w w w . r b h h . o r g
Revista
Brasileira
de
Hematologia
e
Hemoterapia
Brazilian
Journal
of
Hematology
and
Hemotherapy
Original
article
Nutritional
assessment
as
predictor
of
complications
after
hematopoietic
stem
cell
transplantation
Marcela
Espinoza,
Javiera
Perelli,
Roberto
Olmos,
Pablo
Bertin,
Verónica
Jara,
Pablo
Ramírez
∗SchoolofMedicine,PontificiaUniversidadCatólicadeChile(UC),Santiago,Chile
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received27May2015 Accepted13October2015
Availableonline27November2015
Keywords:
Hematopoieticcelltransplantation Nutrition
Outcomes
a
b
s
t
r
a
c
t
Introduction:Nutritionalsupportispivotalinpatientssubmittedtohematopoieticstemcell transplantation.Nutritionalstatushasbeenassociatedwithtimeofengraftmentand infec-tionrates.Inordertoevaluatetheassociationbetweennutritionalparametersandclinical outcomesaftertransplantationacohortoftransplantpatientswasretrospectively evalu-ated.
Methods:All50 patientstransplantedbetween2011and2014wereincluded.The nutri-tionalstatusbeforetransplantation,tendaysaftertransplantationandbeforedischarge wasassessedincludinganthropometry,bodymassindex,albumin,prealbuminandtotal urinarynitrogen.
Results:Themedianfollow-uptimewas41monthsandthemedianageofpatientswas41 years.Thirty-twounderwentallogeneicand18autologoustransplants.Diagnosesincluded acuteleukemias(n=27),lymphoma(n=7),multiplemyeloma(n=13),andaplasticanemia (n=3).Thirty-sevenpatientsdevelopedmucositis(threeGrade1,15Grade2,18Grade3and oneGrade4),andtwenty-twoallogeneic,andfiveautologoustransplantpatientsrequired totalparenteralnutrition.Albuminandtotalurinarynitrogenwereassociatedwithlengthof hospitalstayandplateletandneutrophilengraftment.Noneofthenutritionalparameters evaluatedwereassociatedwithoverallsurvival.Non-relapsemortalitywas14%andoverall survivalwas79%at41monthsoffollow-up.
Conclusions: Afterhematopoieticstemcelltransplantation,highcatabolismwasassociated withlongerlengthofhospitalstay,theneedoftotalparenteralnutritionandplateletand neutrophilengraftmenttimes.Nutritionalparameterswerenotassociatedwithoverall sur-vival.
©2015Associac¸ãoBrasileiradeHematologia,HemoterapiaeTerapiaCelular.Published byElsevierEditoraLtda.Allrightsreserved.
∗ Correspondingauthorat:DepartamentodeHematologíayOncología,EscueladeMedicina,PontificiaUniversidadCatólicadeChile,
Lira85,Piso4,Santiago,Chile.
E-mailaddress:pramirez@med.puc.cl(P.Ramírez).
http://dx.doi.org/10.1016/j.bjhh.2015.10.002
Introduction
Nutritional support is one of the most important issues in the management of patients who undergo hematopoi-eticstemcelltransplantation(HSCT).1,2Manyfactorsinduce
changes in the metabolism during HSCT3 including
high-dose chemotherapy and total body irradiation, mucositis with painful ulcers, diminished ingestion, nausea, vomi-ting and diarrhea.2 Allogeneic HSCT (allo-HSCT) usually
produces the greatest changes in body composition and muscle metabolism, infections and acute graft-versus-host disease(aGVHD).4,5
Malnutritionhasbeen identifiedasamajorchallenge in HSCT.Furthermoreinmalnourished(underandoverweight) patients,studieshaveshownahigherriskofcomplications: changes in the body composition resulting in electrolyte imbalanceandimpairmentoftheimmunesystem(both asso-ciatedwithlongerengraftmenttime)andmostofall,higher non-relapsemortalityratesintheimmediatepost-transplant period.6–9
Energyrequirementsaftertransplantationusuallyincrease by30–50%,whichiswhynutritionalsupporthasbeen sug-gestedasacontributingfactortoanimprovedengraftment time and lower risk of infection during the neutropenic stage.9–11Parenteralnutritionissupportivecare,which
main-tainsthenutritionalstatusofpatientsduringthetransplant process.
Thereare nowmanynutritional parametersavailablein thenutritionalassessmentsofcancerpatientsandspecifically HSCTpatients.Thispaperpresentstheimpactofpre-HSCT andpost-HSCTbiochemicalandanthropometricevaluations on the clinical outcomes of HSCT. Thus, the aim of this studywastoidentifyanyassociationsbetweenseveral nutri-tionalparametersand theincidenceofgastrointestinaland hepaticaGVHD,infectiouscomplications,lengthofhospital stay,delayedneutrophilorplateletengraftmentandoverall survival(OS).
Methods
Patients
All patients who underwent autologous HSCT(auto-HSCT) andallo-HSCTbetween2011and2014atthePontificia Uni-versidadCatólicadeChilewereincludedinthisstudy.Data werecollectedfromtheelectronicandpaperchartsaswellas theHSCTprogramdatabase.Thestudywasapprovedbythe institutionalreviewboard.
Transplantprocedure
After the decision to transplant had been made, patients underwentanumberofevaluationstodeterminetheir suit-ability for transplantation and, when apt, auto-HSCT or allo-HSCT was performed. Conditioning regimens for the HSCTareshowninTable1.
Insibling and matchedunrelatedHSCT,prophylaxis for graft-versus-hostdisease(GVHD)wasmadewithcyclosporine
Table1–Patientcharacteristics.
Gender–n(%)
Male 33(66)
Female 17(34)
MedianAge–years(range) 41(17–67)
Diagnosis–n(%)
Acuteleukemia 26(52)
Myelodysplasticsyndrome 1(2)
Lymphoma 7(14)
Myeloma 13(26)
Aplasticanemia 3(6)
Averagelengthofstay–days(range) 32(19–109)
Typeoftransplant–n(%)
Autologous 18(36)
Allogeneic 32(64)
Related 20(63)
Unrelated 9(28)
Cord 3(9)
Conditioning–n(%)
Myeloablative 42(84)
Reducedintensity 8(16)
and methotrexate ortacrolimus andmethotrexate. Incord bloodHSCT,GVHDprophylaxiswasmadewithcyclosporine andmycophenolatemofetil.
Prophylaxisagainstinfectiousdiseasesforallthepatients included levofloxacin(500mgq.d.) startingonDay−1until
neutrophilrecoveryorfebrileneutropenia,acyclovir(400mg t.i.d)startingonDay−1untilDay+365,fluconazole(200mg
q.d.)startingonDay−1untilDay+100andsulfamethoxazole
trimethoprim(q.d.3timesaweek)startingwithneutrophil recoveryuntilDay+365. Similarly,allpatientswere keptin isolatedroomswithhighefficiencyparticulateairfiltersand positivepressureduringtheneutropenicphaseofthe trans-plant. Patients were givena neutropenic dietand received intravenous filgrastim300gstarting onDay +5until
neu-trophilengraftment.
Nutritionalevaluation
A nutritional evaluation was conducted at the time of HSCT, ten days after HSCT and before patient discharge. Pre-transplant assessments included body mass index (BMI), anthropometry, and measurements of the albu-min, prealbumin and total urinary nitrogen (TUN) levels. Clinical and laboratory variables including cell counts, hematological condition and conditioning regimens were recorded.
Post-transplantassessmentincludedBMI,albumin, preal-bumin,TUNandtypeofnutritionalsupport[oral,oralplus supplement, enteral nutrition or total parenteral nutrition (TPN)].
Definitions
BMI was calculated according to Hannan.12 BMI<20kg/m2
wasconsidered underweight,between 20–25kg/m2 normal,
25–30kg/m2overweightand>30kg/m2obese.Prealbuminwas
quantifiedusingthenephelometrymethodwithnormal val-uesbetween18and38mg/dL,albuminwasquantifiedusing thecolorimetricmethodwithnormalvaluesbetween3.5and 5.0mg/dL and 24-h TUN was assessed using the Kjeldahl method.PatientswhorequiredTPNwereprescribedfora spe-cificnumberofdays.Mucositis(Grade1to4)andinfectious complications(Grade 1 to5) were graded according tothe NationalHealthInstituteandCommonTerminologyCriteria forAdverseEventsv4.03.13AcuteGVHD(hepaticand
intesti-nal)wasgradedaccordingtotheInternationalBoneMarrow TransplantRegistry(IBMTR)scale.14Timetoneutrophiland
plateletengraftmentwasdefinedaccordingtostandard def-initions:neutrophilcount>500cells/Lforthreeconsecutive
daysandplateletcount>50,000cells/Lforsevenconsecutive
dayswithoutthepatientrequiringtransfusions.
Statisticalanalysis
Statistical analysis was performed using the Statistical PackagefortheSocialSciences(SPSS)software(Version20; Chicago,IL,USA).Resultsarepresentedasmeanvalues.The ANOVAtestwasusedtocomparethreemean valuesofthe evaluationsperformedbeforethetransplant, tendaysafter transplantand atdischarge and the t-testto comparetwo
means(auto-HSCTvs.allo-HSCT).Multivariateanalysisused theSpearmancoefficient.BMI,dynamometry,albumin, pre-albumin,TUN,triglycerides,timetoplateletandneutrophil engraftment,lengthofhospitalstayandOSwereconsidered continuousvariablesandtheneedofTPN,aGVHDand pres-enceofmucositis,categoricalvariables.TheCoxProportional Hazards test was used toestimate the OS.15 OS and
non-relapsemortalitywereanalyzedbytheKaplan–Meiermethod. Statisticalsignificancewassetforp-values<0.05.
Results
Characteristicsofpatientsandthehematopoieticstemcell transplantationprocedure
Fifty patients transplanted between 2011 and 2014 were analyzed.PatientcharacteristicsareshowninTable1. Thirty-three(66%)weremenandseventeen(34%)werewomen.The averageagewas41years(range:17–67years).Inall,32 allo-HSCTand18auto-HSCTwereperformed.IndicationsforHSCT wereacuteleukemiasin26patients(52%),multiplemyeloma in13 (26%),lymphomainseven(14%),severe aplastic ane-miainthree(6%)andmyelodysplasticsyndromeinone(2%). Theaveragelengthofhospitalstaywas32days(range:19–109 days).
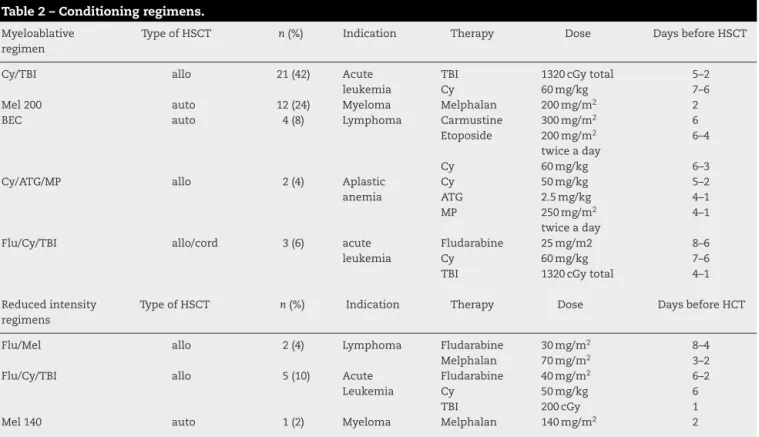
Conditioningregimens(Table2)weremyeloablativein42 cases(84%)andreducedintensityineightcases(16%).The medianfollow-uptimewas41months(range:2–83years).
Table2–Conditioningregimens.
Myeloablative regimen
TypeofHSCT n(%) Indication Therapy Dose DaysbeforeHSCT
Cy/TBI allo 21(42) Acute
leukemia
TBI Cy
1320cGytotal 60mg/kg
5–2 7–6
Mel200 auto 12(24) Myeloma Melphalan 200mg/m2 2
BEC auto 4(8) Lymphoma Carmustine
Etoposide
Cy
300mg/m2 200mg/m2 twiceaday 60mg/kg
6 6–4
6–3
Cy/ATG/MP allo 2(4) Aplastic
anemia
Cy ATG MP
50mg/kg 2.5mg/kg 250mg/m2 twiceaday
5–2 4–1 4–1
Flu/Cy/TBI allo/cord 3(6) acute
leukemia
Fludarabine Cy TBI
25mg/m2 60mg/kg 1320cGytotal
8–6 7–6 4–1
Reducedintensity regimens
TypeofHSCT n(%) Indication Therapy Dose DaysbeforeHCT
Flu/Mel allo 2(4) Lymphoma Fludarabine
Melphalan
30mg/m2 70mg/m2
8–4 3–2
Flu/Cy/TBI allo 5(10) Acute
Leukemia
Fludarabine Cy TBI
40mg/m2 50mg/kg 200cGy
6–2 6 1
Mel140 auto 1(2) Myeloma Melphalan 140mg/m2 2
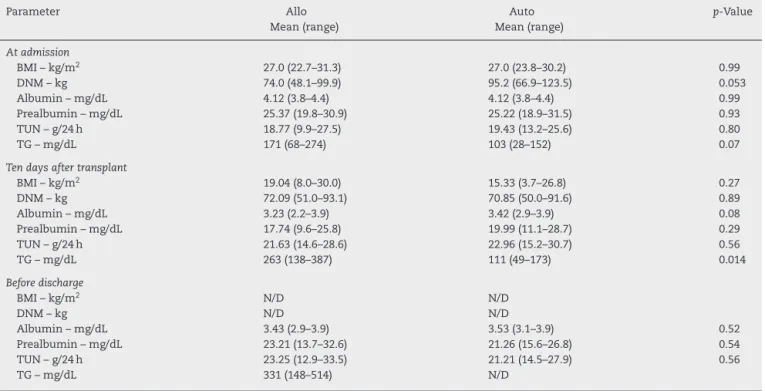
Table3–Nutritionalassessmentcomparingallogeneicandautologoushematopoieticstemcelltransplantationat
differenttimepoints.
Parameter Allo
Mean(range)
Auto Mean(range)
p-Value
Atadmission
BMI–kg/m2 27.0(22.7–31.3) 27.0(23.8–30.2) 0.99
DNM–kg 74.0(48.1–99.9) 95.2(66.9–123.5) 0.053
Albumin–mg/dL 4.12(3.8–4.4) 4.12(3.8–4.4) 0.99
Prealbumin–mg/dL 25.37(19.8–30.9) 25.22(18.9–31.5) 0.93
TUN–g/24h 18.77(9.9–27.5) 19.43(13.2–25.6) 0.80
TG–mg/dL 171(68–274) 103(28–152) 0.07
Tendaysaftertransplant
BMI–kg/m2 19.04(8.0–30.0) 15.33(3.7–26.8) 0.27
DNM–kg 72.09(51.0–93.1) 70.85(50.0–91.6) 0.89
Albumin–mg/dL 3.23(2.2–3.9) 3.42(2.9–3.9) 0.08
Prealbumin–mg/dL 17.74(9.6–25.8) 19.99(11.1–28.7) 0.29
TUN–g/24h 21.63(14.6–28.6) 22.96(15.2–30.7) 0.56
TG–mg/dL 263(138–387) 111(49–173) 0.014
Beforedischarge
BMI–kg/m2 N/D N/D
DNM–kg N/D N/D
Albumin–mg/dL 3.43(2.9–3.9) 3.53(3.1–3.9) 0.52
Prealbumin–mg/dL 23.21(13.7–32.6) 21.26(15.6–26.8) 0.54
TUN–g/24h 23.25(12.9–33.5) 21.21(14.5–27.9) 0.56
TG–mg/dL 331(148–514) N/D
Allo:allogeneic;Auto:autologous;BMI:bodymassindex;DNM:dynamometry;TUN:totalUrinaryNitrogen;TG:triglycerides;N/D:nodata available.
Nutritionalstatusbeforeandafterhematopoieticstemcell transplantation
AtadmissionforHSCT,therewerenosignificantdifferences regardingnutritionalparametersbetweenthegroupsof allo-HSCTandauto-HSCTpatients(Table3).Aftertransplantation onlythetriglycerides levelsweresignificantlyhigherinthe allo-HSCTGroupcomparedtoauto-HSCTGroup.Theother parametersweresimilarbetweenbothgroups(Table3).
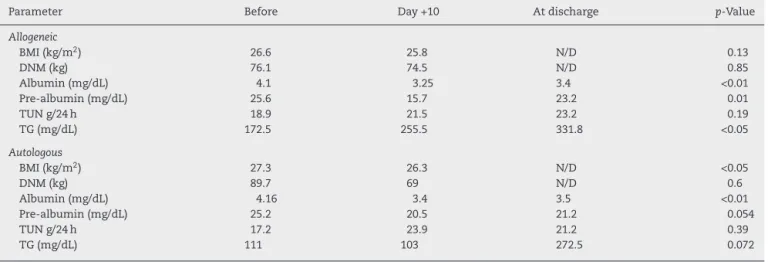
On combining the HSCT groups, there were significant reductionsinthe BMI,and prealbumin and albuminlevels inthepost-transplantperiodcomparedtothepre-transplant period. Triglyceride levels were significantly higher in the post-transplant assessment. No differences in TUN and dynamometry were found between the three evaluations (Table4).
Consideringthetype ofHSCT,albumin levelsdecreased significantly inboth the allo-HSCT and auto-HSCT Groups aftertransplantation.However,thereductioninprealbumin,
aswellastheincreaseintriglyceridelevels,wereonly signif-icantintheallo-HSCTgroup,whileasignificantdropinBMI wasonlyseenintheauto-HSCTgroup(Table5).
Post-transplantcomplications
Consideringallpatients,37(74%)developedmucositis [allo-HSCT:n=24(75%)andauto-HSCT:n=13(72%);p-value<0.05]. AccordingtothedegreeofmucositisthreepatientshadGrade 1,15patientsGrade2,18patientsGrade3andonehadGrade4 (Figure1).Ofthe37patientswithmucositis,27(73%)required TPN[allo-HSCT:n=22(81%)andauto-HSCT:n=5(19%)]and 10 (27%)someother kindofnutritional support.According tothetypeoftransplant,28%(5/18)ofauto-HSCTand 69% (22/32)of allo-HSCTpatients requiredTPN. Figure 2shows thedistributionofnutritionalsupportinthedifferentgroups. EightpatientswithoutmucositisalsorequiredTPNbecauseof severenauseaandvomiting.
Table4–Nutritionalassessmentbeforetransplant,10daysaftertransplantandatdischarge.
Parameter Beforetransplant
Mean(range)
Day+10 Mean(range)
Beforedischarge Mean(range)
p-Value
BMI(kg/m2) 26.9(20.9–34.6) 26.1(20.0–34.7) N/D <0.01
DNM(kg) 79.7(24.3–142.0) 72.5(33.0–109.0) N/D 0.9
Albumin(mg/dL) 4.1(3.5–4.9) 3.3(2.2–4.0) 3.5(2.0–4.4) <0.01
Pre-albumin(mg/dL) 25.4(14.6–35.5) 18(7.2–34.5) 21.9(10.9–50.4) <0.01
TUNg/24h 18.2(4.0–44.6) 22.1(9.9–41.4) 22.6(9.0–50.0) 0.1
TG(mg/dL) 148.7(40–465) 235(46–557) 324.8(96–863) <0.01
Table5–Nutritionalassessmentbeforeandafterhematopoieticstemcelltransplantationaccordingtothetypeof transplantation.
Parameter Before Day+10 Atdischarge p-Value
Allogeneic
BMI(kg/m2) 26.6 25.8 N/D 0.13
DNM(kg) 76.1 74.5 N/D 0.85
Albumin(mg/dL) 4.1 3.25 3.4 <0.01
Pre-albumin(mg/dL) 25.6 15.7 23.2 0.01
TUNg/24h 18.9 21.5 23.2 0.19
TG(mg/dL) 172.5 255.5 331.8 <0.05
Autologous
BMI(kg/m2) 27.3 26.3 N/D <0.05
DNM(kg) 89.7 69 N/D 0.6
Albumin(mg/dL) 4.16 3.4 3.5 <0.01
Pre-albumin(mg/dL) 25.2 20.5 21.2 0.054
TUNg/24h 17.2 23.9 21.2 0.39
TG(mg/dL) 111 103 272.5 0.072
Resultsshownasmeans.
BMI:bodymassindex;DNM:dynamometry85%standardforageandgender;TUN:totalurinarynitrogen;TG:triglycerides;N/D:nodata available.
Consideringthe32 allo-HSCTpatients, nine(28%) devel-opedintestinalaGVHD(fivepatientssubmittedtounrelated HSCTandfourtorelatedHSCT)and23(72%)didnotdevelop intestinalaGVHD.TheseveritywasGradeII-IV infive(56%) andGradeIII-IVinfour(44%).TheaveragetimefromHSCTto aGVHDwas34days(range:16–80days).Overall,69%(22/32)of theallo-HSCTpatientsrequiredTPN.Allofthepatientswho developedintestinalaGVHDrequiredTPNand57%(13/23)of thepatientswithoutintestinalGVHDrequiredTPN,mainly duetoanorexia.
The41-monthOS was 79% (auto-HSCT: 81%;allo-HSCT: 75%;p-value=NS).The non-relapse mortality rate (2 auto-HSCTand4allo-HSCT)was12%at41months(11%auto-HSCT and13%allo-HSCT;p-value=NS).
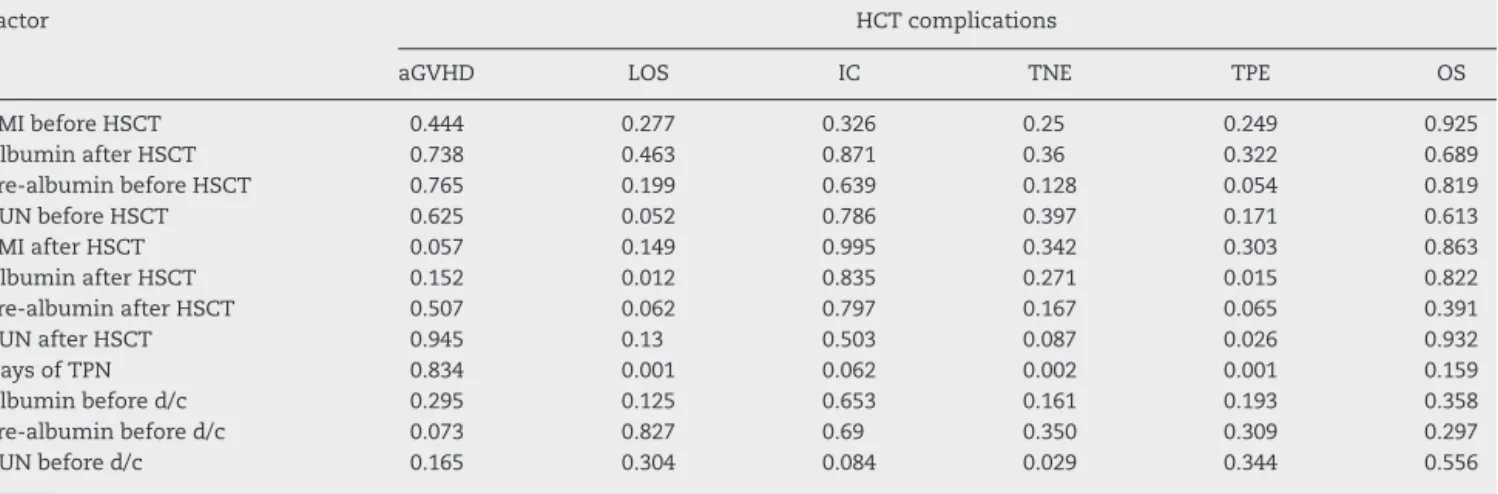
Multivariateanalysis
In the multivariate analysis, none of the pre-HSCT nutri-tionalparameterswasassociatedwithtransplantoutcomes.
20
15
Number of patients
10
5
0
0 1 2
Severity of mucositis (grade)
3 4
Auto n=18
Allo n=32
Figure1–Distributionofmucositisaccordingtogradeand typeofhematopoieticstemcelltransplantation.
auto:autologoushematopoieticstemcelltransplantation; allo:allogeneichematopoieticstemcelltransplantation.
However,severalpost-HSCTnutritionalparameterswere sta-tistically associated with transplant outcomes. Specifically, tendaysaftertransplant,albuminwasassociatedwithlength ofhospitalstayandtimetoplateletengraftment;TUNwas correlatedwithtimetoplateletengraftmentanddaysofTPN withlengthofhospitalstay,timetoneutrophilengraftment andtimetoplateletengraftment.OnlyTUNwasassociated withtimetoneutrophilengraftmentinthepre-discharge eval-uation. Finally, OSwas not affected byany variable in the multivariateanalysis(Table6).
Discussion
This is the first study from Chile to report on nutritional supportinHSCTpatients. Nutritionalimpairmentis signif-icant after transplantation16 and is associated with worse
outcomes.17 Malnourishment increases the risk of death,
25
20
15
Number of patients
10
5
0
Oral Oral+NS
Type of nutritional support
TPN EN Auto n=18
Allo n=32
Figure2–Typeofnutritionalsupportrequired.
Table6–Significance(p-values)bymultivariateanalysisoffactorspotentiallyassociatedwithcomplicationsof
hematopoieticstemcelltransplantation.
Factor HCTcomplications
aGVHD LOS IC TNE TPE OS
BMIbeforeHSCT 0.444 0.277 0.326 0.25 0.249 0.925
AlbuminafterHSCT 0.738 0.463 0.871 0.36 0.322 0.689
Pre-albuminbeforeHSCT 0.765 0.199 0.639 0.128 0.054 0.819
TUNbeforeHSCT 0.625 0.052 0.786 0.397 0.171 0.613
BMIafterHSCT 0.057 0.149 0.995 0.342 0.303 0.863
AlbuminafterHSCT 0.152 0.012 0.835 0.271 0.015 0.822
Pre-albuminafterHSCT 0.507 0.062 0.797 0.167 0.065 0.391
TUNafterHSCT 0.945 0.13 0.503 0.087 0.026 0.932
DaysofTPN 0.834 0.001 0.062 0.002 0.001 0.159
Albuminbefored/c 0.295 0.125 0.653 0.161 0.193 0.358
Pre-albuminbefored/c 0.073 0.827 0.69 0.350 0.309 0.297
TUNbefored/c 0.165 0.304 0.084 0.029 0.344 0.556
aGVHD:acutegraftversushostdisease;LOS:lengthofhospitalstay;IC:infectiouscomplications;TNE:timetoneutrophilengraftment;TPE: timetoplateletengraftment;OS:overallsurvival;HSCT:hematopoieticstemcelltransplantation;BMI:bodyMassIndex;TUN:totalurinary nitrogen;TPN:totalparenteralnutrition;d/c:discharge.
mucositis, aGVHDand infectious complicationsinpatients submittedtoHSCT.9,17,18
Several studies have addressed the topic of specific nutritional parameters in HSCT, with discordant findings. Schulteetal.,withoutdemonstratinganyassociationbetween BMI and transplant complications, reported a significant decrease inBMI afterHSCT,which revertedone year after transplantation.10 Other authors have identified low
pre-transplantBMIasanindependentriskfactorformortality.19–22
Urbainetal.showedthataGVHDandanorexiaduring trans-plantwereassociatedwithsignificantreductionsinBMIin anallo-HSCTcohort.9ThisstudyfoundanoveralldropinBMI
afterHSCT,withstatisticalsignificanceonlyfortheauto-HSCT Group.
Whenconsideringotherparameters,thestudyofSchulte et al. showed a significant reduction in prealbumin levels atDay +14 and+28 afterHSCT.10 Inthe currentstudy,this
reductionwasnoticedevenbefore,atDay+10,andpersisted untilpatientdischarge.Albuminlevelsshowedasignificant reductioninthesameperiodirrespectiveofthetypeofHSCT, whichcorrelatedwithbothalongerlengthofhospitalstayand plateletengraftmenttime.
Thedifferencesfoundbetweenallo-HSCTandauto-HSCT maysuggestahigherdegreeofcatabolismintheallo-HSCT setting.Specifically, this study observedthat earlier inthe courseofHSCT,theTUNlevelstendtobehigherafter auto-HSCTcomparedtoallo-HSCT.However,beforedischargeTUN washigher,albeitnotsignificantly, intheallo-HSCTGroup than the auto-HSCT Group. Moreover, albumin levels can changeinacuterenalfailureandduringtheuseoftransfusion support,whichisverycommoninthiskindofpatient.23,24A
studyofUnderzoetal.25showedthatafterTPN,albuminlevels
afterHSCTdidnotchangeoveroneweekbutprealbumin lev-elsdid,whichmakesthisvariableamoreaccurateparameter fordietandnutritionalassessments.Togetherwith prealbu-min,researchhasshowndecreasesofotherparametersafter HSCT suchas transferrin and retinol binding proteinthat mightpredictmalnutritioninallo-HSCTandauto-HSCT.26In
this study, higher TUNlevels were associated with slower neutrophilandplatelet engraftment.Thismaysuggestthat higherTUNlevelsareasurrogateofmoresevereinfectious complications,whichcouldbeassociatedtodelayed engraft-menttime.Researchfailedtoshowanassociationbetween nutritionalsupportandtimetoneutrophilengraftment.27,28
However,astudybyHabjibabaieetal.suggestedthatBMI,but notTUN,wasinverselycorrelatedwiththeneutrophil engraft-menttime.29
WhenconsideringcomplicationsafterHSCT,theincidence ofmucositisreportedinthis studywas 74%,similar tothe incidenceof70%reportedintheliterature.30DaysofTPN
cor-relatedwiththelengthofhospitalstayandtimetoplatelet andneutrophilengraftment.
Noneofthenutritionalfactorsanalyzedatdifferenttime points including BMI, albumin, prealbumin,TUN and TPN, wereassociatedwithOSinthisstudy,andsurvivalrateswere similarbetweenallo-HSCTandauto-HSCTpatients,possibly duetotheearlynutritionalsupportprovidedtoallpatients andthesmallnumberofpatientsanalyzedwhichprecluded statisticallysignificantdifferences.Thehighmortalityratein auto-HSCTpatientsispossiblyassociatedwiththelow num-berofthistypeofpatientsincludedinthisstudy.
Thisresearchwasunabletodemonstrateanyassociation betweenTPNandahigherrateofintestinalaGVHD.However, therearepossibleexplanationsfortheassociationbetween mucositis,aGVHDandTPNthathavebeensuggestedbefore. Mucosa-associated lymphoid tissue(MALT),whilenormally actingasanimmunologicalbarrier,maysufferseveredamage duringconditioningforHSCT.Thesubsequentbacterialand toxin translocationmayactasapotentinflammatory stim-ulusforthedevelopmentofacuteaGVHD.31,32Asshownby
Mattssonetal.,theoralfeedingrouteseemstohavea protec-tiveroleagainstthedevelopmentofGVHD.33Intheirstudyof
withoralintake,there wasa cumulativeincidenceofonly 7%ofaGVHD.Inthe currentstudy,allofthepatients with gastrointestinalaGVHDrequiredTPN and less thanhalf of thepatientswithoutintestinalaGVHDrequiredTPN,mainly foranorexia.However,duetothesmallnumberofpatients with aGVHDno conclusions can be reachedregarding the associationbetweenaGVHDandnutritionalsupport.TPNhas beenassociatedwithintestinalatrophyandenhanced expres-sionofinterferongamma,whilelocallevelsofcytokinesthat protectfromGVHD, suchasIL-4and IL-10,usuallyshow a significantdecreaseinpatientsusingthistypeofnutritional support.34Furthermore,manystudiesincriticalpatientshave
consistentlyshownahigherincidenceofinfectious compli-cationsinTPNversus oral/enteralnutrition, whichmay be anotherpossiblelinkbetweenthefeedingrouteand compli-cationssuchasmucositisandaGVHD.35
Inthe current series, the majority of patientsrequiring nutritionalsupportreceivedTPN.Controversyexistsonthe bestnutritionalsupportaftertransplantation.Astudyby Szel-uga et al.36 showed that compared to oral nutrition, TPN
wasnotassociatedwithOSor hematopoieticrecoveryand lengthofhospitalizationbutwasassociatedwithalongeruse ofdiuretics,morehyperglycemiaandmorecatheter-related complications. Recent studies have suggested that early enteral support could be associated with better outcomes compared to TPN, including faster engraftment times.37,38
However up to90% of the patients undergoing myeloabla-tiveallo-HSCTwillstillreceiveTPN.39Inthecurrentseries,
one-thirdoftheauto-HSCTandtwothirdsoftheallo-HSCT receivedTPN.
Themainlimitationofthisstudyisitsretrospectivenature, whichprecludesthe investigationofcausativeassociations betweenvariablesandoutcomes.However,thisstudy identi-fiessomevariablesthatshouldbeconsideredtopredictthe evolutionofpatientsduringtheacutephasesofHSCT,andto developmoreprecisewaystoassessnutritionalstatus.
Conclusions
This study shows that allo-HSCT and auto-HSCT patients becomesignificantlyhypercatabolicduringtheacutephase oftransplantsandthemajoritywilldevelopmucositis requir-ingnutritionalsupportearlyinthecourseofthetransplant process.Ofallthevariablesanalyzed,albuminandTUNwere associatedwithclinicaloutcomes.OSwasnotassociatedwith anynutritionalparameter.
Sincethisisnotacomparativestudy,wecannotpredictthe outcomeofpatientswithoutappropriatenutritionalsupport. Howeverduetothefrequencyandseverityofmucositisand thedegreeofcatabolismitseemsreasonabletodeliver appro-priatenutritional supportalthough the best source isstill understudy,withstudies suggestingadvantagesofenteral nutritionoverTPN.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgments
Theauthorsgratefullyacknowledgethehelpprovidedbythe nursesandhematologyfellowsparticipatinginthecareofour patients.
r
e
f
e
r
e
n
c
e
s
1.MousaviM,HayatshahiA,SarayaniA,HadjibabaieM,Javadi M,TorkamandiH,etal.Impactofclinicalpharmacist-based parenteralnutritionserviceforbonemarrowtransplantation patients:arandomizedclinicaltrial.SupportCareCancer. 2013;21(12):3441–8.
2.RzepeckiP,BarzalJ,OborskaS.Bloodandmarrow transplantationandnutritionalsupport.SupportCare Cancer.2010;18Suppl.2:S57–65.
3.ThompsonJL,DuffyJ.Nutritionsupportchallengesin hematopoieticstemcelltransplantpatients.NutrClinPract. 2008;23(5):533–46.
4.HicksonRC,MaroneJR.Exerciseandinhibitionof
glucocorticoid-inducedmuscleatrophy.ExercSportSciRev. 1993;21:135–67.
5.LaPierTK.Glucocorticoid-inducedmuscleatrophy.Theroleof exerciseintreatmentandprevention.JCardiopulmRehabil. 1997;17(2):76–84.
6.FaghihiT,IravaniM,ShamshiriAR,HadjibabaieM,Mousavi SA,AlimoghaddamK,etal.Serumelectrolytechangesat engraftmenttimeinpatientsundergoing
allogeneichematopoieticstemcelltransplantation.Ann Transplant.2009;14(3):51–7.
7.HackerED,FerransCE.Qualityoflifeimmediatelyafter peripheralbloodstemcelltransplantation.CancerNurs. 2003;26(4):312–22.
8.McDiarmidS.Nutritionalsupportofthepatientreceiving high-dosetherapywithhematopoieticstemcellsupport.Can OncolNursJ.2002;12(Spring(2)):102–15.
9.UrbainP,BirlingerJ,LambertC,FinkeJ,BertzH,BiesalskiHK. Longitudinalfollow-upofnutritionalstatusandits
influencingfactorsinadultsundergoingallogeneic
hematopoieticcelltransplantation.BoneMarrowTransplant. 2013;48(3):446–51.
10.SchulteC,ReinhardtW,BeelenD,MannK,SchaeferU.Low T3-syndromeandnutritionalstatusasprognosticfactorsin patientsundergoingbonemarrowtransplantation.Bone MarrowTransplant.1998;22(12):1171–8.
11.LipkinAC,LenssenP,DicksonBJ.Nutritionissuesin
hematopoieticstemcelltransplantation:stateoftheart.Nutr ClinPract.2005;20(August(4)):423–39.
12.HannanWJ,WrateRM,CowenSJ,FreemanCP.Bodymass indexasanestimateofbodyfat.IntJEatDisord. 1995;18(1):91–7.
13.BrunerDW,HanischLJ,ReeveBB,TrottiAM,SchragD,SitL, etal.StakeholderperspectivesonimplementingtheNational CancerInstitute’spatient-reportedoutcomesversionofthe CommonTerminologyCriteriaforAdverseEvents
(PRO-CTCAE).TranslBehavMed.2011;1(1):110–22.
14.RowlingsPA,PrzepiorkaD,KleinJP,GaleRP,PasswegJR, Henslee-DowneyPJ,etal.IBMTRSeverityIndexforgrading acutegraft-versus-hostdisease:retrospectivecomparison withGlucksberggrade.BrJHaematol.1997;97(4):855–64.
15.CoxC.Multinomialregressionmodelsbasedoncontinuation ratios.StatMed.1988;7(3):435–41.
17.ArendsJ,ZuercherG,DossettA,FietkauR,HugM,SchmidI, etal.Non-surgicaloncology–GuidelinesonParenteral Nutrition,Chapter19.GerMedSci.2009;7:Doc09.
18.RodgersC,WalshT.Nutritionalissuesinadolescentsafter bonemarrowtransplant:aliteraturereview.JPediatrOncol Nurs.2008;25(5):254–64.
19.FlemingDR,RayensMK,GarrisonJ.Impactofobesityon allogeneicstemcelltransplantpatients:amatched case–controlledstudy.AmJMed.1997;102(3):265–8.
20.LeBlancK,RingdenO,RembergerM.Alowbodymassindex iscorrelatedwithpoorsurvivalafterallogeneicstemcell transplantation.Haematologica.2003;88(9):1044–52.
21.LenssenP,SherryME,CheneyCL,NimsJW,SullivanKM,Stern JM,etal.Prevalenceofnutrition-relatedproblemsamong long-termsurvivorsofallogeneicmarrowtransplantation. JAmDietAssoc.1990;90(6):835–42.
22.NikolousisE,NagraS,PaneeshaS,DelgadoJ,HolderK,Bratby L,etal.Allogeneictransplantoutcomesarenotaffectedby bodymassindex(BMI)inpatientswithhaematological malignancies.AnnHematol.2010;89(11):1141–5.
23.BernsteinLH,Leukhardt-FairfieldCJ,PlebanW,RudolphR. Usefulnessofdataonalbuminandprealbumin
concentrationsindeterminingeffectivenessofnutritional support.ClinChem.1989;35(2):271–4.
24.NitenbergG,RaynardB.Nutritionalsupportofthecancer patient:issuesanddilemmas.CritRevOncolHematol. 2000;34(3):137–68.
25.UderzoC,RovelliA,BonomiM,FomiaL,PirovanoL,MaseraG. Totalparenteralnutritionandnutritionalassessmentand leukaemicchildrenundergoingbonemarrowtransplantation. EurJCancer.1991;27(6):758–62.
26.RzepeckiP,BarzalJ,SarosiekT,SzczylikC.Biochemical indicesfortheassessmentofnutritionalstatusduring hematopoieticstemcelltransplantation:aretheyworth using?Asinglecenterexperience.BoneMarrowTransplant. 2007;40(6):567–72.
27.FerreiraEE,GuerraDC,BaluzK,deResendeFurtadoW,da SilvaBouzasLF.Nutritionalstatusofpatientssubmittedto transplantationofallogeneichematopoieticstemcells:a retrospectivestudy.RevBrasHematolHemoter. 2014;36(6):414–9.
28.SommacalHM,GazalCH,JochimsAM,BeghettoM,PazA, SillaLM,etal.Clinicalimpactofsystematicnutritionalcare inadultssubmittedtoallogeneichematopoieticstemcell transplantation.RevBrasHematolHemoter.2012;34(5):334–8.
29.HadjibabaieM,IravaniM,TaghizadehM,Ataie-JafariA, ShamshiriAR,MousaviSA,etal.Evaluationofnutritional statusinpatientsundergoinghematopoieticSCT.Bone MarrowTransplant.2008;42(7):469–73.
30.GabrielDA,SheaT,OlajidaO,SerodyJS,ComeauT.Theeffect oforalmucositisonmorbidityandmortalityinbonemarrow transplant.SeminOncol.2003;306Suppl.18:76–83.
31.HillGR,FerraraJL.Theprimacyofthegastrointestinaltractas atargetorganofacutegraft-versus-hostdisease:rationalefor theuseofcytokineshieldsinallogeneicbonemarrow transplantation.Blood.2000;95(9):2754–9.
32.HorsleyP,BauerJ,GallagherB.Poornutritionalstatuspriorto peripheralbloodstemcelltransplantationisassociatedwith increasedlengthofhospitalstay.BoneMarrowTransplant. 2005;35(11):1113–6.
33.MattssonJ,WestinS,EdlundS,RembergerM.Poororal nutritionafterallogeneicstemcelltransplantationcorrelates significantlywithseveregraft-versus-hostdisease.Bone MarrowTransplant.2006;38(9):629–33.
34.SigaletDL,MackenzieSL,HameedSM.Enteralnutritionand mucosalimmunity:implicationsforfeedingstrategiesin surgeryandtrauma.CanJSurg.2004;47(2):109–16.
35.GramlichL,KichianK,PinillaJ,RodychNJ,DhaliwalR, HeylandDK.Doesenteralnutritioncomparedtoparenteral nutritionresultinbetteroutcomesincriticallyilladult patients?Asystematicreviewoftheliterature.Nutrition. 2004;20(10):843–8.
36.SzelugaDJ,StuartRK,BrookmeyerR,UtermohlenV,Santos GW.Nutritionalsupportofbonemarrowtransplant
recipients:aprospective,randomizedclinicaltrialcomparing totalparenteralnutritiontoanenteralfeedingprogram. CancerRes.1987;47(12):3309–16.
37.SeguyD,DuhamelA,RejebMB,GomezE,BuhlND,BrunoB, etal.Betteroutcomeofpatientsundergoingenteraltube feedingaftermyeloablativeconditioningforallogeneicstem celltransplantation.Transplantation.2012;94(3):
287–94.
38.GuièzeR,LemalR,CabrespineA,HermetE,TournilhacO, CombalC,etal.Enteralversusparenteralnutritionalsupport inallogeneichaematopoieticstem-celltransplantation.Clin Nutr.2014;33(3):533–8.