www.jped.com.br
ORIGINAL
ARTICLE
Prevalence
and
risk
factors
associated
with
wheezing
in
the
first
year
of
life
夽
Olivia
A.
A.
Costa
Bessa
a,∗,
Álvaro
J.
Madeiro
Leite
b,
Dirceu
Solé
c,
Javier
Mallol
daMedicine,UniversidadedeFortaleza(UNIFOR),Fortaleza,CE,Brazil
bMother-ChildDepartment,SchoolofMedicine,UniversidadeFederaldoCeará(UFCE),Fortaleza,CE,Brazil cEscolaPaulistadeMedicina,UniversidadeFederaldeSãoPaulo(EPM-UNIFESP),SãoPaulo,SP,Brazil
dDepartmentofPediatricRespiratoryMedicine,HospitalElPino,UniversidadedoChile,Santiago,Chile
Received14May2013;accepted21August2013 Availableonline21December2013
KEYWORDS
Prevalence; Riskfactors; Cross-sectional studies; Infant
Abstract
Objective: toinvestigatetheprevalenceandriskfactorsassociatedwithwheezingininfants inthefirstyearoflife.
Methods: thiswasacross-sectionalstudy,inwhichavalidatedquestionnaire(Estudio Interna-cionaldeSibilanciasenLactantes-InternationalStudyofWheezinginInfants-EISL)wasapplied toparentsofinfantsagedbetween12and15monthstreatedin26of85primaryhealthcare unitsintheperiodbetween2006and2007.Thedependentvariable,wheezing,wasdefined usingthefollowingstandards:occasional(uptotwoepisodesofwheezing)andrecurrent(three ormoreepisodesofwheezing).Theindependentvariableswereshownusingfrequency distri-butiontocomparethegroups.Measuresofassociationwerebasedonoddsratio(OR)witha confidenceintervalof95%(95%CI),usingbivariateanalysis,followedbymultivariateanalysis (adjustedOR[aOR]).
Results: atotalof1,029(37.7%)infantshadwheezingepisodesinthefirst12monthsoflife;of these,16.2%hadrecurrentwheezing.Riskfactorsforwheezingwerefamilyhistoryofasthma (OR=2.12;95%CI:1.76-2.54)andsixormoreepisodesofcolds(OR=2.38;95%CI:1.91-2.97)and pneumonia(OR=3.02;95%CI:2.43-3.76).Forrecurrentwheezing,riskfactorswere:familial asthma(aOR=1.73;95%CI:1.22---2.46);earlyonsetwheezing(aOR=1.83;95%CI:1.75-3.75); nocturnalsymptoms(aOR=2.56;95%CI:1.75-3.75),andmorethansixcolds(aOR=2.07;95% CI1.43-.00).
夽 Pleasecitethisarticleas:BessaOA,LeiteÁJ,SoléD,MallolJ.Prevalenceandriskfactorsassociatedwithwheezinginthefirstyearof
life.JPediatr(RioJ).2014;90:190---6.
∗Correspondingauthor.
E-mail:oliviabessa@gmail.com,oliviabessa@unifor.br(O.A.A.C.Bessa).
Conclusion: themainriskfactorsassociatedwithwheezinginFortalezawererespiratory infec-tionsandfamilyhistoryofasthma.Knowingtheriskfactorsforthisdiseaseshouldbeapriority forpublichealth,inordertodevelopcontrolandtreatmentstrategies.
©2013SociedadeBrasileiradePediatria.PublishedbyElsevierEditoraLtda.Allrightsreserved.
PALAVRAS-CHAVE
Prevalência; Fatoresderisco; Estudostransversais; Lactente
Prevalênciaefatoresderiscoassociadosàsibilâncianoprimeiroanodevida
Resumo
Objetivo: verificar aprevalência efatores de riscoassociados àsibilância em lactentes no primeiroanodevida.
Métodos: estudotransversal,ondefoiaplicadooquestionáriopadronizadoevalidado(Estudio Internacional deSibilancias enLactantes-EISL) aospaisde lactentescomidade entre12 e 15 mesesqueprocuraram26das85unidadesdeatenc¸ão básica,noperíodo 2006a2007.A variável dependente, sibilância,foi definidautilizando os seguintespadrões: ocasional(até doisepisódiosdesibilância)erecorrente(trêsoumaisepisódios).Asvariáveisindependentes foramapresentadasusandodistribuic¸ãodefrequências,utilizadasparacompararosgrupos.As medidasdeassociac¸õesforambaseadasemrazãodechances(oddsratio-OR),comintervalode confianc¸ade95%(IC95%),comanálisebivariada,seguidadeanálisemultivariada(ORajustada).
Resultados: umtotalde1.029(37,7%)lactentesapresentousibilâncianosprimeiros12meses devidaedestes,16,2%tiveramsibilânciarecorrente.Osprincipaisfatoresderiscoassociados àsibilânciaforam:históriafamiliardeasma(ORa=2,12;IC95%:1,76-2,54);seisoumais episó-diosderesfriado(ORa=2,38;IC95%:1,91-2,97)epneumonia(ORa=3,02;IC95%:2,43-3,76)e sibilânciarecorrenteforam:asmanafamília(ORa=1,73;IC95%:1,22-2,46);inícioprecocede sibilância(ORa=1,83;IC95%:1,75-3,75);sintomasnoturnos(ORa=2,56;IC95%:1,75-3,75);mais de6resfriados(ORa=2,07;IC95%:1,43-3,00).
Conclusão: osprincipaisfatoresderiscoassociadosàsibilânciaforamasinfecc¸õesrespiratórias ehistóriadeasmanafamília.Conhecerosfatoresderiscodessaenfermidadedeveseruma prioridadeparaasaúdepública,quepoderádesenvolverestratégiasdecontroleetratamento.
©2013SociedadeBrasileiradePediatria.PublicadoporElsevierEditoraLtda.Todososdireitos reservados.
Introduction
Wheezingisaverycommonsymptom ininfants,1 whichis
usuallyaccountableforahighdemandofmedical consulta-tionsandemergencycareservices,withrelativelyhighrates ofhospitalization.Along withacuterespiratoryinfections, itplaysanimportantroleininfantmortality.2InLatin
Amer-ica,approximately100,000childrendieinthefirstyearof lifeduetoacuterespiratoryinfection,andasignificant pro-portionofthemhaveahistoryofwheezing.3InBrazil,data
fromtheMinistryofHealthshowthataround35%ofinfant hospitalizationsinthefirstyearoflifeinBrazilaredueto respiratorydiseases.4
Nevertheless, the real extent of this problem remains unknown, aswell ashowmany of theseinfants are actu-allyasthmaticpatients.5Thefactorsthatestablishthestart,
evolution,andprognosisofwheezingininfantshavenotyet beenwelldefined.Asitoccursinolderchildren,itislikely thatindividualgeneticandimmunologicalpatterns, associ-atedwithenvironmentalfactors,areresponsibleformostof wheezingphenotypesinchildhood.6,7Moststudiesindicate
amultifactorialetiologyinthepathogenesisofwheezingin the first year of life, in addition tothe close association withrespiratory infections. However, howthese different elementsrelate toeachother is stillthesubjectofmuch controversy.8,9
TheInternational StudyofWheezinginInfants(Estudio InternacionaldeSibilanciasenLactantes[EISL])was devel-opedinordertodeterminetheprevalenceandriskfactors associatedwithwheezingininfantsinthefirstyearoflife.10
TheEISLprojectevaluatedtheriskfactorsassociatedwith wheezing in the first year of life in children from Latin America,Spain,andtheNetherlands.Datashowedalarge variationintheprevalenceandseverityofwheezingatthe centers,butwithatendencyofhigherprevalenceand sever-ityinLatinAmericanchildren.Thepresentstudyispartof theEISLproject-phase1.
This studyaimedtodetermine theprevalence andrisk factorsassociatedwithwheezingininfantsinthefirstyear oflife,livinginFortaleza,Brazil,usingtheEISLprotocol.
Methods
Thepresent studywasconductedin thecityof Fortaleza, capitalof thestate ofCeará,NortheasternBrazil,aspart oftheEISLproject-phase1.10TheEISLisacross-sectional,
withotherrespiratorydiseases,especiallypneumonia,and todefine the risk factors for wheezing in infants in their first12monthsoflife,similarlytothe‘‘InternationalStudy ofAsthmaandAllergiesinChildhood’’(ISAAC).11
Thestudywasperformedin26of85primarycareunits, selectedatrandomandproportionaltothedemographic dis-tributioninthesixregions(regionalexecutivesecretariats [RES])ofFortaleza.EachREShasitsuniquecharacteristics regarding geographic location (coastal region, peripheral region),distributionofincome,territorialoccupation,and extension.12
The study population comprised infants aged between 12and15months,selectedduringroutineconsultationsor immunizations.Childrenwithchronicdiseasesinother sys-temswhopresentedanyrespiratoryimpact(neuropathies, heart disease, severe somatic malformations and genetic diseases,amongothers)wereexcluded.
DatacollectionwasconductedfromDecemberof 2006 toDecemberof2007usingthewrittenquestionnaire(WQ) ofEISLasthecollectiontool,whichwasstandardizedand validatedforthelocalenvironment(Brazilianculture)after beingtranslated intoBrazilian Portuguese.13 The WQ-EISL
comprisesquestionsregardingdemographiccharacteristics, wheezing,respiratoryinfections,andriskfactors,namely: gender, age, ethnicity, birth weight and height, current weight and height, type of delivery, maternal schooling, characteristics of wheezing, medication use, hospitaliza-tion,association with pneumonia, andenvironmental and familyfactors,amongothers.
Thequestionsareverysensitive,andarebasedonclinical practiceaswell asoninternational studies oninfants, to ensurecomparableinformationontheepidemiologicaland clinicalissuesrelatedtothisdisease.
The dependent variable,wheezing,wasdefined inthis studyasthepresenceofwheezingorbronchitisinthefirst 12 months of the child’s life, and categorized as occa-sional(uptotwoepisodesofwheezing)orrecurrent(three or more episodes of wheezing). The independent varia-bles (exposure) were grouped according to demographic, socioeconomic,environmental,family,andclinical charac-teristics.
Dataanalysis
Datawereorganizedinastandardformat;dataentrywas performedusingEPI INFO,version3.5.1,anddataanalysis wasconductedusingSTATA,version10.Thevariableswere shown usingthe distribution of frequencies andPearson’s chi-squared test was used to compare groups of infants. Measuresofassociationwerebasedonoddsratio(OR)witha 95%confidenceinterval(95%CI),withbivariateanalysis fol-lowedbymultivariateanalysis(logisticregression-adjusted OR).Intheunivariateanalysis,theassociationbetweeneach explanatoryvariableandthedependentvariable(wheezing) wasinvestigatedseparately,whichwasusedasaselection criterion for the independent variables used in the final model.Then,thesevariableswereincludedinthelogistic regressionmodel(adjustedOR),whichevaluatedtheeffect oftheselectedvariablesontheoutcome.Inthiscase,the influenceofeachexplanatoryvariablewascontrolledbythe effectoftheothers,eliminatingpotentialconfounders.
The study was approved by the Ethics Committees of theUniversidadeFederaldoCeará(No.734/06andCOMEPE protocol 238/06) and of the Universidade Federal de São Paulo(No.0804/09),inaccordancewiththeDeclarationof Helsinki.TheresearchprotocolwasapprovedbytheHealth SecretariatofFortaleza.Voluntaryandanonymous partici-pationwasguaranteedbytheinformedconsentgivenbefore theinterviews.
Results
The study included 2,732 infants, of whom 1,024 (37.7%) hadwheezingepisodesinthefirst12monthsoflife;16.2% ofthesehadrecurrentwheezing,withthreeormorecrises inthefirstyearoflife.
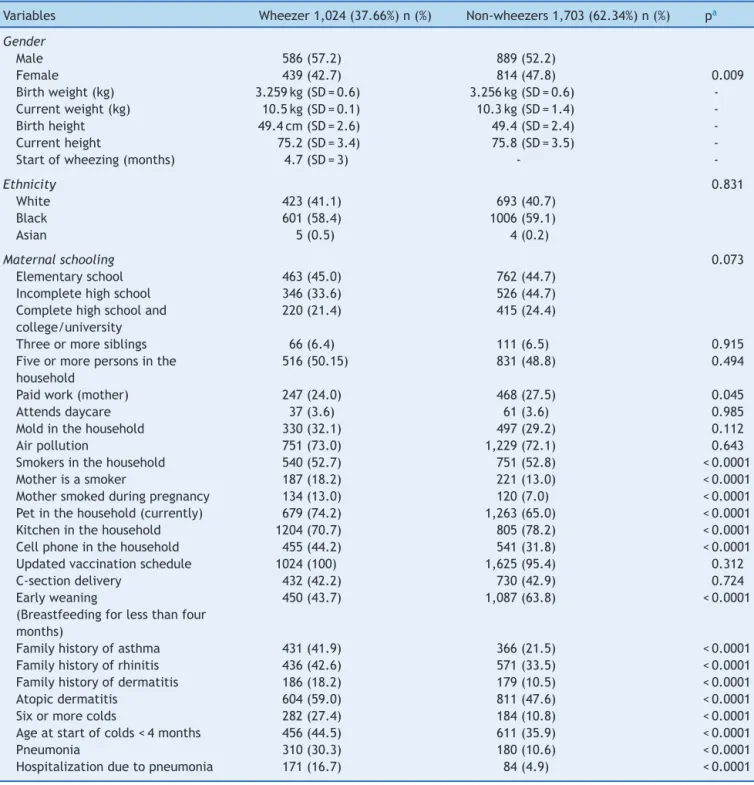
Around 57% of the wheezing infants were males, and 60%wereofblackormixed-raceethnicity.Themothersof these infants had low educationallevel, 70% had nopaid work, 18% were smokers, and 13% smoked during preg-nancy. The wheezing infants had twice the incidence of familyhistoryof asthma whencomparedtonon-wheezing infants,andthreetimesgreaterhistoryofcoldsand pneu-monia.Table1showsthecomparativeanalysisofwheezers andnon-wheezersaccordingtothedemographic, socioeco-nomic,environmental,family,andclinicalcharacteristicsof thestudypopulation.
Recurrent wheezers had more severe symptoms, noc-turnal symptoms, and visits to emergency rooms and hospitalizations for wheezing and pneumonia, when com-paredtoinfants withoccasionalwheezing. Around60% of recurrentwheezershadthefirstcrisisofwheezingbefore4 monthsofage,41.9%hadoversixepisodesofcoldsinthe firstyearof life,36.3%hadpneumoniainthefirstyear of life,and50.9%hadafamilyhistoryofasthma(Table2).
Thecomparativeanalysisbetweenthegroupsidentified severalisolatedfactorsthatwerethenevaluatedseparately regarding the outcome (wheezing). The univariate analy-sisidentifiedpossibleriskandprotectivefactors.Then,the independentvariableswereselectedtoconstitutethe logis-ticregressionmodel(adjustedOR),inordertocontroland eliminatepossibleconfoundingvariables.
Therewasanassociationofwheezingwithmalegender, lowmaternaleducation,familyhistoryofasthmaand der-matitis,moldinthehousehold,andmaternalsmokingduring andafterpregnancy.Therewasalsoasignificantassociation ofwheezingwithdermatitisandhighnumber(sixormore)of coldandpneumoniaepisodesinthefirstyearoflife. Mater-nal breastfeedinglastinglessthanfourmonthswasalsoa riskfactor,asshowninFig.1.
Themainriskfactorsassociatedwithrecurrentwheezing were familial asthma, early onsetof wheezing, nocturnal symptoms,oversixepisodesofcolds,asthmadiagnosis,and severesymptoms(Fig.2).
Discussion
Many studies worldwide have observed a high prevalence of wheezing during the first years of life. The first inter-nationalcomparisonofEISL14 studiedover 30,000children
Table1 Comparativeanalysisbetweenwheezers andnon-wheezersinthefirst yearoflife,accordingtothedemographic, socioeconomic,family,andclinicalcharacteristics.
Variables Wheezer1,024(37.66%)n(%) Non-wheezers1,703(62.34%)n(%) pa
Gender
Male 586(57.2) 889(52.2)
Female 439(42.7) 814(47.8) 0.009
Birthweight(kg) 3.259kg(SD=0.6) 3.256kg(SD=0.6) -Currentweight(kg) 10.5kg(SD=0.1) 10.3kg(SD=1.4)
-Birthheight 49.4cm(SD=2.6) 49.4(SD=2.4)
-Currentheight 75.2(SD=3.4) 75.8(SD=3.5)
-Startofwheezing(months) 4.7(SD=3) -
-Ethnicity 0.831
White 423(41.1) 693(40.7)
Black 601(58.4) 1006(59.1)
Asian 5(0.5) 4(0.2)
Maternalschooling 0.073
Elementaryschool 463(45.0) 762(44.7) Incompletehighschool 346(33.6) 526(44.7) Completehighschooland
college/university
220(21.4) 415(24.4)
Threeormoresiblings 66(6.4) 111(6.5) 0.915
Fiveormorepersonsinthe household
516(50.15) 831(48.8) 0.494
Paidwork(mother) 247(24.0) 468(27.5) 0.045
Attendsdaycare 37(3.6) 61(3.6) 0.985
Moldinthehousehold 330(32.1) 497(29.2) 0.112
Airpollution 751(73.0) 1,229(72.1) 0.643
Smokersinthehousehold 540(52.7) 751(52.8) <0.0001
Motherisasmoker 187(18.2) 221(13.0) <0.0001
Mothersmokedduringpregnancy 134(13.0) 120(7.0) <0.0001 Petinthehousehold(currently) 679(74.2) 1,263(65.0) <0.0001 Kitcheninthehousehold 1204(70.7) 805(78.2) <0.0001 Cellphoneinthehousehold 455(44.2) 541(31.8) <0.0001 Updatedvaccinationschedule 1024(100) 1,625(95.4) 0.312
C-sectiondelivery 432(42.2) 730(42.9) 0.724
Earlyweaning
(Breastfeedingforlessthanfour months)
450(43.7) 1,087(63.8) <0.0001
Familyhistoryofasthma 431(41.9) 366(21.5) <0.0001 Familyhistoryofrhinitis 436(42.6) 571(33.5) <0.0001 Familyhistoryofdermatitis 186(18.2) 179(10.5) <0.0001
Atopicdermatitis 604(59.0) 811(47.6) <0.0001
Sixormorecolds 282(27.4) 184(10.8) <0.0001
Ageatstartofcolds<4months 456(44.5) 611(35.9) <0.0001
Pneumonia 310(30.3) 180(10.6) <0.0001
Hospitalizationduetopneumonia 171(16.7) 84(4.9) <0.0001
SD,standarddeviation.
a p-value(Pearson’schi-squaredtest).
thereis a greatvariabilityin the prevalenceand severity ofwheezing inthedifferentcenters,butwithatendency to higher prevalence and severity in children from Latin America.
The prevalence of wheezing in that study, consider-ingthetotal studypopulation,was45.2%, 20.3%ofwhich corresponded torecurrent wheezing. When the data was stratifiedforLatinAmerica,theprevalencewas47.3%and 21.4% for wheezing andrecurrent wheezing, respectively,
andforEurope,34.4%,and15.0%,respectively.14 InBrazil,
theprevalence ofwheezinginthefirstyearofliferanged between43%and63.6%,and21.9%and36.6%foroccasional andrecurrentwheezing,respectively.Thevaluesobserved hereshowgreatvariability;thisdifferenceispossibly associ-atedwithdifferencesinclimatological,environmental,and socioeconomiccharacteristicsofdifferentregions.14
Table2 Comparisonbetweeninfantsthatareoccasionalandrecurrentwheezers,accordingtotheclinicalfeaturesandfamily history.
Variables Occasionalwheezer <threecrisesn=580(%)
Recurrentwheezer≥
threecrisesn=444(%)
pa
Malegender 309(53.3) 277(37.6) 0.003
Pneumonia 149(25.7) 161(36.3) <0.0001
Hospitalizationduetopneumonia 79(13.6) 92(20.7) 0.003 Hospitalizationduetobronchitis 29(5) 165(37.6) <0.0001
Passivesmoking 307(52.9) 233(52.5) 0.885
Maternalsmoking 92(15.9) 95(21.4) 0.024
Mothersmokedduringpregnancy 68(11.7) 66(14.9) 0.140 Historyofasthmainthefamily 205(35.3) 226(50.9) <0.0001 Historyofrhinitisinthefamily 255(43.9) 181(40.8) 0.305 Historyofdermatitisinthefamily 98(16.9) 88(19.8) 0.229
Dermatitis 331(57.1) 273(61.5) 0.154
Sixormorecolds 96(16.5) 186(41.9) <0.0001
Ageatstartofcolds<4months 204(35.2) 252(56.8) <0.0001 Ageofwheezing<4months 182(37.7) 238(60.7) <0.0001 Updatedvaccinationschedule 580(100) 444(100) 0.451
C-sectiondelivery 244(42.1) 188(42.3) 0.930
Useofbronchodilator 461(82.6) 371(85.3) 0.257
Useofinhaledcorticoids 120(23.7) 89(22.9) 0.786
Useofantileukotrienes 23(4.9) 10(2.9) 0.152
Visitstotheemergencyroom 360(62.1) 346(77.9) <0.0001
Severeepisodes 374(47.2) 278(62.6) <0.0001
Hospitalizationduetowheezing 75(12.9) 117(26.3) <0.0001
Diagnosisofasthma 59(10.2) 91(20.5) <0.0001
Frequentnocturnalsymptoms 930(16.0) 185(41.7) <0.0001 Maternalbreastfeeding<4months 163(31.5) 145(35.8) 0.634
ap-value(Pearson’schi-squaredtest).
ofrecurrentwheezingisbelowthatfoundinotherstudies usingtheEISLprotocol,10especiallyinBrazil.
The identification of the determinants of wheezing in infants has been the subject of several studies. In fact, several factors appear to play a decisive role in the triggering and maintenance of wheezing in infants, such as genetic, immunological, and environmental variables, as well as infection and maternal breastfeeding, among others.
This study showed a significant association of wheez-ing with respiratory infection for all types of wheezing. Respiratory infections are commonin childhood andhave an important role in infant morbimortality. They require several outpatient clinic visits, hospital admissions, and consequently increase public health care costs in many countries.15 There appearstobean importantassociation
betweenrespiratoryinfections,particularlythosecausedby viruses,andthepathogenesisofwheezinginchildhood.16,17
Male gender (OR=1.23) Low maternal schooling (OR=1.18) Paid work (OR=0.83) Pneumonia (OR=3.68)
Hospitalization due to pneumonia (OR=3.86) Smoker mother (OR=1.48)
Mother smoked during pregnancy (OR=1.97) Smokers at home (OR=1.114) History of asthma in the family (OR=2.63) History of rhinitis in the family (OR=1.46) History of dermatitis in the family (OR=1.89) Six or more colds (OR=3.11)
Age at start of colds < 4 months (OR=1.42) Dermatitis (OR=1.58)
Pet at home at birth (OR=0.88) Current pet at home (OR=0.67) Maternal breastfeeding < 4 months (OR=1.35)
Elementary maternal education (aOR=1.23)
IC OR Male gender (aOR=1.21)
Six or more colds (aOR=2.38)
Pneumonia (aOR=3.02) Dermatitis (aOR=1.36)
Mother smoked during pregnancy (aOR=1.44)
Smokers in the household (aOR=1.33) Mold in the household (aOR=1.25)
History of asthma in the family (aOR=2.12) History of dermatitis in the family (aOR=1.54)
Maternal breastfeeding < 4 months (aOR=1.22) Protective factors Risk factors
0.1 1.0 10.0
0.0 1.0 2.0 3.0 4.0
Male gender (OR=1.45)
Age at start of wheezing < 4 months (OR=2.55)
Pneumonia (OR=1.64) pneumonia por Hospitalization due to pneumonia
(OR=1.65)
bronquite por Hospitalization due to bronchitis (OR=2.40)
Smoker mother (OR=1.44)
Mother smoked during pregnancy (OR=1.31)
History of asthma in the family (OR=1.89)
Six or more colds (OR=3.63)
Hospital/emergency room visits (OR 2.15)
Severe crises and difficulty breathing (OR=1.87)
Medical diagnosis of asthma (OR=2.27)
Frequent nocturnal symptoms (OR=3.74)
Frequent nocturnal symptoms (aOR=2.56; 95%CI: 1.75-3.75) History of asthma in the family (aOR=1.73; 95%CI: 1.22-2.46)
Start of wheezing (aOR=1.83; 95%CI: 1.75-3.75)
More than six colds (aOR=2.07; 95%CI: 1.43-3.00)
Diagnosis of asthma (aOR=1.67; 95%CI: 1.02-2.76)
Severe symptoms and difficulty breathing (aOR=1.53; 95%CI: 1.10-2.17)
6.0 4.0 2.0 0.0 Age at start of colds < 4 months (OR=2.41)
Figure2 Riskfactorsassociatedwithrecurrentwheezingininfantsinthefirstyearoflife.CI,confidenceinterval;aOR,adjusted oddsratio.
The EISL showed a significant association between the occurrence of colds in the first three months of life and wheezingininfantsincountriesfromEuropeandLatin Amer-ica,especiallythosewithrecurrentwheezing.18
Otherfactorsalsocontributetotheriskofwheezing.In this study, a correlation was observed between wheezing andlowmaternaleducation,malegender,familyhistoryof asthma, and dermatitis. Several studies indicate genetics asadeterminantfactor forallergicdiseases.19,20 TheEISL
demonstratedastatisticallysignificantassociationbetween wheezingandfactorssuchasfamilyhistoryofasthmaand rhinitis.18 Italsoshowedtheassociation ofwheezing with
the male gender, especially in European countries when compared toLatin America.18 The male gender has been
identifiedasariskfactorforwheezingduringthefirstyears oflifeinseveralstudies.21
Otherfactorsalsocontributetotheriskofwheezingin infants. In this study,early weaning,defined asmaternal breastfeedinglastinglessthanfourmonths,appearedasa riskfactor.Breastfeedingiswidelypromotedasanimportant factorinreducingtheriskforatopyandasthma;however, theevidenceforthiseffectisstillveryconflicted.22
A prospective study performed in New Zealand with approximately1,000childrenindicated thatbreastfeeding isnotaprotectivefactorandmayevenincreasetheriskfor atopy.23Otherstudies,incontrast,havedemonstratedthat
exclusive breastfeedinghas asignificant protective effect against the development of recurrent wheezing, asthma, and atopy. However, this protective effect appears to be mediatedbynutrientsandindividualprotectionmechanisms and,toalesserextent,tofactorsrelatedtoatopy.24
Thisstudydemonstratedanassociationbetween wheez-ingandmaternal smokingduringandafterpregnancy.The harmful effects of smoking on children’s health are well known,but their potential impact onearly lung develop-mentislessclear.25Itisdifficulttoseparatetheeffectsof
pre-andpostnatalexposure,asmostwomenwhocontinue tosmokeduringpregnancy(approximately30%worldwide) donotstopthehabitafterthechildisborn26
However, assessments conducted before any postnatal exposure have shown significant changes in lung function innewborns whosemotherssmoked duringpregnancy,and thepersistenceoftobaccoexposureinthepostnatalperiod probablyincreasestheriskofrespiratorydiseases.27Astudy
conductedin Spain withover 20,000children and adoles-cents demonstratedthat environmental tobacco smoke is associatedwithahigherprevalence of asthmasymptoms, particularlyifthemotherorbothparentssmoke.28
In the present study, infants with recurrent wheezing episodes had early-onset wheezing, severe episodes, dif-ficulty breathing, nocturnal symptoms, family history of asthma,andamedicaldiagnosisofasthma.TheEISLfound similarresults,especiallyinLatinAmericancountries18and
inBraziliancities.29
Somepotentiallimitationsofthisstudywereidentified, suchastheveryhomogeneousstudypopulation(mostly low-income)anditscross-sectionaldesign,whichcouldpossibly influencethe results.In addition,interviews withparents orcaregiversabouteventsthatoccurredduringtheinfants’ firstyearoflifemaydepend ontheabilityofrespondents torecallfacts,especiallyregardingquestionsthatcontain ahighdegreeof subjectivity,suchasthethoserelatedto familyhistory.
Another important possible limitation was the evalua-tionofoutcomes(wheezing)inthisstudy,whichwasbased oninformationcollectedduringinterviews ratherthan on medicalrecords.However,thefactthatthepresentstudy is multicenter and that all the data come fromdifferent nationalandinternationalcentersmayminimizethese lim-itations.
thosefoundinotherstudiesusingtheEISLprotocol, espe-cially in Brazil. It also evidenced a strong association of wheezingwithahistory ofrespiratoryinfections, asthma, and atopic dermatitis in the family. Moreover, it demon-stratedthat infants withover threeepisodesof wheezing haddifficultybreathing,severeepisodes,nocturnal symp-toms,andamedicaldiagnosisofasthma.
This study indicates a multifactorial pathogenesis of wheezingin thefirst yearof life,which is closely related to respiratory infections.Considering that many cases of asthmapresenttheinitialsymptomsearlyinthefirstyear oflife,itshouldbeapriorityofpublichealthpolicytoknow theprevalence andriskfactorsofthisdisease,inorderto develop control and treatment strategies that impact on morbidityandmortalityofthesediseases,andimprovethe qualityoflifeofthesechildrenandtheirfamilies.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgements
TheauthorswouldlikethanktheteamsoftheBasicFamily HealthUnitsofFortalezafortheirsupportandcooperation.
References
1.SoléD.Sibilâncianainfância.JBrasPneumol.2008;34:337---9.
2.DeJongBM,vanderEntCK,vanPutteKatierN,vanderZalm MM,VerheijTJ,KimpenJL,etal.Determinantsofhealthcare utilizationforrespiratorysymptomsinthefirstyearoflife.Med Care.2007;45:746---52.
3.Organizac¸ão Pan-Americana de Saúde. Saúde nas Américas 2007. [cited 15 Sept 2010]. Available from: http://bvsms.saude.gov.br/bvs/publicac¸ões
4.Ministério da Saúde (Brasil). Sistema de Informac¸ões Hos-pitalares do SUS - SIH/SUS/SE/Datasus, 2008. [cited 20 Sept2010].Availablefrom.http://tabnet.datasus.gov.br/cgi/ tabcgi.exe?idb2009/d13.def
5.KoopmanLP,BrunekreefB,deJongsteJC,NeijensHJ.Definition ofrespiratorysymptomsanddiseaseinearlychildhoodinlarge prospectivebirthcohortstudiesthatpredictthedevelopment ofasthma.PediatrAllergyImmunol.2001;12:118---24.
6.Piippo-SavolainenE,KorppiM.Wheezybabies:wheezyadults? Reviewonlong-termoutcomeuntiladulthoodafterearly child-hoodwheezing.ActaPaediatr.2008;97:5---11.
7.JacksonDJ,LemanskeJrRF.Theroleofrespiratoryvirus infec-tionsinchildhoodasthmainception.ImmunolAllergyClinNorth Am.2010;30:513---22.
8.SinghAM,MoorePE,GernJE,LemanskeJrRF,HartertTV. Bron-chiolitistoasthma:areviewandcallforstudiesofgene---virus interactionsinasthmacausation.AmJRespirCritCareMed. 2007;175:108---19.
9.KurukulaaratchyRJ,MatthewsS,HolgateST, ArshadSH. Pre-dictingpersistentdiseaseamongchildrenwhowheezeduring earlylife.EurRespirJ.2003;22:767---71.
10.InternationalStudyofWheezinginInfants2006.[cited15Aug 2010].Availablefrom:http://www.respirar.org
11.InternationalStudyofAsthmaandAllergiesinChildhood Steer-ingCommittee.Worldwidevariationinprevalenceofsymptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema. Lancet.1998;351:1225-32.
12.Secretaria Municipal (Fortaleza). Relatório de gestão da saúde, 2007. [cited 19 Sept 2010]. Available from: www.sms.fortaleza.ce.gov.br
13.ChongNetoHJ,RosarioN,DelaBiancaAC,SoléD,MallolJ. Vali-dationofaquestionnaireforepidemiologicstudiesofwheezing ininfants.PediatrAllergyImmunol.2007;18:86---7.
14.MallolJ,García-MarcosL,SoléD,BrandP,theEISLStudyGroup. Internationalprevalenceofrecurrentwheezingduringthefirst yearoflife:variability,treatmentpatternsanduseofhealth resources.Thorax.2010;20:1---26.
15.StevensCA,TurnerD,KuehniCE,CourielJM,SilvermanM.The economicimpactofpreschoolasthmaandwheeze.EurRespir J.2004;23:961.
16.Busse WW, Lemanske Jr RF, Gern JE. Role of viral respira-toryinfectionsinasthmaandasthmaexacerbations.Lancet. 2010;376:826---34.
17.KuselMM,deKlerkNH,HoltPG,KebadzeT,JohnstonSL,SlyPD. Roleofrespiratoryvirusesinacuteupperandlowerrespiratory tractillnessinthefirstyearoflife:abirthcohortstudy.Pediatr InfectDisJ.2006;25:680---6.
18.Garcia-MarcosL,MallolJ,SoléD,BrandPL,EISLStudyGroup. Internationalstudyofwheezingininfants:riskfactorsin afflu-ent and non-affluent countries during the first year of life. PediatrAllergyImmunol.2010;21:878---88.
19.HollowayJW, Arshad SH, Holgate ST. Usinggenetics to pre-dict the naturalhistory of asthma? J Allergy Clin Immunol. 2010;126:200---9.
20.OberC,YaoTC.Thegeneticsofasthmaandallergicdisease:a 21stcenturyperspective.ImmunolRev.2011;242:10---30.
21.Melen E, Kere J, Pershagen G, Svartengren M, Wickman M. Influence of male sex and parental allergic disease on childhood wheezing: role of interactions. Clin Exp Allergy. 2004;34:839---44.
22.OddyWH.A reviewoftheeffects ofbreastfeedingon respi-ratory infections, atopy, and childhood asthma. J Asthma. 2004;41:605---21.
23.SearsMR,GreeneJM,WillanAR,TaylorDR,FlanneryEM,Cowan JO,etal.Long-termrelationbetweenbreastfeedingand devel-opmentofatopyand asthmainchildrenandyoung adults:a longitudinalstudy.Lancet.2002;360:901---7.
24.ScholtensS,WijgaAH,BrunekreefB,KerkhofM,HoekstraMO, GerritsenJ,etal.Breastfeeding,parentalallergyandasthma inchildrenfollowedfor8years.ThePIAMAbirthcohortstudy. Thorax.2009;64:604---9.
25.Le Souef PN. Pediatric origins of adult lung diseases Tobacco related lung diseases begin in childhood. Thorax. 2000;55:1063---7.
26.Stocks J, Dezateux C. The effect of parental smoking on lung function and development during infancy. Respirology. 2003;8:266---85.
27.DiFranzaJR, AligneCA,WeitzmanM.Prenataland postnatal enviromentaltobacco smokeexposureand children’shealth. Pediatrics.2004;113:1007---15.
28.Gonzalez-BarcalaFJ,PertegaS,SampedroM,LastresJS, Gon-zalezMA,Bamonde L, et al. Impactofparental smoking on childhoodasthma.JPediatr(RioJ).2013;89:294---9.