154
Case R eport
REVISTA PAULISTA DE MEDICIN AVanishing Bile Duct Syndrome in
Hodgkin’s Dise ase : case re port
Department of Internal Medicine and Hematology and Blood Transfusion Center,
Universidade Estadual de Campinas, Campinas, Brazil
a b s t r a c t
CO N TEX T: Liver damag e is relatively co mmo n in patients affected by Ho dg kin’s disease. A smaller pro po rtio n o f cases develo ps jaun-dice. Recently, the vanishing bile duct syndro me was described in Ho dg kin’s disease. The mechanisms o f this severe co mplicatio n have been po o rly understo o d until no w.
O BJECTIV E: To describe a rare case o f intra-hepatic cho lestasis due to vanishing bile duct syndro me.
DESIGN : Case repo rt.
CASE REPO RT: A 3 8 -year-o ld male patient affected by Ho dg kin’s disease. Liver bio psy sho wed no detectable Ho dg kin’s disease. In-tra-hepatic cho lestasis was fo und and no ne o f the six po rtal tracts analyz ed co ntained no rmal bile ducts. The treatment was based o n co nventio nal and hig h-do se escalatio n chemo therapy. The patient died fro m an irreversible liver failure while in co mplete remissio n fro m Ho dg kin’s disease.
KEY W O RDS: Ho dg kin’s disease. Vanishing bile duct syndro me. Liver failure.
• Marta So ares Ro ssini • Irene Lo rand-Metz e • G islaine Bo rba O liveira • Cármino Anto nio De So uz a
INTRODUCTION
Liver damage is relatively co mmo n in patients affected by Ho dgkin’s disease. No n-specific inflamma-tio n in po rtal areas is seen in appro ximately 50% o f liver bio psies, but Reed-Sternberg cells can be dem-o nstrated in abdem-o ut 5% dem-o f them.1 Ho wever, a smaller
pro po rtio n o f cases develo p jaundice.2 Other causes
o f cho lestasis in Ho dgkin’s disease include b iliary o bstructio n (by lymph no de enlargement), hemo lysis, viral hepatitis and drug to xicity. In the past, many cases that presented no detectable cause o f jaundice were called “idio pathic jaundice”. Recently, the vanishing bile duct syndro me2,3 was described in Ho dgkin’s
dis-ease. The mechanisms o f this severe co mplicatio n have been po o rly understo o d until no w.2
Ho wever, this syndro me has been described in many o ther diseases such as primary biliary cirrho sis, graft-versus-ho st-dis-ease o r primary sclero sing cho langitis.4,5 Vanishing bile
duct syndro me is also a majo r histo lo gical finding in rejectio n after liver transplantatio n.2,4
Advanced van-ishing bile duct syndro me is pro bably a manifestatio n o f irreversible liver damage.2-6 We describe a case o f
Ho dgkin’s disease asso ciated with vanishing bile duct syndro me.
CASE REPORT
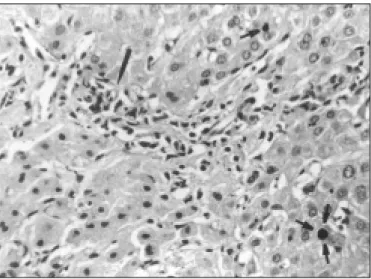
A 38-year o ld male was seen at the General Ho spital o f the State University o f Campinas, Brazil, in Decemb er 1997. He presented a fo ur-week histo ry o f cervical lymphadeno pathy, jaundice and pruritus. The lymph no de histo lo gy sho wed typical Ho dgkin’s
155
dise ase , with mixe d ce llularity (Figure 1). The ab -d o m in a l c o m p u te -d to m o g ra p h y re ve a le -d o n ly hepato megaly. The X-ray o f the tho rax and b ilateral b o ne marro w b io psies were no rmal. Hb = 15.6 g/dl; WBC = 7.6 x 109/L; Platelets 392 x 10 9/L. At the time
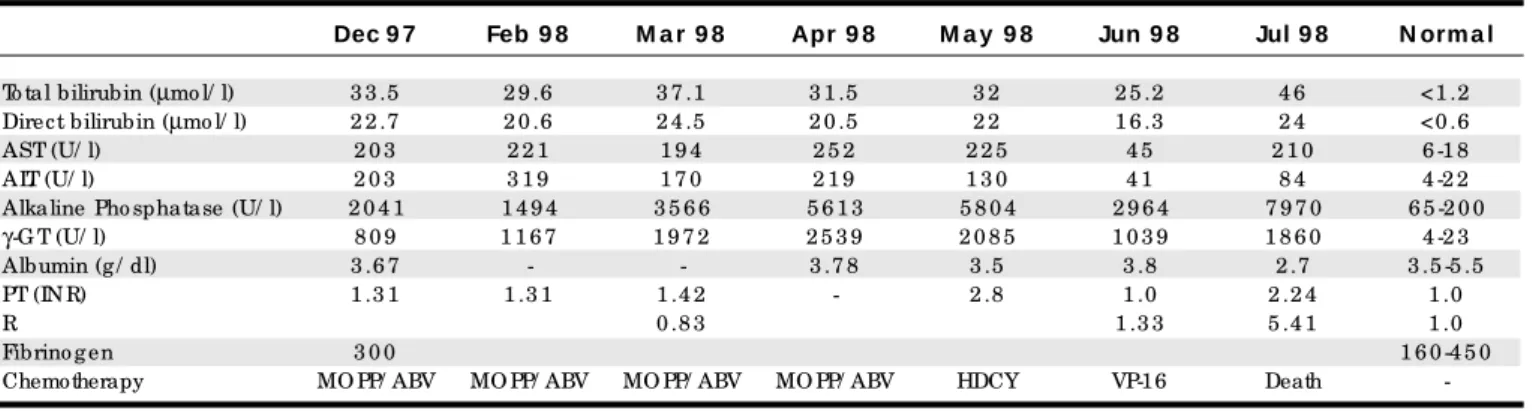
o f ad m is s io n the b io c he m ic al value s ind ic ate d cho lestasis witho ut signs o f hepatic failure (Tab le) Sero lo gical tests fo r hepatitis A, B and C, HIV and cyto megalo virus were negative. Needle b io psy o f the liver (Figure 2) sho wed intra-hepatic cho lestasis. In-terlo b ular b ile ducts were ab sent in all o f the six po r-tal tracts examined. Invo lvement b y Ho dgkin’s dis-ease co uld no t b e detected. The patient was treated with standard chemo therapy (fo ur cycles o f MOPP-ABV7). Cho lestasis pro gressively increased with signs
o f hepatic failure (decrease o f serum alb umin level and e lo ngatio n o f the pro thro m b in tim e ). During chemo therapy, the patient presented enlargement o f a left axillary lymph no de. Then, salvage therapy us-ing high do se Cyclo pho sphamide 7 g/m² (HD-CY) fo l-lo wed b y Eto po side 2 g/m² (VP-16-213) was given to reduce tumo r b urden and to co llect peripheral b lo o d pro genito r cell in o rder to perfo rm auto lo go us b o ne marro w transplantatio n. The lymphadeno pathy dis-appeared and there was a sho rt perio d o f stab iliza-tio n o f hepatic funciliza-tio n and cho lestasis. One mo nth later there was deterio ratio n o f the liver functio n and th e p a tie n t p re s e n te d a n e p is o d e o f m a s s ive hematemesis with dehydratio n and acute renal fail-ure. Altho ugh a liver transplantatio n was co nsidered, the patient died due to hepatic failure.
DISCUSSION
Liver invo lvement is unco mmo n in Ho dgkin’s
disease at diagno sis. Cervantes et al8 fo und 7.4% o f
liver invo lvement in Ho dgkin’s disease in 421 cases studied. Infiltratio n is defined by the presence o f Reed Sternberg cells usually acco mpanied by lympho cytes, histio cytes, eo sino phils and plasma cells in the po r-tal tracts. This infiltratio n o f the live r can le ad to cho lestasis and jaundice. Other causes o f jaundice in Ho dgkin’s disease include extra-hepatic biliary o b-structio n b y enlarged po rtal lymph no des, hemo ly-sis, viral hepatitis and drug to xicity.4 Recently, the
vanishing b ile duct syndro me has b een describ ed as a rare and severe cause o f intra-hepatic cho lestasis in Ho dgkin’s disease.2,3
This syndro me co nsists o f the destructio n o f the b iliary apparatus with the disappearance o f the small and medium-sized intra-hepatic b ile ducts.2,3,5
It has b een o b served in different co ngenital o r ac-q uire d dise ase s such as chro nic re je ctio n o f live r transplantatio n, resulting in graft failure in 5% to 20% o f allo graft recipients; graft-versus-ho st-disease af-ter b o ne marro w transplantatio n; primary b iliary cir-rho sis; primary sclero sing cho langitis; chro nic drug-induce d cho le stasis (clindamycin; carb amaze pine ; trimetho prim-sulphametho xazo le) and histio cyto sis X in children.4-6,9-11
Hub s c he r, e t al.2 d e s c rib e d thre e c as e s o f
Ho dgkin’s dise ase that pre se nte d re ductio n o f b il-iary ducts. The three cases died with intractab le liver damage. The first case, a 26-year-o ld man (Ho dgkin’s dise ase o f the no dular scle ro sing type ), pre se nte d a two -we e k histo ry o f jaundice , fatigue and we ight lo ss. Lab o rato ry studie s sho we d se ve re cho le stasis, a lth o u g h a b d o m in a l u ltra s o u n d e xa m in a tio n sho we d no e vide nce o f b iliary o b structio n. He was tre ate d with che m o the rapy. He die d 24 we e ks late r
Figure 1. Lymph node biopsy specimen from patient showing typical Hodgkin’s Disease, mixed cellularity sub type.
Figure 2. Liver biopsy specimen from the patient. Portal space showing slight mononuclear inflammatory infiltrate. Long arrow shows arteriole without intra-lobular duct. Short arrows show biliary parenchyma plug.
156
with he patic e nce phalo pathy, re nal failure , se ve re diarrhe a and ne utro pe nia. The cause o f the de ath was disseminated fungal infectio n. No residual lym-pho m a was de te cte d in any o f the o rgans e xam ine d at auto psy. The seco nd case, a 44-year-o ld man, pre-se nte d a 2-we e k histo ry o f jaundice . The live r b i-o psy shi-o we d intrahe patic chi-o le stasis i-o f unkni-o wn patho ge ne sis. The diagno sis o f Ho dgkin’s dise ase (lympho cyte predo minant type) was made 7 mo nths late r. At this tim e the jaundice go t wo rse and the live r b io psy sho we d invo lve m e nt b y Ho dgkin’s dis-e asdis-e . Hdis-e b dis-e gan trdis-e atm dis-e nt with rad io thdis-e rap y and che m o the rapy and die d thre e days late r. The third c as e , a 37- ye ar- o ld wo m an p re s e nte d p ruritus , we ight lo ss, pe rsiste nt co ugh and night swe ats. The diagno sis o f Ho dgkin’s dise ase o f the no dular scle -ro sing type was m ade b y tho raco to m y. Te n days af-te r che m o the rapy she de ve lo pe d jaundice . The ul-traso und e xam inatio n was no rm al. Live r functio n de te rio rate d and the patie nt de ve lo pe d re nal and re spirato ry failure and die d. At auto psy no re sidual l ym p h o m a wa s d e te c te d . In th e th re e c a s e s cho le stasis and paucity o f b ile ducts we re no te d in the live r b io psie s. Only case 2 sho we d e vide nce o f lympho mato us infiltratio n. Go ttrand e t al de scrib e d a 3.5yearo ld child with a threeweek histo ry o f sub -maxillary lymphadeno pathy. The lymph no de b io psy sho we d a m ixe d ce llularity Ho dgkin’s dise ase . On ad m issio n she had jaund ic e witho ut he p ato sp le -no m e galy. The b io che m ical value s we re co nsiste nt with cho le stasis. No infiltratio n b y Ho dgkin’s dis-e asdis-e was fo und at thdis-e livdis-e r b io psy. Thdis-e rdis-e was a pau-city o f inte rlo b ular b ile ducts. Cho le stasis pro gre s-sive ly incre ase d witho ut any signs o f he patic fail-ure . Che m o the rap y and rad io the rap y we re give n. Five m o nths late r, the lym p had e no p athy had re -gressed, b ut cho lestasis co ntinued to increase. Liver transplantatio n was co nsidered, b ut the patient died with signs o f he patic failure .
In all the se fo ur case s de scrib e d in the lite ra-ture , as we ll as in the pre se nt o ne , vanishing b ile duct syndro me was de te cte d at diagno sis o r at le ast whe n Ho d gkin’s d is e as e s ho we d tum o r ac tivity. Ho we ve r, e ve n afte r a go o d re sp o nse to c he m o -the rapy, and co m ple te re m issio n o f Ho dgkin’s dis-e asdis-e , vanishing b ildis-e duct syndro m dis-e pro grdis-e ssdis-e d. All patie nts die d fro m irre ve rsib le he patic failure . At auto p s y, no e vid e nc e o f Ho d gkin’s d is e as e was fo und.
The p atho p hysio lo gy o f vanishing b ile d uc t syndro m e is no t we ll unde rsto o d. Im m uno lo gical m e chanism s se e m to b e invo lve d. Hub sche r, e t al.2
sugge ste d that the re is a re le ase o f to xic cyto kine s fro m lym pho m a ce lls in Ho dgkin’s dise ase . The de -structio n o f b ile ducts in prim ary b iliary cirrho sis, p rim ary sc le ro sing c ho langitis and live r allo graft re je ctio n se e m s to b e re late d to ce llm e diate d im -m uno lo gical attack b y cyto to xic T ly-m pho cyte s o f e ithe r CD4 o r CD8 phe no type . Othe r inve stigatio ns have indicate d the pre se nce o f im m uno glo b ulins in inte rlo b ular b ile ducts, sugge sting the invo lve m e nt o f hum o ral im m une re actio ns. Ho dgkin’s dise ase may b e asso ciated with auto immune manifestatio ns b ut, e ve n with co mple te re missio n o f Ho dgkin’s dis-e asdis-e aftdis-e r chdis-e m o thdis-e rapy, vanishing b ildis-e duct syn-dro m e is irre ve rsib le , pro b ab ly due to the fact that the affe cte d b ile ducts have a lo w re ge ne ratio n ca-pacity.
Patie nts with live r dise ase as the initial m anife statio n o f Ho dgkin’s dise ase have a po o r pro gno -sis. In particular, vanishing b ile duct syndro m e is a pro gre ssive and always fatal co m plicatio n in this se tting, altho ugh so m e re ve rsib le case s have b e e n de scrib e d in asso ciatio n with o the r live r transplan-tatio ns.12 Live r transp lantatio n fo r vanishing b ile
duct syndro m e in Ho dgkin’s dise ase sho uld b e co n-s id e re d . O ur p atie nt d ie d b e fo re any p ro c e d ure co uld b e do ne .
Table . Bioche mical change s and che mothe rapy in the Hodgkin’s dise ase patie nt
Dec 9 7 Feb 9 8 M a r 9 8 Apr 9 8 M a y 9 8 Jun 9 8 Jul 9 8 N orm a l
To tal bilirubin (µmo l/ l) 3 3 .5 2 9 .6 3 7 .1 3 1 .5 3 2 2 5 .2 4 6 <1 .2 Direct bilirubin (µmo l/ l) 2 2 .7 2 0 .6 2 4 .5 2 0 .5 2 2 1 6 .3 2 4 <0 .6
AST (U/ l) 2 0 3 2 2 1 1 9 4 2 5 2 2 2 5 4 5 2 1 0 6 -1 8
ALT (U/ l) 2 0 3 3 1 9 1 7 0 2 1 9 1 3 0 4 1 8 4 4 -2 2
Alkaline Pho sphatase (U/ l) 2 0 4 1 1 4 9 4 3 5 6 6 5 6 1 3 5 8 0 4 2 9 6 4 7 9 7 0 6 5 -2 0 0
γ-G T (U/ l) 8 0 9 1 1 6 7 1 9 7 2 2 5 3 9 2 0 8 5 1 0 3 9 1 8 6 0 4 -2 3 Albumin (g / dl) 3 .6 7 - - 3 .7 8 3 .5 3 .8 2 .7 3 .5 -5 .5
PT (IN R) 1 .3 1 1 .3 1 1 .4 2 - 2 .8 1 .0 2 .2 4 1 .0
R 0 .8 3 1 .3 3 5 .4 1 1 .0
Fibrino g en 3 0 0 1 6 0 -4 5 0
Chemotherapy MO PP/ ABV MO PP/ ABV MO PP/ ABV MO PP/ ABV HDCY VP-16 Death
157
1. Jaffe ES. Malignant Lympho ma: Patho lo gy o f hepatic invo lvement. Semin Liver Dis 1987;7:257-68.
2. Hubscher SG, Lumley AL, Elias E. Vanishing bile duct syndro me: a p o s s ib le m e c hanis m fo r intrahe p atic c ho le s tas is in Ho d gkin’s lympho ma. Hepato lo gy 1993;17(1):70-7.
3. Go ttrand F, Cullu F, Mazingue F, et al. Intrahepatic cho lestasis related to vanis hing b ile d uc t s ynd ro m e in Ho d g kin’s d is e as e . J Pe d Gastro entero l Nutr 1997;24:430-3.
4. Desmet VJ. Vanishing bile duct diso rders. Pro g Liver Dis 1992;10:89-121. 5. Burra P, Elias E. Vanishing bile duct syndro me. Br J Surg 1992;79:604-5. 6. Galperin C, Gershwin ME. Immuno patho genesis o f gastro intestinal
and hepato biliary diseases. JAMA 1997;278(22):1946-55.
7. Klim o P, Co nno rs JM. MOPP/ABV hyb rid p ro gram : c o m b inatio n chemo therapy based o n early intro ductio n o f seven effective drugs fo r advanced Ho dgkin’s disease. J Clin Onco l 1985;3:1174-82.
8. Cervantes F, Brio nes J, Bruguera M, et al. Ho dgkin’s disease presenting as a cho lestatic febrile illness: incidence and main characteristics in a series o f 421 patients. Ann Hemato l 1996;72:357-60.
9. Fo rb e s GM, Je ffre y GP, Shilkin KB, Re e d WD. Carb am aze p ine hepato to xicity: ano ther cause o f the vanishing bile duct syndro me. Gastro entero lo gy 1992;102:1385-8.
10. Altraif I, Lilly L, Wanless IR, Heathco te J. Cho lestatic liver disease with ducto penia (vanishing bile duct syndro me) after administratio n o f clindamycin and trimetho prim-sulphametho xazo le. Am J Gastro entero l 1994;89(8):1230-4.
11. Davies MH, Harriso n RF, Elias E, Hubscher SG. Antibio tic-asso ciated acute vanishing bile duct syndro me: a pattern asso ciated with severe, pro lo nged, intrahepatic cho lestasis. J Hepato l 1994;20(1):112-6. 12. Hubscher SG, Buckels JAC, Elias E, et al. Reversible Vanishing Bile
Duc t Synd ro m e afte r Live r Transp lantatio n: Re p o rt o f 6 Case s. Transplant Pro c 1991;23(1):1415-6.
REFERENCES
r e s u m o
CO N TEX TO : Lesõ es no fígado são relativamente co muns em pacientes co m a Do ença de Ho dg kin. Uma pequena pro po rção do s caso s d e se nvo lve m ic te ríc ia . Re c e nte me nte , a Sínd ro me d o de sa pa re c ime nto do duto b ilia r de se nvo lve u-se na Do e nç a de Ho dg kin. O s mecanismo s dessa do ença são muito po uco co nhecido s até ho je.
O BJETIV O : Descrever um raro caso de co lestase relacio nada à síndro me do desaparecimento do s duto s biliares.
TIPO DE ESTUDO : Relato de Caso .
RELATO DO CASO : Paciente masculino , 3 8 ano s, po rtado r de Do ença de Ho dg kin. A bió psia hepática revelo u ausência de HD e co lestase intra-hepática sendo que do s seis espaço s po rta analisado s ne nhum a pre se nta va duto s b ilia re s no rma is. O tra ta me nto fo i baseado em quimio terapia co nvencio nal e po sterio r quimio terapia e m a lta s do se s e sc a lo na da s. O pa c ie nte a pre se nto u uma má evo lução e faleceu devido a falência irreversível da função hepática, em remissão co mpleta do linfo ma.
PA LAV RA S- CH AV E: Do e nç a d e Ho d g kin. Sínd ro me d o desaparecimento do s duto s biliares. Falência hepática.
Marta Soare s Rossini, MD. Hemato lo gy and Blo o d Transfusio n Center, State University o f Campinas, Campinas, Brazil.
Ire ne Lorand-Me tze , MD. Department o f Internal Medicine, State University o f Campinas, Campinas, Brazil.
Gislaine Borba Olive ira, MD. Hemato lo gy and Blo o d Transfusio n Center, State University o f Campinas, Campinas, Brazil.
Cármino Antonio De Souza, MD. PhD. Department o f Internal Medicine, State University o f Campinas, Campinas, Brazil.
Source s of funding: No t declared
Conflict of inte re st: No t declared
Last re ce ive d: 11 August 1999
Acce pte d: 25 No vember 1999
Addre ss for corre sponde nce :
Cármino Anto nio de So uza
Departamento de Medicina Interna, Faculdade de Ciências Médicas da Universidade de Campinas
Cidade Universitária “Zeferino Vaz” – Caixa Po stal 6198 Campinas/SP – Brasil - CEP 13081-970
e-mail: carmino @ o belix.unicamp.br
p u b lis hin g in fo r m a t io n