jcoloproctol(rioj).2015;35(2):124–127
w w w . j c o l . o r g . b r
Journal
of
Coloproctology
Case
Report
Granular
cell
tumor
of
rectal
submucosa:
case
report
Suheyla
Pollyana
Pereira
Ribeiro
a,∗,
Stephanie
Fonseca
Levy
a,
Flávia
Motta
Corrêa
a,
Aryanna
Musme
de
Araujo
e
Sousa
a,
Felipe
da
Costa
Silveira
b,
Marcos
Rodrigo
Carvalho
b,
Fang
Chia
Bin
baFaculdadedeCiênciasMédicasdaSantaCasadeMisericórdiadeSãoPaulo(FCMSCSP),SãoPaulo,SP,Brazil
bUniversityHospital,FaculdadedeCiênciasMédicasdaSantaCasadeMisericórdiadeSãoPaulo(FCMSCSP),SãoPaulo,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received2October2013 Accepted11August2014 Availableonline7April2015
Keywords:
Granularcelltumor Granularcellmyoblastoma Colonoscopy
Rectum
Immunohistochemistry
a
b
s
t
r
a
c
t
Thisisacasereportofgranularcelltumorofrectalsubmucosainafemale,35-years-old patientcomplainingofhematochezia.Wedescribethehistologicaland immunohistochem-icalfeaturesofthelesionresponsiblebythisclinicalfind.Followingthat,wepresenta discussionofthecasebasedontheliteraturereview,whichallowedtoprovingthe infre-quencyofthetumorintherectalareaandconfirmsthebenignnatureofthetumorinthis case.
©2015SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.All rightsreserved.
Tumor
de
células
granulares
da
submucosa
rectal:
relato
de
caso
Palavraschave:
Tumordecélulasgranulares Mioblastomadecélulasgranulares Colonoscopia
Reto
Imunohistoquímica
r
e
s
u
m
o
Esteartigorelataocasodeumtumordecélulasgranularesdasubmocosaretal,empaciente de35anos,comqueixadehematoquezia.Fazemosadescric¸ãodosachadoshistológicose imuno-histoquímicosdalesão.Alémdisso,apresenta-seumadiscussãodocasocombase narevisãodaliteratura,quepermitiucomprovarainfrequênciadotumornaregiãoretale corroborarabenignidadedotumornopresentecaso.
©2015SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda. Todososdireitosreservados.
∗ Correspondingauthor.
E-mail:suheylaribeiro@hotmail.com(S.P.P.Ribeiro).
http://dx.doi.org/10.1016/j.jcol.2014.08.015
jcoloproctol(rioj).2015;35(2):124–127
125
Introduction
Thegranularcelltumor,formerlycalledgranularcelltumor myoblastomaorAbrikossoftumor,isarareneoplasticprocess predominantlybenign.Itaffectsdifferentregionsofthebody, butthelesionsinthegastrointestinaltractrepresentonly10% ofthecases.1–4
Thepatientwiththistumorisusuallyasymptomaticand diagnosedasanincidentalfinding duringtheinvestigation ofotherpathologies. Thestudy withpathologicalassays is thegoldstandardforconfirmingthepresenceofthiskindof tumor.5–7
Althoughmostpartofthelesionsarebenign,asmall num-ber shows malignant behavior and about 2%of them can metastasize,especiallythosewithatypicalhistologyorlarge diameter.Inthesecases,it isnecessarytoconduct further investigationsandapplymoreaggressivesurgeryresections asplan oftreatment.8–10 Wereporta caseof granularcell
tumor, in a young female patient complaining of hema-tocheziaforoneyear,attheColoproctologyDepartmentofthe UniversityHospitalSantaCasadeSãoPauloin2013.
Case
report
L.V.A., female, 35 years old, born and raised in São Paulo –Brazil,complainedofanone-yearhistoryofhaemochezia associatedwithcolicabdominalpaininthelowerquadrants, withnobowelhabitschange,duringamedicalattendingof theColoproctologyClinicsatUniversityHospitalSantaCasa deSãoPaulo.Regardingherpastmedicalhistory,shehadbeen smokingfor10yearsandhadahistoryofhemorrhoidal dis-easefor17years.Withregardtothefamilyhistory,hermother hadintestinalpolypsanddiverticulardisease.
Physicalexamination
Onphysicalexamination,thepatientwasinpainonpalpation oftherightiliacfossa,withnoreboundtenderness.On procto-logicalexamination,skintagscompatiblewithhemorrhoids wereobservedintherightlateral,posteriorleft lateraland anterior regions. The anuscopy showed hemorrhoidal pro-trudingnipplesintherightlateral,leftlateralandposterior left.
Complementaryexams
The upper endoscopy identified an erosive esophagitis classifiedasLosAngelesA,aflatandmoderateerosive bul-boduodenitisandanesophagealpolypoidlesion.Pathologic examinationrevealedamildchronicesophagitis.
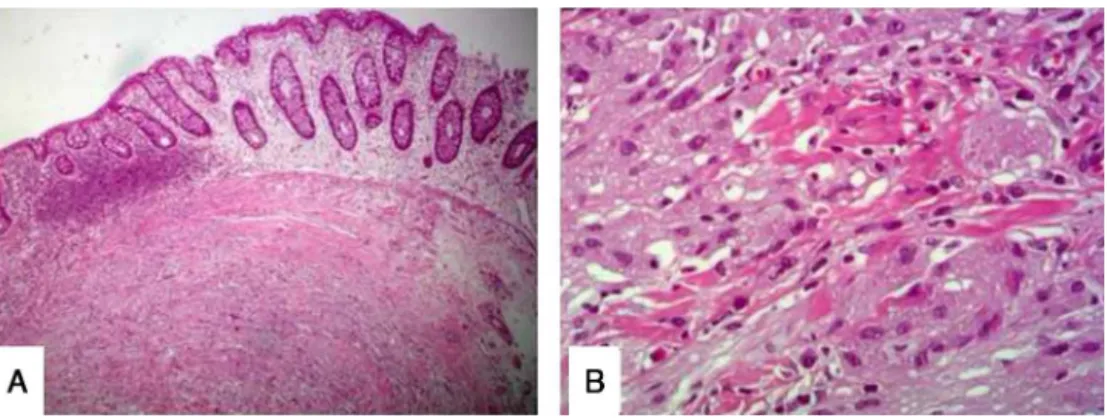
Thecolonoscopy exam revealed two polypsin the rec-tum and sigmoid colon and ayellowish elevated lesion of 0.5cmindiameter,5cmawayfromtheanaledge,whichwas totallyresected.Thepathologyofthe earlylesionsshowed hyperplastic polypsofcolon and rectal mucosa.The latter injury, however, was a polypoid fragment coated byrectal mucosaconsistingofmatureneoplasmcharacterizedbya pro-liferationofcellswithabundantcytoplasm,micro-vacuoles,
eventually granular, and building blocks interspersed with bandsofcollagenfibers,asshowninFig.1.The immunohisto-chemistryrevealedtheexpressionofCD56,S100,CD34inthe normalvascularendothelium,CD68inthenormalhistiocytes andalow(1%)percentageofKi67cellproliferation(Fig.2).
Diagnosis
Throughtheproctologicalexam,internalhemorrhoidswere diagnosed. The upper endoscopy showed mild chronic esophagitis and the colonoscopy revealed a granular cells tumoroftherectalsubmucosa.
Medicalmanagement
Preoperative tests were ordered to perform hemorrhoidec-tomy.Giventhebenignnatureofgranularcelltumorinthis case,itwaschosentomonitorthepatientafterendoscopic resection.
Discussion
Thegranularcelltumorwasdescribedforthefirsttimeinthe oralcavitybyAbrikossof,in1926anditisarareneoplasm, pre-dominantlybenign1.Itcanaffectanyareaofthebody,being morefrequentintheoralcavityandsubcutaneoustissue.3In
thegastrointestinaltract,theorganwiththehighest preva-lence ofthetumoristhe esophagus,followed bythe large intestine4.Theincidenceishigherinfemales(1.5:1),withwide variationintherangeofageinthediagnosis,butwithapeak ofincidencebetweenthefourthandsixthdecadesoflife.2
Thisneoplasmhasamesenchymalorigin,probablyderived fromSchwanncells,ahypothesisthathasbecomestrongdue tothe discoveryofahighimmunohistochemicalaffinityof this tumorforS-100protein,myelinandmyelin-associated glycoprotein.8
The granulosa cells have typically benign pattern, with polygonal or fusiform arranged shape in compact nests separatedbycollagenfibers.4Thesecellshaveabundant
cyto-plasm,eosinophilicwithPAS-positivegranulesandsmalland uniformnuclei.11,12Thehistologicaland
immunohistochem-icaldescriptionsfoundinthecaseareconsistentwiththose foundintheliterature.
The tumorusually presents as a non-ulcerated nodule, painless,withlessthan 3cm, withslowgrowth.5–7 Inmost
of thecases, the tumoris asymptomatic,but the onset of symptoms is more common proportionally to the size or numberoftheneoplasticlesions.4About10%ofthepatients
havemultipletumors.11Therateofrecurrenceaftersurgical
resectionisalsolow:around5–10%.8Thefindingofthisinjury
is usuallymade during the investigation ofother diseases throughthetestssuchasendoscopyandcolonoscopy.8The
tumorusuallypresentsasasessilepolyp,yellow-grayish,with firmconsistency.4,8Thediagnosisismadethroughexcisional
biopsyandpathologicalstudy.
Themalignantpotentialofthetumoranditscriteriaare stillquestionedintheliterature.About2%oftumors gener-atemetastasis.7Yamadaetal.suggestthatthemainfactorfor
126
jcoloproctol(rioj).2015;35(2):124–127Fig.1–(A)Histologicoverviewofthelesion.(B)Detailofthehistology.
Fig.2–Immunohistochemistryofthelesion.(A)ImmunohistochemistryforS100marker.(B)Immunohistochemistryfor CD56marker.
in tumors larger than 4cm in diameter.8,9 Fanburg-Smith
etal.suggesttheuseofhistologicalcriteriasuchascellular necrosis,pleomorphism,increasednuclear-cytoplasmicratio, enlargednucleoli,increasedmitoticactivityandcell elonga-tion.Malignancyissuspectedwhen3ormoreofthesefactors arepresent.10Besidesthose,localrecidivationorrapidgrowth
tumorshouldalsobeconsideredascriteria.4 Noneofthese
featureswerepresentinthelesionfoundinthepatient, sug-gestingbenignity.
Intheabsenceofmalignancycriteria,therecommended treatmentisendoscopic excision,and eventhe trackingof tumorssmallerthan1cmcanbemadewithoutresection.4,13
Incasesofmultipletumors,it isnecessarytomonitorthe patient,duetothehigherriskofmalignity.13Duetothebenign
featuresofthetumorinourpatientwechosetofollowherwith annualcolonoscopies.
Thegranularcelltumorisarareneoplasm,predominantly benignthatcanaffectanypartofthebody,includingthe gas-trointestinaltract.Asmallpercentageoftheselesionshave malignantpotentialandgeneratemetastasis,beingimportant toanalyzethediameterand histologicalfeaturesbeforeits management.Inmajorityofthecases,wecansafelyperform theendoscopicresection.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1.AbrikossoffAL.UberMyome,ausgehendvonder
quergestreifterwillknerilicherMuskulatur.VirchowsArchA PatholAnatHistopathol.1926;260:215–33.
2.SohnD,ChoiH,ChangY,HuhJ,KimD,KimD,etal.Granular celltumorofthecolon:reportofacaseandreviewofthe literature.WorldJGastroenterol.2004;10(16):2452–4.
3.ParfittJR.Granularcelltumoursofthegastrointestinaltract: expressionofnestinandclinicopathologicalevaluationof11 patients.Histopathology.2006;48:424–30.
4.NarraSL,TombazziC,DattaV,IsmailMK.Granularcelltumor oftheesophagus:reportoffivecasesandreviewofthe literature.AmJMedSci.2008;355(5):338–41.
5.BarrosJA,TaniguchiDP,MartinezMAR,FilhoCDSM,MoyaMC, TebcheraniAJ,etal.Tumordecélulasgranulosas(tumorde Abrikossoff)vulvar–Relatodecaso.SurgCosmetDermatol. 2011;3(2):157–9.Availableinhttp://www.surgicalcosmetic. org.br/public/artigo.aspx?id=136#ref2[access03.09.13]. 6.EspinoDC,LagamaAND,LimaMG,SoriaPT,PérezRC,Plaza
DM,etal.Tumordecélulasgranulares;localizaciónatípicaen launiónrecto-sigma.In:VCongresoVirtual
HispanoamericanodeAnatomiaPatologica;2002.Availablein
http://conganat.uninet.edu/autores/trabajos/T110/[access 03.09.13].
7.BolognaJL,JorizzoJL,RapiniRP.Neuralandneuroendocrine neoplasms.In:BolognaJL,JorizzoJL,RapiniRP,editors. Dermatology.Philadelphia:Mosby;2003.p.1843–59.
jcoloproctol(rioj).2015;35(2):124–127
127
Anal:RelatodeCasoeRevisãodeLiteratura.RevBras Coloproct.2006;26(4):454–8.
9. YamadaT,FujiwaraY,SasatomiE,NakanoS,TokunagaO. Granularcelltumoroftheascendingcolon.InternMed. 1995;34(7):657–60.
10.Fanburg-SmithJC.Malignantgranularcelltumorofsoft tissue:diagnosticcriteriaandclinicopathologiccorrelation. AmJSurgPathol.1998;22:779–94.
11.LlanoRC,GaitánMH,BanosFJ,HoyosAV,VélezMHR, RestrepoJIR,etal.Tumordecélulasgranulareseneltracto Gastrointestinal.RevColGastroenterol.2005;21(2): 79–85.
12.ItkinM.TrerotolaSO.SIR2004filmpanelcase:multicentric granularcelltumorwithbiliary,subcutaneous,andbreast involvement.JVascIntervRadiol.2004;15(9):1021–3.
13.MeloAUC,RibeiroCF,MeloGC,Martins-FilhoPRS,Ramalho LMP,AlbuquerqueJúniorRLC.Tumoresdecélulasgranulares nalíngua,relatode2casos.RevPortEstomatolMedDentCir Maxilofac.2012;53:159–64.Availablein