w w w . j c o l . o r g . b r
Journal
of
Coloproctology
Original
Article
The
impact
of
laparoscopic
surgery
in
colorectal
cancer
resection
with
respect
to
the
development
of
liver
metastasis
in
the
long-term
Renata
Rostirolla
a,∗,
Paulo
Fontes
a,
Mauro
Pinho
b,
Miguel
Pedroso
c,
Tatiana
Masuko
a,
Paula
Novelli
d,
Renato
Lima
d,
José
Sampaio
aaUniversidadeFederaldeCiênciasdaSaúdedePortoAlegre(UFCSPA),PortoAlegre,RS,Brazil
bUniversidadedaRegiãodeJoinville(Univille),Joinville,SC,Brazil
cGeneralSurgeryServiceDepartment,HospitaldoServidorPublicoEstadualdeSãoPaulo(HSPESP),SãoPaulo,SP,Brazil
dLubeckInstituteofResearchandEducation,Lübeck,Germany
a
r
t
i
c
l
e
i
n
f
o
Articlehistory:
Received15August2015 Accepted6December2015 Availableonline1February2016
Keywords: Colorectalcancer Laparoscopicsurgery Video-assistedcolectomy Long-termresults Hepaticmetastases
a
b
s
t
r
a
c
t
Introduction:Colorectalcancer(CRC)showshighincidenceandmortalityworldwide, partic-ularlyinWesternanddevelopedcountries.Theobjectiveofthisstudyistoevaluatethe oncologicresultsduringaminimumfollow-upof2yearsofcurableCRCpatients submit-tedtolaparoscopicresectioninourenvironment,regardingtothedevelopmentofhepatic metastases.
Methods:Medicalrecordsof189colonandrectalpatientswithpotentiallycurable adenocar-cinomawhohavebeensubmittedtolaparoscopicresectionhavebeenreviewedthrougha retrospectivecohortbetweenJanuary2005andMarch2012atasingleinstitutionregarded asreferencetothistypeoftreatment.Pearson’s2andLong-ranktestshavebeenusedfor
statisticalanalysisanddatawasanalyzedbystatisticpackageSTATAversion11.0. Results:Theeligiblepopulationforthestudywas146patients,91 women(62%),witha meanageof61±13years.Minimumfollow-upwas24months,havinganmeanfollow-up of60±27monthsandanmeanfollow-upofglobaldiseaserecurrenceof27±11months. Hepaticmetastasesoccurredin7.5%ofthepopulation,mostfromstageIII,andthemean recurrenceperiodwas25±16months.
Conclusions:LaparoscopicresectionforpotentiallycurableCRCinthiscohortdidnotchange thelong-termincidenceofhepaticmetastases,consideringthatourresultsarecomparable tolargerandomizedclinicaltrialresults.Laparoscopicresectionwaseffectiveandsafefor analyzedpatients,regardinglong-termoncologicresults.
©2016SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.All rightsreserved.
∗ Correspondingauthor.
E-mail:rerostirolla@terra.com.br(R.Rostirolla).
http://dx.doi.org/10.1016/j.jcol.2015.12.002
Impacto
da
cirurgia
videolaparoscópica
em
ressecc¸ões
de
câncer
colorretal
quanto
ao
desenvolvimento
de
metástases
hepáticas
a
longo
prazo
Palavras-chave: Câncercolorretal Cirurgialaparoscópica Colectomiavídeo-assistida Resultadosalongoprazo Metástaseshepáticas
r
e
s
u
m
o
Introduc¸ão: Ocâncercolorretal(CCR)apresentaelevadaincidênciaemortalidademundial, especialmentenospaísesocidentaisedesenvolvidos.Oobjetivodesteestudoéavaliar, duranteum seguimentomínimode2anos,pacientescomCCRpotencialmentecurável submetidosaressecc¸õeslaparoscópicas,emrelac¸ãoaosurgimentodemetástases hepáti-cas.
Métodos: Atravésdecoorte retrospectivaforamrevisadosos prontuários de189 porta-doresdeadenocarcinomadecóloneretopotencialmentecuráveis,submetidosaressecc¸ão laparoscópicaentrejaneirode2005emarc¸ode2012,numaúnicainstituic¸ãoconsiderada dereferêncianestetipodetratamento.Paraanáliseestatísticaforamusadosoteste2de PearsoneotesteLog-rank,eosdadosforamanalisadospelopacoteestatísticoSTATAversão 11.0.
Resultados: Apopulac¸ãoelegíveldoestudofoide146pacientes,sendo91mulheres(62%), comidademédiade61±13anos.Oseguimentomínimofoide24meses,sendootempo médiodeseguimentode60±27meses,eotempomédioderecorrênciaglobaldadoenc¸a de27±11meses.Metástaseshepáticasocorreramem7,5%dapopulac¸ão,amaioria prove-nientedoestadioIII,eotempomédioderecorrêncianofígadofoide25±16meses. Conclusões:Paraestacoortearessecc¸ãodoCCRpotencialmentecurávelporvialaparoscópica nãomodificouaincidênciademetástaseshepáticasalongoprazo,aocompararnossos resultadosaosdosgrandesensaiosclínicosrandomizados.Paraospacientesanalisados,a ressecc¸ãolaparoscópicafoieficazeseguraemrelac¸ãoaosresultadosoncológicosalongo prazo.
©2016SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda. Todososdireitosreservados.
Introduction
Worldwide,colorectal cancer (CRC)is the third most com-monmalignancyandthefourthmostresponsibleformortality relatedtocancer.1Itsincidenceishigherinindustrializedand
Westerncountries,suchasthoseinWesternEurope,USAand Australia, andis growingin Asiancountries suchas Japan andHongKong,wherehistoricallytheriskofthediseasewas low.2–6 Itsincidenceisalsohigh inBrazil;and fortheyear
2014,theNationalCancerInstitute(INCA)estimated32,600 newcases.7
Despitethemedicaltechnologyandpharmaceutical indus-try advancementsobserved, surgicalresectionremains the maintherapeuticmodalityforCRC,beingtheonlyconsidered curative.8–11
Afterinitialreportsofcolorectalresectionsbylaparoscopy, fromthefirstpublicationin1991byJacobsetal.12the
tech-niquehasbecomewidespread.Concernsaboutthequalityof resection,including the statusofsurgical marginsand the radicalismofthelymphadenectomy,andalsoaboutthe long-term oncologicalresults, prompteda series ofstudies and randomizedprospective clinical trials, the most important beingtheBarcelona,COST,CLASICCandCOLORstudies.13–23
Theresultsofthesetrialsshowedthat,inexperiencedhands, laparoscopyhasabeneficialeffectonpost-operativerecovery, whencomparedtoopensurgery,withoutcompromisingthe oncologicalresultsinthelongrun.
Becauseofnumerouspublicationsspeakinginfavorofthe techniqueandtheincreasingabilityofsurgeons,therewas asignificant increaseinthe numberofcolorectalsurgeries bylaparoscopyinthelastdecadearoundtheworld,andalso amongus.Astheapproachhadastrongpenetrationinthe treatmentofmalignant disease,webelievethatitis neces-sarytoensurethatthegoodresultsobtainedinrandomized clinical trials are similarly occurring also outside of these contexts.
Whereasthemostfrequentsiteofcolorectalmetastasisis theliver,24andlivermetastasesarethemaincauseof
mortal-ityinthesepatients,25thisstudyaimstoverifytheemergence
oflivermetastasisinpotentiallycurableCRCpatients oper-atedbylaparoscopyinareferencecenterinourmidstduring aminimumfollow-upof2years.
Patients
and
methods
Patients
Thisstudyfollowsaretrospectiveobservationalmodel, hav-ingbeensubmittedandapprovedbytheEthicalCommitteeof theHospitaleMaternidadeMunicipalNossaSenhoraMonte Serrat.
(AJCC)andtheInternationalUnionAgainstCancer(IUAC),26
and which underwent laparoscopic surgical resection with curative intent between January 2005 and March 2012 by the same surgical team at a referral center for advanced laparoscopic colorectal surgery: Instituto Lubeck, Itu – São Paulo.
Patientsoperatedinemergencyduetointestinal obstruc-tionor perforation,patients withsynchronousliver metas-tases or other distant metastases (stage IV by AJCC and IUAC),26patientsundergoingsurgerywithoutcurativeintent,
those carriersofconcomitant inflammatory bowel disease, patientsinStage0(carcinomainsitu),andpatientswhose lossoffollow-upoccurredbeforereachingtwoyears postop-erativelywereexcluded.
Preoperativeevaluation
The standard pre-operative evaluation included laboratory tests,includingcarcinoembryonicantigen(CEA),radiography orchesttomography,computedtomography(CT)abdominal andpelvic(incasesofrectaltumor)andcolonoscopy.
Surgicaltechnique
Laparoscopicsurgeryfollowed currentoncologicalpatterns: high lymphovascular ligation, longitudinal and circumfer-entialsafetymargins,comprehensivelymphnoderesection, bowel mobilization and identification of anatomical struc-tureswithouttumormanipulation,protectionofthesiteused forspecimenextraction, and exploration ofthe abdominal andpelviccavity.Thedissectionofthecolonwasperformed onamedial-lateraldirection,withtotalresectionofthe corre-spondingmesocolon.Theresectionoftherectumwasheldin conjunctionwithatotalmesorectalexcision,orfrom mesorec-tumtothelevelofrectalsection.Theanastomosesintheright, transverseanddescendingcolonwereextracorporeal proce-dures,throughtheincisionusedforspecimenextraction,and madebymanualormechanicaltechnique.Colorectal anas-tomosesinsurgeryforsigmoidcolonandrectumconsisted in intracorporeal and mechanical procedures (double stapling).
Complementarytherapy
PatientswithrectaladenocarcinomainclinicalstageT3,T4or withpositivelymphnodesunderwentpreoperativeradiation therapyand chemotherapy, and were treatedwith surgical resectionbetween6and8weeksaftercompletionof neoad-juvanttherapy.
Adjuvantchemotherapywasadministeredtopatientswith cancerof the colonor rectum in stageIII, and topatients in stage II with poorer prognosis criteria, such as vascu-lar,lymphaticandperineuraltumorinvasion,tumorspoorly differentiated,and intestinal wallimpairment ofT4 grade. Patientsagedover75yearsandthosewhorejectedthe treat-mentwerenotsubmittedtoadjuvanttherapy.
Therapeutic radiotherapy and chemotherapy were per-formed as recommended by the National Comprehensive CancerNetwork(NCCN).27
Datacollection
Fromchartreview,thefollowingdatawasrecorded:dateof surgery and ageat thetime ofthe procedure, tumor loca-tionandtypeofcolorectallaparoscopicresection,pathological tests, including degreeof tumordifferentiation, numberof lymphnodesresectedandtheirinvolvement,degreeof intesti-nal wall invasion, and tumor stage according to the TNM stagingsystemproposedbyAJCCandIUAC,statusof proxi-mal,distalandcircumferentialsurgicalmarginsofthesurgical specimen,and postoperativemortalityconsidered untilthe 30thdayofsurgery.
The follow-up data collected were CEA, abdominal and pelvicCT(incasesofrectaltumor),chestradiographyorCT and colonoscopy. Patients without acomplete colonoscopy before the treatmentwere examined aftersurgeryor after adjuvant therapy. The remaining patients repeated the colonoscopyafteroneyearoftreatment;andall,froma com-pleteexamination,underwentendoscopicsurveillanceevery 3–5years.
Follow-up
Thefollow-upwasconsideredfromthedateofsurgerytothe appearanceoflivermetastasis,ordevelopmentofadistant metastasisinanothersite,locoregionalrecurrence,untilthe dateofdeathforreasonsnotrelatedtotheprimarytumor,or untilthelastmedicalvisit.
Statistical
analysis
Thestatisticalanalysisconsistedinverifyingthedistribution and re-codingofthe variables.For thedescriptive analysis, the variables were expressedas mean,standard deviation, frequencydistribution,confidenceintervalsat95%,and per-centage. Weconductedcomparisonsofproportionsamong variablesusingPearson’s2test.
Theassociationamongexposurevariablesandthe appear-anceofmetastasiswasevaluatedbyKaplan–Meieranalysis, using the log-rank test. For this purpose, behavior of the variable “responseatthe endoftheexposureintime”was interpretedinthefollowingpresentation:(i)characterization, foreachpatient,ofthefailuresituation(recurrenceof can-cer), interpreted bythe elapsed timebetween the entryof thepatientinthestudyuntiltheoccurrenceoftheeventof interest; (ii)definition, foreach patient, of thesituation of censorship, interpretedwhenthe eventofinterest hadnot occurreduntiltheendofobservation,oruntilthepatientloss duringfollow-up.
Pvalues<0.05wereconsideredstatisticallysignificant,and thedatawereanalyzedusingthestatisticalpackageSTATA version11.0(StataCorp,CollegeStation,TX,USA).
Results
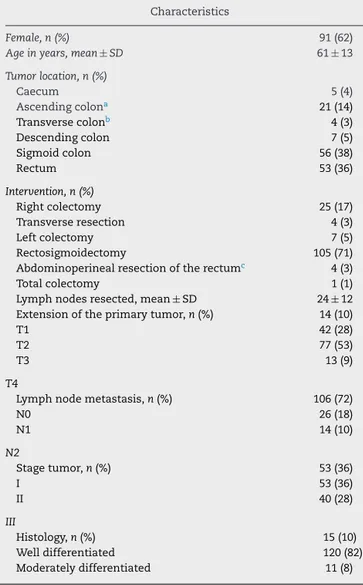
Table1–Clinicalcharacteristicsofpatients.
Characteristics
Female,n(%) 91(62)
Ageinyears,mean±SD 61±13
Tumorlocation,n(%)
Caecum 5(4)
Ascendingcolona 21(14)
Transversecolonb 4(3)
Descendingcolon 7(5)
Sigmoidcolon 56(38)
Rectum 53(36)
Intervention,n(%)
Rightcolectomy 25(17)
Transverseresection 4(3)
Leftcolectomy 7(5)
Rectosigmoidectomy 105(71)
Abdominoperinealresectionoftherectumc 4(3)
Totalcolectomy 1(1)
Lymphnodesresected,mean±SD 24±12 Extensionoftheprimarytumor,n(%) 14(10)
T1 42(28)
T2 77(53)
T3 13(9)
T4
Lymphnodemetastasis,n(%) 106(72)
N0 26(18)
N1 14(10)
N2
Stagetumor,n(%) 53(36)
I 53(36)
II 40(28)
III
Histology,n(%) 15(10)
Welldifferentiated 120(82)
Moderatelydifferentiated 11(8)
Samplesize=146patients;n,numberofpatients;%Percentage;SD, standarddeviation.
a Includesthehepaticangle.
b Includessplenicangle.
c Rectumamputation.
2012,werereviewed.Astheexclusioncriteria,43patientswere excludedfromthissample.
The population eligible for analysis in this study was composed of 146 patients; 91 were female (62%) and the mean age was 61±13 years. The most frequent tumor site was sigmoid colon (56/38%), and the more often per-formed intervention was a retosigmoidectomy (105/71%). The mean number of resected lymph nodes was 24±12, and 3 cases had compromised their circumferential surgi-cal margin (<2mm disease-free margin); these were cases ofrectalcancerwith infiltrationoftheintestinal wall(T4). A patient with impaired surgical margin showed locore-gionalrecurrence24 monthsafterresectionoftheprimary tumor. There were no cases of compromised longitudinal margins. Tumor stages more incident in this population were I and II, with 53 cases each. Most tumors exhib-iteda moderate degree oftumor differentiation (120/82%). The characteristics of the study population are shown in
Table1.
Table2–Tumorrecurrenceandmortality.
Overalltumorrecurrence,n(%) 19(13.5) Recurrencetype,n(%)
Livermetastasis 11(7.5)
Pulmonarymetastasis 4(3)
Regionallocus 3(2)
Carcinomatosis 1(1)
Recurrencetimeinmonths, mean±SD
27±11
Follow-uptimeinmonths, mean±SDPerioperative mortality,n(%)
60±27
Overalltumorrecurrence,n(%) 1(1)
Samplesize=146patients;n,numberofpatients;%,percentage;SD, standarddeviation.
As the minimumfollow-up given inthe study was two
years,patientsoperateduntilMarch2012wereincluded. Theoveralltumorrecurrenceoccurredin19patients, rep-resentinganincidenceof13%ofthestudypopulation.Liver, lung,locoregionalsitesandperitoneum(carcinomatosis)were the sitesofrecurrence,asshown inTable2. There wasno recurrenceatthesiteoftrocars.Themostfrequentlocationof metastaseswasintheliver,occurringin11patients(7.5%).The meantimeofoveralldiseaserecurrencewas27±11months, with a mean follow-up of the study population of 60±27 months.Theoperativemortalitywasonlyonefemalepatient withstageII,victimizedbyapulmonarythromboembolismon the12thpostoperativeday.Table2showsthetypesof recur-renceandthefollow-uptimeuntiltheevent.
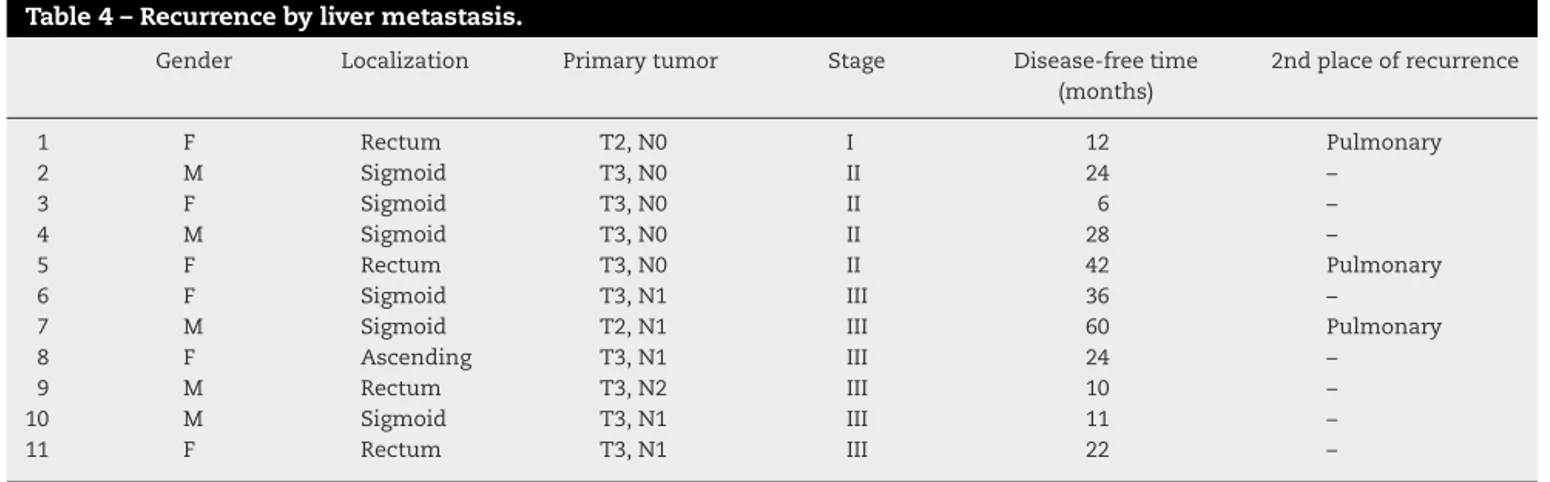
PatientswithstageIIIhadahighernumberofrecurrences (10/7%)(P0.030),andalowermeantimeuntilitsoccurrence (21months),comparedtotheotherstages(CI95%:16–26)(P 0.05),astatisticallysignificantdifference,asshowninTable3. Of the 11 patients who developed livermetastases, the majority came from the stage III, and seven patients had primary colon tumor. Three patients with liver metastasis simultaneouslypresentedlungmetastases,andtwoofthese patientsexhibitedprimaryneoplasmoftherectum,andoneof thecolon.Themeantimetorecurrenceintheliverwas25±16 months.Table4showstheprofileofpatientswhodeveloped livermetastases.
Discussion
Colorectal cancer is a public health problem worldwide, becauseinadditionofitshighincidence,thisdiseaseis asso-ciatedwithhighmortality.Theprognosisisgoodifthedisease isdiagnosedatanearlystage,1,2,28butabout25%ofpatients
already have liver metastases at diagnosis.24,29 The policy
Table3–Recurrenceofdiseasebystage.
Recurrence I II III Total
Numbera,n(%) 3(2) 6(4) 10(7) 19(13)
Timeinmonthsb,Mean(CI95%) 40(9–71) 31(24–38) 21(16–26) 27(21–33)
Samplesize=146patients;n,numberofpatients;%,percentage;CI95%,confidenceintervalof95%. a Pearson’s2test,P0.030.
b Log-ranktest,P0.05.
Table4–Recurrencebylivermetastasis.
Gender Localization Primarytumor Stage Disease-freetime (months)
2ndplaceofrecurrence
1 F Rectum T2,N0 I 12 Pulmonary
2 M Sigmoid T3,N0 II 24 –
3 F Sigmoid T3,N0 II 6 –
4 M Sigmoid T3,N0 II 28 –
5 F Rectum T3,N0 II 42 Pulmonary
6 F Sigmoid T3,N1 III 36 –
7 M Sigmoid T2,N1 III 60 Pulmonary
8 F Ascending T3,N1 III 24 –
9 M Rectum T3,N2 III 10 –
10 M Sigmoid T3,N1 III 11 –
11 F Rectum T3,N1 III 22 –
oncologicalresultsinthelongrun.30 Theaimofthisstudy
wastodeterminewhetherthe goodresultsoflaparoscopic colorectalsurgery thatabound inthe currentinternational literature,14–23 are in fact occurringin ourcountry, thatis,
outsidethefavorablecontextofrandomizedcontrolledtrials. Despitethedifficultyofperformingaretrospectivecohort due the incomplete data storage and loss to follow up of patients,146patientswithcolonandrectaladenocarcinomas instagesI–IIIsubmittedtosurgicallaparoscopywithcurative intentandwithaminimumfollow-upof2yearswereenrolled inthisstudy.Patientstreatedattheinstitutionhere consid-eredare submitted tosurgerythrough laparoscopy,almost withoutexception,irrespectiveofexhibitingphysicaland/or tumorcharacteristicsfavorabletothetechnique.Duetothe highdegreeofsurgicalteamexpertise,conversionsto laparo-tomyoccuronlyrarely,althoughcompliancewiththeserates extrapolatesthenature ofthisstudy.Patients withtumors atall stages,exceptthosemetastatic ones,includingthose with locally advanced, bulky tumors, were included. Like-wise,patientswithtransversecolon,splenicangleandrectum malignancies,whichare consideredtechnicallymore labor-intensiveanddifficulttoresectlaparoscopically,participated inthisstudy,makingoursamplebroader,comparedtothatof recentlypublishedclinicaltrialsthatexcludedpatientswith tumorsintheselocations.14,18,20,22,31
Inthepopulationstudied,62%oftumorshadinfiltration into the intestinalwall(T3 and T4),making up agroup of patientswithlocallyadvancedtumors;andalmostonethird ofpatients(28%)wasinstageIII. Despitethe greater tech-nicaldifficulty toresect rectal tumors,taking into account thatthepelviccavityisnarrowandsurroundedbyrigidbony structuresthatmakeitdifficultthelaparoscopic instrumen-tation, 36% of our population was operated for colorectal neoplasia.
Sixty-twopercentofpatientswerefemale,differingfrom theworldliterature,whichpointstomaleshavingahigher incidence inmost populations,1,2,4 but accordingto
Brazil-iandata,thatshowahigherrelativeriskforwomeninour country.1Regardingage,thestudypopulationhadameanage
of61years,andthisageprofilematchesuptocurrentdata, showingthat90%ofCRCpatientswereover50yearsoldat diagnosis.4,6
Thestudy wasdesignedforaminimum follow-upof24 months,accordingtodataoftheAmericanSocietyof Clini-calOncology(ASCO)andotherstudiesthatdemonstratethe occurrenceof75–80%ofrelapsesoccurringwithinthefirsttwo years afterresectionoftheprimarytumor.32,33 Considering
thatthemeanfollow-upwas60±27monthsforthiscohort, itislikelythatourrecordshaveincludedthemajorityofthe recurrences,makingthisarelevantstudyfortheverification oflong-termoncologicalresults.
Theliteraturepointstotwomajorcriteriarelatedto qual-ityoftumorresection:thestatusofsurgicalmarginsandthe qualityoflymphadenectomy.2,33
Regarding thesurgicalmarginswefoundarateof5.66% ofcircumferentialmarginscommitted,consideringonlycases ofrectalsurgery,sincethiscommitmentwasobservedin3 of 53 patients operated forrectal adenocarcinoma, and in nocaseofcolonictumor.Thefirstlargerandomizedclinical trialincluding patientswithrectalcancerwastheCLASICC study,whichshowedpositivecircumferentialmarginsin12% for the group laparoscopically operated versus 6% for the groupofopensurgery.20 AlsoincomparisonwithCOLORII
study,weconsideredaspositivityforcircumferentialmargin commitmentthepresenceoftumorcellsinthoseoutermost radial2mmofthesurgicalspecimen.Althoughsomeauthors considerthethicknessof1mmfreeofneoplasticcellsas suffi-cient,andNagtegaaletal.concludedthatthelocalrecurrence riskofrectalneoplasmschangesfrom5.8%to16%whenthe circumferentialsurgical safetymargin isgreater orsmaller than2mm,respectively.35
Thenumberoflymphnodesremovedduringresectionof colorectal malignancyis used as aquality criterion ofthe oncologicalresection.36 TheAJCCconsidersthatatleast12
lymphnodesshouldbeinthesurgicalspecimenforaproper oncologicalstaging.2Inthisstudy,themeannumberoflymph
nodesresectedwas24±12which,besidesdemonstratingthe adequacyoflymphadenectomy,exceedsthemeanpublished byseveralotherauthorslikeLacyetal.,Bragaetal.andLiang etal.,amongothers.37,38
Theoverallrecurrencerateofthediseasewas13%,with the additionof hepatic,lung, and locoregionalrecurrences and of peritoneal carcinomatosis. Historically, these sites arethemostaffectedwhenthereistumordissemination.32
The data in the literature are quite variable, with rates of relapse between 9% and almost 30%, usually observed up to 5 years after resection of the primary tumor.16–23
Amongthe studies with a greater number of patients are theBarcelona,19 ConventionalversusLaparoscopic-Assisted
Surgery in Colorectal Cancer (CLASICC),21 and the Colon
CancerLaparoscopicorOpenResection(COLOR),23which
pub-lishedoverallrecurrenceratesof16.98%,23.57%and19.66%, respectively.Consideringtheseandotherlarge-scaletrials,we foundthattheoverallrecurrenceratefoundinthisstudyis lowerthanthemeanofcontemporarystudies.37,38Webelieve
thatthefavorableresultsobtainedheremaybedue,atleast inpart,tothehightechnicalexpertiseandextensive experi-enceinlaparoscopiccolorectalsurgeryofthesurgicalteam, consideringthecriteriathatqualifytheoncologicresections aforementioned.
Some authors such as Braga et al., Leung et al., Liang etal.,andMirzaetal.foundincidencesofdistantmetastases between14%and20%inthelongterm.37,38
Ourgoalwastoidentify,specifically,theincidenceofliver metastases,sincethesearemainlyresponsibleforthe mor-tality associated with CRC.25 In our study, we found liver
diseaserecurrencein7.5%ofpatientsoperated laparoscop-ically.MostpatientswiththisrelapsepatternwereinstageIII. Inaprospectivenon-randomizedstudycoordinatedby Felli-ciottietal.whichevaluated197patientsundergoingrightor lefthemicolectomyfortreatmentofCRC,the grouptreated withlaparoscopyhadaliverrecurrencerateof8.1%fromthe disease,comparedto10.7% inpatients operatedby laparo-tomywithafollow-upofthreeyears.39Stilltakingintoaccount
the incidenceofliver metastases published inthe Clinical OutcomesofSurgicalTherapy(COST)study14whichanalyzed
872patientsoperatedforcolorectaladenocarcinoma(except transversecolon),andthatshowed5.8%ofhepaticrecurrence after5yearsinthegroupoperatedbylaparotomyand5.5% inpatientsundergoinglaparoscopy,ourresultsarethus com-parable.InarecentlypublishedAustraliantrialinvolving601 patientswithcoloncancer(excepttransversecolon),the dis-easerecurredin13.7% ofpatientsoperatedbylaparoscopy,
with60%oftheserecurrenceswereintheliver(8.22%),and mostofthemoccurringinthefirst2yearsaftersurgeryofthe primarytumor.31
Ouranalyzesincludedallcasesofcolonandrectum neo-plasms,anditisworthmentioningthefactthatmorethana thirdofpatientshavebeenoperatedforcolorectalcancer,a locationnotincludedinmostrandomizedclinicaltrials pub-lishedtodate.InaJapanesestudyevaluatingonlyrectaland rectosigmoidtransitiontumors,therateoflivermetastases wasonly1.5%inafollow-upof3years.Thisfinding proba-blywasrelatedtothefactthatonlyT1andT2tumorswere included.40
Incontrast,Laurentietal.,inastudywhichincludedonly rectal neoplasms, with most of the locally advanced type, founddisease-freesurvivalat5yearssimilartolaparoscopy andlaparotomysurgerygroups,withdistantmetastasisrate of20,6%and 24.9%,respectively.41 Inameta-analysisthat
pooled2095patientswithrectalcancerfrom12publications, lateoncologicalresultssimilarbetweenlaparoscopyandopen surgery groups were found.42 COLOR II, an ongoing
clini-cal study,randomized 1044patients with rectal cancerfor laparoscopicresectionoropensurgery;soon,thisstudywill bringmoredefinitiveoncologicalresultsinthelongrun,with respecttotheuseoflaparoscopyforthetreatmentofrectal cancer.34
Inourstudy,wefoundarelationshipbetweenthe segmen-tallocationoftheprimarytumorandincreasedchanceofliver metastasisdevelopment.
Themean timetorecurrenceofthedisease intheliver was27±11months,andthisfinding isconsistentwiththe literature,thatshowstheoccurrenceofmostrelapsesuntil thefirst2.5yearsaftertreatmentoftheprimarytumor.32,33
Theoperativemortalityoccurredinawomanwithastage IItumorduetopulmonarythromboembolismonthe12thday afterthesurgery,despitetheroutineadministrationof anti-coagulantsandearlyambulationintheperioperativeperiod. Thus, the study population had 1% ofoperative mortality, whichiscomparabletodatafromthemeta-analysis involv-ingstudiesofBarcelona,COSTandCLASSIC,whichfounda mortalityof1.6%forconventionalcolorectalsurgeryand1.4% forlaparoscopicsurgery.43
In light of current knowledge, it is observed that the extent and quality ofoncologic resection– specifically the number oflymph nodes removed, colonic or rectal length resected and corresponding mesos, as well as circumfer-ential margins – do not differ between laparoscopy and laparotomy.17,18,20,22 Also withrespecttolong-termresults,
acurrentmeta-analysisthatcompileddatafrommorethan 4500patientsfrom12randomizedclinicaltrialsshowedno differenceastooverallrecurrence,localordistantrecurrence, overall mortality or mortality associated with cancer, and disease-freesurvivalat3and5yearsbetweenresectionsby laparoscopyversusopensurgery.37,38 Whatisstilldebatable
are thelong-termoncologicalresultsoflaparoscopic resec-tions forCRCoutside thecontextofrandomizedcontrolled trials.14,19,21,34
Conclusion
Weconcludethat,forthe populationofthis study,theuse oflaparoscopyintheresectionofpotentiallycurableCRCdid notaltertheincidenceoflivermetastasesinthelongterm, comparedtopublicationsofinternationalrandomizedclinical trials.Forthepatientsanalyzed,laparoscopicresectionwas consideredasaneffectiveandsafemethodinthetreatment ofCRC,concerningoncologicalresultsinthelongrun.
Conflict
of
interests
Theauthorsdeclarenoconflictofinterests.
r
e
f
e
r
e
n
c
e
s
1. LabiancaR,NordlingerB,BerettaGD,MosconiS,MandalàM, CervantesA,etal.Earlycoloncancer:ESMOclinicalpractice guidelinesfordiagnosis,treatmentandfollow-up.AnnOncol. 2013;24Suppl6:vi64–72.
2. Habr-GamaA,CamposFGCM,PerezRO,JuliãoGPS,
ProscurshimI.Prevenc¸ãoerastreamentodocâncercolorretal.
In:CamposFGCMde,RegadasFSP,PinhoM,deSL,editors.
TratadodeColoproctologia.SãoPaulo:Atheneu;2012.p.
331–8.
3. AmericanCancerSocietyColorectalCancerFacts&Figures 2014–2016.Availableat:http://www.cancer.org/acs/groups/ content/@epidemiologysurveilance/documents/document/
acspc-028323.pdf[Accessed2015].
4. WestNP,KobayashiH,TakahashiK,PerrakisA,WeberK,
HohenbergerW,etal.Understandingoptimalcoloniccancer
surgery:comparisonofJapaneseD3resectionandEuropean
completemesocolicexcisionwithcentralvascularligation.J
ClinOncol.2012;30(15):1763–9.
5. DinizFF,PerondiF,Gonc¸alvesJA.Epidemiologiaefatoresde
risco.In:CamposFGCMde,RegadasFSP,PinhoM,deSL,
editors.TratadodeColoproctologia.SãoPaulo:Atheneu;2012.
p.303–11.
6. PolignanoFM,QuynAJ,SanjayP,HendersonNA,TaitIS.
Totallylaparoscopicstrategiesforthemanagementof
colorectalcancerwithsynchronouslivermetastasis.Surg
Endosc.2012;26(9):2571–8.
7. InstitutoNacionaldeCâncerJoséAlencarGomesdaSilva, Coordenac¸ãodePrevenc¸ãoeVigilância(2014).Estimativa 2014:IncidênciadeCâncernoBrasil.Availableat:http://www. inca.gov.br/estimativa/2014/estimativa-24042014.pdf
[Accessed2015].
8. LawWL,PoonJTC,FanJKM,LoOSH.Survivalfollowing
laparoscopicversusopenresectionforcolorectalcancer.IntJ
ColorectalDis.2012;27:1077–85.
9. VendraminiDL,AlbuquerqueMM,SchmidtEM,Rossi-Junior
EE,GerentWdeA,CunhaVJ.Laparoscopicandopen
colorectalresectionsforcolorectalcancer.ArqBrasCirDig.
2012;25(2):81–7.
10.LeeJK,DelaneyCP,LipmanJM.Currentstateoftheartin laparoscopiccolorectalsurgeryforcancer:updateonthe multi-centricinternationaltrials.AnnalSurgInnovRes. 2012;6:5.
11.CormanML.Carcinomaofthecolon.In:CormanML,editor.
Colonandrectalsurgery.Philadelphia:LippincottWilliams&
Wilkins;2005.p.767–904.
12.JacobsM,VerdejaJC,GoldsteinHS.Minimallyinvasivecolon
resection(laparoscopiccolectomy).SurgLaparoscEndosc.
1991;1(3):144–50.
13.MoussaOM,RajaganeshanR,AbouleidA,CorlessDJ,SlavinJP,
KhanA,etal.Single-centercomparativestudyoflaparoscopic
versusopencolorectalsurgery:a2-yearexperience.Surg
LaparoscEndoscPercutanTech.2012;22(1):29–32.
14.FleshmanJ,SargentDJ,GreenE,AnvariM,StrykerSJ,Beart
RWJr,etal.Laparoscopiccolectomyforcancerisnotinferior
toopensurgerybasedon5-yeardatafromtheCOSTstudy
grouptrial.AnnSurg.2007;246(4):655–64.
15.JayneDG,ThorpeHC,CopelandJ,QuirkeP,BrownJM,Guillou
PJ.Five-yearfollow-upofthemedicalresearchcouncil
CLASSICCtrialoflaparoscopicallyassistedversusopen
surgeryforcolorectalcancer.BrJSurg.2010;97:1638–45.
16.WeeksJC,NelsonH,GelberS,SargentD,SchroederG.
Short-termquality-of-lifeoutcomesfollowing
laparoscopic-assistedcolectomyvsopencolectomyforcolon
cancer.JAMA.2002;287(3):321–8.
17.NelsonH,SargentDJ,WieandHS,FleshmanJ,AnvariM,
StrykerSJ,etal.Acomparisonoflaparoscopicallyassisted
andopencolectomyforcoloncancer.NEnglJMed.
2004:2050–9.
18.LacyAM,García-ValdecasasJC,PiquéJM,DelgadoS,CampoE,
BordasJM,etal.Short-termoutcomeanalysisofa
randomizedstudycomparinglaparoscopicvsopencolectomy
forcoloncancer.SurgEndosc.1995;9:1101–5.
19.LacyAM,DelgadoS,CastellsA,PrinsHA,ArroyoV,Ibarzabal
A,etal.Thelong-termresultsofarandomizedclinicaltrialof
laparoscopy-assistedversusopensurgeryofcoloncancer.
AnnSurg.2008;248(1):1–7.
20.GuillouPJ,QuirkeP,ThorpeH,WalkerJ,JayneDG,Smith
AMH,etal.Short-termendpointsofconventionalversus
laparoscopy-assistedsurgeryinpatientswithcolorectal
cancer(MRCCLASSICtrial):multicentre,randomised
controlledtrial.Lancet.2005;365:1718–26.
21.GreenBL,MarshallHC,CollinsonF,QuirkeP,GuillouP,Jayne
DG,etal.Long-termfollow-upofthemedicalresearch
councilCLASSICtrialofconventionalversuslaparoscopically
assistedresectionincolorectalcancer.BrJSurg.2013;100:
75–82.
22.BonjerHJ,HaglindE,JeekelJ,KazemierG,PahlmanL,Hop
WCJ,etal.Laparoscopicsurgeryversusopensurgeryforcolon
cancer:short-termoutcomesofarandomizedtrial.Lancet
Oncol.2005;6:477–84.
23.BuunenM,VeldkampR,HopWCJ,KuhryE,JeekelJ,HaglindE,
etal.Survivalafterlaparoscopicsurgeryversusopensurgery
forcoloncancer:long-termoutcomeofarandomizedclinical
trial.LancetOncol.2009;10:44–52.
24.FrankelTL,D’AngelicaMI.Hepaticresectionforcolorectal
metastases.JSurgOncol.2014;109:2–7.
25.RuersT,BleichrodtRP.Treatmentoflivermetastases,an
updateonthepossibilitiesandresults.EurJCancer.
2002;38:1023–33.
26.EdgeSB,ComptonCC.TheAmericanJointCommitteeon
Cancer:the7theditionoftheAJCCcancerstagingmanualand
thefutureofTNM.AnnSurgOncol.2010;17:1471–4.
27.NationalComprehensiveCancerNetwork.Availableat:
http://www.nccn.org/[Accessed2014].
28.CamposFGCMde,CaiadoAHM,PintoRA.Estadiamento
pré-operatóriodocâncercolorretal.In:CamposFGCMde,
RegadasFSP,PinhoMdeSL,editors.Tratadode
Coloproctologia.SãoPaulo:Atheneu;2012.
p.343–54.
29.WangC-C,LiJ.Anupdateonchemotherapyofcolorectalliver
metastases.WorldJGastroenterol.2012;18(1):25–33.
30.MatsudaT,FujitaH,KunimotoY,KimuraT,KitaokaH,Asano
advancedcoloncancer:acommunityhospital’sexperience.
Hepatogastroenterology.2012;59(117):1433–6.
31.BagshawPF,AllardyceRA,FramptonCM,FrizelleFA,Hewett
PJ,McMurrickPJ,etal.Long-termoutcomesofthe
Australasianrandomizedclinicaltrialcomparing
laparoscopicandconventionalopensurgicaltreatmentsfor
coloncancer:theAustralasianLaparoscopicColonCancer
Studytrial.AnnSurg.2012;256(6):915–9.
32.CiquiniSA.Seguimentopós-operatórionocâncercolorretal.
In:deCamposFGCM,RegadasFSP,dePinhoMSL,editors.
TratadodeColoproctologia.SãoPaulo:Atheneu;2012.p.
487–92.
33.MeyerhardtJA,ManguPB,FlynnPJ,KordeL,LoprinziCL,
MinskyBD,etal.Follow-upcare,surveillanceprotocol,and
secundarypreventionmeasuresforsurvivorsofcolorectal
cancer:AmericanSocietyofClinicalOncologyclinical
practiceguidelineendorsement.JClinOncol.
2013;31(35):4465–70.
34.vanderPasMHGM,HaglindE,CuestaMA,FürstA,LacyAM,
HopWCJ,etal.LaparoscopicversusopenSurgeryforrectal
cancer(COLORII):short-termoutcomesofarandomised,
phase3trial.LancetOncol.2013;14:210–8.
35.NagtegaalID,MarijnenCA,KranenbargEK,vandeVeldeCJ,
vanKriekenJH.Circunferencialmargininvolvementisstillan
importantepredictoroflocalrecurrenceinrectalcarcinoma:
notonemillimeterbuttwomillimetersisthelimit.AmJSurg
Pathol.2002;26:350–7.
36.AslaniN,Lobo-PrabhuK,HeidaryB,PhangT,RavalMJ,Brown
CJ.Outcomesoflaparoscopiccoloncancersurgeryina
population-basedcohortinBritishColumbia:aretheyas
goodastheclinicaltrials?AmJSurg.2012;204(4):411–5.
37.OhtaniH,TamamoriY,ArimotoY,NishiguchiY,MaedaK,
HirakawaK.Ameta-analysisoftheshort-andlong-term
resultsofrandomizedcontrolledtrialsthatcompared
laparoscopy-assistedandopencolectomyforcoloncancer.J
Cancer.2012;3:49–57.
38.OhtaniH,TamamoriY,ArimotoY,NishiguchiY,MaedaK,
HirakawaK.Ameta-analysisoftheshort-andlong-term
resultsofrandomizedcontrolledtrialsthatcompared
laparoscopy-assistedandconventionalopensurgeryfor
colorectalcancer.JCancer.2011;2:425–34.
39.FelliciottiF,PaganiniAM,GuerrieriM,DeSanctisA,
CampagnacciR,LezocheE.Resultsoflaparoscopicvsopen
resectionsforcoloncancerinpatientswithaminimum
follow-upof3years.SurgEndosc.2002;16:1158–61.
40.HasegawaH,IshiiY,NishiboriH,EndoT,WatanabeM,
KitajimaM.Short-andmidtermoutcomesoflaparoscopic
surgerycomparedfor131patientswithrectaland
rectosigmoidcancer.SurgEndosc.2007;21:920–4.
41.LaurentC,LeblancF,WütrichP,SchefflerM,RullierE.
Laparoscopicversusopensurgeryforrectalcancer.
Long-termoncologicresults.AnnSurg.2009;250(1):54–61.
42.OhtaniH,TamamoriY,AzumaT,MoriY,NishiguchiY,Maeda
K,etal.Ameta-analysisoftheshort-andlong-termsresults
ofrandomizedcontrolledtrialsthatcompared
laparoscopy-assistedandconventionalopensurgeryfor
rectalcancer.JGastrointestSurg.2011;15:1375–85.
43.ReaJD,ConeMM,DiggsBS,DeveneyKE,LuKC,HerzigDO.
UtilizationoflaparoscopiccolectomyintheUnitedStates
beforeandaftertheclinicaloutcomesofsurgicaltherapy