w w w . j c o l . o r g . b r
Journal
of
Coloproctology
Original
Article
Proposed
tuberculosis
investigation
and
management
protocol
in
complex
and
recurrent
fistula-in-ano
Leonardo
Guedes
Leite
de
Oliveira
a,
João
de
Aguiar
Pupo
Neto
a,
Eduardo
de
Paula
Vieira
a,
Monika
Pereira
Kim
a,
Luciana
da
Costa
Flach
a,
Barbara
Cristina
Rodrigues
de
Almeida
b,
Edna
Delabio
Ferraz
a,∗aColorectalSurgeryUnit,HospitalUniversitárioClementinoFragaFilho(HUCFF),UniversidadeFederaldoRiodeJaneiro(UFRJ),
RiodeJaneiro,RJ,Brazil
bPathologyUnit,HospitalUniversitárioClementinoFragaFilho(HUCFF),UniversidadeFederaldoRiodeJaneiro(UFRJ),RiodeJaneiro,
RJ,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received10July2014 Accepted2February2015 Availableonline8April2015
Keywords: Tuberculosis Rectalfistula Analcanal Recurrence Protocol Diagnosis
a
b
s
t
r
a
c
t
Background:Tuberculosis(TB)isanancientdisease,endemicinsomeregions,causedby Mycobacteriumtuberculosis.Among22countriesaccountingfor90%oftuberculosiscases worldwide,Braziloccupiesthe17thplace.Thegastrointestinalformrankssixth(5%)of extrapulmonarycases,while anorectalrepresents2–7% ofcasesoffistula-in-ano,more commoninmidlifemen,fromendemicregions.Inourcountryepidemiologicaldataand accumulatedclinicalevidencestronglysuggesttheneedforasystematicTBresearchasa responsibleco-factorforcomplexanalfistulasoralsothoseimmunosuppressionassociated, inanattempttoreducethehighratesofrecurrenceofanalfistula(>30%).
Purpose:Thecoursefromacomplexanaltuberculosisassociatedfistula,confirmedafter initialsuspicionofCrohn’sdisease,ispresentedinordertoemphasizetherelevanceof suspicionandadiagnosisprotocol,aswellashealingcriteriainfistulascontaminatedby thebacilli.
Discussion: Sphincterdamageriskinrepeatedfistula-in-anosurgicalapproachesrequires consideringtuberculosisinfection,anunderdiagnosedcondition,andapreoperative diag-nostic routine should be suggested. In the absence of description in the literature, preliminaryclinicalprotocolsmustbeprovidedinordertoreducerecurrenceandsphincter damagerates,whenindicatingsurgicaltreatmentofthedisease.
©2015SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.All rightsreserved.
∗ Correspondingauthor.
E-mail:edna.delferraz@yahoo.com.br(E.D.Ferraz). http://dx.doi.org/10.1016/j.jcol.2015.02.004
Proposta
de
investigac¸ão
e
tratamento
da
tuberculose
em
fístulas
anorretais
complexas
e
recorrentes
Palavraschave: Tuberculose Fístulaanal Canalanal Recorrência Protocolo Diagnóstico
r
e
s
u
m
o
Introduc¸ão: Atuberculose(TB)éumadoenc¸aancestral,endêmicaemalgumasregiões,e causadapeloMycobacteriumtuberculosis.Entre22paísesresponsáveispor90%doscasosde tuberculoseemtodoomundo,oBrasilocupao17◦lugar.Aformagastrointestinalestáem
sextolugar(5%)doscasosextrapulmonares,enquantoaanorretalrepresenta2–7%doscasos defístulaanal,sendomaiscomumemhomensdemeia-idadeederegiõesendêmicas.Em nossopaís,osdadosepidemiológicoseevidênciaclínicaacumuladasugeremfortementea necessidadedeumainvestigac¸ãosistemáticaTBcomoumcofatorresponsávelporfístulas anaiscomplexasoutambémassociadaàimunossupressão,natentativadereduzirasaltas taxasderecorrênciadefístulaanal(>30%).
Objetivo: Ocursodeumafistulaanalcomplexaassociadaàtuberculose,confirmadaapós suspeitainicialdedoenc¸adeCrohn,éapresentadaafimdeenfatizararelevânciadasuspeita edeumprotocolodediagnóstico,bemcomooscritériosdecuraemfístulascontaminados pelobacilo.
Discussão: Oriscode danosnoesfíncternasabordagenscirúrgicasrepetidasda fistula analrequerconsiderarainfecc¸ãoportuberculosecomoumadoenc¸asubdiagnosticada.Na ausênciadedadosdaliteratura,sugere-seumarotinadediagnósticopré-operatórioe proto-colosclínicospreliminaresafimdereduzirarecorrênciadadoenc¸aeaocorrênciadedanos aoesfíncter.
©2015SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda. Todososdireitosreservados.
Introduction
Tuberculosis,anendemicworldwidecondition,hasits inci-denceaggravatedbytheAIDSepidemic,multidrugresistance pulmonarytuberculosis,highpovertyrateandmigration.1,2
According to the WHO up to a third population would beinfectedwithMycobacteriumtuberculosis,reachingalmost 9 million new cases and 1.4 million deaths in 2011 (990,000amongHIV-seronegativeindividualsand430,000HIV seropositive).3Inthiscontext,Braziloccupiesthe17thplace
amongthe 22countriesresponsiblefor90%oftuberculosis casesworldwide, therefore responsible forthe higher inci-denceandmortalityin2012.3
Fistula-in-anorecognitionisdatedfromancienttimes,4,5
constituting a commonly benign disease found in surgical practice,revealingahighincidence–2:10,000inhabitants– andmostoftenaffectingmales(2:1).6
Complexandrecurrentanalfistulasmayrequirerepeated surgicalinterventionsresultinginahighriskofincontinence.5
Mostfistulashavecryptoglandularnonspecificorigin.Less fre-quent,butnotleast,analfistulasattributedtoothercauses, suchasCrohn’sdiseaseandtuberculosis(TB),7andthisshould
bereminded.
Anoperineal tuberculosis commonly coexists with anal fistulapresentation,representing90%ofcases.2Complex
fis-tulasinpatientswithhumanimmunodeficiencyvirus(HIV) andactivepulmonaryTBshouldbeevaluatedwithahighlevel ofsuspicionfortuberculosisetiology.1,8,9However,diagnosis
isdifficultinhealthypatients.DatahavesuggestedTBasa relevantfactorresponsibleinrecurrence.10
Thelackofconsensus,regardingdiagnosticinvestigation routinesforTBinfectioninthetreatmentofanalfistula,5,10
allowsrekindlingthisdebate.Toexcludethe persistenceof TBasacausalagentofrecurrenceissuggestingasystematic routinelaboratoryresearch,basedonclinicaldataofthiscase, whichfeaturedatotallyatypicalprofileinafemalepatient.
Case
report
Asingle24-year-oldwomanwasadmittedpresenting anovul-varabscessandfistulousholesintheleftglutealandperianal region.
Symptomsstarted12monthsearlierwithapainfulgluteus bulgingwhichdrainedspontaneously. Onclinical examina-tion werefoundfourfistulous orifices(leftgluteous,rootof theleftthigh,rightofthevaginalfourchetteandrightperianal region), posterior edematous fibrotic anal plicoma, sphinc-terhypertoniaandanuscopyunderminedbypain.Amonth beforeadmission,fistulographyatanotherinstitutionshowed complexhighsupralevatorhorseshoefistula,andsecondary tracks to perianal right left gluteus. Another track ending blindly,ontheright,goestowardvulva(Fig.1AandB).AMRI (magnetic resonance imaging) and ERUS (endorectal ultra-ssound)confirmedthetracks(Fig.1C–F).
A
B
Vaginal track
E
3
2
Gluteous
Vulvar
Vulvar track Horseshoe
track 1
5 4
6
Perineal track
Gluteal track
I.O.
E.O.
C
D
E
F
Fig.1–Fistulographyimagesofhorseshoetrackinantero-posteriorfistulography(A)showingleftglutealexternalorifices
[1,2],lefthorseshoetrackcommunicatingleftischiorectalfossatrackandhole[3],righthorseshoetracknexttolevatorani,
whichcommunicateswiththeinternalholeinanteriorposition[4],perianalipsilateralexternalorifice[5]andthe
superficialblindlybranchinrightlargelabia[6]thatevolvesintonewexternalorifice,observedonadmission;andits
schematicsuperposition(B).MRIimageshowingtheischiopubictrackandleftperinealovalfistulaextendingtothegluteal
region(C)andperianaltrackandvulvarcompromise(D).Endoanal3Dultrasonography(ERUS)confirmedahorseshoe
multipleandcomplextracksfistula(EandF).
A
B
C
Gluteous Vulvar
Fig.2–Perianalregionappearance.InitialFoleysetondrainage(A)changedtopolypropylenesetonatthesecondsurgical
exploration(B).Thevulvartrackwastreatedbycuttingsetontechnique(blackarrow).Finally,12monthsafteranti-TB
Fig.3–Photomicrographsofhistologicalsectionsoffistula.(A)and(B)Areawithgiantcellgranuloma(Langerhanscells)
techniqueusinghematoxylin–eosin;notethecharacteristicalignmentofnucleiinthevicinityofthegiantcell,
characteristicoffusionofmacrophages(400×).(C)and(D)Hematoxylin–eosinstaininginanoutbreakofliquefaction
necrosisamidchronicinflammatoryinfiltrate(10×and40×magnification).(E)and(F)Anicheofalcohol-acid-fastbacilli,
somewithinhistiocytes,inWadestainingtechnique(40×and100×magnification).
and therefore Crohn’s disease was strongly suspected. In ileocolonoscopymilderosivelesionsinterminalileumwere found,reinforcingtheinitialsuspicion,butbiopsiesshowed “chronicgranulomatousileitiswithnecrosis”.Afterdischarge, drainagepersisted,withreappearingfeverandvaginal phleg-mon, and the patient was readmitted for new surgical exploration and seton change was carried out. Secretions werecollectedrevealingEscherichiacoligrowinginculture,“a chronicgranulomatousprocess”andthepresenceof alcohol-acid-fast bacilli, observed in hematoxylin–eosin and Wade stainingparaffinsections(Fig.3C–F).Theintradermaltestwith purifiedproteinderivative(PPD)was7mm.Serologictestsfor HIV,hepatitisandLueswerenegative.
Whenreferredtoatuberculosiscontrolprogram,patient reportedweightlossandvespertinefever,andspecific treat-mentwasstarted.Achestradiographicreevaluationrevealed streaks and dense nodules in the apical segment at the rightlung.Inducedsputumbacilloscopywasnegativebut a mycobacterial culturewas positive on the 34th day and a
schemewithRifampicin,Isoniazid,Pyrazinamideand Etham-butol(RIPE)wasstarted.Fivemonthsafterthebeginningof RIPEscheme,shewasasymptomaticandtherewasa signif-icant improvementoffistulassuppuration; sodrugschema was reduced toRifampicin and Isoniazid atfourth month. Twoinducedsputumbacilloscopywerenegative. Mycobacte-rialculture(inducedsputum)wasnegativeinthesixthmonth oftreatment.
Discussion
Fistula-in-ano is known since Hippocrates and has been describedoverthecenturies.In1835,FrederickSalmon inau-gurated the Fistula Infirmary – a clinical precursor of St. Mark’sHospitalforFistulaandotherDiseasesoftheRectum – where he treated fistula of several authorities.11
Good-sall (1900)became populardescribing fistula-in-anodetails andlaterParks(1976)namedtheworld’smostwidelyused classification.6Thiscryptoglandularnonspecificinfection
sur-gicalconditionisresponsiblefor90%ofallanorectalabscesses focusing on 5.6/100,000 women and 12.3/100,000 men.1,10
Thetuberculosis origin is uncommon and possibly under-diagnosed.Amongthe anorectal manifestationscommonly associatedwithtuberculosis(TB),fistulaisthemostfrequent complication.1,7Pathogenesisofperianalfistulasinpatients
withTBisstillcontroversial.Authorsconsiderthetropismof Koch’sbacillusintolymphatictissues.12However,other
mech-anismsmay explainthe presenceofKoch’sbacillus inthe perianalregion,suchas:(a)hematogenous,1,2,9(b)lymphatic,
originatingfrominfectedlymphnodes,2,9(c)ingestionof
con-taminatedmilk1 orswallowinginfectedbacillisputumfrom
activepulmonaryfoci1,2,9oreven(d)directdisseminationfrom
infectedadjacentorgans.2,9
Europeanstudiesshowastrongassociationofanalfistula andpulmonaryTB,althoughIndiandataarenotconvincedof thisassociation.1,13SexualtransmissionofM.tuberculosis
dur-inganalintercoursehasbeensuspected,butnotyetproven.2
Ontuberculosis,thisaccompaniedmankindsince prehis-torictimes.Itscharacteristiclesionswerefoundinmummies, andinIncaandAmericanIndiansbeforeColumbus.InBrazil, itisanendemicinfectiousdiseasecausedbyM.tuberculosis, theprincipaletiologicagent,identifiedbyRobertKoch(1882), whonamedthe bacillus.14 M.bovis maybeinvolved
some-times, and rarely other mycobacteria. Itremains a serious global health infectious condition, causing pulmonary dis-easeinmostcases.1TheWorldHealthOrganization(WHO)
estimatesthatone-thirdofthepopulationcouldbeinfected withM.tuberculosisin2012.Theincreasingincidence world-wideisduetotheAIDSepidemic,TBwithstandardmultidrug resistance,highlevelsofpovertyandmigration.1,15Brazilstill
remainsinthe22countriesgroupresponsiblefor82%ofTB casesintheworld.16
AnoperinealTBisconsidered anuncommonevent1 and
anorectalfistulaisthemostfrequentpresentation(upto90% ofcases)indistinguishablefromthoseofcryptoglandular ori-gin. TBincidence in complex fistulae is above 60%.17 Low
incidencehasbeenreported,suchasintheUnitedKingdom(6 casesinthelast25years)1aswellasinendemicregionssuch
asMorocco,whichdoesnotexceed1%.8However,these
num-bersarehigherinIndiawhichhighlightsShuklaetal.series18
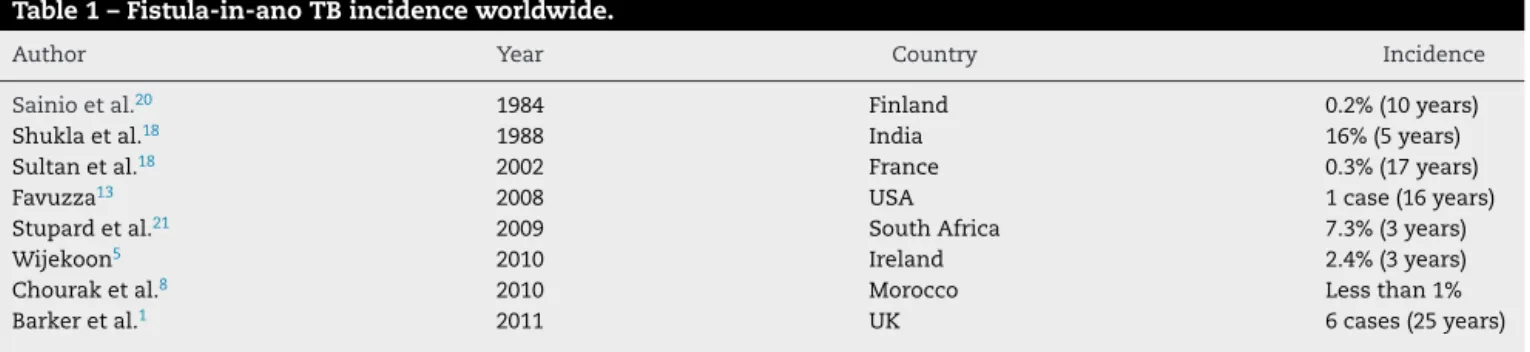
confirmingtuberculosisorigininalmost16%ofcasesofanal fistula.ThetypicalcaseoffistulaTBoriginwouldbean immi-grantman,middleagedandbelongingtoalowsocioeconomic class.17,19Wesummarizethestudiesreviewed(Table1).
ClinicalsuspicionofTBinanalfistulaisextremelydifficult duetotheabsenceofatypical,localorsystemicpattern. Fur-thermore,pulmonarylesionsoccurrencemaynotprecedethe fistulatuberculosisinfection.Thecasepresentedinthisarticle hasanatypical profile,and theradiologicdiagnosisof pul-monarylesioncamelater,leadingtoanothergranulomatous diseasessuspicion,suchasCrohn’sdisease,alsosupportedby thepresenceofileitisinwhichilealbiopsiesalsocollaborated fornotincludingTBasinitialsuspicion,sincetheyshowed nonspecificchanges.TheclinicalpresentationofTBinanal fistularecordedintheliteratureisdiverse,butahighdegree ofsuspicionshouldbeconsideredwhenevaluatingapatient with recurrentcomplex anal fistula,inimmunosuppressed patients,orwhenthereisaninitialsuspicionofCrohn’s dis-ease.
Laboratory diagnosis of Koch’s bacillus from collected secretions depends on the use of specific stains such as Ziehl–Neelsenorbacteriologicalstudies.Thesetestsshouldbe performedroutinelyinallpatientswithcasesofcomplex fis-tulas,especiallyinpatientsfromendemicregions.Evenso,the diagnosismaybelimited,asinthepresentcaseinwhich etio-logicagentidentificationoccurredcasuallyinthefirstsample (rarebacilliinhistologicsections).EventhoughTBtests sen-sitivityisstilllimited,asalreadyindicatedbythemajorityof authorswhostudythesubject,moleculardetectionmethods, suchasPCR(proteinchainreaction),arenowavailable.
Itisalsoimportantthatsurgeonsandendoscopistsbealert forthehighdegreeofsuspicioncases,requiringbacilloscopy withappropriatestainingandculture,fromallcollected mate-rialssuchassamplesofmucosa,skinorexcisedfistuloustract. Innegativecases,whensuspecteddiagnosticsuspicion per-sists,thePCRshouldbeindicated.
Finally,itisworthemphasizingtheabsenceofcure crite-riadefinitionforTBassociatedtocomplexfistula-in-anoin literaturedata.9,14Unlikelyulcerativeanorectalandperianal
TBforms,whereit iseasy todetermineclinicalcure (clini-calhealingfindingsinresponsetotreatment),analfistulas, withmultiple/meanderingpathsandcomplexpresentation, may have local TB curedifficult to determine, raising the
Table1–Fistula-in-anoTBincidenceworldwide.
Author Year Country Incidence
Sainioetal.20 1984 Finland 0.2%(10years)
Shuklaetal.18 1988 India 16%(5years)
Sultanetal.18 2002 France 0.3%(17years)
Favuzza13 2008 USA 1case(16years)
Stupardetal.21 2009 SouthAfrica 7.3%(3years)
Wijekoon5 2010 Ireland 2.4%(3years)
Chouraketal.8 2010 Morocco Lessthan1%
Search for Mycobacterium tuberculosis
Bacilloscopy
Saline swab, secretions or tissue Ziehl-Neelsen or Wade
1-3 days
Culture
Saline swab or secretions or tissue sample
3-8 days
Real time PCR
Saline swab, secretions or parafine Xpert® MTB/RIF
24 hours
Seton
(loose seton drainage)
Complex fistula-in-ano
(multiple holes/tracks, recurrence, immunosuppression, Crohn’s suspicion)
Fig.4–Diagnosisandmanagementoffistula-in-anoinhighdegreeofsuspicionforTBinfectionscheme.
riskoffailureofdefinitivesurgicaltreatment,andthe con-sequent unfortunate recurrence. Authors correlate surgical fistularecurrencetoTBasaco-responsiblefactor.9Basedon
thesedatawecanaffirmthatthedefinitivesurgicaltreatment shouldonly beperformedafter excluding TBorconfirmed healing oflocal TB infection. Therefore, curing lung focus shouldnotbeenoughtodeterminethehealingofperineal TBfocusinfection.Inthediagrambelow,thestepsforproper researcharesuggested(Fig.4).
Conclusion
Inthose strong initialTBsuspicion cases,aswell asthose confirmed TBfistulas,curettage ofthe tracks and biopsies shouldbeperformed.Samplesshouldbesentforbacilloscopy andTBculture.Diagnosticconfirmationmay include histo-logicalanalysisbyZiehl–NeelsenorWadestain,mycobacterial cultureandpolymerasechainreaction(PCR).PCRmaybe indi-catedwithagreatcost-effectivemethodcurrentlyavailable, whichhasgreatlyhelpedtheconfirmationofcure.Whilethis confirmationdoesnotoccur,keepingthetracksdrainedand repairedwithsetonmaybethebestapproach.Definitive fis-tulasurgerybeforeconfirmingTBfocuseliminationmayresult indiseaserecurrence.
r
e
f
e
r
e
n
c
e
s
1. BarkerJA,ConwayAM,HillJ.Supralevatorfistula-in-anoin tuberculosis.ColorectalDis.2011;13(2):210–4.
2. GuptaPJ.Ano-perianaltuberculosis–solvingaclinical dilemma.AfrHealthSci.2005;5(4):345–7.
3. WorldHealthOrganizationGlobalTuberculosisReport;2012. Availablefrom:http://apps.who.int/iris/bitstream/
10665/75938/1/9789241564502eng.pdf[accessedApril2013].
4.GeorgeU,SahotaA,RathoreS.MRIinevaluationofperianal fistula.JMedImagingRadiatOncol.2011;55(4):391–400. 5.WijekoonNS,SamarasekeraDN.Thevalueofroutine
histopathologicalanalysisinpatientswithfistulain-ano. ColorectalDis.2010;12(2):94–6.
6.OmmerA,HeroldA,BergE,FürstA,SailerM,SchiedeckT, etal.Cryptoglandularanalfistulas.DtschArzteblInt. 2011;108(42):707–13.
7.BeckDE,RobertsPL,RombeauJL,StamosJ,WexnerSD. Benignanorectalabscessandfistula.In:TheASCRS manualofcolonandrectalsurgery.Springer;2009. p.273–309[Chapter13].
8.ChourakM,BentamaK,ChamlalI,RaissM,HroraA,SebbahF, etal.Analfistulawithatuberculousorigin.IntJColorectal Dis.2010;25(8):1035–6.
9.ShanYS,YanJJ,SyED,JinYT,LeeJC.Nestedpolymerase chainreactioninthediagnosisofnegativeZiehl–Neelsen stainedMycobacteriumtuberculosisfistula-in-ano:reportof fourcases.DisColonRectum.2002;45(12):1685–8.
10.BokhariI,ShahSS,InamullahMehmoodZ,AliSU,KhanA. Tubercularfistula-in-ano.JCollPhysSurgPak.
2008;18(7):401–3.
11.BlackN.ThelosthospitalsofStLuke’s.JRSocMed. 2007;100(3):125–9.
12.NadalSR,NadalCRM,LopesMC,SperanziniMB.Fístula perianalemtuberculosos.RevBrasColoproct.
1993;13(4):141–3.
13.FavuzzaJ,BrotmanS,DoyleDM,CounihanTC.Tuberculous fistulaeinano:acasereportandliteraturereview.JSurg Educ.2008;65(3):225–8.
14.FelicioF,D’AcamporaA,BauerO,SantosJM,CorreaMB, HeinzenRPS.Tuberculoseano-retal.ArqCatarinMed. 1991;20(213):109–12.
15.Seow-ChoenF,NichollsRJ.Reviewanalfistula.BrJSurg. 1992;79(3):197–205.
17.SultanS,AzriaF,BauerP,AbdelnourM,AtienzaP.Anoperineal tuberculosis:diagnosticandmanagementconsiderationsin sevencases.DisColonRectum.2002;45(3):407–10.
18.ShuklaHS,GuptaSC,SinghG,SinghPA.Tubercularfistulain ano.BrJSurg.1988;75(1):38–9.
19.MolloyD,SayanaMK,KeaneJ,MehiganB.Analfistula:an unusualpresentationoftuberculosisinamigranthealthcare professional.IrJMedSci.2009;178(4):527–9.
20.SainioP.Fistula-in-anoinadefinedpopulationincidenceand epidemiologicalaspects.AnnChirGynaecol.
1984;73(4):219–24.
![Fig. 1 – Fistulography images of horseshoe track in antero-posterior fistulography (A) showing left gluteal external orifices [1,2], left horseshoe track communicating left ischiorectal fossa track and hole [3], right horseshoe track next to levator ani, w](https://thumb-eu.123doks.com/thumbv2/123dok_br/14977524.510170/3.918.186.746.97.720/fistulography-horseshoe-posterior-fistulography-horseshoe-communicating-ischiorectal-horseshoe.webp)