jcoloproctol(rioj).2016;36(1):4–7
w w w . j c o l . o r g . b r
Journal
of
Coloproctology
Original
Article
Neoadjuvant
radiotherapy
in
stage
I
cancer
of
the
lower
rectum
José
Alfredo
dos
Reis
Neto
a,
José
Alfredo
dos
Reis
Junior
b,
Odorino
Hideyoshi
Kagohara
b,
Joaquim
Simões
Neto
b,
Sergio
Oliva
Banci
b,
Luciane
Hiane
Oliveira
b,
Gustavo
Alejandro
Gutierrez
Espinoza
a,
Antonio
José
Tiburcio
Alves
Júnior
a,∗aServiceofColoproctology,ClínicaReisNeto,Campinas,SP,Brazil
bClínicaReisNeto,Campinas,SP,Brazil
a
r
t
i
c
l
e
i
n
f
o
Articlehistory: Received12June2015 Accepted18August2015
Availableonline21December2015
Keywords: Rectalneoplasms Radiotherapy Mortality Irradiation
a
b
s
t
r
a
c
t
Introduction:Themortalityrateinlowrectalcancerisrelatedtopelvicanddistant recur-rence.ForstageItumors,localexcisionhasbeingusedincreasingly,butrecentstudiesshow theneedforcautionwiththeuseofthistechnique,astheydonotconsiderthepossibility ofapositivenodeinstageIrectaltumors.Therefore,preoperativeradiotherapyshouldbe consideredforearlytumors,asanattempttopreventrecurrence.
Objective:ShowtheeffectivenessofneoadjuvantradiotherapyinstageIcancerofthelower rectumofacohortpopulation.
Materialandmethod:Acohortstudyinaprospectivedatabasewasmadewithatotalof538 patients,ofwhichwereconsidered75patientswithstageIlowerrectalcancer.Preoperative radiotherapywasperformedandpatientswerefollowedupforaminimumperiodoffive years.
Results:StageI/TIgrouphad27patients.Allofthempresentedcompleteresponsetothe treatmentanddidnotneedtobeoperated.Duringthefollowuptimeoffiveyears,this groupshowednorecurrencerate.ThestageI/TIIgrouphad48patients.Duringthefollow up,8patientshadtobeoperatedduetosuspiciouslesionorscar.Theyweresubmittedto fulltotallocalexcision.Afterevaluatingthepathologicalspecimen,noneofthemprovedto beadenocarcinoma.
Conclusion:Preoperativeradiation,notonlyreducedthelocalrecurrenceandmortalityrate inlowerrectalcancer,butalsoreducedtheneedforsurgeryinpatientswithstageIcancer. ©2015SociedadeBrasileiradeColoproctologia.PublishedbyElsevierEditoraLtda.All rightsreserved.
∗ Correspondingauthor.
E-mails:antonioxxxv@yahoo.com.br,reisneto@lexxa.com.br(A.J.T.AlvesJúnior). http://dx.doi.org/10.1016/j.jcol.2015.12.001
jcoloproctol(rioj).2016;36(1):4–7
5
Terapia
neoadjuvante
para
tumores
de
reto
baixo
estadio
I
Palavras-chave: Neoplasiasretais Radioterapia Mortalidade Irradiac¸ão
r
e
s
u
m
o
Introduc¸ão: Opercentualdemortalidadeempacientescomcâncerderetobaixoestá rela-cionadoarecorrênciaspélvicaeremota.NocasodetumoresnoestágioI,aexcisãolocalvem sendoutilizadacadavezmais;contudo,estudosrecentementepublicadosdemonstrarama necessidadedesetercautelacomousodessatécnica,pornãoselevaremconsiderac¸ãoa possibilidadedeumnodopositivoemtumoresderetonoestágioI.Portanto,aradioterapia pré-operatóriaéumaopc¸ãoviávelparaostumoresemfaseinicial,comoumatentativade evitarrecorrência.
Objetivo: Demonstraraeficáciadaradioterapianeoadjuvanteemcasosdecâncerdereto baixonoestágioIemumacoortedapopulac¸ão.
Materiaisemétodos: Foirealizadoumestudodecoorteemumbancodedados prospec-tivo,comenvolvimento,nototal,de538pacientes,dosquais75foramconsideradoscomo tendocâncerderetobaixonoestágioI.Nopré-operatório,ospacientesforamtratadoscom radioterapiaeseguidosduranteumperíodomínimode5anos.
Resultados: OGruponoestágioI/TIconsistiaem27pacientes.Todosobtiveramresposta completaaotratamentoenãohouvenecessidadedereoperac¸ão.Duranteoperíodode5 anosdeseguimento,nãohouverecorrênciasnessegrupo.OgruponoestágioI/TIIconsistia em48pacientes.Duranteoseguimento,8pacientestiveramqueseroperados,devidoà sus-peitadelesão,oucicatriz.Paraessescasos,optou-seporexcisãolocaltotalcompleta.Após aavaliac¸ãodosespécimespatológicos,nenhumdelestevediagnósticodeadenocarcinoma. Conclusão: O usoda radiac¸ão pré-operatória nãosó diminuiua recorrência local e o percentualde mortalidadeemcasosde câncerde retobaixo,mas tambémdiminuiua necessidadedecirurgiaempacientescomcâncernoestágioI.
©2015SociedadeBrasileiradeColoproctologia.PublicadoporElsevierEditoraLtda. Todososdireitosreservados.
Introduction
Preoperativeradiotherapyincancerofthelowerrectumhas beenusedsince1975.1However,duringthelastdecade
sub-stantialprogresshasbeenmadeintreatmentmodalities.The surgicalmanagementcurrentlyincludesabroadspectrumof operativeproceduresrangingfromradicaloperationsto inno-vative sphincter-preserving techniques; new and improved radiationtechniquesemerged(conformalradiotherapy, intra-operative radiotherapy) with or without combinations of chemotherapies.2–5Themortalityrateisrelatedtopelvicand
distantrecurrence.6Therefore,adequatesurgicaltechniqueis
mandatoryinthetreatmentoftherectalcancer.6,7Also
crit-icalistheroleofprognosticfactorssuchasthepathologicT (tumor)andN(nodal)classification,circumferentialresection margin,andresponsetopreoperativetherapy.3Nodescanbe
positiveeveninearlytumors.8
For stage I rectal cancer, local excision has being used increasingly, but recent studies show the need forcaution withthe useofthistechnique,astheydonotconsiderthe possibilityofapositivenodeinstageIrectaltumors.3,7,8
Nowadays, appropriate staging plays an increasingly importantrole,becausemanytreatmentdecisionsmust be basedonpreoperativestaging.2,3
Currentguidelinesadvocateforneoadjuvanttreatmentfor stageIIandIIItumors,onceithasbeenprovedthat preop-erativeradiationreduceslocalrecurrenceriskand improve long-termsurvival.9–12
However,knowingthatpre-operativeradiotherapyisable todecrease,significantly,thenumberofundifferentiatedcells; diminishthegradeoftumorinvasionintherectalwall;reduce, statistically,theincidenceoflocalrecurrenceandalter long-termsurvivalrateleadstobelievethatneoadjuvanttherapy shouldbeusedinearlytumorsaswell,preventinga recur-renceratemanytimesreportedinstageIpatients.1
Objectives
ShowtheeffectivenessofneoadjuvantradiotherapyinstageI cancerofthelowerrectumofacohortpopulation.
Methods
Acohortstudyinaprospectivedatabasewasmadefrom1978 to2012,withatotalof538patientswithlowerrectum can-cer,ofwhichwereconsidered75patientswithstageIcancer. Theseindividuals weresubmittedtopreoperative radiothe-rapy.Theywere27patientsstageI/TIand48patientsstage I/T2.Allofthemhadlowerrectumadenocarcinomaandwere followedbya5-yearminimum.
Therewasnogender,raceandagedistinction.
6
jcoloproctol(rioj).2016;36(1):4–7performedtoevaluatesizeandinfiltrationofthetumorbefore andaftertheirradiation.
Proctoscopy and digital examinationwere performed at diagnosis andafterthe endofthe irradiationtreatment to evaluatetumorextensionandwallinfiltration.
Preoperative radiotherapy was performed with 200cGy/dailyfor4consecutiveweeksuptoatotalof4500cGy, by means of a linear megavoltage accelerator (25MeV), in anteriorandposteriorpelvicfields.
Post-radiation protocol included periodical examination every 3monthsforthe firsttwo years,withdigital exami-nation(orcarefulperinealpalpation)and evaluationofthe CEAandevery6monthsforthenextconsecutivethreeyears. Abdominalultrasoundwasperformedyearlyandcolonoscopy everyotheryear.Whenclinicalassessmentsuggestedlocalor generalrecurrence,aCTscanorMRwasaccomplished.
Results
The75patientswithlowerrectumcancerwerefollowedfora minimumperiodof5years.
ThestageI/TIgrouphad27patients,allofthemsubmitted tothesameprotocolofneoadjuvanttherapy.Everyone pre-sentedcompleteresponsetothetreatmentanddidnotneed tobeoperated.Duringthefollowuptimeoffiveyears,this groupshowednorecurrencerate.
ThestageI/TIIgrouphad48patients,allofthemsubmitted tothesameprotocolofneoadjuvanttherapy.Duringthefollow up,8patientshadtobeoperatedduetosuspiciouslesionor scar.Theywere submittedtofulltotallocalexcision.After evaluatingthepathologicalspecimen,noneofthemproved tobeadenocarcinoma.Itwasfounddysplasiaandadenoma (Fig.1).
Onepatientofthisgrouphadadistantmetastasis,after5 yearsthatoccurredinthelungs(Fig.2).
Theother40patientshadcompleteresponseafter neoad-juvantradiotherapy.
Discussion
Treatmentofrectalcancerhasdramaticallyevolvedduring the last three decades shifting toward a tailored approach
27
48
75
0
8
0 10 20 30 40 50 60 70 80
total Stage I/TII
Stage I/TI
Patients Patients operated
Fig.1–Operatedpatients.
50
45
40
35
30
25
20
15
10
5
0
Patients Local recurrence
Distant metastasis
Stage I/TI Stage I/TII 27
48
0 0 0 1
Fig.2–Followupresultsafter5years.
basedonpreoperativestagingandresponsetoneoadjuvant therapy.13
Preoperativeradiotherapyreducestheriskoflocal recur-renceinpatientswithoperablerectalcancerandrecurrence, especially locally, is responsible for the great majority of deathsinthefirsttwoyearsaftersurgery.14
Previous studies showed that there is a significant dif-ference in the five-yearsurvivalrates inpatients receiving preoperativeradiotherapy,whohadacorrectedsurvivalrate of80%versus34.4%ofnonirradiatedpatients.Thelocal recur-rence rate was2.9% inpatients that received neoadjuvant therapyversus23.5%inthosewhohadnot.1
Endorectalultrasound(ERUS)displaysaccuracyof71–91% and69–97%forTstage,and62–83%fornodalstaging.15Results
confirmedin200patients,thataftertheirradiationan involu-tionofthetumorsizeandvolumeoccurred.1
Comparingtootherstudieswhenpreoperative radiothe-rapywasnotusedtherecurrenceratewasmuchhigher.15–19
AccordingtoAguilar, patientsundergoinglocalresection presentedrecurrencerateof18%(T1)and 37%(T2)with54 monthsoffollow-up.
Patyetal.showedratesof17–74%forT1rectalcancersand 26–72%forT2cancerswithamediantimetorelapseof1.4 years(range0.4–7.0).
Patients undergoing localexcision withtransanal endo-scopicmicrosurgerypresentedrecurrenceof13%(T1),17%(T2) withfollowupof24months.18
Bebenekshowed4.4%recurrencerateforT1andT2intwo yearfollowupafterabdominoperinealresection.20
Ontheotherhand,Lezochshowedarecurrencerate simi-lartotheonepresentedinthisstudy,withnorecurrenceinT1 and2.85%inT2.Thesimilarresultsareduetotheuse preoper-ativeradiotherapybeforeperformingatransanalendoscopic microsurgery.21,22
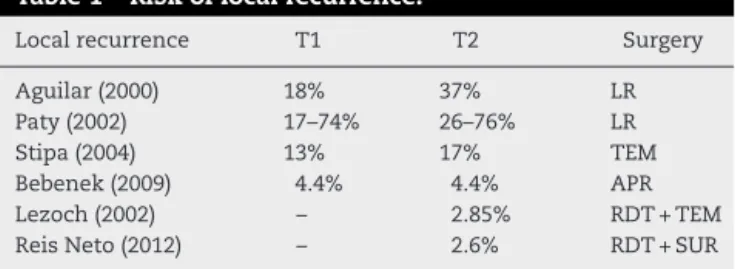
Thoseresultsshownthatreceivingneoadjuvanttherapy carrieslessriskoflocalrecurrencethansurgicaltechniques that did notreceive pre operativeradiotherapy (local exci-sion, transanalendoscopicmicrosurgery, abdominoperineal resection,lowanteriorresection)(Table1).
jcoloproctol(rioj).2016;36(1):4–7
7
Table1–Riskoflocalrecurrence.
Localrecurrence T1 T2 Surgery
Aguilar(2000) 18% 37% LR
Paty(2002) 17–74% 26–76% LR
Stipa(2004) 13% 17% TEM
Bebenek(2009) 4.4% 4.4% APR
Lezoch(2002) – 2.85% RDT+TEM
ReisNeto(2012) – 2.6% RDT+SUR
throughendorectalultrasound,digitalexaminationand endo-scopicaninvolutiononthesizeandvolumeofthetumor.23,24
Thisstudydidnotcontemplatethepossiblecomplications presentedbyradiotherapy oralludedtomolecularanalysis sincethiswasnotitsgoal.
Conclusion
Inthiscohort,theuseofneoadjuvantradiotherapyreduced theriskoflocalrecurrence,themortalityrate,andtheneeded ofsurgeryinstage1cancerofthelowerrectum.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
r
e
f
e
r
e
n
c
e
s
1. ReisNetoJA,ReisJAJr,KagoharaO,SimoesNetoJ,BanciSO, OliveiraLH.Adjuvanttherapyoncancerofthelowerrectum. Evaluationoftheeffectsofpreoperativeradiotherapyonthe prognosisofpatientswithcancerofthelowerrectum.J CancerTher.2012;3:912–9.
2. FicheraA,AllaixME.Paradigm-shiftingnewevidencefor treatmentofrectalcancer.JGastrointestSurg.2014;18:391–7. 3. DasP,CraneCH.Staging,prognosticfactors,andtherapyof
localizedrectalcancer.CurrOncolRep.2009;11:167–74. 4. KachnicLA.Adjuvantchemoradiationforlocalizedrectal
cancer:currenttrendsandfuturedirections.Gastrointest CancerRes.2007;1:64–72.
5. SauerR.Adjuvantandneoadjuvantradiotherapyand concurrentradiochemotherapyforrectalcancer.PatholOncol Res.2002;8:7–17.
6. WagnerTD,FakihMG,YangGY.ManagementofstageII/III rectalcancer.JGastrointestOncol.2010;1:112–9.
7. SauerR,RödelC.Adjuvantandneoadjuvant radiochemotherapyofrectalcarcinoma.Praxis. 2002;91:476–84.
8. PucciarelliS,CapirciC,EmanueleU,ToppanP,FrisoML, PennelliGM,etal.RelationshipbetweenpathologicT-stage andnodalmetastasisafterpreoperativechemoradiotherapy forlocallyadvancedrectalcancer.AnnSurgOncol.
2005;12:111–6.
9. LoosM,QuentmeierP,SchusterT,NitscheU,GertlerR,Keerl A,etal.Effectofpreoperativeradio(chemo)therapyon long-termfunctionaloutcomeinrectalcancerpatients:a
systematicreviewandmeta-analysis.AnnSurgOncol. 2013;20:1816–28.
10.KuluY,UlrichA,BüchlerMW.Resectablerectalcancer:which patientdoesnotneedpreoperativeradiotherapy?DigDis. 2012;30:118–25.
11.RödelC,TrojanJ,BechsteinW-O,WoesteG.Neoadjuvant short-orlong-termradio(chemo)therapyforrectalcancer: howandwhoshouldbetreated?DigDis.2012;30:102–8. 12.KimDY,JungKH.Radiationtherapyforrectalcancer.KoreanJ
Gastroenterol.2006;47:285–90.
13.QuirkP,SteeleR,MonsonJ,GrieveR,KhannaS,CoutureJ, etal.Effectoftheplaneofsurgeryachievedonlocal recurrenceinpatientswithoperablerectalcancer:a prospectivestudyusingdatafromtheMRCCR07and NCIC-CTGCO16randomizedclinicaltrial.Lancet. 2009;373:821–8.
14.Sebag-MontefioreetD,StephensRJ,SteeleR,MonsonJ,Grieve R,KhannaS,etal.Preoperativeradiotherapyversusselective postoperativechemoradiotherapyinpatientswithrectal cancer(MRCCR07andNCIC-CTGC016):amulticentre, randomizedtrial.Lancet.2009;373:811–20.
15.Garcia-AguilarJ,MellgrenA,RothenbergerDA.Localexcision ofrectalcancerwithoutadjuvanttherapy.AnnSurg. 2000;231:345–51.
16.SenguptaS,TiandraJJ.Localexcisionofrectalcancer.Dis ColonRectum.2001;44:1345–61.
17.PhillipP,NashGM,WongWD.Long-termresultsoflocal excisionforrectalcancer.AnnSurg.2002;236:522–30. 18.StipaF,LucandriG,FerriM,CasulaG,ZiparoV.Localexcision
ofrectalcancerwithtransanalendoscopicmicrosurgery (TEM).AnticancerRes.2004;24:1167–72.
19.SuppiahA,HunterIA,CowleyJ,GarimellaV,CastJ,HartleyJE, etal.Magneticresonanceimagingaccuracyinassessing tumordown-stagingfollowingchemoradiationinrectal cancer,MedicalResearchCouncil(UK)andtheNational CancerInstituteofCanada.ColorectalDis.2009;11:249–53. 20.BebenekM,PudełkoM,Cisar ˙zK,BalcerzakA,TupikowskiW,
WojciechowskiL,etal.Abdominosacralamputationofthe rectumforlowrectalcancers:tenyearsofexperience. Therapeuticresultsinlowrectalcancerpatientstreatedwith abdominosacralresectionaresimilartothoseobtainedby meansofanteriorresectioninmid-andupperrectalcancer cases.EurJSurgOncol.2007;33:320–3.
21.LezochE,GuerrieriM,PaganiniAM,D’AmbrosioG,Baldarelli M,LezocheG,etal.Transanalendoscopicversustotal mesorectallaparoscopicresectionsofT2–N0lowrectal cancersafterneoadjuvanttreatment.SurgEndosc. 2005;19:751–6.
22.LezochG,BaldarelliM,GuerrieriM,PaganiniAM,DeSanctis A,BartolacciS,etal.Aprospectiverandomizedstudywitha 5-yearminimumfollow-upevaluationoftransanal
endoscopicmicrosurgeryversuslaparoscopictotal
mesorectalexcisionafterneoadjuvanttherapy.SurgEndosc. 2008;22:278.
23.Habr-GamaA,PerezRO,LynnPB,NetoAS,Gama-RodriguesJ. Nonoperativemanagementofdistalrectalcancerafter chemoradiation:experiencewiththe‘watch&wait’protocol. In:SantoroGA,editor.Rectalcancer,amultidisciplinary approachtomanagement.SaoPaulo:InTechInc.;2011. Chapter17.