou
remod-elamentodosono,bemcomodiáriosdopadrãodesono.Todasasabordagensapresentaram
resultadospositivos.
Conclusões: Apesar de a abordagem comportamental no manejo do sono na faixa etária
pediátrica ser de simples execuc¸ão e adesão, existem poucos estudos na literatura que
avaliaramsuaefetividade.Osestudosrevisadosevidenciaramqueestasmedidassãoefetivas
nahigieneerefletememmelhorianaqualidadedevidadospais.Édefundamental
importân-ciaospediatrasemédicosdefamíliaconheceremestasabordagens,paraquepossamoferecer
orientac¸õesadequadasaseuspacientes.
©2014SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Todososdireitos
reservados.
Introduction
Theprevalenceof sleepdisordersishigh inchildhoodand mayaffectupto30% ofschool-agechildren.1,2 These
dis-orders are important due to the effects they can have
not only on the child, but also on their families and
society.3 Thus, a child with chronic sleep disorders may
have learning and memory consolidation impairment at
school,irritabilityandmoodmodulation alterations,
diffi-cultysustainingattention,andbehavioralalterationssuch
asaggression,hyperactivity,orimpulsivity.4---7Furthermore,
thechronicsleepdeficit lowersthethresholdfor
acciden-talinjuryandpromotesmetabolicchangesthat,inthelong
term,cancauseother conditions,suchasoverweightand
itsconsequences.8,9
Pediatriciansandfamilyphysiciansplayakeyrolein
pro-motingquality of sleepin children.10,11 For this purpose,
theyneedtohave knowledge ofmethods of sleepquality
promotion,ofphysiologyaspectsandage-dependentsleep
modifications,andoftheimportanceofgood-qualitysleep
inchildhood.12 Arecentstudydemonstratedthat,although
96%of Americanpediatricians consideritto betheir role
toadvise parents about sleephygiene methods, only 18%
reportedhavingreceivedformaltrainingonthesubject.10
Moreover,intheUnitedStates,theSleepinAmericaPoll,
conductedin 2004,includingapproximately1,500families
ofchildrenupto10yearsold,demonstratedthatonly13%of
pediatriciansaskedparentsaboutpossiblesleepdisorders.13
Asurveyconductedinpediatricsresidencyprogramsinthe
UnitedStates,Canada,Japan,India,Vietnam,SouthKorea,
Singapore,andIndonesiaobservedthatthemeantimespent
in sleep education at the institutions in those countries
wastwohoursduringthetrainingperiod,andthata
quar-terofthereportedprogramsofferednoinstructiononthe
subject.14
Sleep disorders are divided into eight different
cate-gories,whichincludeinsomnia,sleepdisorderedbreathing,
hypersomnia of central origin, circadian rhythm
dis-orders, parasomnias sleep-related movement disorders,
unresolved issues and isolated symptoms (which include
snoring, somniloquy, and benign myoclonus), and other
sleep disorders.15 The latter category includes sleep
dis-orders considered to be physiological or environmental.16
Theenvironmentaldisorders,oftenofbehavioralorigin,can
be prevented if properly managed throughsleep hygiene
measures.17
Objective
The objective of thisarticle wasto performa systematic reviewof interventionsaimingat sleephygiene, andtheir applicabilityandeffectivenessinpediatricclinicalpractice, sothattheycanbeusedinparentalguidance.
Methods
withcomorbidities (hospitalizationduring the study, neu-rologicalor respiratory diseases, behavioralor psychiatric disorders).
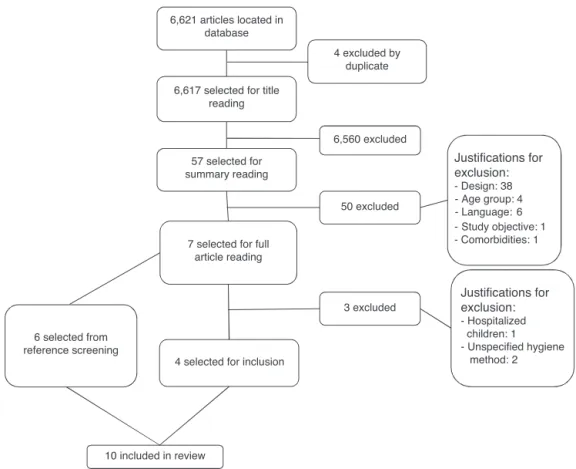
Studies of childrenwithdiagnosis of parasomnias were alsoexcludedfromthisanalysis,aswellasthoseinwhich the sleep hygiene method was not properly specified in themethodssection.OnlystudiespublishedinPortuguese, English, and Spanish were reviewed. The search totaled 6,621articles,ofwhichfourwereexcludedasduplicates.Of theremaining6,617,afterreadingthetitles,57were con-sideredpossiblyrelevantandhadtheirabstractsreviewed. Ofthese, 50were excludedfor not meetingthe inclusion criteria,andsevenwereselectedtobereadasfull texts. Ofthese,fourwereconsideredrelevantforthisstudy.18---21
Thesamesearch,butwithdescriptorsinPortuguese,was
conducted in the LILACS and SciELO databases. The
key-wordsusedwerehigieneEsono,educac¸ãoEsono,educac¸ão
EsonoEcrianc¸as,ehigieneEsonoEinfância.IntheLILACS
database,tworeferenceswerefound,neitherofwhichmet
thescopeofthisreview.IntheSciELOdatabase,the
descrip-torshigieneEsonoresultedin20articles,noneofwhichmet
thecriteriaforinclusioninthisstudy.Inthissamedatabase,
thedescriptorseducac¸ãoEsonoEcrianc¸asresultedinfive
articles,noneofwhichmetthescopeofthisreview.
The analysis of the studies and their references also
offeredthepossibilityofaccesstootherpublications,and
thusatotalofsixnewreferencesweresoughtandincluded
in this review.22---27 Fig. 1 shows the process of search,
selection, andexclusionof articlespresent in thecurrent
literature.
Definitions
The diagnosis of sleep disorders requires the presence of specificcriteria,whichmustbepresentforaspecificperiod oftimeandhavenegativeconsequencesonthechildand/or parents.1 Thus, mild or moderate symptoms arenot
con-sidereddisorders,althoughtheycancausesomedegreeof
impairment.28
The mean latency to sleep onset is usually about 19
minutesin children up to2 years of age, and 17minutes
from the age of 3 until the beginning of adolescence.29
In children, insomnia, defined as difficulty initiating or
maintaining sleep and comprising a number of
sub-classifications,usuallyfallsunderthediagnosisofbehavioral
insomnia.30 That, in turn, is divided between 1)
sleep-onsetassociation typeand2) limit-setting type,or mixed
form.
Themost commonsubtype,‘‘limit-setting type’’,
com-prisesthe attempttopostpone goingto sleepor refusing
todoso,characterizedbycrying, refusingtostay inbed,
orrequestsforfood,drink,orthereadingofstories.Inthis
context,itiscustomarytoidentifyparentswithinconsistent
routinesthattendtogiveintotheirchildren’srequests.31
Inthe‘‘sleep-onsetassociation’’subtype,certainbehaviors
needtoberepeatedateverywakingepisodeforthechildto
resumesleep.Thus,achildthatassociatessleeponsetwith
thepresenceofoneorbothparents,food,orbeingrocked
tosleep,whenawakeningduringthenight-evenwith
nor-malawakeningsexpectedfortheiragegroup-needstohave
theritualrepeatedtoresumesleep.32
6,621 articles located in database
6,617 selected for title reading
57 selected for summary reading
7 selected for full article reading
4 selected for inclusion
4 excluded by duplicate
6,560 excluded
50 excluded
Justifications for exclusion:
- Design: 38 - Age group: 4 - Language: 6
-Study objective:1 - Comorbidities: 1
3 excluded
Justifications for exclusion:
- Hospitalized children: 1 - Unspecified hygiene method: 2 6 selected from
reference screening
10 included in review
Parents′ perception of their child having poor quality sleepisdirectlyrelatedtothenumberofnightwakingsand tohowdemandingthechildistoinitiatesleepatbedtime andretake sleep afternight wakings.29,33 A recent
analy-sisofdatafromBrazilianbirthcohortfound,at12months,
aprevalenceof nocturnalawakeningsof 64.4%in thetwo
weeksprecedingthestudy,with56.5%ofthechildren
wak-ingupeverynight,andmostofthematleasttwotimeseach
night.34
Theterm‘‘sleephygiene’’includeschangesinsleep
envi-ronment,aswellasengagingthechildandtheirparentson
routineandpracticesthatencouragesleepofgoodquality
andsufficientduration.Italsoincludesthepracticeof
sooth-ingactivitiesduringwakefulnessaimingtopropitiatesleep
onset.11Themostusualpracticesarehavingconsistent
bed-timeandwake-uptimeforboththenocturnalanddaytime
sleep(amongchildrenattheagegroupwherenapsare
con-sideredphysiological),establishingtheappropriateplaceto
initiatesleep,and avoiding environmental andbehavioral
associationswithsleeponset(beingrockedtosleep,parents
layingonthechild’sbeduntilsleeponset,nursingtosleep,
watchingTVinbed,ordrinkingbeveragesrichincaffeine
closetobedtime).17
Childrenwhoneedbehavioralassociationstofallasleep,
uponawakeningduringthenight,willneedtheseresources
againinordertoresumesleep.1Thepassivepresenceofa
parent,however,appearstobepositiveatsomeagegroups,
aswellastheuseofthechild’sownresources,suchasusing
apacifierorthumb-suckingandsleepingwithatransitional
object.35
Methodsofsleephygienepromotion
The most studied methods are discussed below. These strategiesappeartoworkbetterinchildrenaged2yearsand older,whenarewardsystemcanbeused.2However,some
studieshaveattemptedtoadvisepregnantwomenor
par-entsofinfantsinordertopromoteproblemprevention.1,33
Extinction:Parentsshouldputthechildinbedata
pre-specifiedtimeandignorethechilduntilacertaintimeon
thefollowing morning,while monitoringforthepossibility
ofinjury.Themethodisbasedoneliminatingtheactsthat
reinforcecertainbehaviors(suchascryingonawakening),
aimingat their extinction over time.36 The greatest
diffi-cultyinimplementingthis strategyis theparents’lack of
consistencyandtheparentalanxietythatisgenerated.Asa
result,somedefendthestrategyofextinctioninthe
pres-enceofparents,suchthatparentsremainintheroombut
donotrespondtothechild’sbehavior.2,36
Gradualextinction:Inspiteofcomprisingdifferent
tech-niques,the gradual extinction method usually consists of
ignoringthedemandsofthechildforspecifictimeperiods;
these periods are usually determined by the child’s age
andtemperamentandtheparents’discretioninrelationto
howlong theytoleratetheirchild’scrying. Parentsshould
calmthechildfor shortperiods,whichusuallyrangefrom
15secondstooneminute. Thetechniqueaimstopromote
thechild’scapacitytoself-sootheandreturntosleep,
with-outundesirableassociationsorparentalinterference.1,2,36
When assessing 79 children with a mean age of 10.2
months (3-24 months) whose parents were instructed to
implementthegradualextinctiontechniqueduring
noctur-nal sleep,Skuladottir etal.observedthatthe durationof
nocturnal sleep increasedfrom 10.27hours to10.57hours
(p<0.001) afterthe intervention, aswell asreducing the
frequency ofnocturnal awakenings(from4.57to1.57per
night,p<0.001).18
Eckerbergconductedastudy toassesswhether
recom-mendations provided only in written form tothe parents
of children treated at a clinic for sleep disorders would
work aswell as clinical follow-up, which hadbeen
previ-ouslyadvocated.19Guidancetoparentsofchildrenincluded
in the study followed the gradualextinction method, the
same provided by the physician during routine
consulta-tions. Atotal of39 children between 4and 30months of
ageparticipated inthestudy,divided intoan intervention
group(writteninformationsentby email,withoutcontact
withtheclinician) and acontrol group(information given
bytheclinician).Aftertheintervention,childrenfromboth
groups fell asleepfaster (p<0.001) and earlier (p<0.01),
which amounted to 30minutes earlier after a one-month
intervention.
In both groups, there was also a significant reduction
in nocturnal awakenings (from 4.6 to 4.2 awakenings in
thecontrolandfrom3.3to2.8in theinterventiongroup,
p<0.001)inthetwoweeksfollowingtheintervention.The
probability of resume sleep on their own also increased
aftertheintervention(2.1-foldinthecontroland2.0-fold
in the intervention group,p<0.001). After threemonths,
thisdecrease continuedin bothgroups, and therewasan
increaseinthedurationofnocturnalsleep(by59minutesin
thecontrolandby72minutesintheinterventiongroup)and
adecreaseintimeofwakefulnessduringthenight(from82
to18minutes,p<0.001),withnodifferencesbetweenthe
groups.
InanAustraliancase-controlstudycarriedoutbyHiscock
&Wake,146childrenbetween7and9monthsofagewere
recruited from an outpatient setting.22 The intervention
group received specialized guidance on the physiology of
sleepandtheapplicationofthegradualextinctionmethod,
whereasthecontrolgroupreceivedanewsletterabout
nor-mal sleeppatterns at theage range of6-12 months. Two
monthslater,childrenintheinterventiongrouphadresolved
more sleep problems than those in the control group
(p=0.005), andthe remainingproblems wereless intense
in the intervention group. Maternal depressive symptoms
decreasedinbothgroupsaftertwomonths,butdecreased
moresignificantly intheinterventiongroup (p=0.02),the
groupwhosemothersalsoreportedthattheirownsleepwas
ofbetterquality(p=0.02)attheendofthefollow-up.
Aiming to compare the effectiveness of the gradual
extinction and extinction methods, and of these in
rela-tiontono sleephygienemethod,ReidMJ etal. analyzed
43children aged16to48months(14extinction,13
grad-ualextinction,and16controls)priortointervention,andat
21daysandtwomonthsafterintervention.23Theyobserved
that families allocated to the extinction group had more
difficulty adheringtothe methodduringthe secondweek
inrelationtothegradualextinctiongroup(interruptingthe
interventiononaverage3.4timeseachweek,comparedto
1.1timesintheothergroup,p=0.02).Duringtheremaining
time,adherenceremainedhighandsimilarinbothgroups
The intervention groups also had better assessments
regarding qualityat both themoment of sleeponset and
sleepmaintenance,whencomparedtothecontrolgroup.In
thesubscaleregarding qualityofsleepin theCBCL(Child
Behavior Checklist), both intervention groups also scored
betterinrelationtothecontrolgroup,andsimilarlytoeach
other.Twomonthslater,anewevaluationshowedthatthe
benefitsremained inthe groups thatunderwent
interven-tions.
Minimalcheckingwithsystematic extinction:Similarto
theextinctionmethod,butthechildcanbecheckedevery5
to10minutes,andtheparentcancomfortthechildquickly
whennecessary,arrangingthecovers,andmakingsurethat
therearenocomplications.2
Adachi etal. analyzed 99 children taken for childcare
consultation at 4 months of age, randomly dividing them
between intervention and control groups.20 The
interven-tion consisted of information about positive routines for
initiating sleep, appropriate and inappropriate behaviors
to resume sleep at night, and the method of minimal
checking with systematic extinction. At the end of the
study, the intervention group had a greater decrease in
the rates of behaviorslisted as‘‘inadequate’’. The
char-acteristicof‘‘givingfoodoradiaperchangeimmediately’’
decreasedfrom66.7%to36.4%(p=0.001),andthe
charac-teristicdescribedas‘‘holdingandcomfortingimmediately’’
decreased from 22.7% to10.6% (p=0.021). In the control
group,thenumberof nocturnal awakeningsincreased
sig-nificantlyfrom53%to66.7%(p=0.022),asdidthenumber
ofawakeningswithcrying(from8.1%to19.4%,p=0.065).
AninterventionconductedbyHalletal.included39
fam-iliesofinfantsaged6to12months,whoseparentssought
helpthroughatelephoneansweringservice forparentsof
infantswithdifficultysleeping.21Theaimofthestudywasto
analyzetheimprovementintheparents’qualityoflife,and
at theend of theintervention, a significant improvement
intheparents’qualityofsleepwasobserved,aswellasof
symptomsofdepressedmoodandfatigue.Theco-sleeping
ratesalsodecreasedsignificantly(from70%practicingthem
before the intervention to 74% not practicing them after
theintervention,p<0.001),withnochangeinthepractice
ofbreastfeeding.
Positive routines: This methodconsistsof the
develop-ment of routines preceding bedtime, comprisingpeaceful
andpleasurable activities.37 Anotherstrategy thatcan be
used is delaying the time to go to bed to ensure that,
whenlyingdown,thechildwillfallasleepquickly,untilthis
habit offalling asleepquicklyis consolidated. After that,
startanticipatingbedtimeby15to30minutesonsuccessive
nights until the time considered appropriate is achieved.
Thechildshouldnotsleepduringtheday,exceptattheage
groupsinwhichdaytimesleepisphysiological.2,36
Positiveroutinesareoftenusedincombinationwithother
methods of sleep hygiene. Adachi et al. included
behav-ioral recommendationsin theirintervention group.At the
end of the intervention, they found that the practice of
positiveroutinescharacterizedby‘‘playingandstimulating
duringtheday’’(p=0.003),‘‘establishingaplacetosleep’’
(p=0.008),and‘‘establishingatimetabletosleepandwake
up’’(p=0.007)hadincreasedsignificantly.20
Mindelletal.performedastudyincludingchildrenintwo
groups(7-18monthsand18-36months),inwhicharoutine
precedingsleepwasimplemented,consistingofabath
fol-lowedbymassageandquietactivities,withatimeperiod
betweenthebathandturningoffthelightsof30minutes.24
Theroutinesignificantlyreducedproblembehaviorsinboth
groups,withdecreasedsleeplatencyandthenumberand
durationof nocturnalawakenings(p<0.001). Themothers
inthegroupofchildrenagedupto18monthsshowed
reduc-tioninsymptomsofstress,depression,anger,fatigue,lack
ofstamina,andconfusion(p<0.001)and,inthegroupolder
than18months,therewasanimprovementinthesymptoms
ofstress,anger,fatigue,andconfusion(p<0.001).
This study had a long-term follow up, in which 65%
of participants in the group aged up to 18 months were
randomized into three groups: one received instructions
exclusively via the internet, another received
instruc-tions via the internet in addition to those described
in the previous study, and a third group was used as
control.25 After one year, the improvements observed in
the twogroups that received the interventions regarding
sleeplatency, difficulty falling asleep, number and
dura-tionof nocturnal awakenings,periodof continuous sleep,
and maternal confidence in relation to her child’s sleep
management persisted (p<0.001). After three weeks of
intervention, the qualityof maternal sleep improved
sig-nificantly(p<0.001);afteroneyear,however,itdecreased
back to levels close to those at the start of the
intervention.
Aiming tocompare the effectiveness between positive
routinesandgradualextinctioninreducingtempertantrums
with bouts of anger at bedtime, Adams and Rickert
fol-lowed, for six weeks, two groups of children targeted
for each intervention compared to a control group, in
a total of 36 children (12 per group) aged between 18
and48months.26 The children inthe groups submittedto
any of the interventions had significantly fewer bouts of
anger, which were of shorter duration than the controls
(p<0.05 and p<0.001, respectively). There was no
sig-nificant difference in response between the intervention
groups, although children in the group submittedto
pos-itive routines showed faster favorable responses. Parents
inthegroupallocatedtoimplementpositiveroutinesalso
scoredbetterontheMaritalAdjustmentScaleattheendof
theintervention,whichwasvalidatedforthatpopulation,
andinvestigatestheperceptionthatthecouplehasoftheir
relationship.38
Programmed awakening: It consists in waking up the
childatnight,between15and30minutesbeforetheusual
timeofspontaneousawakening,andafterthat,comforting
hertoreturntosleep.Thenumber ofprogrammed
awak-eningsshould varywiththe usual number of spontaneous
awakenings.Overtime,ittendstoextinguishspontaneous
awakenings,andtheprocessofreducingscheduled
awaken-ingsbegins,resultinginincreasedsleepconsolidation.1,2,36
Rickert&Johnsoncomparedthemethodsofprogrammed
awakeningandsystematicextinctionwithacontrolgroupin
33childrenwitha meanageof 20months(6-54months),
randomly allocating them into three groups of 11
chil-dren (programmed awakening, systematic extinction, and
acontrolgroup).27Theinterventionlastedeightweeks,and
parentswerere-contactedthreeandsixweekslater.
Chil-drenwhoexperiencedtheinterventionsshowed,attheend
Halal
CS,
Nunes
ML
Table1 Studiesreviewed,authors,agerangeofstudy,numberofparticipants,objectives,typeofintervention,andoutcomes.
Author/yearof
publication
Agerange n Mainobjective Sleephygienemethod Results
Adachietal.,20
2009
4months Intervention:99 Control:95
-Decreaseofinappropriatebehavior, nighttimeawakenings,andarousals withcrying
-Positiveroutines -Minimalcheckingwith systematicextinction
-Decreaseofinappropriatebehaviors
-Preventionofincreasednocturnalawakenings withage
Halletal.,21
2006
6to12 months
39 -Assessmentofparents’qualityof lifeafterimprovementofthechild’s sleepquality
-Minimalcheckingwith systematicextinction
-Improvementofsleepqualityanddepressed moodsymptomsofparents
-Decreaseinco-sleeping Rickert&
Johnson,27
1988
6-54 months
33(11ineach interventiongroup, 11incontrolgroup)
-Evaluationofthereductioninthe numberofnocturnalawakenings
-Programmedawakening -Systematicextinction -Control
-Lowernumberofnighttimeawakeningsin bothgroupsthatunderwentinterventions
Mindelletal.,24
2009
7to18 months 18to36 months
206(7-18m) 199(18-36m)
-Changesinmaternalmoodafter improvedsleepqualityofthechild
-Positiveroutines -Decreasedsleeplatencyinchildren -Decreaseinthedurationofnocturnal awakenings
-Decreaseindepressivesymptomsinmothers Mindelletal.,25
2011
18to48 months
171 -Changeinsleepqualityofchildand mother
-Changeinmaternalself-confidence
-Positiveroutines -Decreaseinsleeplatency,difficultyfalling asleep,numberanddurationofnocturnal awakenings
-Maternalself-confidenceimprovement -Temporaryimprovementofthequalityof maternalsleep
Skuladottir etal.,182005
3to24 months
79 -Changesinthenocturnalsleep patternwithimproveddaytimesleep pattern
-Positiveroutinesfordaytime sleep
-Gradualextinctionfor nighttimesleep
-Remodelingfordaytimesleep
-Increaseinnocturnalsleep -Decreaseinnocturnalawakenings
Adams& Rickert,26
1989
18and48 months
36(12ineach interventiongroup; 12incontrolgroup)
-Effectonthenumberoftemper tantrums
-Positiveroutines -Gradualextinction
-Lowernumberoftempertantrumsand shorterepisodesinbothinterventiongroups -Bestscoreintheparents’group
positiveroutinesintheMaritalAdjustment Scale
Eckerberg,19
2002
4to30 months
39 -Effectivenessofwritteninformation oververbalinstructionsbythe physician
-Gradualextinction -Decreaseinsleeplatencyinbothgroups -Decreaseofawakeningsinbothgroups -Increasedchancetogobacktosleepontheir owninbothgroups
Hiscock& Wake,222002
7to9 months
Intervention:75 Control:71 (total146)
-Effectivenessoftheadvicegivenby thephysicianinrelationtowritten adviceonsleepqualityofthechild andmaternaldepressivesymptoms
-Gradualextinction -Fewersleepproblemsintheintervention group
-Decreaseinmaternaldepressivesymptomsin theinterventiongroup
Reidetal.,23
1999
16to48 months
43(14inextinction group,13ingradual extinctiongroup, and16controls)
-Comparisonoftheeffectivenessof methodsofsleephygiene
-Extinction -Gradualextinction
although this decrease occurred faster in the group sub-mittedtotheextinctionmethod.Thisdifferenceremained statisticallysignificantduringthereassessments.
Sleepremodeling:Consistsofnotallowingnapstooccur attimesthatcandisruptnocturnalsleeponset,which com-prisesfourhoursbeforebedtimeinchildrenatanagerange thatallowstwonapsperday,andsixhoursbeforebedtime inchildrenwhousuallyhaveonenapaday.18
ThestudydevelopedbySkuladottiretal.usedthis
tech-nique for daytime naps.18 As demonstrated above, they
observedpositiveresultsregardingthedurationofnocturnal
sleep.
Table1summarizes thestudiesincluded inthepresent
review by author, age group andsample size, objectives,
typeofintervention,andmainresults.
Discussion
The number of studies available in the literature on interventions targeting sleep hygiene in children without comorbid conditions is scarce.18---27 It is noteworthy that
no Brazilian studies were found in this search. A recent
cross-sectionalstudyperformedin theUnitedStates,with
children aged5 to6years froma low-incomecommunity
consistingpredominantlyofLatinofamilies,observeda
four-fold higher prevalence of sleep alterations than normally
expectedatthisage,suggestingthatunfavorable
socioeco-nomicconditionsmaycontributetopoorsleepquality.39
This finding indicates the potential importance of this
typeofstudyandsubsequentinterventionsintheBrazilian
population,consideringthatthesleepqualityimprovement
amongchildrenofdifferentagerangesandsocioeconomic
levelscould also contribute tothe improvement of other
indicesofqualityoflife.
Some studies observed that groups of children
receiv-ing no intervention also obtained improvements in sleep
quality indices at the reassessments. One possible
expla-nation is the existence of an association between neural
maturationandphysiological circadianmechanisms,which
inthemselvesactasasleepregulator,improvingsleep
qual-ityovertime.1However,itisnoteworthythatchildrenwho
receivedinterventionsconsistentlyshowedmoresignificant
improvements regardingindicesof sleepquality.This fact
suggeststheimportanceoftheexternalenvironmentonthe
sleepmaturationprocess.
Informationprovidedonlyinwriting(brochures,
newslet-ters)canbeequallyeffective.19 Thisispossiblyduetothe
factthesecanbeconsultedasoftenasparentsdeem
nec-essary, and asdoubts arise in the implementation of the
techniques.
Theinterventionsperformedinthereviewedstudiesare
simpleandeffective,andrepresentsecondaryeducational
measures for parentsthat donotimply additionalcostto
themortothehealthsystem,becausetheybasicallyconsist
ofrecommendations.Itispossiblethattheseinterventions
wouldactuallyimplycostsavingstothesystem,aswellto
advisedparents,whosechildrensleepbetter,andthuswould
probablyhavealowerchanceofseekingspecializedcare,in
additiontohavingbetterperformanceintheirprofessional
activities.Thefavorableresultsofalltheinterventionsthat
objectively sought to analyzemood and qualityof life of
parentscorroboratethishypothesis.
Thereviewedstudiesaddressedabroadagerange,
vary-ingfrom3monthsto4years,mostlycomprisingchildrenin
theirfirstyearoflife. Theimportanceof thisinformation
liesinthefactthatinterventionsinchildrenyoungerthan
2yearsalsoappeartobeeffective,allowingearlychanges
andpreventingchildren’sexposuretolongperiodsofpoor
sleep.
The role of the health professional who works with
children is to know the physiologyof sleepand its
phys-iological maturation process. The inclusion of questions
aboutsleepqualityandpossiblesleepimpairmentfactorsin
theanamnesis,inadditiontoofferingsleephygiene
guide-linesregardingthepreventionortreatmentofpathological
behaviors,shouldbepartofeverypediatricvisit.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.MindellJA,KuhnB,LewinDS,MeltzerLJ,SadehA.Behavioral treatmentofbedtimeproblemsandnightwakingsininfantsand youngchildren.Sleep.2006;29:1263---76.
2.NunesML,CavalcanteV.Avaliac¸ãoclínicaemanejodainsônia empacientespediátricos.JPediatr(RioJ).2005;81:277---86. 3.Karraker KH, Young M. Night waking in 6-month-old infants
and maternal depressive symptoms. J Appl Dev Psychol. 2007;28:493---8.
4.HaleL,BergerLM,LeBourgeoisMK,Brooks-GunnJ.A longitu-dinalstudyofpreschoolers’language-basedbedtimeroutines, sleepduration,andwellbeing.JFamPsychol.2011;25:423---33. 5.Blunden SL, Chapman J, Rigney GA. Are sleep education programs successful? The case for improved and consistent researchefforts.SleepMedRev.2012;16:355---70.
6.QuachJ,GoldL, ArnupS,SiaK-L,WakeM,HiscockH.Sleep well-be well study: improving school transition by improv-ing child sleep: a translational randomisedtrial. BMJ Open. 2013;3:e004009.
7.Owens J.Classification and epidemiology ofchildhood sleep disorders.PrimCareClinOfficePract.2008;35:533---46. 8.Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E,
Stranges S, et al.Meta-analyses ofshort sleep duration and obesityinchildrenandadults.Sleep.2008;31:619---26. 9.Blunden SL,ChervinRD.Sleep problemsare associated with
pooroutcomesinremedialteachingprogrammes:Apreliminary study.JPaedChildHealth.2008;44:237---42.
10.Faruqui F, Khubchandani J, Price JH, Bolyard D, Reddy R. Sleep disorders in children: a national assessment of pri-marycarepediatrician practicesandperceptions.Pediatrics. 2011;128:539---46.
11.Gruber R, Cassoff J, Knäuper B. Sleep health education in pediatriccommunitysettings:rationaleand practical sugges-tionsforincorporatinghealthysleepeducationintopediatric practice.PediatrClinNorthAm.2011;58:735---54.
12.MindellJA,MolineML,ZendellSM,BrownLW,FryJM. Pedia-triciansandsleepdisorders:trainingandpractice.Pediatrics. 1994;94:194---200.
13.NationalSleepFoundation.SleepinAmericaPoll.2004.[cited
on20Mar2014].Availablefrom:www.sleepfoundation.org
14.Mindell Ja, Bartle A, Ahn Y, Ramamurthy MB, Huong HTD, KohyamaJ,etal.Sleepeducationinpediatricresidency pro-grams:across-culturallook.BMCResNotes.2013;6:130. 15.Oliveiero B,NovelliL. Sleepdisordersinchildren. ClinEvid.
16.AmericanAcademyofSleepMedicine.International classifica-tionofsleepdisorders:diagnosticandcodingmanual.2nded.
Westchester:AmericanAcademyofSleepMedicine;2005. 17.Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD.
Devel-opmental aspects of sleep hygiene: Findingsfrom the 2004 NationalSleepFoundationSleep inAmericaPoll.SleepMed. 2009;10:771---9.
18.Skuladottir A, Thome M, Ramel A. Improving dayand night sleepproblemsininfantsbychangingdaytimesleeprhythm: a single group before and after study. Int J Nurs Studies. 2005;42:843---50.
19.Eckerberg B. Treatment of sleep problems in families with smallchildren: iswritten informationenough?ActaPaediatr. 2002;91:952---9.
20.AdachiY,SatoC,NishinoN,OhryojiF,HayamaJ,YamagamiT.A briefparentaleducationforshapingsleephabitsin4-month-old infants.ClinMedRes.2009;7:85---92.
21.HallWA,ClausonM,CartyEM,JanssenPA,SaundersRA.Effects onparentsofaninterventiontoresolveinfantbehavioralsleep problems.PedNurs.2006;32:243---50.
22.HiscockH,WakeM.Randomisedcontrolledtrialofbehavioural infantsleepinterventiontoimproveinfantsleepandmaternal mood.BMJ.2002;324:1062---7.
23.Reid MJ, Walter AL, O’Leary SG. Treatment of young chil-dren’sbedtime refusaland nighttime wakings:a comparison of‘‘standard’’and graduatedignoringprocedures.JAbnorm ChildPsychol.1999;27:5---16.
24.MindellJA,TelofskiLS,WiegandB,KurtzES.Anightlybedtime routine:impactonsleepinyoungchildrenandmaternalmood. Sleep.2009;32:599---606.
25.MindellJA,DuMondCE,SadehA,TelofskiLS,KulkarniN,GunnE. Long-termefficacyofaninternet-basedinterventionforinfant andtoddlersleepdisturbances:oneyearfollow-up.JClinSleep Med.2011;7:507---11.
26.AdamsLA,RickertVI.Reducingbedtimetantrums:comparison betweenpositiveroutinesandgraduatedextinction.Pediatrics. 1989;84:756---61.
27.Rickert VI, Johnson CM. Reducing nocturnal awakening and crying episodes in infantsand young children: a comparison
betweenscheduledawakeningsandsystematicignoring. Pedi-atrics.1988;81:203---12.
28.ThorpyMJ.Classificationofsleepdisorders.Neurotherapeutics. 2012;9:687---701.
29.Galland BC, Taylor BJ, Elder DE, Herbison P. Normal sleep patternsininfantsandchildren:Asystematicreviewof obser-vationalstudies.SleepMedRev.2012;16:213---22.
30.MorgenthalerTI,OwensJ, AlessiC,BoehleckeB, BrownTM, ColemanJ,etal.Practiceparametersforbehavioraltreatment ofbedtimeproblems andnight wakingsininfantsandyoung children.Sleep.2006;29:1277---81.
31.WardTM,RankinS,LeeKA.Caringforchildrenwithsleep prob-lems.JPediatrNurs.2007;22:283---95.
32.AnuntasereeW,Mo-suwanL,VasiknanonteP,KuasirikulS, Ma-a-leeA,ChoprapawanC.NightwakinginThaiinfantsat3months ofage:associationbetweenparentalpracticesandinfantsleep. SleepMed.2008;9:564---71.
33.CookF,BayerJ, LeHN,MensahF,Cann W, Hiscock H.Baby business: a randomised controlled trial of a universal par-entingprogram that aims to prevent early infantsleep and cryproblemsandassociatedparentaldepression.BMCPediatr. 2012;12:13.
34.SantosIS,MotaDM,MatijasevichA.Epidemiologyofco-sleeping andnighttimewakingat12monthsinabirthcohort.JPediatr (RioJ).2008;84:114---22.
35.Moore M, Meltzer LJ, Mindell JA. Bedtime problems and night wakings in children. Prim Care Clin Office Pract. 2008;35:569---81.
36.KuhnBR,ElliottAJ.Treatmentefficacyinbehavioralpediatric sleepmedicine.JPsychosomRes.2003;54:587---97.
37.GallandBC,MitchellEA.Helpingchildrensleep.ArchDisChild. 2010;95:850---3.
38.SpanierGB.Themeasurementofmaritalquality.JourSexMarit Ther.1979;5:288---300.